Abstract
Background
There are no clear psychosocial predictors of weight loss following bariatric surgery. The purpose of this study was to investigate whether preoperative problematic eating behaviors predict weight loss outcomes following bariatric surgery.
Methods
Clinical records were utilized to examine outcomes of 101 patients who completed a pre-surgical psychosocial evaluation and underwent gastric bypass or sleeve gastrectomy. Information analyzed included binge eating history and scores from the Hospital Anxiety and Depression Scale, Yale Food Addiction Scale, and Emotional Eating Scale. Measures of weight loss 1 year post-surgery were compared to pre-surgical assessments.
Results
One-year follow-up data were available for 60 patients. Patients with higher levels of eating in response to anger/frustration (p = .02), anxiety (p = .01), or depression (p = .05) were more likely to miss the 1-year follow-up appointment. Eating in response to anger/frustration and depression were related to poorer weight loss outcomes. There was a trend for binge eating to predict greater %EWL (p = .06). A higher number of food addiction symptoms increased the likelihood that patients would experience less weight loss (p = .01). Psychiatric symptoms were not related to weight loss outcomes.
Conclusions
Patients who endorsed higher levels of pre-surgical emotional eating and food addiction symptoms had poorer weight loss 1 year post-surgery. Providers should consider screening patients for these behaviors during the pre-surgical psychosocial evaluation which would allow opportunities for psychotherapy and potential improvement in weight loss outcomes. Future research should examine which interventions are successful at improving problematic eating behaviors.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Research has examined potential pre-surgical psychosocial predictors of weight loss following bariatric surgery; however, findings are mixed. Because there are not reliable predictors of weight loss post-surgery, it is difficult for providers to determine how to conduct a psychosocial evaluation prior to bariatric surgery [1, 2]. Some studies have found a negative association between pre-surgical psychiatric disorders (i.e., depression, personality disorders, and substance use disorders) and post-surgical weight loss outcomes [3, 4]. Other work has found a positive relationship between psychiatric co-morbidity and weight loss after surgery [5], suggesting that increased stress (including symptoms of anxiety and depression) pertaining to concerns with weight prior to surgery could be positive predictors of post-surgical weight loss [6,7,8]. Perhaps, the reason for these inconsistent findings is that there are other variables, such as problematic eating behaviors, that are associated with psychiatric symptoms that impact weight loss outcomes [9]. There are recently published guidelines on what should be evaluated in this pre-surgical evaluation, including psychiatric symptoms and problematic eating behaviors such as binge eating and night eating [2]. However, there is a lack of data to guide the evaluation with regard to emotional eating and food addiction symptoms.
The influence of pre-surgical problematic eating behaviors, especially binge eating, on post-surgical outcomes has been increasingly explored. Although binge and hyper-caloric eating have been associated with less post-surgical weight loss [7, 10], other studies have not found these poorer outcomes for patients who engaged in binge eating prior to surgery [3, 11]. One reason for this variability could be because of how binge eating is measured. Recent research found that those who met criteria for a binge eating diagnosis had higher BMIs at a long-term follow-up [12]. Another recent study found that those who experience a loss of control when eating had poorer dietary adherence, suggesting that there are factors associated with binge eating that could be causing poorer outcomes rather than the binge eating behavior itself [13].
Problematic eating behaviors other than binge eating have not been as closely considered, such as food addiction and emotional eating. Food addiction is the idea that people can become addicted to certain types of foods (i.e., sweets, fats, carbohydrates, salt) in a similar manner as other substance use addictions [14]. While the concept of food addiction remains somewhat controversial, there is increasing attention to this clinical construct as it presents in weight management populations, including individuals pursuing bariatric surgery. Original criteria for “food addiction” were the same as those for other substance use addictions in the DSM-IV-TR. Criteria were met if an individual endorsed clinically significant distress or problems in daily function related to eating and at least three of seven associated symptoms: tolerance, withdrawal, loss of control, a desire or repeated failed attempts to cut down, a great deal of time spent in obtaining, using, or recovering from food, giving up other important activities, and/or continued use despite physical or psychological consequences [15]. Based on these criteria, prevalence rates of food addiction in populations pursuing nonsurgical weight loss treatment range from 7 to 25% [16, 17]. There appears to be even greater prevalence of food addiction found among bariatric surgical candidates, with rates ranging from 14 to 58% [9, 18, 19]. Individuals engaging in emotional eating are identified as eating in response to negative emotions, such as anxiety, anger/frustration, and depression [20], with prevalence rates ranging from 25 to 41% in candidates for bariatric surgery [9]. Positive relationships exist between the severity of psychiatric symptoms and emotional eating and food addiction [9, 21,22,23].
Emotional eating and food addiction are common among patients pursuing bariatric surgery, yet it is unclear how they may affect post-surgical outcomes. In one study with a small sample size, emotional eating among bariatric patients was related to inferior weight loss [6]; however, other studies did not find this relationship [3, 24]. The effect of food addiction on weight loss outcomes post-surgery is also unclear [18, 19]. One problem with the current studies is that short follow-up time periods have been used (i.e., 6–8 months). While pre-surgical problematic eating behaviors may not impact short-term weight loss outcomes, there may be more of an impact on longer term weight loss or successful weight maintenance as problematic eating behaviors resurface.
The purpose of this study was to investigate whether pre-surgical psychiatric symptoms and problematic eating behaviors are predictors of weight loss outcomes 1 year after gastric bypass or sleeve gastrectomy.
Methods
Participants
Chart reviews were conducted on 146 consecutive patients who completed a required pre-surgical psychosocial evaluation prior to bariatric surgery between October 2012 and January 2013.
Measures
Binge Eating
Binge eating was assessed in a semi-structured interview. A patient was categorized as having binge eating behaviors if he/she endorsed currently experiencing (e.g., past 6 months) criteria based on the DSM-IV-TR: (1) eating a larger amount of food over a short duration than most would in a similar circumstance and (2) experienced a lack of control over eating during the episode.
Emotional Eating Scale
The Emotional Eating Scale (EES) measures three types of emotional eating (anger/frustration, anxiety, and depression) on a Likert scale ranging from “No Desire to Eat” to “An Overwhelming Urge to Eat” [25]. Higher scores indicate higher levels of emotional eating. A principal component analysis revealed three separate factors, with adequate internal consistency for each of the factors of anger/frustration, anxiety, and depression as well as the total score (e.g., .78, .78, .72, and .81, respectively) [25].
Yale Food Addiction Scale
The Yale Food Addiction Scale (YFAS) is a 27-item measure that assesses the seven symptoms of food addiction which are the same symptoms as those for other substance use addictions in the DSM-IV-TR [15]. The score for number of symptoms a patient can have ranges from 0 to 7. This measure has been validated with a bariatric surgery population [26].
Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS) assesses severity of anxiety (HADS-A; 7 items) and depression symptoms (HADS-D; 7 items) [27]. Patients respond to the degree they have experienced symptoms over the past week. Scores increase with level of severity and are interpreted as normal (0–7), mild (8–10), moderate (11–14), or severe (15–21).
Weight Loss Outcomes
Patients’ charts were reviewed to record their initial height, weight, and BMI at the surgeon consultation appointment. The type of surgery the patient underwent (e.g., adjustable gastric banding, Roux-en-Y gastric bypass, or gastric sleeve) was recorded. Whether they completed their 1-year follow-up appointment with the surgeon was also recorded along with their weight and BMI at that appointment. Adhering to the standardized outcomes to report, the change in BMI (ΔBMI), percent of total weight loss (%TWL), and percent of excess weight loss (%EWL) was calculated for each patient based on their weight at the 1-year follow-up [28]. Whether a patient experienced a lack of additional weight loss was also recorded. A patient was identified as lacking additional weight loss if they did not lose at least an additional 5% of their total weight at the 1-year appointment as compared with the previous appointment with the surgical team (3 months post-surgery), unless they were already below a BMI of 30.
Procedure
This study was approved by the hospital’s Institutional Review Board. Statistical analyses were conducted with SPSS version 23. Prevalence rates were calculated for patient demographics. Chi-square analyses and independent sample t tests were conducted to determine whether there were differences in problematic eating behaviors among those who did and did not have bariatric surgery. Correlations were calculated to determine the relationships among problematic eating behaviors, psychiatric symptoms, and weight loss outcomes among those who had bariatric surgery. Independent sample t tests were conducted to determine whether problematic eating behaviors were related to missing the 1-year follow-up appointment and whether patients experienced a lack of additional weight loss. Cohen’s d values were calculated to report effect sizes. Analyses were considered statistically significant if p < .05.
Results
Patient Demographics
Of those completing the psychosocial evaluation, 74% (n = 108) underwent bariatric surgery. Seven of these patients underwent adjustable gastric banding and given the small sample size and the different expected weight loss outcomes with this procedure, these patients were excluded from further analyses. There was no difference in problematic eating behaviors between those who did and did not have bariatric surgery. There was no statistically significant difference in weight loss outcomes between those who underwent Roux-en-Y gastric bypass and sleeve gastrectomy. There were also no differences between surgery type for food addiction symptoms, emotional eating, depression, anxiety, binge eating, and whether a patient missed the 1-year follow-up appointment. See Table 1 for the demographics of the patients who had bariatric surgery. Most patients were White females with a mean age of 46 ± 11.8 and initial BMI of 49.3 ± 8 kg/m2.
Problematic Eating Behaviors and Psychiatric Symptoms
There were significant, positive relationships among all types of emotional eating, the number of food addiction symptoms endorsed, and depressive and anxiety symptoms (Table 2). A history of binge eating was not related to emotional eating or psychiatric symptoms, but there was a trend for binge eating to be related to a higher number of food addiction symptoms (t = − 1.91, p = .06, Cohen’s d = .43).
Predictors of Weight Loss Outcomes
Problematic eating behaviors were related to whether a patient attended their 1-year surgical follow-up appointment. There were 41 patients (40.6%) who did not attend the 1-year appointment. Patients with higher levels of eating in response to anger/frustration (t = 2.33, p = .02, Cohen’s d = .50) and anxiety (t = 2.64, p = .01, Cohen’s d = .55) were more likely to miss their 1-year follow-up appointment. There was a trend for eating in response to depression and missing the 1-year follow-up appointment (t = 1.97, p = .05, Cohen’s d = .43).
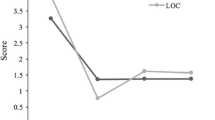
Weight loss outcomes were available for 60 patients (59.4%) at the 1-year follow-up appointment. Several significant findings emerged when analyzing the relationship of pre-surgical symptoms to weight loss outcomes at the 1-year post-surgical follow-up. Patients who endorsed higher levels of emotional eating, specifically eating in response to anger/frustration and depression, had a lower %TWL and %EWL (Table 2). Those who endorsed higher levels of eating in response to anger/frustration also had a lower ΔBMI at 1 year (Table 2). Although not statistically significant, there was a trend for binge eating predicting %EWL (t = −2.01, p = .06, Cohen’s d = .46). Specifically, those that were engaging in current binge eating behaviors at the pre-surgical evaluation had a higher %EWL 1 year post-surgery (57.1 ± 6.7) compared to those that did not endorse current binge eating at the pre-surgical evaluation (49.6 ± 22.1). Depressive and anxiety symptoms were not related to ΔBMI, %TWL, or %EWL (Table 2).
Finally, the number of food addiction symptoms was related to a lack of additional weight loss between 3 months and 1 year after surgery (t = 2.28; p = .03, Cohen’s d = .67). Those that did not lose additional weight (n = 21) endorsed a higher number of pre-surgical food addiction symptoms (2.8 ± 1.7) than those that continued to lose weight 1 year post-surgery (1.86 ± 1.0).
Discussion
We found that patients who endorsed higher levels of pre-surgical emotional eating and food addiction symptoms had poorer weight loss 1 year following gastric bypass or sleeve gastrectomy. The main preoperative emotional eating behaviors that were associated with poorer weight loss 1 year following surgery were eating in response to anger/frustration or eating in response to depression. Furthermore, patients who experienced a stall in weight loss between 3 and 12 months after surgery endorsed a higher number of pre-surgical food addiction symptoms.
The impact of problematic eating behaviors on post-surgical outcomes, such as a pre-surgical binge eating disorder [29,30,31] or loss of control over eating [11] have been investigated in the past with mixed results. It has been suggested in these studies that reverting back to problematic eating behaviors after surgery will likely lead to limited weight loss and/or weight regain. Perhaps this is better understood by exploring factors which may underlie these problematic behaviors, such as emotional eating and food addiction, as was investigated in this study. Unexpectedly, those that were engaging in binge eating behaviors at the pre-surgical psychosocial evaluation trended towards a higher %EWL. This could be because our center routinely refers patients with current binge eating behaviors for treatment so that patients can gain coping skills to reduce this behavior. The treatment of patients with binge eating behaviors in our center could partially explain these unexpected results. Alternatively, it is possible that those who engaged in binge eating behaviors prior to surgery were unable to re-engage in this behavior in the first year after surgery due to the restriction. A longer term follow-up suggests that pre-surgical binge eating is associated with poorer outcomes 5 years after surgery [12]. It is likely important to identify whether patients experience post-surgical binge eating behaviors as these behaviors can resurface [32]. Additionally, it may be easier for patients to continue food addiction and emotional eating behaviors in the year following surgery because foods can be eaten in problematic ways in smaller portions.
Unfortunately, many patients are lost to follow-up after bariatric surgery [33] and those with a lower %EWL at 1 year are less likely to follow-up [34]. In the current study, those who endorsed higher levels of emotional eating were less likely to follow-up a year after surgery than those who reported less frequent emotional eating. It is possible that factors such as emotional eating contribute to lack of weight loss post-surgery, which in turn leads to poor follow-up with the surgical team. Patients may feel embarrassed by a perceived lack of success and ongoing problematic eating behaviors and choose not to follow-up. Consistent with previous findings [7], there was no relationship between symptoms of depression and anxiety and weight loss post-bariatric surgery, yet these psychiatric symptoms were related to emotional eating and food addiction symptoms. This suggests the importance of investigating other factors that may be contributing to poor outcomes.
There are several limitations with this study. First, due to the correlational methodology of the study, it is not certain that these problematic eating behaviors are the direct cause of poorer weight loss post-surgery. Additionally, the sample size is relatively small. Because providers inconsistently documented the frequency of binge eating behaviors, we were unable to compare this to weight loss outcomes. Future research could also evaluate whether the frequency of pre-surgical binge eating impacts weight loss post-surgery. Finally, it would be useful to have longer term follow-up given that many patients may still be losing weight at the 1 year mark and problematic eating behaviors could still resurface. Future investigation could evaluate whether these outcomes are similar for larger sample sizes and at longer follow-up periods.
There are important implications for clinical practice based on these findings. Providers conducting psychiatric evaluations should consider routine screening for emotional eating and food addiction during their pre-surgical evaluation. If patients with these behaviors are identified prior to bariatric surgery, they can be referred for treatment to help improve these behaviors. Treatments that may be successful at reducing problematic eating behaviors include cognitive behavioral therapy [35]; mindfulness [36], and psychoeducation offered in the group therapy context [37]. Additionally, if patients are struggling to lose weight post-surgery, it may be useful to evaluate patients for problematic eating behaviors at this stage as well. Future research should examine which interventions are successful at improving problematic eating behaviors and whether treatment results in better weight loss outcomes. Finally, patients who undergo gastric bypass may experience different eating challenges post-surgery than those with sleeve gastrectomy. Therefore, future research could assess problematic eating behaviors after bariatric surgery and how these impact long-term weight loss outcomes.
References
Ashton D, Favretti F, Segato G. Preoperative psychological testing—another form of prejudice. Obes Surg. 2008;18(10):1330–7. https://doi.org/10.1007/s11695-008-9469-z.
Sogg S, Lauretti J, West-Smith L. Recommendations for the presurgical psychosocial evaluation of bariatric surgery patients. Surg Obes Relat Dis. 2016;12(4):731–49. https://doi.org/10.1016/j.soard.2016.02.008.
Kinzl JF, Schrattenecker M, Traweger C, et al. Psychosocial predictors of weight loss after bariatric surgery. Obes Surg. 2006;16(12):1609–14. https://doi.org/10.1381/096089206779319301.
Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012 Jan;22(1):70–89. PubMed Epub 2011/08/13. eng. https://doi.org/10.1007/s11695-011-0472-4.
Clark MM, Balsiger BM, Sletten CD, et al. Psychosocial factors and 2-year outcome following bariatric surgery for weight loss. Obes Surg. 2003 Oct;13(5):739–45. PubMed Epub 2003/11/25. eng. https://doi.org/10.1381/096089203322509318.
Canetti L, Berry EM, Elizur Y. Psychosocial predictors of weight loss and psychological adjustment following bariatric surgery and a weight-loss program: the mediating role of emotional eating. Int J Eating Disord. 2009 Mar;42(2):109–17. PubMed Epub 2008/10/25. eng. https://doi.org/10.1002/eat.20592.
Herpertz S, Kielmann R, Wolf AM, et al. Do psychosocial variables predict weight loss or mental health after obesity surgery? A systematic review. Obes Res. 2004 Oct;12(10):1554–69. PubMed Epub 2004/11/13. eng. https://doi.org/10.1038/oby.2004.195.
Ray EC, Nickels MW, Sayeed S, Sax HC. Predicting success after gastric bypass: the role of psychosocial and behavioral factors. Surgery 2003 Oct;134(4):555–563; discussion 63-4. PubMed Epub 2003/11/08. eng, DOI: https://doi.org/10.1016/S0039-6060(03)00279-4.
Miller-Matero LR, Armstrong R, McCulloch K, et al. To eat or not to eat; is that really the question? An evaluation of problematic eating behaviors and mental health among bariatric surgery candidates. Eating Weight Disord-Studies Anorexia, Bulimia Obes. 2014;19(3):377–82. https://doi.org/10.1007/s40519-014-0118-3.
Sysko R, Devlin MJ, Hildebrandt TB, et al. Psychological outcomes and predictors of initial weight loss outcomes among severely obese adolescents receiving laparoscopic adjustable gastric banding. J Clin Psychiatr. 2012;73(10):1351–7. https://doi.org/10.4088/JCP.12m07690.
White MA, Kalarchian MA, Masheb RM, et al. Loss of control over eating predicts outcomes in bariatric surgery patients: a prospective, 24-month follow-up study. J Clin Psychiatry. 2010 Feb;71(2):175–84. https://doi.org/10.4088/JCP.08m04328blu.
Marek RJ, Ben-Porath YS, van Dulmen MH, et al. Using the presurgical psychological evaluation to predict 5-year weight loss outcomes in bariatric surgery patients. Surg Obes Relat Dis. 2017;13(3):514–21. https://doi.org/10.1016/j.soard.2016.11.008.
Adler S, Fowler N, Robinson AH, et al. Correlates of dietary adherence and maladaptive eating patterns following Roux-en-Y bariatric surgery. Obes Surg. 2017:1–6.
Ifland J, Preuss H, Marcus M, et al. Refined food addiction: a classic substance use disorder. Med Hypotheses. 2009;72(5):518–26. https://doi.org/10.1016/j.mehy.2008.11.035.
Gearhardt AN, Corbin WR, Brownell KD. Food addiction: an examination of the diagnostic criteria for dependence. J Addict Med. 2009;3(1):1–7. https://doi.org/10.1097/ADM.0b013e318193c993.
Chao AM, Shaw JA, Pearl RL, et al. Prevalence and psychosocial correlates of food addiction in persons with obesity seeking weight reduction. Compr Psychiatry. 2017;73:97–104. https://doi.org/10.1016/j.comppsych.2016.11.009.
Meule A. How prevalent is “food addiction”? Frontiers in psychiatry. 2011;2
Koball AM, Clark MM, Collazo-Clavell M, et al. The relationship among food addiction, negative mood, and eating-disordered behaviors in patients seeking to have bariatric surgery. Surg Obes Relat Dis. 2016;12(1):165–70. https://doi.org/10.1016/j.soard.2015.04.009.
Sevinçer GM, Konuk N, Bozkurt S, et al. Food addiction and the outcome of bariatric surgery at 1-year: prospective observational study. Psychiatry Res. 2016;244:159–64. https://doi.org/10.1016/j.psychres.2016.07.022.
Fischer S, Chen E, Katterman S, et al. Emotional eating in a morbidly obese bariatric surgery-seeking population. Obes Surg. 2007;17(6):778–84. https://doi.org/10.1007/s11695-007-9143-x.
Meule A, Heckel D, Jurowich C, et al. Correlates of food addiction in obese individuals seeking bariatric surgery. Clin Obes. 2014;4(4):228–36.
Brunault P, Ducluzeau P-H, Bourbao-Tournois C, et al. Food addiction in bariatric surgery candidates: prevalence and risk factors. Obes Surg. 2016;26(7):1650–3. https://doi.org/10.1007/s11695-016-2189-x.
Sevinçer GM, Konuk N, İpekçioğlu D, et al. Association between depression and eating behaviors among bariatric surgery candidates in a Turkish sample. Eating Weight Disord-Stud Anorexia, Bulimia Obes. 2017;22(1):117–23. https://doi.org/10.1007/s40519-016-0296-2.
Wedin S, Madan A, Correll J, et al. Emotional eating, marital status and history of physical abuse predict 2-year weight loss in weight loss surgery patients. Eat Behav. 2014 Dec;15(4):619–24. PubMed Epub 2014/09/23. eng. https://doi.org/10.1016/j.eatbeh.2014.08.019.
Arnow B, Kenardy J, Agras WS. The Emotional Eating Scale: the development of a measure to assess coping with negative affect by eating. Int J Eat Disord 1995;18(1):79–90.
Clark SM, Saules KK. Validation of the Yale Food Addiction Scale among a weight-loss surgery population. Eat Behav. 2013;14(2):216–9.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
Brethauer SA, Kim J, El Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606. https://doi.org/10.1007/s11695-015-1645-3.
de Zwaan M, Lancaster KL, Mitchell JE, et al. Health-related quality of life in morbidly obese patients: effect of gastric bypass surgery. Obes Surg. 2002;12(6):773–80. https://doi.org/10.1381/096089202320995547.
Pekkarinen T, Koskela K, Huikuri K, et al. Long-term results of gastroplasty for morbid obesity: binge-eating as a predictor of poor outcome. Obes Surg. 1994;4(3):248–55. https://doi.org/10.1381/096089294765558467.
Latner JD, Wetzler S, Goodman ER, et al. Gastric bypass in a low-income, inner-city population: eating disturbances and weight loss. Obesity. 2004;12(6):956–61. https://doi.org/10.1038/oby.2004.117.
Sheets CS, Peat CM, Berg KC, et al. Post-operative psychosocial predictors of outcome in bariatric surgery. Obes Surg. 2015;25(2):330–45. https://doi.org/10.1007/s11695-014-1490-9.
Ma Y, Pagoto SL, Olendzki BC, et al. Predictors of weight status following laparoscopic gastric bypass. Obes Surg. 2006;16(9):1227–31. https://doi.org/10.1381/096089206778392284.
Harper J, Madan AK, Ternovits CA, et al. What happens to patients who do not follow-up after bariatric surgery? Am Surg. 2007;73(2):181–4.
Beck JS. The Beck diet solution: train your brain to think like a thin person: Hachette UK; 2012.
Daubenmier J, Kristeller J, Hecht FM, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: an exploratory randomized controlled study. J Obes. 2011;2011:1–13. https://doi.org/10.1155/2011/651936.
Hilker I, Sánchez I, Steward T, et al. Food addiction in bulimia nervosa: clinical correlates and association with response to a brief psychoeducational intervention. Eur Eat Disord Rev. 2016;24(6):482–8. https://doi.org/10.1002/erv.2473.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was waived by the IRB due to the retrospective methodology.
This study has been approved by the institution’s research ethics committee and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Miller-Matero, L.R., Bryce, K., Saulino, C.K. et al. Problematic Eating Behaviors Predict Outcomes After Bariatric Surgery. OBES SURG 28, 1910–1915 (2018). https://doi.org/10.1007/s11695-018-3124-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3124-0