Abstract
Background
Significant weight regain occurs for 10% to 20% of patients after Roux-en-Y gastric bypass (RYGB). Potential causative factors include anatomic abnormalities such as enlargement of the gastric pouch and gastrojejunostomy (GJ). This report describes endoscopic findings for patients referred for investigation of weight regain and presents the outcomes of revisional therapy for patients with abnormal anatomy.
Methods
To evaluate gastric pouch and stoma size, RYGB patients referred for weight regain underwent upper endoscopy. A GJ was defined as enlarged if it had a diameter greater than 2 cm in any dimension, and a pouch was defined as enlarged if its length exceeded 6 cm long or its width exceeded 5 cm. Patients with abnormal anatomy who subsequently underwent revisional procedures were arbitrarily categorized into three groups based on the interval from RYGB to endoscopic evaluation: less than 5 years (group 1), 5 to 10 years (group 2), longer than 10 years (group 3). The percentage of regained weight lost (%RWL) after revision was compared between the groups.
Results
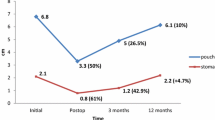
In this study, 205 RYGB patients (176 women with a mean age of 47 ± 10 years and a current body mass index [BMI] of 43.4 ± 8.4 kg/m2) were evaluated. The mean time from primary RYGB was 6.9 ± 3.7 years, and the increase in BMI from its nadir was 9.78 ± 5.80 kg/m2. Abnormal endoscopic findings (n = 146, 71.2%) included large GJ (n = 86, 58.9%), large pouch (n = 42, 28.8%), or both (n = 18, 12.3%). Of the 205 patients, 51 (24.9%) underwent a revisional surgical or endoluminal procedure. At a mean follow-up assessment 13 months after revision, group 1 (n = 12) had a mean %RWL of 103% ± 89.3%, and 62% of these patients lost all their regained weight. The mean %RWL was 45% ± 12.6% in group 2 (n = 30) and 40% ± 13.6% in group 3 (n = 9).
Conclusion
Endoscopy is a valuable tool for evaluating weight regain after bariatric surgery that can identify abnormal post-RYGB anatomy in a majority of patients. Revisional procedures to restore normal RYGB anatomy appear to be most successful if performed within 5 years after the primary procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Roux-en-Y gastric bypass (RYGB) currently is the most commonly performed and successful bariatric procedure performed in the United States. Despite its excellent outcomes in terms of weight loss and resolution of metabolic comorbidities, ~10 to 20% of RYGB patients experience weight regain during 5 to 10 years postoperatively [1–3].
This phenomenon of weight regain has been attributed to a combination of anatomic, behavioral, and psychological factors. Among the anatomic features presumed to be associated with weight regain are dilation of the gastric pouch, gastrojejunostomy (GJ), or both [4–7]. However, evidence demonstrating clear associations between pouch and stoma enlargement and weight regain is sparse, and it is unclear what contribution such anatomic factors make toward gastric bypass failure. Furthermore, it is not certain whether gastric pouch and stoma reduction restore the efficacy of the bypass procedure in all patients who experience weight regain.
Evidence suggests that tightening of a patulous stoma can lead to an excess weight loss (EWL) of approximately 23% [8]. Bessler et al. [9] also reported success with placement of a nonadjustable gastric band around an enlarged gastric pouch to restore the restrictive component of the bypass procedure, achieving an EWL of 38% at 12 months and 44% at 24 months.
Various revision procedures have been described to amend these anatomic defects. Surgical techniques, even those approached laparoscopically, carry a significant risk of operative morbidity and mortality. This concern led to the development of less invasive endoscopic techniques to reduce gastric bypass pouch and stoma diameter. The promising technologies include endoscopic suturing devices and gastric tissue plication platforms [10, 11].
It is not known whether the outcomes of gastric pouch and stoma revision in bypass patients who have regained weight are influenced by the time from initial weight loss surgery to the revision procedure. Given that the risk–benefit ratio for some revisional procedures can be high, it is imperative to identify and select the patients most likely to benefit from further intervention and to intervene at the most appropriate time.
This study aimed primarily to describe the endoscopic findings for gastric bypass patients referred to our practice for investigation of weight regain. Secondarily, the study sought to examine the outcomes of revisional surgery in this cohort, in particular, to assess the relationship between successful weight loss and the interval between primary RYGB and revision.
Methods
Study cohort
Institutional review board approval to conduct this review of a prospectively maintained database at a tertiary referral bariatric center was obtained. All patients who underwent upper endoscopy for investigation of weight regain after RYGB between July 2006 and August 2010 were identified. Patients’ charts were reviewed, and data on their baseline demographics, primary bariatric procedure or procedures, and current presentation for investigation and management of weight regain were obtained.
The patients’ primary bariatric procedure (RYGB) either had been performed at our institution or they had been referred from other centers for management of postoperative weight gain. Three expert surgical endoscopists had performed all the endoscopy procedures.
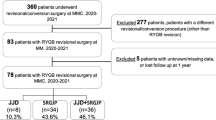
Of the 205 patients who underwent upper endoscopy as part of a workup for weight regain after gastric bypass, 51 proceeded to undergo revisional procedures. The primary indication for intervention in these patients who had regained weight was objective evidence of an anatomic abnormality at upper endoscopy. Additionally, all these patients were assessed preoperatively by a multidisciplinary team including a nutritionist, a psychologist, and a bariatric physician as a minimum. This group also either had insurance to cover the cost of the revision or met criteria for investigational endoluminal procedures.
The revision procedures included laparoscopic placement of an adjustable gastric band or silicone ring around the gastric pouch, resection of an enlarged pouch or stoma with revision of the GJ anastomosis, and endoscopic stoma reduction procedures such as suturing of the anastomosis, use of the EndoCinch device (C.R. Bard, Murray Hill, NJ, USA), or use of the StomaphyX device (EndoGastric Solutions, Inc., Redmond, WA, USA).
This revision cohort was arbitrarily classified into three groups according to the interval between their current presentation with weight regain and their RYGB: less than 5 years after RYGB (group 1), 5 to 10 years after RYGB (group 2), and longer than 10 years after RYGB (group 3). Regained weight was defined as weight gained after a patient’s nadir was reached subsequent to the gastric bypass. The outcome of revisional surgery was assessed using the percentage of regained weight lost (%RWL), which was calculated as follows [12]:
Definition of enlarged gastric bypass pouch and stoma
Consistent with previous reports, abnormal post-RYGB anatomy was defined in this study as a GJ larger than 2 cm or dilation of the gastric pouch (length > 6 cm or width > 5 cm) [13]. The endoscopist measured all gastric pouch and stoma dimensions using an articulating measuring instrument (Fig. 1), introduced through the working channel of a flexible endoscope (Olympus, Centre Valley, PA, USA).
Statistical analysis
Data were analyzed using the software package PASW 18.0 for Windows (Chicago, IL). Descriptive statistics were computed for all variables. Data regarding patient characteristics, management, and outcome are outlined in numbers and percentages. Distribution of the data was checked for normality using the Kolmogorov-Smirnov test. Parametric data are presented as mean ± standard deviation and were analyzed using Student’s two-sample t test for any two-sample comparisons and analysis of variance (ANOVA) followed by the Tukey HSD post hoc test where appropriate. Differences between proportions and categorical variables were determined using the chi-square test.
To determine which variables may be associated with successful weight loss after revision of gastric bypass (p ≤ 0.1), univariate analysis was performed. To identify independent predictors for success, variables identified as significant in univariate analysis without significant intervariable correlation were subsequently entered into a logistic regression model. All tests were two-tailed, and results with a p value less than 0.05 were considered statistically significant.
Results
Characteristics of patients who regained weight after RYGB
Between July 2006 and August 2010, 205 gastric bypass patients (86% women with a mean age of 47 ± 10 years) underwent upper endoscopy for investigation of weight regain. Their baseline characteristics are outlined in Table 1.
All the patients initially lost weight after their primary RYGB, showing a mean EWL of 72.2% (range, 18.5–147.8%). The mean interval from RYGB to upper endoscopy was 6.9 ± 3.7 years. These patients regained an average of 59.9 lb (range, 3–226 lb) from their lowest postbypass weight, resulting in a body mass index (BMI) increase from a nadir of 9.78 ± 5.80 kg/m2. At presentation for endoscopy, their mean BMI was 43.4 ± 8.4 kg/m2.
Endoscopic findings
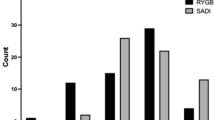
An abnormal post-RYGB anatomy was observed in 71.2% of the patients (n = 146, Fig. 2). Dilation of the GJ was the most common anomaly, identified in 58.9% of the patients (n = 86). An enlarged gastric pouch was found in 28.8% of the patients (n = 42). Abnormalities of both pouch and stoma were observed in 12.3% of the patients (n = 18). The estimated gastric pouch dimensions were a mean length of 5.8 ± 2.6 cm and a mean width of 4.0 ± 1.7 cm. The greatest average diameter of the stoma was 2.5 ± 1.0 cm.
Weight gain was greatest among the patients who had an enlarged stoma as the single anatomic aberration (mean weight gain from nadir, 66 lb; n = 86) compared with those who had enlargement of the pouch alone (mean weight gain from nadir, 53.2 lb; n = 42; p = 0.238) and those who had enlargement of both pouch and stoma (mean weight gain from nadir, 28.3 lb; n = 18; p < 0.001, Fig. 3). There was no significant correlation between the amount of weight regained and the dimensions of the gastric pouch or stoma, although a trend toward a positive relationship between increasing pouch and stoma size and the amount of weight regained was observed (Table 2).
Revision of abnormal pouch or stoma
After endoscopic investigation and evidence of abnormal postbypass gastric anatomy, 51 patients (24.9%) underwent a revision procedure to reduce the size of their gastric pouch, stoma, or both. Of these interventions, 58.8% (n = 30) were performed surgically (all laparoscopically), with 41.2% performed for patients (n = 21) undergoing endoscopic revision. One of the following three endoscopic procedures was performed: (1) endoscopic suturing of the gastrojejunal anastomosis as part of the RESTORe trial (randomized evaluation of endoscopic suturing transorally for anastomotic outlet reduction), which was most commonly performed (17 of 21 cases); (2) use of the endoscopic StomaphyX device (3 of 21 cases), and (3) endoscopic stoma reduction using the EndoCinch device (1 of 21 cases).
On the average, this entire revision cohort had regained 65.5 ± 41.5 lb after their primary RYGB, and their BMI before undergoing the revision procedure was 43.4 ± 8.4 kg/m2. At upper endoscopy, the mean pouch length was 5.9 ± 2.6 cm, and the pouch width was 4.2 ± 1.8 cm. The stoma diameter was 2.5 ± 0.9 cm. During a mean follow-up period after revision of 13 months (range, 3–36 months), this group achieved a mean %RWL of 58.9% ± 160.8%.
A successful outcome, defined as loss of some or all regained weight, was observed for 78.4% of the patients (n = 40). Comparing the mean %RWL of the patients according to the interval between their primary RYGB and their current presentation with weight regain, the %RWL was highest in group 1 (< 5 years after RYGB; 103% RWL) and lowest in group 3 (>10 years after RYGB; 40% RWL) The difference in %RWL between the three groups did not reach statistical significance, although a clear trend toward greater weight loss with a shorter interval from the RYGB was observed (Fig. 4).
Box plot illustrating the percentage of regained weight lost by patients who underwent revision procedures to reduce size of their gastric pouch, stoma, or both according to their time of their presentation with significant weight gain after gastric bypass. Patients did not differ significantly in the percentage of regained weight lost (%RWL) based on whether they presented for a further weight loss intervention within 5 years, in 5 to 10 years, or as late as 10 years after Roux-en-Y gastric bypass (RYGB)
The patients who underwent surgical revision procedures (n = 30) such as placement of a gastric band around an enlarged gastric pouch or resection and redo of the gastrojejunal anastomosis attained a higher %RWL than the patients who underwent endoscopic revisions (n = 21), although the difference between these two groups was not statistically significant (91.6% ± 199.4% and 9.1% ± 36.1%, respectively, p = 0.082).
Only two patients had the Roux limb of their gastric bypass lengthened in addition to revision of the proximal gastrojejunal anastomosis. Furthermore, the surgical revision patients had a significantly higher starting BMI before undergoing revision of their gastric bypass (46.7 ± 9.1 vs. 39.6 ± 3.4 kg/m2; p = 0.001) and they had regained more weight after their primary procedure than the patients who proceeded to undergo endoscopic revision (74.6 ± 51.4 vs 56.7 ± 21.0 lb; p = 0.099).
No difference in %RWL was observed between the three endoscopic revisional procedures (RESTORe, StomaphyX, and EndoCinch; p = 0.224; Table 3). Multivariate analysis, accounting for variables such as age, gender, pre-revision BMI, amount of weight regained, and interval from primary RYGB, showed that the approach to revision (surgery or endoscopic) was not an independent predictor of successful outcome in terms of weight loss achieved (p = 0.063).
No mortality occurred in this series, and the overall morbidity rate after revision procedures was 7.8% (n = 4). All the morbidity occurred for patients who underwent surgical revision. No morbidity was recorded among patients who underwent endoscopic intervention. The morbidity included two cases of gastrojejunal anastomotic stricture, an adjustable gastric band port infection, and a bile leak from liver injury.
Discussion
It is well established that bariatric surgery is the gold standard treatment for the attainment of significant and durable weight loss by morbidly obese patients [14]. Of all the bariatric procedures, the RYGB has consistently demonstrated achievement of optimal results with minimal operative risk and long-term complications. Hence, it has become the procedure of choice in the United States over the past decade [15]. Despite the success of RYGB, 10% to 20% of bypass patients regain weight in the medium to long term and may be offered revisional bariatric surgery [16].
Abnormalities of the postgastric bypass anatomy are postulated to play a significant role in weight regain after RYGB. In particular, enlargement of the gastric pouch and GJ, resulting in loss of restriction, are thought to be responsible for the loss of early satiety and for the increased intake associated with weight regain. Evidence to support this lies in reported findings that restrictive procedures fail if the pouch and stoma are too large [17, 18] and that reduction of the gastric pouch dimensions and stoma diameter induce weight loss once again [19–21]. However, few previous studies have investigated the precise anatomy of a large consecutive series of gastric bypass patients presenting for management of weight regain.
Using upper endoscopy to measure the dimensions of the gastric pouch and stoma in a series of 205 RYGB patients referred to our unit for investigation of significant weight regain, we demonstrate that 71.2% had post-bypass anatomic abnormalities, namely, enlargement of the pouch or stoma. Dilation of the GJ was the most frequently encountered abnormality at upper endoscopy. A total of 104 patients were found to have this defect, 18 of whom also had a dilated gastric pouch.
Our data suggest that stoma enlargement, as an isolated defect, is associated with greater weight regain than an enlarged pouch or even a common dilation of both pouch and stoma. Catalano et al. [19] reported similar findings in a small series of gastric bypass patients, all of whom had a dilated stoma, as determined by endoscopy or upper gastrointestinal barium studies (n = 28). In their series, enlargement of stomas beyond 1.2 cm was associated with a mean weight regain of 28.7 kg (63.3 lb), and reduction of the GJ to less than 1.2 cm using endoscopic injection sclerotherapy was associated with an average weight loss of 22.3 kg (49.2 lb) during a mean follow-up period of 18 months.
Revision procedures to correct pouch and stoma dilation after RYGB have been performed for decades [19, 22–26]. Despite advances in perioperative care and a paradigm shift to performing most revisional surgeries laparoscopically, these procedures still are fraught with high complication and mortality rates [27]. This prompted the development of less invasive endoluminal techniques and devices to achieve further restriction of the pouch and gastric outlet.
In this study, revisional procedures were performed for 24.9% of the patients (n = 51), 41.2% (n = 21) of which were carried out endoscopically. The decision to perform either a surgical or endoluminal revision was based on anatomic endoscopic findings, the ability to perform an endoluminal therapy, and surgeon preference.
The majority of the endoscopic interventions in this series were performed as part of the RESTORe trial, a double-blinded, sham-controlled multicenter study for the treatment of inadequate weight loss or weight regain after RYGB [28]. In the treatment arm of this study, gastric outlet reduction was achieved by endoscopic placement of interrupted sutures at the GJ anastomosis to reduce its diameter to 10 mm or less. From 43 patients recruited into the study arm of the RESTORe trial, 17 had their procedure performed at our institution and therefore were included in this study.
Other endoscopic techniques applied were use of the StomaphyX and EndoCinch devices, both of which have been successful in early series investigating their efficacy for the treatment of weight regain after RYGB [8, 23, 29]. Reasonable success was attained using these novel therapies in our cohort, as reflected by the finding that almost three-fourths of these patients (15/21) lost some or all of their regained weight after endoscopic intervention and by the fact that all cases were managed without complication. Nevertheless, there is potential for improving these techniques to achieve outcomes comparable with those attainable by surgical revision procedures.
In addition to addressing some technical limitations of currently available devices, the durability of endoscopic weight loss therapies remains to be proven. However, to date, this approach has an attractive safety profile and cost benefit, and use of the successful devices currently available has been welcomed by patients and referring physicians alike. With continued developments in endoluminal surgery, we are potentially at the beginning of another major paradigm shift in the treatment of obesity. Until then, conventional surgical approaches to revisional bariatric surgery remain the gold standard.
In this study, 59% of the revision cases were managed using the laparoscopic surgical approach. Placement of an adjustable gastric band around a dilated gastric pouch was the most commonly performed procedure, but in a small number of cases, the GJ was revised. Only two patients had their Roux limb lengthened in addition to revision of the GJ. Our success rate with these traditional surgical approaches was high, with 93% of the patients losing weight postoperatively and an overall mean %RWL exceeding 91%.
As with any revisional bariatric surgery series, the trade-off for such successful weight loss was of course a slightly higher complication rate than observed with primary procedures. We report a morbidity rate of 7.8%, which is at the lower end of the spectrum compared with other revisional surgery series. Even so, patients must be forewarned, and every effort must be made to select revision bariatric candidates carefully to minimize complications.
Although more than 70% of our series would have merited reintervention based on endoscopic evidence of abnormal post-bypass anatomy contributing to weight regain, most medical insurance companies decline to cover such procedures. In our experience, this impediment prevented a significant number of patients from undergoing potentially the most appropriate treatment for their weight regain. This is an issue that needs to be addressed urgently, particularly because the number of primary bariatric procedures performed in the United States is increasing rapidly and the demand for revisional procedures consequently will increase in due course.
Successful outcome in bariatric surgery generally is defined as an initial loss exceeding 50% of excess body weight. A less well-accepted definition, proposed by Reinhold et al. [30], classifies weight loss outcome as excellent if the BMI decreases to less than 30 kg/m2, good if BMI falls within the range 30 to 35 kg/m2, and poor if BMI remains above 35 kg/m2. However, it is suggested that BMI may not be an appropriate unit by which to determine the success of bariatric surgery. For example, substantial weight loss by a super-obese patient (BMI, > 50 kg/m2) is unlikely to fall into the “excellent” category although this weight loss may have induced remission of many obesity-related comorbidities and dramatically improved the patient’s quality of life.
There is no consensus regarding the measurement of success after revisional bariatric surgery. Borao et al. [12] proposed that measuring the amount of regained weight lost again after a revision procedure (%RWL) may be a more reasonable metric for defining success among these patients. Hence, that was the approach used in this study.
The timing of revisional surgery is critical to the achievement of optimal outcomes. We demonstrated that patients with abnormalities of their post-bypass anatomy who are treated within 5 years of their primary RYGB attained the greatest weight loss. Conversely, those who presented as late as 10 years postoperatively had much lower success rates with secondary procedures. The reasons for this disparity in outcomes according to the timing of presentation are unclear. Perhaps chronic distension of the pouch and dilation of the stoma make the tissues noncompliant with attempts at revision. Alternatively, behavioral factors are likely to play a role in long-standing weight regain.
All patients with weight regain or failure of adequate weight loss must be reentered into a multidisciplinary bariatric program for comprehensive preoperative evaluation before they undergo any further intervention. Our data also support offering early intervention to bariatric patients who re-present with weight gain and are found to have an abnormal gastric anatomy.
Despite the positive relationship between increasing pouch/stoma size and weight regain observed in this study and others, some issues remain to be addressed. The definition of pouch and stoma enlargement is inconsistent. The majority of studies, including the current series, use a stoma diameter exceeding 2 cm to define dilation [5, 8], although lesser dimensions have been used, such as a diameter exceeding 1.2 cm in a study by Catalano et al. [19].
Additionally, no standardized technique exists for measuring pouch and stoma sizes. The devices or methods used to estimate these dimensions are likely to differ between units. Among the various methods used to measure the gastric pouch and stoma are endoscopic placement of a gastric balloon, use of a calibrating device, getting patients to eat a known volume of food (e.g., cottage cheese), or measuring dimensions on radiographs [4, 31–33]. Factors that may affect these measurements and thus hinder the reproducibility and reliability of the various techniques include the distensibility and compliance of the pouch as well as observer variability. Ongoing developments in endoscopic technology should aim to address these inconsistencies so that patients presenting with weight regain may be reliably investigated and appropriately selected for revision procedures.
Conclusion
Enlargement of the gastric pouch and the GJ after RYGB is frequently encountered in patients presenting with weight regain. Although suboptimal weight loss after bariatric procedures has a multifactorial etiology, anatomic factors are likely to have an influence on weight regain. In particular, it appears that dilation of the stoma is associated with greatest amount of weight regain. Revision of stoma or pouch size, surgically or endoscopically, can rescue the majority of these patients and reinitiate weight loss. Prompt early intervention may yield the greatest benefit in addition to ongoing appropriate postbariatric surgery follow-up practices.
Endoscopy is an important asset in the bariatric surgeon’s armamentarium. Not only does it have diagnostic utility in the pre- and postoperative setting, but it also is emerging as a novel therapeutic tool for revisional bariatric surgery. For patients presenting with weight regain after gastric bypass, its use is valuable in both settings, as highlighted by the results of this study.
Disclosures
Stacy Brethauer received research support from C. R. Bard, is a speaker for Covidien, and serves as a member of the advisory committee for Ethicon Endosurgery Inc. Philip Schauer is on the scientific advisory board of SurgiQuest, Barosense, and Surgical Excellence. He acts as a consultant for C.R. Bard, Ethicon Endo-surgery Inc., BaxterHealthcare, Stryker, Cardinal Health, and W. L. Gore & Associates Inc. Dr. Schauer also acts in afiduciary capacity for the MISS Surgery Symposium, Physician Reviews of Surgery, and RemedyMD. Matthew Kroh is a consultant for C.R. Bard, Covidien, and Ethicon Endo-Surgery, Inc. Bipan Chand is a research investigator for C.R. Bard and a speaker for Aventis Inc. andEthicon Endo-Surgery, Inc. Panot Yimcharoen, Helen M Heneghan, Manish Singh, and Tomasz Rogula have no conflicts of interest or financial ties to disclose.
References
Christou NV, Look D, Maclean LD (2006) Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg 244:734–740
Magro DO, Geloneze B, Delfini R, Pareja BC, Callejas F, Pareja JC (2008) Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg 18:648–651
Meguid MM, Glade MJ, Middleton FA (2008) Weight regain after Roux-en-Y: a significant 20% complication related to PYY. Nutrition 24:832–842
Flanagan L (1996) Measurement of functional pouch volume following the gastric bypass procedure. Obes Surg 6:38–43
Herron DM, Birkett DH, Thompson CC, Bessler M, Swanstrom LL (2008) Gastric bypass pouch and stoma reduction using a transoral endoscopic anchor placement system: a feasibility study. Surg Endosc 22:1093–1099
Muller MK, Wildi S, Scholz T, Clavien PA, Weber M (2005) Laparoscopic pouch resizing and redo of gastrojejunal anastomosis for pouch dilatation following gastric bypass. Obes Surg 15:1089–1095
Schwartz RW, Strodel WE, Simpson WS, Griffen WO Jr (1988) Gastric bypass revision: lessons learned from 920 cases. Surgery 104:806–812
Thompson CC, Slattery J, Bundga ME, Lautz DB (2006) Peroral endoscopic reduction of dilated gastrojejunal anastomosis after Roux-en-Y gastric bypass: a possible new option for patients with weight regain. Surg Endosc 20:1744–1748
Bessler M, Daud A, DiGiorgi MF, Olivero-Rivera L, Davis D (2005) Adjustable gastric banding as a revisional bariatric procedure after failed gastric bypass. Obes Surg 15:1443–1448
Brethauer SA, Pryor AD, Chand B, Schauer P, Rosenthal R, Richards W, Bessler M (2009) Endoluminal procedures for bariatric patients: expectations among bariatric surgeons. Surg Obes Relat Dis 5:231–236
Ellsmere JC, Thompson CC, Brugge WR, Chuttani R, Desilets DJ, Rattner DW, Tarnoff EM, Kaplan LM (2009) Endoscopic interventions for weight loss surgery. Obes Silver Spring 17:929–933
Borao F, Gorcey S, Capuano A (2010) Prospective single-site case series utilizing an endolumenal tissue anchoring system for revision of post-RYGB stomal and pouch dilatation. Surg Endosc 24:2308–2313
Brethauer SA, Nfonsam V, Sherman V, Udomsawaengsup S, Schauer PR, Chand B (2006) Endoscopy and upper gastrointestinal contrast studies are complementary in evaluation of weight regain after bariatric surgery. Surg Obes Relat Dis 2:643–648 (discussion 649–650)
Brolin RE (2002) Bariatric surgery and long-term control of morbid obesity. JAMA 288:2793–2796
Tice JA, Karliner L, Walsh J, Petersen AJ, Feldman MD (2008) Gastric banding or bypass? A systematic review comparing the two most popular bariatric procedures. Am J Med 121:885–893
Lim CS, Liew V, Talbot ML, Jorgensen JO, Loi KW (2009) Revisional bariatric surgery. Obes Surg 19:827–832
Fobi MA (2004) Surgical treatment of obesity: a review. J Natl Med Assoc 96:61–75
Powers MA, Pappas TN (1989) Physiologic approaches to the control of obesity. Ann Surg 209:255–260
Catalano MF, Rudic G, Anderson AJ, Chua TY (2007) Weight gain after bariatric surgery as a result of a large gastric stoma: endotherapy with sodium morrhuate may prevent the need for surgical revision. Gastrointest Endosc 66:240–245
Ryou M, Mullady DK, Lautz DB, Thompson CC (2009) Pilot study evaluating technical feasibility and early outcomes of second-generation endosurgical platform for treatment of weight regain after gastric bypass surgery. Surg Obes Relat Dis 5:450–454
Spaulding L, Osler T, Patlak J (2007) Long-term results of sclerotherapy for dilated gastrojejunostomy after gastric bypass. Surg Obes Relat Dis 3:623–626
Carpenter RO, Williams DB, Richards WO (2010) Laparoscopic adjustable gastric banding after previous Roux-en-Y gastric bypass. Surg Obes Relat Dis 6:93–95
Mikami D, Needleman B, Narula V, Durant J, Melvin WS (2010) Natural orifice surgery: initial U.S. experience utilizing the StomaphyX device to reduce gastric pouches after Roux-en-Y gastric bypass. Surg Endosc 24:223–228
Morales MP, Wheeler AA, Ramaswamy A, Scott JS, de la Torre RA (2010) Laparoscopic revisional surgery after Roux-en-Y gastric bypass and sleeve gastrectomy. Surg Obes Relat Dis 6:485–490
Valezi AC, Mali Junior J, de Menezes MA, de Brito EM, de Souza SA (2010) Weight loss outcome after silastic ring Roux-en-Y gastric bypass: 8 years of follow-up. Obes Surg 20:1491–1495
Schauer P, Chand B, Brethauer S (2007) New applications for endoscopy: the emerging field of endoluminal and transgastric bariatric surgery. Surg Endosc 21:347–356
Spyropoulos C, Kehagias I, Panagiotopoulos S, Mead N, Kalfarentzos F (2010) Revisional bariatric surgery: 13-year experience from a tertiary institution. Arch Surg 145:173–177
Thompson CC, Roslin MS, Chand B, Chen YK, de Marco DC, Miller LS, Schweitzer M, Rothstein RL, Lautz DB, Ryan MB, Brethauer SA, Schauer PR, Mitchell MC, Starpoli AA, Haber GB, Catalano MF, Edmundowicz SA, Fagnant A, Kaplan LM (2010) RESTORe: randomized evaluation of endoscopic suturing transorally for anastomotic outlet reduction: a double-blinded, sham-controlled multicenter study for treatment of inadequate weight loss or weight regain following Roux-en-Y gastric bypass. Gastroenterology (2010 DDW Abstract Suppl) 138:S-388
Fogel R, De Fogel J, Bonilla Y, De La Fuente R (2008) Clinical experience of transoral suturing for an endoluminal vertical gastroplasty: 1-year follow-up in 64 patients. Gastrointest Endosc 68:51–58
Reinhold RB (1982) Critical analysis of long-term weight loss following gastric bypass. Surg Gynecol Obstet 155:385–394
Fried M, Peskova M (1996) Does laparoscopic gastric banding demand sophisticated measurement devices? Obes Surg 6:336–340
Nishie A, Brown B, Barloon T, Kuehn D, Samuel I (2007) Comparison of size of proximal gastric pouch and short-term weight loss following routine upper gastrointestinal contrast study after laparoscopic Roux-en-Y gastric bypass. Obes Surg 17:1183–1188
Roberts K, Duffy A, Kaufman J, Burrell M, Dziura J, Bell R (2007) Size matters: gastric pouch size correlates with weight loss after laparoscopic Roux-en-Y gastric bypass. Surg Endosc 21:1397–1402
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yimcharoen, P., Heneghan, H.M., Singh, M. et al. Endoscopic findings and outcomes of revisional procedures for patients with weight recidivism after gastric bypass. Surg Endosc 25, 3345–3352 (2011). https://doi.org/10.1007/s00464-011-1723-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1723-0