Abstract
Background
Problematic eating behaviors and general psychopathology have been associated with poor weight loss after bariatric surgery. However, little is known about how these aspects impact weight loss outcomes for the increasing number of patients undergoing reoperative surgeries. This study compares disordered eating and weight-related outcomes before and 6 months after surgery in patients undergoing primary (P-Group) and reoperative bariatric surgery (R-Group).
Methods
This longitudinal study assessed 122 P-Group and 116 R-Group patients before and 6 months after surgery. The assessment included the eating disorder examination diagnostic items, and a set of self-report measures assessing eating disorder symptomatology, grazing, depression, anxiety, and negative urgency.
Results
Preoperatively, no differences were found between the R- and P-Groups in terms of disordered eating-related variables (except for shape concern, which was higher for the R-Group). At 6 months after surgery, the R-Group revealed significantly higher values for restraint (F(1,219) = 5.84, p = 0.016), shape (F(1,219) = 5.59, p = 0.019), weight concerns (F(1,219) = 13.36, p = 0.000), depression (F(1,219) = 7.17, p = 0.008), anxiety (F(1,219) = 6.94, p = − 0.009), and compulsive grazing (F(1,219) = 6.13, p = 0.014). No significant pre- or post-surgery predictors of weight loss were found for the P-Group (χ2 = 0.70, p = 0.872). In the R-Group, post-surgery anxiety (Waldχ2(1) = 6.19, p = 0.01) and the post-surgery number of days with grazing in the previous month (Waldχ2(1) = 3.90, p = 0.04) were significant predictors of weight loss.
Conclusion
At 6 months after surgery, the R-Group presented more problematic eating and general psychological distress, which may put these patients at greater risk of poorer long-term weight outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has been considered the most effective treatment for severe obesity, long-term weight loss, and resolution of medical comorbidities [1,2,3]. However, there is considerable variability in weight outcomes, with some patients failing to achieve a significant amount of weight loss [4], and others experiencing weight regain after initially successful weight results [3, 5,6,7,8]. Secondary surgeries have been performed in patients experiencing poor outcomes and/or complications in their first procedure. The need to resort to reoperative bariatric surgeries has been increasing exponentially worldwide over the recent years [9, 10]. The current global incidence of reoperations is estimated to vary from 5 to 50% [11,12,13]. Some studies found different reoperation rates according to the procedure, suggesting that restrictive procedures, such as gastric banding, present a high reoperation rate of approximately 30.29% [14] compared to 0.92% for gastric bypass [14], and 6.8% for gastric sleeve [15].
The literature has shown that great variability in weight outcomes is also observed in patients undergoing reoperative surgery. Some studies show inferior weight loss in secondary surgery [16,17,18], while others report similar weight loss in primary and reoperative surgeries [19,20,21]. As in primary surgeries, most of the weight is lost within the first 12 months after reoperation [16, 22, 23]. Despite inducing significant weight loss [24], it is estimated that 8.8% of patients will require a third surgery [25].
However, there is little knowledge regarding the factors that may impact the results of these reoperative bariatric surgeries. Research has shown that psychological and behavioral aspects influence weight loss results after primary surgeries, which may also be expected after secondary surgeries. Several studies report that the post-surgery presence of binge eating or other dysfunctional eating problems, such as loss of control, uncontrolled eating, or graze eating, is associated with less weight loss and weight regain [6, 26,27,28]. Moreover, it is known that a significant percentage of candidates for a second surgery (42.8%) experience poor weight outcomes in their first surgery due to problematic behavioral aspects [29].
In addition to eating behaviors, a number of studies suggest that pre-surgical anxiety and depression result in less weight loss in the short term after surgery [30,31,32]. Nevertheless, mixed findings have been published, as other authors have found no association between mood disorders at baseline and weight loss 1 year after surgery [29, 33]. Other studies showed that high impulsivity levels are associated with problematic eating behaviors [34, 35] and contribute to the reduced success of bariatric surgery. Schag and colleagues [36] found that impulsivity is associated with problematic eating behaviors and that this association is mediated by depression, suggesting that a high score in impulsivity associated with high depressive symptoms results in problematic eating behaviors and, consequently, poor weight loss.
Despite the link between psychological/behavioral factors and weight loss or weight regain after bariatric surgery [37,38,39], little is known about whether patients who undergo a second surgical procedure after poor primary outcomes represent a risk group requiring specific clinical attention. Thus far, only Kafri and colleagues [18] compared psychobehavioral outcomes of reoperative and primary surgery patients 18 months after surgery. Their findings suggest that the reoperative group reported more nonnormative eating patterns and vomiting, lower rates of physical activity, lower levels of healthy eating, less weight loss, and higher levels of psychological distress than the primary group. However, the data are limited to this study, and further research is needed to investigate the psychological and behavioral factors that may compromise the outcomes of the reoperative surgery group [24].
This study aims to compare behavioral and weight outcomes, including eating behaviors and related psychological characteristics, before and 6 months after surgery in patients undergoing primary (P-Group) and reoperative (R-Group) surgeries. Short-term (6 months postoperatively) psychobehavioral predictors of weight loss were also investigated for both the P- and R-Groups.
Materials and Methods
Procedure
This study is part of a larger longitudinal study that was conducted at a central hospital in the north of Portugal and that assessed consecutive patients undergoing primary and reoperative bariatric surgery at baseline and at different points in time (6, 12, 18, and 24 months) following surgery. All patients admitted to bariatric surgery from April 2014 to April 2017 were considered eligible for the larger study. The preoperative characterization of these patients is published elsewhere [40]. For the purpose of this study, only data from patients who completed both the preoperative and 6-month follow-up assessments at the time of this manuscript’s preparation were included.
Baseline assessment was completed the day before surgery, and the 6-months follow-up assessment was conducted after the medical appointments at the hospital. The exclusion criteria included pregnancy after surgery, severe cognitive compromise that limited the autonomy of the patient, acute presentation of psychiatric conditions with severe impairment of global functioning (assessed by the accompanying psychiatrist), not being able to understand written and spoken Portuguese, and use of a ketogenic or liquid diet during the months before surgery. In this clinical center, patients were not required to undergo any specific diet or eating plan before surgery, except for very specific cases in which the patient was on a ketogenic diet.
The study protocol was approved by the ethical review committees of the university and hospital involved. All the participants signed an informed consent form and were informed about the aims of the study and the voluntary nature of their participation.
Participants
In total, 395 patients undergoing bariatric surgery were eligible for the larger longitudinal study and four patients chose not to participate. The baseline assessment included 225 patients undergoing primary surgery and 166 undergoing reoperative surgery. Of these patients, only 122 primary surgery and 116 reoperative patients completed the 6-month follow-up. Patients lost to follow-up included no-shows to the appointments with the multidisciplinary team at 6 months (n = 28), patients who refused to participate in the secondary assessment (n = 12), patients transferred to a different hospital (n = 2), patients with delays in previous medical appointments resulting in conflicting schedules with the research interviews (n = 49), patients who were diagnosed with cancer (n = 2), and a patient who was pregnant (n = 1). Fifty-four participants had not completed the 6-month follow-up by the time of the preparation of the manuscript. Considering the low proportion of reoperative patients who had undergone gastric sleeve 5 (2.06%) as their first surgery, it was decided that these patients would not be included in this study. All other patients received an adjustable gastric band as their first surgery.
Measures
Clinical Interview
This interview was conducted in a face-to-face format by a trained psychologist and assessed sociodemographic variables and clinical features, such as gender, age, type of surgery, diet, and weight history. Height, pre-surgery weight, and post-surgery weight were obtained from hospital charts. The diagnostic items of the eating disorder examination [41] assessed objective binge episodes, characterized by episodes of eating an objectively large amount of food with a feeling of loss of control, and subjective binge episodes, characterized by eating small/modest amounts of food with loss of control perceived as excessive by the respondent. The Rep(eat) interview [38] was used to assess grazing behavior, generally defined as eating repetitively small/modest amounts of food in an unplanned manner and not in response to sensations of hunger/satiety. The interviewer rated the number of days per week in the previous month in which the participant engaged in grazing behavior.
Eating Disorder Examination—Questionnaire, EDE-Q [42]
The Portuguese version of this 28-item self-report measure [43] was used to evaluate eating disorder psychopathology. It generated four subscales (restraint, shape concern, weight concern, and eating concern) and a global score. Higher scores indicated greater psychopathology.
Depression Anxiety Stress Scale—DASS-21 [44, 45]
This 21-item self-report scale assessed depression, anxiety, and stress. A higher score revealed greater distress.
Negative Urgency—UPPS-P [46]
This subscale of the impulsivity measure UPPS-P Impulsive Behavior Scale was composed of 12 items and evaluated the tendency to act impulsively when under negative emotions. Higher scores indicated greater negative urgency.
Repetitive Eating Questionnaire—Rep(eat)-Q [47]
This 12-item self-report questionnaire assessed a grazing-type eating pattern and generated two subscales: compulsive grazing and repetitive eating. Higher scores corresponded to more grazing.
Statistical Analysis
Data were analyzed using IBM SPSS® statistics V24 software. T tests and chi-squared tests were used to compare the P-Group and R-Group patients for problematic eating behaviors and weight-related variables. When appropriate, Bonferroni correction was used to adjust for multiple tests by dividing the p value by the number of comparisons conducted, resulting in statistical significance when p < 0.0125 (i.e., 0.05/4). Multivariate analysis of variance (MANOVA) was performed to test differences in the subscales of each measure between the P-Group and R-Group at baseline and 6 months after surgery.
Generalized estimating equations (GEEs) were used to investigate changes in self-report measures over time. Generalized linear models (GLMs) with gamma distribution and log link were used to test predictors of the percentage of total weight loss (%TWL). Two models were tested that included pre- and post-surgery predictors: one model for the R-Group and one model for the P-Group. Type of surgery was included as a covariant in all models.
The different weight-related variables were computed as follows: Body mass index (BMI): weight/(height2); Percentage of total weight loss (%TWL): (weight pre-surgery−weight post-primary surgery/weight pre-surgery) × 100; Percentage of excessive weight loss (%EWL): (weight pre-surgery−weight post-surgery/excess weight) × 100. Excess weight was calculated based on the metropolitan guidelines.
Results
In the R-Group, 48.3% of patients (n = 56) mentioned weight regain/poor weight loss as the reason for reoperative surgery, while 29.3% (n = 34) referred to anatomical and medical complications, and 22.4% (n = 26) mentioned both. The duration of the first procedure ranged from 1 to 17 years (M = 6.50; SD = 2.92), and the mean BMI preprimary surgery was 44.70 (SD = 5.94). The mean %TWL was 14.15 (SD = 13.86), and the mean %EWL was 34.94 (SD = 36.17). No patient presented successful weight loss (%EWL ≥ 50) at the time of band removal.
There were no statistically significant differences in sociodemographic variables, except for age (Table 1). Compared to the P-Group patients, patients undergoing reoperative surgery were older. Additionally, compared to the P-Group patients, the R-Group patients presented a similar pre-surgery BMI but a superior BMI after surgery and a significantly lower %TWL. A higher percentage of R-Group patients underwent gastric bypass than P-Group patients (67.2% vs 50.8%), and the P-Group had a higher percentage of gastric sleeve (49.2%) than the R-Group (32.8%).
Table 2 summarizes the percentage of patients in both groups who reported each problematic eating behavior based on the EDE and Rep(eat) interview. Overall, approximately 63.9% of patients presented at least one problematic eating behavior in the pre-surgery assessment and 22.7% in the 6-month assessment. In the pre-surgery assessment, the percentage of patients reporting any of the different problematic eating behaviors assessed (objective/subjective binge-eating episodes or grazing) was not significantly different in the two groups. Regarding the post-surgery assessment, neither group reported objective binge-eating episodes. However, a statistically significant difference was found in the percentage of patients reporting grazing episodes at least once a week in the post-surgery assessment; this percentage was higher for the R-Group (21.6% vs 8.2%).
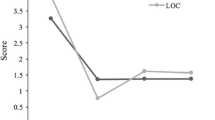
Table 3 describes the scores of the self-report psychological and behavioral measures: disordered eating, depression, anxiety and stress, negative urgency, and grazing evaluated pre- and post-surgery. Considering the preoperative assessment, the R-Group showed significantly higher shape concern (EDE-Q subscale). No statistically significant differences between groups were found for the other EDE-Q subscales or self-report measures assessing depression, anxiety, stress, and grazing. However, significant differences were found in most of the self-report measures at 6 months after surgery. The R-Group scored significantly higher on restraint, shape, and weight concern (EDE-Q subscales); depression and anxiety (DASS-21); and compulsive grazing (the Rep(eat)-Q subscale).
This study also aimed to investigate if both groups had different changes in terms of psychological and behavioral variables from pre- to post-surgery. Globally, a significant main effect of time was found, i.e., both groups improved from pre-surgery to 6 months after surgery regarding disordered eating (global EDE-Q; β = 0.293, SE = 0.346; Waldχ2 = 162.60, p = 0.000), depression (β = 0.365, SE = 0.102; Waldχ2 = 39.78, p = 0.000), anxiety (β = 0.298, SE = 0.080; Waldχ2 = 42.70, p = 0.000), stress (β = 0.283, SE = 0.069; Waldχ2 = 34.70, p = 0.000), UPPS-P (β = 0.143, SE = 0.027; Waldχ2 = 58.64, p = 0.000), and total Rep(eat)-Q (β = 0.478, SE = 0.069; Waldχ2 = 174.62, p = 0.000). Moreover, a significant group main effect was found concerning disordered eating (global EDE-Q; β = − 0.18, SE = 0.05; Waldχ2 = 13.85, p = 0.000), depression (β = −0.39, SE = 0.140; Waldχ2 = 5.64, p = 0.018), and stress (β = − 0.20, SE = 0.102; Waldχ2 = 4.11, p = 0.043), suggesting that despite the improvement, the R-Group presented more disordered eating symptoms, depression, and anxiety than the P-Group in both assessment moments. Finally, GEEs showed significant interaction effects between groups and time for total Rep(eat)-Q (β = 0.22, SE = 0.09; Waldχ2 = 6.11, p = 0.013), suggesting a significantly different trend in time, with the P-Group presenting a more pronounced improvement in grazing from pre- to post-surgery than the R-Group. A significant interaction effect was also found for anxiety (β = 0.28, SE = 0.14; Waldχ2 = 4.44, p = 0.035), showing that the P-Group presents a more marked improvement in anxiety than the R-Group. GEE models found nonsignificant interaction effects on the global EDE-Q (β = 0.07, SE = 0.05; Waldχ2 = 1.91, p = 0.167), stress (β = 0.09, SE = 0.11; Waldχ2 = 0.63, p = 0.428), and UPPS-P (β = 0.01, SE = 0.04; Waldχ2 = 0.08, p = 0.774), suggesting that the P-Group and R-Group changed similarly across time in these dimensions.
Finally, this study intended to investigate short-term predictors of weight loss (%TWL) for both groups. Tested predictors included pre- and post-assessment of the global EDE-Q and subscales; depression, anxiety, and stress subscales; negative urgency (UPPS-P); total Rep(eat)-Q and subscales, and frequency of different problematic eating behaviors. Regarding the P-Group, no significant predictors were found at baseline or at the 6-months follow-up (likelihood ratio χ2 = 0.70, p = 0.872). On the other hand, considering the R-Group, GLM generated a significant model (likelihood ratio χ2 = 9.09, p = 0.01) in which increased post-surgery anxiety (Waldχ2(1) = 6.19, p = 0.01) and higher number of days with post-surgery grazing the previous month (Waldχ2(1) = 3.90, p = 0.04) emerged as significant predictors of less %TWL at 6 months.
Discussion
Despite the similarities between the P- and R-Groups in the preoperative assessment, differences at 6 months after surgery were more pronounced. Although both groups showed similar pre-surgery sociodemographics and BMI, the R-Group had a significantly higher percentage of patients reporting grazing episodes postoperatively (21.6% vs 8.2%). The R-Group also scored higher in most of the psychopathological self-report measures assessed after surgery, presenting greater restraint, shape and weight concern, depression, anxiety, and compulsive grazing. Moreover, although the groups presented significant improvements in eating behavior and related psychological aspects from pre- to post-surgery, these results showed that the R-Group had significantly less pronounced improvement in grazing and anxiety. Considering that these aspects are associated with poor treatment outcomes [28, 29], these data bring evidence to the hypothesis that the R-Group may be a risk group for poorer psychological, behavioral, and weight-related outcomes.
Finally, no significant pre- or post-predictor of weight loss was found for the P-Group. Likewise, no pre-surgery predictor of weight loss was found in the R-Group. However, more post-surgery anxiety and more frequent postoperative grazing were associated with less %TWL for the R-Group at the 6-month follow-up. Research has shown that post-surgery grazing is a risk factor for worse long-term weight loss in primary bariatric surgery [6, 27, 28, 47, 48]. Grazing behavior has been associated with poor compliance with diet and medical appointments in primary bariatric surgery [49]. Past research has stressed that post-surgery anxiety is related to worse weight loss results in primary surgery [31, 50], and this study has shown that the same situation occurs in patients undergoing reoperative surgery. This study shows evidence that this behavior is a risk factor for poor weight outcomes at earlier stages of treatment for patients undergoing reoperative surgery.
Together, these data suggest that the increased presence of problematic eating behaviors, greater psychological distress, and disordered eating psychopathology may play a role in the poorer weight outcomes of patients undergoing reoperative surgeries. In particular, the assessment and earlier detection of grazing behavior and psychological distress in patients undergoing a secondary surgery may represent an important strategy to optimize weight loss with this treatment. As suggested by previous research with patients undergoing primary surgery, since outcomes tend to deteriorate over time [37], these short-term differences would be expected to become more pronounced in future assessments. Longitudinal research with longer follow-up times is needed to investigate if these differences found as early as at 6 months after surgery result in long-term difficulties for the R-Group. Accordingly, Kafri and colleagues [18] showed that the R-Group patients reported more nonnormative eating patterns and less healthy food selection than P-Group patients at 18 months after surgery.
The strengths of this study include the longitudinal design, the fact that anthropometric data were obtained from hospital charts, and the face-to-face assessment (using a validated clinical interview) of different types of problematic eating conducted by a trained psychologist. Although the analyses were controlled regarding the type of surgery, the two groups differed in the type of surgery received. However, patients receiving gastric sleeve or gastric bypass in this study did not differ in any of the relevant aspects: weight loss [15, 51, 52], problematic eating behaviors, or psychological measures (data not shown but available upon request). Thus, differences between the R- and P-Groups are not expected to be due to the different proportions of gastric bypass/sleeve. Finally, the R-Group included patients reporting a variety of reasons for failure of their first surgery, and future studies should investigate if the reasons for failure of a primary surgery are predictors of success of the reoperative procedure.
Conclusion
Patients undergoing reoperative surgery presented more eating problems and higher levels of psychological distress than primary surgery patients. Reoperative patients lose significantly less weight than primary surgery patients, which seems to be associated with post-surgery psychological and behavioral aspects, particularly postoperative anxiety and grazing behavior. These data suggest that these patients may be at risk of poorer long-term weight outcomes and may require specific clinical follow-up care.
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery. JAMA. 2004;292:1724–37. https://www.ncbi.nlm.nih.gov/pubmed/15479938
Pories WJ. Bariatric surgery: risks and rewards. J Clin Endocrinol Metab. 2008;93:S89–96. http://www.ncbi.nlm.nih.gov/pubmed/18987275
Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:1045–57. https://www.ncbi.nlm.nih.gov/pubmed/15616203
Patel S, Szomstein S, Rosenthal RJ. Reasons and outcomes of reoperative bariatric surgery for failed and complicated procedures (excluding adjustable gastric banding). Obes Surg. 2011;21:1209–19. http://www.ncbi.nlm.nih.gov/pubmed/20676940
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18:648–51. https://www.ncbi.nlm.nih.gov/pubmed/18392907
Kofman MD, Lent MR, Swencionis C. Maladaptive eating patterns, quality of life, and weight outcomes following gastric bypass: results of an internet survey. Obesity. 2010;18:1938–43. https://www.ncbi.nlm.nih.gov/pubmed/20168309
Beck NN, Mehlsen M, Støving RK. Psychological characteristics and associations with weight outcomes two years after gastric bypass surgery: postoperative eating disorder symptoms are associated with weight loss outcomes. Eat Behav. 2012;13:394–7. https://www.ncbi.nlm.nih.gov/pubmed/23121796
Sarwer DB, Dilks RJ, West-Smith L. Dietary intake and eating behavior after bariatric surgery: threats to weight loss maintenance and strategies for success. Surg Obes Relat Dis. 2011;7:644–51. https://www.ncbi.nlm.nih.gov/pubmed/21962227
Hii MW, Lake AC, Kenfield C, et al. Laparoscopic conversion of failed gastric banding to Roux-en-Y gastric bypass. Short-term follow-up and technical considerations. Obes Surg. 2012;22:1022–8. https://www.ncbi.nlm.nih.gov/pubmed/22252745
Spyropoulos C, Kehagias I, Panagiotopoulos S, et al. Revisional bariatric surgery - 13-year experience from a tertiary institution Charalambos. Arch Surg. 2010;145:173–7. https://www.ncbi.nlm.nih.gov/pubmed/20157086
Lanthaler M, Aigner F, Kinzl J, et al. Long-term results and complications following adjustable gastric banding. Obes Surg. 2010;20:1078–85. https://www.ncbi.nlm.nih.gov/pubmed/20496124
Himpens J, Cadière GB, Bazi M, et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011;146:802–7. https://www.ncbi.nlm.nih.gov/pubmed/21422330
Kellogg TA. Revisional bariatric surgery. Surg Clin N Am. 2011;91:1353–71. https://www.ncbi.nlm.nih.gov/pubmed/22054158
Courcoulas AP, King WC, Belle SH, et al. Seven-year weight trajectories and health outcomes in the longitudinal assessment of bariatric surgery (LABS) study. JAMA Surg. 2017;15213:2–9. https://www.ncbi.nlm.nih.gov/pubmed/29214306
Fischer L, Hildebrandt C, Bruckner T, et al. Excessive weight loss after sleeve gastrectomy: a systematic review. Obes Surg. 2012;22:721–31. https://www.ncbi.nlm.nih.gov/pubmed/22411568
Zingg U, McQuinn A, DiValentino D, et al. Revisional vs. primary Roux-en-Y gastric bypass--a case-matched analysis: less weight loss in revisions. Obes Surg. 2010;20:1627–32. https://www.ncbi.nlm.nih.gov/pubmed/20577830
Zhang L, Tan WH, Chang R, et al. Perioperative risk and complications of revisional bariatric surgery compared to primary Roux-en-Y gastric bypass. Surg Endosc. 2015;29:1316–20. https://www.ncbi.nlm.nih.gov/pubmed/25294534
Kafri N, Valfer R, Nativ O, et al. Behavioral outcomes following laparoscopic sleeve gastrectomy performed after failed laparoscopic adjustable gastric banding. Obes Surg. 2013;23:346–52. http://www.ncbi.nlm.nih.gov/pubmed/23104388
Martin MJ, Mullenix PS, Steele SR, et al. A case-match analysis of failed prior bariatric procedures converted to resectional gastric bypass. Am J Surg. 2004;187:666–71. https://www.ncbi.nlm.nih.gov/pubmed/15135688
Topart P, Becouarn G, Ritz P. One-year weight loss after primary or revisional Roux-en-Y gastric bypass for failed adjustable gastric banding. Surg Obes Relat Dis. 2009;5:459–62. https://www.ncbi.nlm.nih.gov/pubmed/18996766
Jennings NA, Boyle M, Mahawar K, et al. Revisional laparoscopic Roux-en-Y gastric bypass following failed laparoscopic adjustable gastric banding. Obes Surg. 2013;23:947–52.
Hamdi A, Julien C, Brown P, et al. Midterm outcomes of revisional surgery for gastric pouch and gastrojejunal anastomotic enlargement in patients with weight regain after gastric bypass for morbid obesity. Obes Surg. 2014;24:1386–90. https://www.ncbi.nlm.nih.gov/pubmed/24634099
Gobble RM, Parikh MS, Greives MR, et al. Gastric banding as a salvage procedure for patients with weight loss failure after Roux-en-Y gastric bypass. Surg Endosc. 2008;22:1019–22. https://www.ncbi.nlm.nih.gov/pubmed/17943353
Pinto-Bastos A, Conceição EM, Machado PPP. Reoperative bariatric surgery: a systematic review of the reasons for surgery, medical and weight loss outcomes, relevant behavioral factors. Obes Surg. 2017;27:2707–15. Erratum in: Obes. Surg. 2017;27:3069–72. https://www.ncbi.nlm.nih.gov/pubmed/28791623
Kuzminov A, Palmer AJ, Wilkinson S, et al. Re-operations after secondary bariatric surgery: a systematic review. Obes Surg. 2016;26:2237–47. https://www.ncbi.nlm.nih.gov/pubmed/27272668
de Zwaan M, Hilbert A, Swan-Kremeier L, et al. Comprehensive interview assessment of eating behavior 18-35 months after gastric bypass surgery for morbid obesity. Surg Obes Relat Dis. 2010;6:79–85. https://www.ncbi.nlm.nih.gov/pubmed/19837012
Sioka E, Tzovaras G, Oikonomou K, et al. Influence of eating profile on the outcome of laparoscopic sleeve gastrectomy. Obes Surg. 2013;23:501–8. https://www.ncbi.nlm.nih.gov/pubmed/23196993
Conceição, Mitchell JE, Vaz AR, et al. The presence of maladaptive eating behaviors after bariatric surgery in a cross sectional study: importance of picking or nibbling on weight regain. Eat Behav. 2014;15:558–62. https://www.ncbi.nlm.nih.gov/pubmed/25213792
Legenbauer T, Petrak F, De Zwaan M, et al. Influence of depressive and eating disorders on short- and long-term course of weight after surgical and nonsurgical weight loss treatment. Compr Psychiatry. 2011;52:301–11. https://www.ncbi.nlm.nih.gov/pubmed/21497225
Dymek MP, le Grange D, Neven K, et al. Quality of life and psychosocial adjustment in patients after Roux-en-Y gastric bypass: a brief report. Obes Surg. 2001;11:32–9. https://www.ncbi.nlm.nih.gov/pubmed/11361166
Kalarchian MA, Marcus MD, Levine MD, et al. Relationship of psychiatric disorders to 6-month outcomes after gastric bypass. Surg Obes Relat Dis. 2008;4:544–9. https://www.ncbi.nlm.nih.gov/pubmed/18514586
Semanscin-Doerr DA, Windover A, Ashton K, et al. Mood disorders in laparoscopic sleeve gastrectomy patients: does it affect early weight loss? Surg Obes Relat Dis. 2010;6:191–6. https://www.ncbi.nlm.nih.gov/pubmed/20189470
Dixon JB, Dixon ME, O’Brien PE. Pre-operative predictors of weight loss at 1-year after lap-band surgery. Obes Surg. 2001;11:200–7. https://www.ncbi.nlm.nih.gov/pubmed/11355027
Espel HM, Muratore AF, Lowe MR. An investigation of two dimensions of impulsivity as predictors of loss-of-control eating severity and frequency. Appetite. 2017;26:9–16. https://www.ncbi.nlm.nih.gov/pubmed/28601678
Fischer S, Wonderlich J, Breithaupt L, et al. Negative urgency and expectancies increase vulnerability to binge eating in bulimia nervosa. Eat Disord. 2018;26:39–51. https://www.ncbi.nlm.nih.gov/pubmed/29384460
Schag K, Mack I, Giel KE, et al. The impact of impulsivity on weight loss four years after bariatric surgery. Nutrients. 2016;8:1–9. https://www.ncbi.nlm.nih.gov/pubmed/27854246
Conceição EM, Mitchell JE, Pinto-Bastos A, et al. Stability of problem eating behaviors and weight loss trajectories following bariatric surgery: a longitudinal observational study. Surg Obes Relat Dis. 2017;13:1063–70. https://www.ncbi.nlm.nih.gov/pubmed/28209532
Conceição E, Mitchell JE, Engle SG, et al. What is “grazing”? Reviewing its definition, frequency, clinical characteristics, and impact on bariatric surgery outcomes, and proposing a standardized definition. Surg Obes Relat Dis. 2014;10:973–82. https://www.ncbi.nlm.nih.gov/pubmed/25312671
García-Ruiz-de-Gordejuela A, Agüera Z, Granero R, et al. Weight loss trajectories in bariatric surgery patients and psychopathological correlates. Eur Eat Disord Rev. 2017;25:586–94. https://www.ncbi.nlm.nih.gov/pubmed/28971543
Conceição E, Pinto-Bastos A, de Lourdes M, Brandão I, et al. Psychological, behavioral and weight-related aspects of patients undergoing reoperative bariatric surgery after gastric band: comparison with primary surgery patients. Surg Obes Relat Dis. 2018;14:603–10. https://www.ncbi.nlm.nih.gov/pubmed/29567056
Fairburn C, Cooper Z, O’Connor M. Eating disorder examination (16.0D). In: Fairburn C, editor. Cogn. Behav. Ther. Eat. Disord. New York: Guilford Press; 2008.
Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16:363–70. https://www.ncbi.nlm.nih.gov/pubmed/7866415
Machado P, Martins C, Vaz A, et al. Eating disorder examination questionnaire (EDE-Q): psychometric properties and norms for the Portuguese population. Eur Eat Disord Rev. 2014;22:448–53. https://www.ncbi.nlm.nih.gov/pubmed/25175299
Lovibond SH, Lovibond PF. Manual for the depression, anxiety, stress scales. 2nd ed. Psychology Foundation: Sydney; 1995.
Pais-Ribeiro JL, Honrado A, Leal I. Contribuição Para O Estudo Da Adaptação Portuguesa Das Escalas De Ansiedade, Depressão E Stress (EADS) De 21 Itens De Lovibond E Lovibond. Psicol Saúde Doenças. 2004;5:229–39.
Whiteside SP, Lynam DR, Miller JD, et al. Validation of the UPPS impulsive behavior scale: a four factor model of impulsivity. Eur J Personal. 2005;19:559–74.
Conceição EM, Mitchell JE, Machado PPP, et al. Repetitive eating questionnaire [Rep(eat)-Q]: enlightening the concept of grazing and psychometric properties in a Portuguese sample. Appetite. 2017;117:351–8. https://www.ncbi.nlm.nih.gov/pubmed/28712976
Colles SL, Dixon JB, O’Brien PE. Grazing and loss of control related to eating: two high-risk factors following bariatric surgery. Obesity. 2008;16:615–22. https://www.ncbi.nlm.nih.gov/pubmed/18239603
Faria SL, De Oliveira KE, Lins RD, et al. Nutritional management of weight regain after bariatric surgery. Obes Surg. 2010;20:135–9. https://www.ncbi.nlm.nih.gov/pubmed/18575942
de Zwaan M, Enderle J, Wagner S, et al. Anxiety and depression in bariatric surgery patients : a prospective , follow-up study using structured clinical interviews. J Affect Disord. 2011;133:61–8. https://www.ncbi.nlm.nih.gov/pubmed/21501874
Leyba JL, Llopis SN, Aulestia SN. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the treatment of morbid obesity. A prospective study with 5 years of follow-up. Obes Surg. 2014;24:2094–8. https://www.ncbi.nlm.nih.gov/pubmed/25012769
Lakdawala MA, Bhasker A, Mulchandani D, et al. Comparison between the results of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-y gastric bypass in the Indian population: a retrospective 1 year study. Obes Surg. 2010;20:1–6. https://www.ncbi.nlm.nih.gov/pubmed/19802646
Acknowledgements
The authors acknowledge the AMTCO group (Avaliação Multidisciplinar do Tratamento Cirúrgico da Obesidade) at the Hospital of São João for conducting the multidisciplinary treatment as usual of the participants of this study.
Funding
This study was partially conducted at Psychology Research Centre (PSI/01662), University of Minho, and supported by the Portuguese Foundation for Science and Technology and the Portuguese Ministry of Science, Technology and Higher Education through national funds, and co-financed by FEDER through COMPETE2020 under the PT2020 Partnership Agreement (POCI-01-0145-FEDER-007653), by the following grants to Eva Conceição (IF/01219/2014 and POCI-01-0145-FEDER-028209), and doctoral scholarship to Ana Pinto-Bastos (SFRH/BD/104159/2014). The funding body had no role in the design, collection, analysis, and interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the institutional ethics committees of the hospital and university involved.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
(DOCX 53 kb)
Rights and permissions
About this article
Cite this article
Pinto-Bastos, A., Conceição, E., de Lourdes, M. et al. Psychological and Behavioral Aspects of Primary and Reoperative Surgery: a 6-Month Longitudinal Study. OBES SURG 28, 3984–3991 (2018). https://doi.org/10.1007/s11695-018-3452-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3452-0