Abstract
Background
Currently, sleeve gastrectomy is most commonly performed laparoscopically. However, robot-assisted approach for sleeve gastrectomy is increasing in number among bariatric surgeons. The aim of our study is to compare perioperative outcomes of robot-assisted (RA-LSG) and laparoscopic sleeve gastrectomy (LSG).
Methods
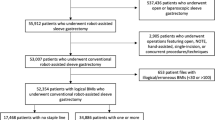
Between June 2008 and December 2014, 647 patients underwent LSG and RA-LSG at our institution. A retrospective review was performed for 379 LSG and 268 R-LSG patients, noting the outcomes and complications of the procedure.
Results
The first 100 LSG and RA-LSG cases were separated to reflect the influence of learning curve. Mean length of hospital stay (LOS) was longer in RA-LSG patients at 1.3 ± 0.6 days (range, 1–4), while it was 1.1 ± 0.3 days (range, 1–2) in LSG patients. Thirty-day readmission rate was similar in both groups, 5.0 % in LSG and 6.0 % in RA-LSG group. One mortality (1.0 %) occurred in the RA-LSG group. In patients after 100 cases, mean LOS was still longer in RA-LSG patients at 1.7 ± 1.8 days (range, 1–21), while it was 1.2 ± 0.5 days (range, 1–5) LSG patients. Thirty-day readmission rate and 30-day reoperation rate did not show a significant difference between the two groups. Overall leak rate was 3.2 % (n = 9) in LSG group, and 1.9 % (n = 5) in RA-LSG group, and the difference was not statistically significant.
Conclusions
Our study showed similar 30-day readmission and reoperation rate between LSG and RA-LSG during the learning curve and after the proficiency has been achieved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the continued rise of obesity and its related comorbid conditions, bariatric surgery remains the therapeutic mode with the highest rate of sustainable weight loss and comorbidity resolution [1, 2]. Among the procedures available today to bariatric surgeons, laparoscopic sleeve gastrectomy (LSG) has recently become increasingly performed as a primary weight loss surgery for new patients, and this trend appears to be continuing [3]. LSG became the most commonly performed bariatric surgery in the USA in 2013 [3]. Other advantages of LSG include near equivalent weight loss to gastric bypass and lower long-term complication rate [4–6]. As the field of bariatrics continues to evolve, new technologies are being introduced that have the potential to change current surgical practice. Among these is the da Vinci Surgical System (Intuitive Surgical, Sunnyvale, CA, USA). Use of this system, more frequently referred to as robotic surgery, gives surgeons advantages such as improved visualization and control through means of articulation and wrist movement [7, 8]. As new and innovative technology becomes available, we must always keep patient safety in mind. Advances such as this must not only continue to do no harm but also provide at least equivalent results in safety and outcomes to our patients. As such, the purpose of this study is to compare the learning curve and perioperative outcomes of da Vinci assisted LSG (RA-LSG) and LSG.
Methods and Materials
After Institutional Review Board approval and following the Health Insurance Portability and Accountability Act guidelines, the authors performed a retrospective chart review of a prospectively maintained database. This consisted of 647 patients who underwent RA-LSG and LSG from June 1, 2008, to December 31, 2014.
RA-LSG and LSG were performed by one surgeon according to the National Institutes of Health criteria for the surgical management of morbid obesity. The surgeon at our institution has been performing laparoscopic Roux-en-Y gastric bypass since 2001 and LSG since 2008 and had performed more than 4000 bariatric cases by 2012. Our surgeon adopted da Vinci assist robotic system (Intuitive Surgical, Sunnyvale, CA, USA) in June, 2012, with LSG procedures.
All patients attended an informational seminar hosted by the performing surgeon followed by a one-on-one physician evaluation. Routine bariatric workup was performed including psychological evaluation, laboratory work, nutritional evaluation, and medical clearance when appropriate. Imaging included chest X-ray and abdominal ultrasound in patients without history of prior cholecystectomy.
All data for age and body mass index (BMI) are demonstrated as mean ± standard deviation, unless otherwise noted. Statistical analysis was performed using descriptive analysis and two-tailed Student’s t test with p < 0.05 regarded as statistically significant.
Surgical Technique
Laparoscopic Sleeve Gastrectomy
Standardized technique was used for all patients. Abdominal access was gained by Veress needle in the left upper quadrant (LUQ) after which a 5-mm trocar is placed. Under direct vision, four further trocars were placed, two 12-mm trocars, one at umbilicus, and one in right midabdomen; and two 5-mm trocars, one in the right upper quadrant (RUQ), one in the epigastrium used for the liver retractor. The gastrocolic ligament was then dissected away from the greater curvature of the stomach starting 4–5 cm from the pylorus and continuing proximally to the angle of His taking down the short gastric vessels. During this dissection, all posterior attachments to the stomach were taken down and the fundus was completely dissected to the left crus. At this point, we assessed for hiatal hernia and if present, it was laparoscopically repaired. This was completed by opening the pars flacida and dissecting superiorly along the right crus taking down the phreno-esophageal ligament as we continued superior and laterally. We then dissected the esophagus from the hiatus until the left crus was visualized, following which the hiatal defect was repaired posteriorly with a nonabsorbable suture. A 34 French (Fr)-sized Edlich tube (Covidien, Mansfield, MA, USA) was advanced toward pylorus as a bougie dilator, and stomach transection was started with a 45-mm linear stapler followed by series of 60-mm stapler loads. After complete transection, the staple line was reinforced with a 2–0 Vicryl suture with a running stitch from the upper portion of the staple line to the apex, and a series of interrupted figure of eight stitches at all distal staple junction points (imbricated oversewing of the most proximal staple line, then in between junction points). An air leak test was performed, and drain was placed, following which the transected stomach was withdrawn through the umbilical incision. If a cholecystectomy or umbilical hernia repair was to be performed, it was completed after the sleeve portion of the procedure.
One laparoscopic procedure was converted to open due to extensive adhesions.
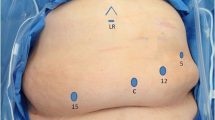
Robot-Assisted Laparoscopic Sleeve Gastrectomy
Abdominal access was gained with Veress needle in the LUQ after which an 8-mm trocar was placed. Under direct vision, five further trocars were placed. First, a long 12-mm trocar was placed at umbilicus to serve as camera port. Three further 8-mm trocars were placed, one in the RUQ along with one each in the right and left midabdomen. Lastly, a 5-mm trocar was placed in the epigastrium and used as the liver retractor. The da Vinci robot was then brought in and docked. The LSG was performed in an identical manner to the laparoscopic procedure as described above with dissection and suturing performed robotically while stapling was performed by a bedside assistant. At completion of the leak test, the robot was undocked, a drain was placed, and the transected stomach was removed from the umbilical incision. As in LSG, any concomitant procedures such as cholecystectomy or umbilical hernia repair were completed laparoscopically after completion of the sleeve portion of the procedure.
One robotic procedure was converted to laparoscopic due to a tear in the liver.
Postoperative Course
All patients were admitted to the bariatric floor of the hospital postoperatively. Patients remained nils per os overnight and were given a methylene blue dye oral challenge on postoperative day 1. If negative, a clear liquid diet was started and patients were discharged home once they were tolerating diet adequately. Patients were followed up at our office clinic at 1, 3, 6, and 12 months postoperatively and yearly thereafter. Follow-up visits included weight measurement, clinical history and examination, and laboratory tests for blood glucose, as well as nutrition deficiency.
Results
Out of 645 procedures, excluding two with a converted approach, 378 were LSG and 267 RA-LSG. Mean age was 44.1 ± 11.5 years (range, 17–71) in LSG patients, and 43.4 ± 11.9 years (range, 19–71) in RA-LSG patients at the time of operation. Preoperative BMI was 45.2 ± 7.6 kg/m2 (range, 33.8–83.2) in LSG patients and 46.7 ± 7.7 kg/m2 (range, 34.4–71.9) in RA-LSG patients. The number and distribution of comorbid conditions (hypertension, diabetes mellitus, hyperlipidemia, obstructive sleep apnea, and gastroesophageal reflux disease) were similar between the two groups (p > 0.14). Full demographic data is shown in Table 1.
Comparison of Initial 100 Patients
Mean length of hospital stay (LOS) was 1.1 ± 0.3 days (range, 1–2) in initial 100 LSG patients and 1.3 ± 0.6 days (range, 1–4) in initial 100 RA-LSG patients. The difference in LOS was significant between the two groups (p < 0.01) (Table 2).
Five (5.0 %) out of 100 initial LSG patients and six (6.0 %) out of 100 initial RA-LSG patients required a readmission within 30 days. Reasons for readmissions were staple line leakage (n = 2), abdominal pain (n = 1), fever (n = 1), and nausea/vomiting (n = 1) in LSG patients, and staple line leakage (n = 4), dehydration (n = 1), and intestinal bleeding (n = 1) in RA-LSG patients. Thirty-day readmission rate did not show significant difference between the two groups (p > 0.37). No patient in these groups required a reoperation within 30 days.
One mortality (1.0 %) occurred in the RA-LSG group. The patient had jogged more than 3 mi 10 days after the procedure, went to an outside hospital, and was found to have portal venous thrombosis. Low-molecular-weight heparin prophylaxis is not part of our postoperative protocol, and it is done only in high-risk patients. This patient did not receive the prophylaxis as he was not a high-risk patient. This patient had an operative time of 157 min at the time of RA-LSG, not significantly longer than other 100 initial RA-LSG patients. He expired 11 days following the index procedure.
Comparison After the Initial 100 Cases
Mean LOS was 1.2 ± 0.5 days (range, 1–5) in 278 LSG patients and 1.7 ± 1.8 days (range, 1–21) in 167 RA-LSG patients. Two patients in the LSG group and four in the RA-LSG group had longer than 3 days of hospital stay. In the LSG group, one patient was found to have a staple line leak on postoperative day (POD) 1 and underwent diagnostic laparoscopy with oversewing of the leak. One patient had an oozing from the Jackson-Pratt (JP) drain due to Lovenox administration. This patient required 6 units of pack red blood cells and was discharged after 5 days of hospital stay.
In the RA-LSG group, one patient had nausea and mild urinary retention, and therefore kept at the hospital for 4 days for observation. One patient showed severe small bowel obstruction in the upper gastrointestinal (UGI) study on POD 2 and was sent back to the operating room for diagnostic laparoscopy. She was found to have ileus without significant mechanical small bowel obstruction. Another patient developed a low-grade fever with turbid JP drain on POD 1, was sent back to the operating room for diagnostic laparoscopy, and had her staple line leak oversewed. The last patient developed a severe skin problem with hypotension, acute kidney injury, and leukocytosis on POD 2. He was diagnosed with Stevens-Johnson syndrome and was medically managed at the hospital for 21 days.
Thirty-day readmission rate was 2.2 % (n = 6) in the LSG group due to staple line leakage (n = 3), dehydration (n = 2), and clostridium difficile infection (n = 1). One patient with a leak required diagnostic laparoscopy with abscess drainage and oversewing of the leak, making 30-day reoperation rate 0.7 % (n = 2) in the LSG group. Thirty-day readmission rate was 2.4 % (n = 4) in the RA-LSG group due to nausea and vomiting (n = 2), pulmonary embolism (n = 1), and abdominal pain (n = 1). No patient required a reoperation, making 30-day reoperation rate 1.2 % (n = 2) in the RA-LSG group.
Comparison of Leak Rates
Overall leak rate was 3.2 % (n = 9) in the LSG group, and 1.9 % (n = 5) in the RA-LSG group, including leaks that were identified beyond 30 days of index procedure (p > 0.67). Of these, four occurred each within the initial 100 cases, making the leak rate 4.0 % in both groups. Leak rates in the latter groups were 1.8 % in the LSG group and 0.6 % in the RA-LSG group. The difference in the leak rate was significant in the RA-LSG group between the initial and latter cases (p < 0.05). However, no significance was observed in the LSG group (p > 0.22).
Discussion
When encountering new techniques in surgery, it is commonly found that there is a learning curve that must be overcome before full proficiency is reached. This must be factored in to the decision to add robotic surgery to bariatric procedures [9, 10]. Along with learning and adjusting for mechanical issues that come with docking and using the system, the change in exposure and need for different instruments can subtly change how procedures must be approached.
In reviewing current literature, there is no established number of cases to account for this curve in robotic bariatric surgery; however, various numbers have been proposed. It has been shown prior that robotic surgery can decrease the learning curve of a procedure when compared to the laparoscopic equivalent [10, 11]. When looking at LSG, Zacharoulis et al. [12] proposed that proficiency required 68 cases. Vilallonga et al. [9] identified a learning curve of approximately 20 cases on the use of RA-LSG procedures performed by experienced bariatric surgeons. In a retrospective study of 134 consecutive LSG by Romero et al. [13], they found similar results with experienced bariatric surgeons developing decreased operative times following approximately 25 cases. In both studies, there were no significant differences in complications or operative blood loss despite relatively large sample sizes.
In the current study, a more conservative number of 100 cases was chosen and compared between laparoscopic and robot-assisted laparoscopic cases. Thirty-day readmission rates were 5.0 and 6.0 % in LSG and RA-LSG cases during the learning curve, respectively. The readmission rate decreased to 2.2 and 2.4 % after 100 cases; however, the difference was not statistically significant. Although RA-LSG patients had a longer mean LOS than LSG patients, 30-day readmission and reoperation rate was similar during the learning curve between the two approaches.
LSG continues to increase in popularity; part of this is due to the conception of lower short- and long-term risk when compared to other bariatric procedures [4–6]. Despite this safety profile, there remain complications with any procedure and the key complication of concern in LSG is leaks [14–16]. Due to the long continuous staple line the procedure results in, there is a large potential surface area for staple line disruption and leak. However, it has been repeatedly found that most leaks occur high on the gastroesophageal junction portion of the staple line [17, 18]. This was consistent with our findings, as all our leaks occurred in this area. Overall leak rates for SG continue to evolve as more procedures are performed, and we obtain increasing follow-up data on patients. A recent meta-review by Parikh et al. [19] looked at the number of leaks found in 8922 patients resulting in a leak rate of 2.2 %. Our overall leak rate in the patients reviewed in this study was 2.2 % despite the learning curve for both LSG and RA-LSG procedures. Our leak rate dropped to 1.1 % when we excluded the initial 100 patients from each group.
No obvious factor was identified to account for the difference in leak rate between LSG and RA-LSG patients. Technically, the procedure was performed identically in relation to points of dissection and transection. A difference does exist in that during RA-LSG, stapling is performed by the bedside assistant, whereas in LSG the performing surgeon handles the stapler. This is countered by improved control over retraction and positioning the surgeon has in RA-LSG. Although there is no tactile feedback for the surgeon at the time of firing, a surgeon should be able to recognize the thickness of the stomach by looking at the monitor after some experience with robots just as with laparoscopic procedures. Therefore, we do not think that it is necessary for the surgeon to fire the stapler due to the fear of mismatch of staple height and stomach thickness. This is backed by our significant decrease in leak rate in the RA-LSG group after the initial 100 cases. Other common factors noted in sleeve leaks include bougie dilator size, with increasing leak rate as size decreases below 40 Fr [18]. Although we used a smaller sized dilator (34 Fr), this was uniform between the two groups and should not have affected the comparative leak rate. We should note that our surgeon started performing LSG before RA-LSG, and therefore, the learning curve for LSG reflects the entire surgical technique while the learning curve for RA-LSG only reflects the new surgical approach with the da Vinci system. This may have accounted for higher leak rate in LSG group after the 100 cases, as three out of five leaks in the latter group occurred during the next set of 100 cases. Of note on the cost, RA-LSG cases had about a 15 % higher cost over LSG cases.
There are several limitations to the findings of our study. The learning curve we identified represents the results for a single, experienced bariatric surgeon. Our study results are therefore difficult to extrapolate to new trainees and are better served for practicing laparoscopic bariatric surgeons seeking to learn robotic-assisted procedures. Finally, this study represents a retrospective observational acquisition of data which is associated with traditional biases such as recall and selection bias. In addition, although not directly a limitation to the results presented, a cost analysis was not able to be performed and this information would certainly be useful in further comparing the positives and negatives between the two procedures.
Despite our limitations, we believe that this study is one of few literatures that include both initial cases of LSG and RA-LSG, with a significant number of procedures.
Conclusion
Robotic-assisted sleeve gastrectomy is a new and evolving technique in bariatric surgery that has been shown previously to be safe as the laparoscopic procedure. Although the mean LOS was longer in the RA-LSG group when compared to that of LSG group, our study showed similar 30-day readmission and reoperation rate between LSG and RA-LSG during the learning curve and after the proficiency has been achieved. The overall leak rate significantly decreased after 100 cases in the RA-LSG group.
References
Colquit JL, Picot J, Loveman E, et al. Surgery for obesity. Cochrane Database Syst Rev. 2009;(2):CD003641.
Pontiroli AE, Morabito A. Long-term prevention of mortality in morbid obesity through bariatric surgery. A systemic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg. 2011;253:484–7.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Iannelli A, Dainese R, Piche T, et al. Laparoscopic sleeve gastrectomy for morbid obesity. World J Gastroenterol. 2008;14:821–7.
Braghetto I, Csendes A, Lanzarini E, et al. Is laparoscopic sleeve gastrectomy an acceptable primary bariatric procedure in obese patients? Early and 5-year postoperative results. Surg Laparosc Endosc Percutan Tech. 2012;22:479–86.
Aggarwal S, Kini S, Herron D. Laparoscopic sleeve gastrectomy for morbid obesity: a review. Surg Obes Relat Dis. 2007;3:189–94.
Moser F, Horgan S. Robotically assisted bariatric surgery. Am J Surg. 2004;188(Supp):38S–44.
Diamantis T, Alexandrou A, Nikiteas N, et al. Initial experience with robotic sleeve gastrectomy for morbid obesity. Obes Surg. 2011;21:1172–9.
Vilallonga R, Fort JM, Gonzalez O, et al. The initial learning curve for robot assisted sleeve gastrectomy: a surgeon’s experience while introducing the robotic technology in a bariatric surgery department. Minim Invasive Surg Nurs. 2012;2012:347131.
Cirocchi R, Boselli C, Santoro A, et al. Current status of robotic bariatric surgery: a systemic review. BMC Surg. 2013;13:53.
Yu SC, Clapp BL, Lee MJ, et al. Robotic assistance provides excellent outcomes during the learning curve for laparoscopic Roux-en-Y gastric bypass: results from 100 robotic-assisted gastric bypasses. Am J Surg. 2006;192:746–9.
Zacharoulis D, Sioka E, Papamargaritis D, et al. Influence of the learning curve on safety and efficiency of laparoscopic sleeve gastrectomy. Obes Surg. 2012;22:411–5.
Romero RJ, Kosanovic R, Rabaza JR, et al. Robotic sleeve gastrectomy: experience of 134 cases and comparison with a systematic review of the laparoscopic approach. Obes Surg. 2013;23:1743–52.
Aggarwal S, Sharma AP, Ramaswamy N. Outcome of laparoscopic sleeve gastrectomy with and without staple line oversewing in morbidly obese patients: a randomized study. J Laparoendosc Adv Surg Tech A. 2013;23:895–9.
Deitel M, Gagner M, Erickson AL, et al. Third International summit: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2011;7:749–59.
Thompson 3rd CE, Ahmad H, Lo Menzo E, et al. Outcomes of laparoscopic proximal gastrectomy with esophagojejunal reconstruction for chronic staple line disruption after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014;10:455–9.
Dapri G, Vaz C, Cadiere GB, et al. A prospective randomized study comparing two different techniques for laparoscopic sleeve gastrectomy. Obes Surg. 2007;17:1435–41.
Chour M, Alami RS, Sleilaty F, et al. The early use of Roux limb as surgical treatment for proximal postsleeve gastrectomy leaks. Surg Obes Relat Dis. 2014;10:106–10.
Parikh M, Issa R, McCrillis A, et al. Surgical strategies that may decrease leak after laparoscopic sleeve gastrectomy: a systematic review and meta-analysis of 9991 cases. Ann Surg. 2013;257:231–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rena C. Moon, Derek Stephenson, Nelson A. Royall, Andre F. Teixeira, and Muhammad A. Jawad have no commercial associations that might be a conflict of interest in relation to this article. Andre F. Teixeira is a consultant of Intuitive Surgical.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Does not apply.
Rights and permissions
About this article
Cite this article
Moon, R.C., Stephenson, D., Royall, N.A. et al. Robot-Assisted Versus Laparoscopic Sleeve Gastrectomy: Learning Curve, Perioperative, and Short-Term Outcomes. OBES SURG 26, 2463–2468 (2016). https://doi.org/10.1007/s11695-016-2131-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2131-2