Abstract
We aim to review the available literature on obese patients treated with one-anastomosis gastric bypass (OAGB) or laparoscopic sleeve gastrectomy (LSG), in order to compare the clinical outcomes and intraoperative parameters of the two methods. A systematic literature search was performed in PubMed, Cochrane Library, and Scopus databases, in accordance with the PRISMA guidelines. Seventeen studies met the inclusion criteria incorporating 6761 patients. This study reveals increased weight loss, remission of comorbidities, shorter mean hospital stay, and lower mortality in the OAGB group. The incidence of leaks and intra-abdominal bleeding was similar between the two approaches. Well-designed, randomized controlled studies, comparing LSG to OAGB, are necessary to further assess their clinical outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity is a rising epidemic, and bariatric surgery continues to be the main therapeutic modality for a high rate of sustainable weigh loss [1] and enhanced metabolic profile [2]. A standalone bariatric procedure that currently has gained increased popularity is laparoscopic sleeve gastrectomy (LSG) [3, 4]. In fact, LSG was the most frequent bariatric procedure in the USA in 2013 [5]. LSG is a mainly restrictive procedure that preserves the normal gastrointestinal continuity without any anastomoses.
One-anastomosis gastric bypass (OAGB) is also an alternative safe, feasible, and effective bariatric procedure [6]. It employs a long gastric tube in conjunction with an antecolic loop gastrojejunal anastomosis [7]. Since the landmark study of Rutledge [7], additional reports [8, 9] have demonstrated excellent outcomes in obese patients treated with OAGB. As the number of studies assessing the feasibility of OAGB increases, it is necessary to examine whether the results between the two techniques are at least equivalent. The purpose of this study is to summarize the existing evidence comparing the surgical outcomes of OAGB and LSG in the treatment of morbid obesity.
Materials and Methods
Search Strategy and Article Selection
The present study was conducted in accordance with the protocol agreed by all authors and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [10]. A thorough literature search was performed in PubMed (Medline), Cochrane Central Register of Controlled Trials (CENTRAL), and Scopus (Elsevier) databases (last search: June 3, 2017) using the following terms in every possible combination: “omega loop,” “one anastomosis,” “single-anastomosis,” “mini-gastric bypass,” and “sleeve gastrectomy.” Inclusion criteria were (1) original reports with >10 patients, (2) written in the English language, (3) published from 1980 to 2017, (4) conducted on human subjects, and (5) reporting outcomes of LSG or OAGB on obese patients. Two independent reviewers (DEM and VST) extracted the data from the included studies. Any discrepancies between the investigators about the inclusion or exclusion of studies were discussed with the guarantor author (DZ) in order to include articles that best matched the criteria, until consensus was reached. Moreover, the reference lists of all included articles were assessed for additional potentially eligible studies.
Data Extraction
For each eligible study, data were extracted relative to demographics (number of patients, mean age, sex, comorbidities, preoperative body mass index (BMI)) and to the intraoperative parameters and outcomes (mean operative time, mean hospital stay, bougie diameter, revisions, intraoperative and postoperative complications, remission of comorbidities, and percentage of excess weight loss (%EWL) after 12 and 24 months). Two authors (DEM and VST) performed the data extraction independently and compared the validity of the data. Any discrepancies were discussed with the guarantor author (DZ), until consensus was reached.
Statistical Analysis
Based on the extracted data, regarding the categorical outcomes, the odds ratios (ORs) and 95% confidence interval (CI) were calculated, based on the extracted data, by means of random-effects model (the Mantel-Haenszel statistical method), where the number of studies providing data was sufficient. OR <1 denoted outcome was more frequent in the OAGB group. Continuous outcomes were evaluated by means of weighted mean difference (WMD) with its 95% CI, using random-effects (inverse variance statistical method) models, appropriately to calculate pooled effect estimates. In cases where WMD <0, values in the OAGB group were higher. We chose the random-effects model because we did not expect that all the included studies would share a common effect size. Between-study heterogeneity was assessed through Cochran’s Q statistic and by estimating I 2 [11].
In cases where multiple studies analyzed the same population (i.e., series from the same hospital), only the larger study or the one with the longest follow-up (if the sample was similar) was included in the meta-analysis.
Quality and Publication Bias Assessment
The Newcastle-Ottawa Quality Assessment Scale (NOS) [12] was used as an assessment tool to evaluate non-RCTs. The scale’s range varies from zero to nine stars. Studies with a score equal to or higher than 5 were considered to have adequate methodological quality to be included. The RCTs were assessed for their methodological quality with the tools that are used to evaluate the risk of bias according to the Cochrane Handbook for Systematic Reviews of Interventions [13]. Two reviewers (DEM and VST) rated the studies independently, and the final decision was reached by consensus.
The existence of publication bias was assessed by the visual inspection of funnel plots. It could not be further evaluated using Egger’s formal statistical test [14] because the number of the studies included in the analysis was not adequate (less than 10), thus compromising substantially the power of the test.
Results
Article Selection and Patient Demographics
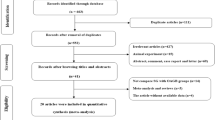
The flow diagram of the literature search is shown in Fig. 1. Among the 97 articles in PubMed, CENTRAL, and Scopus databases that were retrieved, ten comparative studies [15,16,17,18,19,20,21,22,23,24] were included in the qualitative and quantitative synthesis and seven non-comparative studies [7, 25,26,27,28,29,30] were included in the qualitative synthesis. The study design was retrospective in nine [16, 17, 19, 21, 22, 25, 28,29,30], prospective in six [7, 15, 20, 24, 26, 27], and randomized controlled in two [18, 23] studies. The studies included were conducted in India [15, 17, 23], France [16, 27], Taiwan [18], UK [19], Italy [20, 21, 24], Germany [22], Greece [25], Spain [26], Austria [28], Israel [29], USA [7], and Egypt [30] and were published between 2001 and 2017. The OAGB sample size ranged from 15 to 1520 patients. The total sample size was 6761 patients; 1225 patients were treated with LSG and 5536 patients were treated with OAGB. Preoperative mean BMI was ≥30 kg/m2 in all included patients. Characteristics of studies comparing the outcomes between patients treated with LSG and patients treated with OAGB are provided in Table 1. Baseline characteristics of the patients included in non-comparative studies are demonstrated in Table S1. The Newcastle-Ottawa rating scale assessment for all studies is shown in Table 1, and the quality assessment of RCTs is shown in Table S2. Perioperative and postoperative outcomes regarding comparative and non-comparative studies are presented in Table 2 and Table S3, respectively. Pooled ORs and I 2 and p values of heterogeneity for all outcomes are summarized in Table 3.
Mean Operative Time and Length of Hospital Stay
Mean operative time ranged from 44.8 to 112.1 min for the LSG group and from 52 to 92 min for the OAGB group (Table 2). Mean operative time was similar in both groups (WMD 4.80 [−10.71, 20.31]; p = 0.54) as shown in Table 3. The length of hospital stay ranged from 2 to 7.2 days for the LSG group, while it ranged from 2 to 4.5 days for the OAGB group (Table 3). According to our analysis, the length of hospital stay was greater in the LSG group (WMD 1.29 [0.45, 2.12]; p = 0.002).
Complications
According to our six-arm analysis, the incidence of leaks was similar between patients with either LSG or OAGB (OR 2.95 [95% CI 0.81, 10.81]; p = 0.10). Moreover, the incidence of intra-abdominal bleeding (OR 0.95 [95% CI 0.43, 2.11]; p = 0.90) and anemia (OR 0.65 [95% CI 0.34, 1.24]; p = 0.19) was comparable between the two groups. The incidence of malnutrition (OR 0.09 [95% CI 0.01, 0.88]; p = 0.04) and marginal ulcer (OR 0.13 [95% CI 0.02, 0.74]; p = 0.02) was greater in the OAGB group. The incidence of bile reflux disease was greater in patients that underwent LSG (OR 4.55 [95% CI 1.87, 11.05]; p = 0.0008). Forest plots regarding complications are demonstrated in Figure S1.
Revisions and Mortality
The incidence of revisions was significantly increased in the LSG group (OR 6.18 [95% CI 2.09, 18.26]; p = 0.001). Mortality was significantly increased in the LSG group (OR 10.52 [95% CI 1.24, 89.20]; p = 0.03).
Resolution of Comorbidities
Seven studies [15,16,17, 19,20,21, 23] assessed the postoperative type 2 diabetes (T2D) remission which was greater in the OAGB group (OR 0.46 [95% CI 0.32, 0.64]; p < 0.00001) (Fig. 2). According to our six-arm analysis, hypertension (HTN) remission was increased in patients treated with OAGB (OR 0.67 [95% CI 0.49, 0.90]; p = 0.008) (Fig. 2). Resolution of dyslipidemia was also increased in the OAGB group (OR 0.32 [95% CI 0.19, 0.56]; p < 0.0001) (Fig. 2). The postoperative obstructive sleep apnea syndrome (OSAS) remission was similar between the two modalities (OR 0.48 [95% CI 0.21, 1.09]; p = 0.08).
Weight Loss Outcome
In our study, we examined the postoperative %EWL after 12 and 24 months. It ranged between 34.3 and 69 after 12 months and between 38 and 66.2 after 12 months for the LSG group. In addition, the %EWL for the OAGB group ranged between 38.2 and 66.2 after 12 months and between 66 and 71.6 after 24 months. According to our analysis (Fig. 3), the %EWL after 1 year was increased in the OAGB group (WMD −6.52 [95% CI −11.65, −1.40]; p = 0.01). However, the %EWL after 2 years was similar between the two groups (WMD −16.78 [95% CI −38.92, 5.37]; p = 0.14) (Fig. 3). Only one study [28] assessed the %EWL at 10 years postoperatively regarding LSG (%EWL 54.0 ± 26.7).
Forest plot describing the differences in a dyslipidemia remission, b type 2 diabetes remission, and c hypertension remission. a Resolution of dyslipidemia was increased in the OAGB group. b Resolution of type 2 diabetes was increased in the OAGB group. c Resolution of hypertension was increased in the OAGB group
Publication Bias
Heterogeneity was low regarding the categorical outcomes. In contrast, heterogeneity was high regarding the continuous outcomes. The funnel plots that were produced in order to assess publication bias are shown in Figures S2-S4. The asymmetries that were found are mainly attributed to the small number of the included studies, thus proposing that more are necessary in order to eliminate publication bias. Egger’s test was not performed due to the small number of the studies that were included.
Discussion
The LSG has gained increased popularity as a standalone procedure for morbid obesity [3]. However, another bariatric procedure that has attracted the interest of a significant number of bariatric surgeons is OAGB [6]. This systematic review and meta-analysis identified 17 articles comparing LSG and OAGΒ as two alternative bariatric procedures, measuring patients’ outcomes published between 2001 and 2017. No similar meta-analysis was identified through literature search. The articles included in this study bring us closer to linking the implementation of either method with improved standards of safety and efficiency.
The present study demonstrates that both LSG and OAGΒ are well-tolerated, feasible, and effective surgical approaches. Mean operative time was similar between the two approaches. However, mean hospital stay was increased in patients treated with LSG.
Both techniques are associated with small rates of complications and revisions, being significantly safe. Leaks and hemorrhage are the main risks of bariatric procedures, due to the long stapled lines and gastrointestinal anastomosis. According to our findings, the incidence of leaks and hemorrhage was comparable between the two groups. Despite the bypassed duodenum in OAGB, the incidence of anemia was comparable between the two groups. In contrast, the incidence of malnutrition and marginal ulcer was increased in the OAGB group.
The risk of postoperative bile reflux, along with gastritis and/or esophagitis, remains one of the main criticisms regarding OAGB and originates from the first omega procedures performed by Mason and Ito in the 1960s [31]. According to a recent study in animal models [32], although the mean bile acid concentration was higher in rats that underwent OAGB compared to sham rats, the OAGB procedure was not related to an increased risk of precancerous or cancerous conditions of the esophagus. However, the results of the included studies demonstrate that the bile reflux is not a common problem, because the anastomosis is located low in the stomach. In fact, according to our analysis, the incidence of bile reflux disease was increased in the LSG group. These findings are also in accordance with the primarily restrictive characteristics of LSG. In the same context, Tolone et al. [24] have demonstrated that the SG approach contributes to increased esophageal reflux exposure and greater number of reflux episodes, while it has also been associated with augmented rate (14%) of Barrett’s metaplasia at 10 years postoperatively [28].
Reoperation rate is always a concern when a novel technique is examined. In our study, the need for revisional operation was increased in the LSG group. This finding may be attributed to the fact that LSG is performed as a first operation in a two-stage approach, especially in super-obese patients. In the same context, mortality was increased in the LSG group, probably due to the increased preoperative BMI and/or comorbidities.
From the 17 studies included, 5 studies [16, 17, 19, 21, 22, 24, 25, 27,28,29,30] assessed %EWL after 1 year and 2 studies [7, 17, 19, 25,26,27] after 2 years. Only one study [28] assessed %EWL at 10 years postoperatively regarding LSG. According to our analysis, OAGB was associated with increased %EWL in 1 year. However, %EWL was similar between the two groups after 2 years. There was no available long-term data from comparative studies regarding %EWL. Nevertheless, Felsenreich et al. [28] have demonstrated that LSG is associated with increased weight regain at 10 years postoperatively.
Weight loss is directly associated with remission of T2D and dyslipidemia. In fact, OAGB resulted to greater T2D and dyslipidemia remission compared to LSG, that is in accordance with its effect on %EWL. A possible explanation is that OAGB combines the effects of some restriction with fat malabsorption [33]. Moreover, OAGB resulted to increased HTN remission compared to LSG, possibly due to weight loss and the consequent control of obesity-related HTN.
This meta-analysis demonstrates the superiority of OAGB compared to LSG as a standalone procedure. Nonetheless, it also demonstrates the need for additional studies comparing LSG with the OAGB. Ideally, these would be randomized controlled studies, with prospective design and longer follow-up. For rare events, such as complications and mortality, a large sample is needed. The studies included offer a specific linkage to patient outcomes, complications, and weight loss.
The limitations of this meta-analysis reflect the limitations of the studies included. Nine studies [16, 17, 19, 21, 22, 25, 28,29,30] (53%) were retrospective, thus posing a certain limitation in this study. Six studies [7, 15, 20, 24, 26, 27] were prospective, and two studies [18, 23] were randomized controlled studies. Moreover, the small number of the studies included in the quantitative synthesis poses a certain publication bias.
On the other hand, the strengths of this study are (1) the clear data extraction protocol, (2) the well-specified inclusion-exclusion criteria, (3) the search in three different databases, (4) the quality assessment of the included studies, and (5) the detailed presentation of the results of data extraction and analysis.
Conclusion
This systematic review and meta-analysis identified 17 unique peer-reviewed studies of LSG and OAGB procedures with patient outcome data. These studies suggest that OAGB is associated with shorter mean hospital stay, increased %EWL in 1 year, greater remission of T2D, dyslipidemia, HTN, and OSAS, along with fewer cases of bile reflux disease, revisions, and lower mortality. On the other hand, LSG resulted to fewer cases of malnutrition and marginal ulcer. These results should be interpreted with caution due to the small number of randomized controlled studies. Future studies with greater clarity in significant outcomes, as in complications and %EWL, are necessary to demonstrate the differences in efficacy between LSG and OAGB.
References
Colquit JL, Picot J, Loveman E, et al. Surgery for obesity. Cochrane Database Syst Rev. 2009;2:CD003641.
Magouliotis DE, Tasiopoulou VS, Sioka E, et al. Impact of bariatric surgery on metabolic and gut microbiota profile: a systematic review and meta-analysis. Obes Surg. 2017; doi:10.1007/s11695-017-2595-8.
Kueper MA, Kramer KM, Kirschniak A, et al. Laparoscopic sleeve gastrectomy: standardized technique of a potential standalone bariatric procedure in morbidly obese patients. World J Surg. 2008;32(7):1462–5.
Magouliotis DE, Tasiopoulou VS, Sioka E, et al. Robotic versus laparoscopic sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis. Obes Surg. 2017;27:245. doi:10.1007/s11695-016-2444-1.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Mahawar KK, Jennings N, Rown J, et al. “Mini” gastric bypass: systematic review of a controversial procedure. Obes Surg. 2013;23(11):1890–8.
Rutledge R. The mini-gastric bypass: experience with the 1,274 cases. Obes Surg. 2001;11:276–80.
Wang HH, Wei PL, Lee YC, et al. Short-term results of laparoscopic mini-gastric bypass. Obes Surg. 2005;15:648–54.
Noun R, Zeidan S. Laparoscopic mini-gastric bypass: an effective option for the treatment of morbid obesity. J Chir (Paris). 2007;144:301–4.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011. Available from www.cochrane-handbook.org.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
GSE HJ. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. 2011.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-en-Y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg. 2015; doi:10.1007/s11695-015-1869-2.
Kansou G, Lechaux D, Delarue J, et al. Laparoscopic sleeve gastrectomy versus laparoscopic mini gastric bypass: one year outcomes. Int J Surg. 2016;33:18–22. doi:10.1016/j.ijsu.2016.07.051.
Kular KS, Manchanda N, Rutledge R. Analysis of the five-year outcomes of sleeve gastrectomy and mini gastric bypass: a report from the indian sub-continent. Obes Surg. 2014; doi:10.1007/s11695-014-1264-4.
Lee WJ, Chong K, Lin YH, et al. Laparoscopic sleeve gastrectomy versus single anastomosis (mini-) gastric bypass for the treatment of type 2 diabetes mellitus: 5-year results of a randomized trial and study of incretin effect. Obes Surg. 2014;24:1552–62. doi:10.1007/s11695-014-1344-5.
Madhok B, Mahawar KK, Boyle M, et al. Management of super-super obese patients: comparison between mini (one anastomosis) gastric bypass and sleeve gastrectomy. Obes Surg. 2016; doi:10.1007/s11695-016-2181-5.
Milone M, Lupoli R, Maietta P, et al. Lipid profile changes in patients undergoing bariatric surgery: a comparative study between sleeve gastrectomy and mini-gastric bypass. Int J Surg. 2015;14:28–32. doi:10.1016/j.ijsu.2014.12.025.
Musella M, Apers J, Rheinwalt K, et al. Efficacy of bariatric surgery in type 2 diabetes mellitus remission: the role of mini gastric bypass/one anastomosis gastric bypass and sleeve gastrectomy at 1 year of follow-up. A European survey. Obes Surg. 2015; doi:10.1007/s11695-015-1865-6.
Plamper A, Lingohr P, Nadal J, et al. Comparison of mini-gastric bypass with sleeve gastrectomy in a mainly super-obese patient group: first results. Surg Endosc. 2016; doi:10.1007/s00464-016-5085-5.
Seetharamaiah S, Tantia O, Goyal G, et al. LSG vs OAGB—1 year follow-up data—a randomized control trial. Obes Surg. 2016; doi:10.1007/s11695-016-2403-x.
Tolone S, Cristiano S, Savarino E, et al. Effects of omega-loop bypass on esophagogastric junction function. Surg Obes Relat Dis. 2015; doi:10.1016/j.soard.2015.03.011.
Alexandrou A, Michalinos A, Athanasiou A, et al. Laparoscopic sleeve gastrectomy for morbid obesity with intra-operative endoscopy: lessons we learned after 100 consecutive patients. Obes Surg. 2015;25:1223–8. doi:10.1007/s11695-014-1524-3.
Carbajo MA, Fong-Hirales A, Luque-de-Leon E, et al. Weight loss and improvement of lipid profiles in morbidly obese patients after laparoscopic one-anastomosis gastric bypass: 2-year follow-up. Surg Endosc. 2016; doi:10.1007/s00464-016-4990-y.
Chevallier JM, Arman GA, Guenzi M, et al. One thousand single anastomosis (omega loop) gastric bypasses to treat morbid obesity in a 7-year period: outcomes show few complications and good efficacy. Obes Surg. 2015; doi:10.1007/s11695-014-1552-z.
Felsenreich DM, Langer FB, Kefurt R, et al. Weight loss, weight regain and conversions to Roux-en-Y gastric bypass—10-year results of laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016; doi:10.1016/j.soard.2016.02.021.
Lessing Y, Pencovich N, Khatib M, et al. One-anastomosis gastric bypass: first 407 patients in 1 year. Obes Surg. 2017; doi:10.1007/s11695-017-2668-8.
Taha O, Abdelaal M, Abozeid M, et al. Outcomes of omega loop gastric bypass, 6-years experience of 1520 cases. Obes Surg. 2017; doi:10.1007/s11695-017-2623-8.
Mason EE, Ito C. Gastric bypass in obesity. Surg Clin N Am. 1967;47:1345–135.
Bruzzi M, Duboc H, Gronnier C, et al. Long-term evaluation of biliary reflux after experimental one-anastomosis gastric bypass in rats. Obes Surg. 2017; doi:10.1007/s11695-017-2577-x.
Bruzzi M, Rau C, Voron T, et al. Single anastomosis or mini-gastric bypass: long-term results and quality of life after a 5-year follow-up. Surg Obes Relat Dis. 2015;11:321–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Does not apply.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Rights and permissions
About this article
Cite this article
Magouliotis, D.E., Tasiopoulou, V.S., Svokos, A.A. et al. One-Anastomosis Gastric Bypass Versus Sleeve Gastrectomy for Morbid Obesity: a Systematic Review and Meta-analysis. OBES SURG 27, 2479–2487 (2017). https://doi.org/10.1007/s11695-017-2807-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2807-2