Abstract
Introduction
Sleeve gastrectomy has gained popularity over the past decade due to its safety, feasibility, and good results. The purpose of this study is to describe our results, both short and long term, with this procedure.
Material and Methods
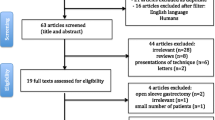
This study is a nonrandomized, controlled, retrospective review of 409 patients who underwent a minimally invasive sleeve gastrectomy at the University of Illinois Hospital and Health System from January 2008 to December 2013. A total of 304 patients underwent a laparoscopic sleeve gastrectomy, and another 105 patients underwent a robotic procedure using the da Vinci Surgical System®. Patient demographics, comorbidities, date of surgery, postoperative morbidity and mortality, operating time, length of stay, and excess weight loss were reviewed.
Results
The mean age was 41 years (18–70) with no statistical difference between the two groups. Patient’s demographics were similar (p = 0.395) in both groups. The mean operative time for the robotic group was 110.6 versus 84.18 min in the laparoscopic group, which was statistically significant (p < 0.05). There were no significant differences between the two groups with regard to the perioperative complications, length of stay, or % excess weight loss.
Conclusion
There is no significant difference between the robotic and laparoscopic group in terms of complications, length of stay, and estimated blood loss. Robot-assisted sleeve gastrectomy is associated with longer operative time and increased cost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a global health problem [1] with one quarter of the adult world population currently considered obese [2]. In the USA alone, more than one third of the population is defined as obese [3]. There are differing comorbidities associated with obesity, including hypertension, diabetes, and dyslipidemia [2, 4–8]. Likewise, a variety of methods are promoted to induce weight loss in adults, including diet [9, 10], exercise, and medication [11, 12] but with poor long-term results leading to weight loss and comorbidity improvement [13].
Bariatric surgery has been shown to produce greater efficacy than lifestyle modifications or medical management for the reduction of comorbid medical conditions [14]. In fact, this is a field that has advanced considerably with the development of newer techniques, modification of standard procedures, and the use of robotic technology. Laparoscopic sleeve gastrectomy (LSG) has increased in popularity over the past decade due to its safety and feasibility [15–18] and is currently performed as a single-stage procedure with good outcomes [4].
The International Sleeve Gastrectomy Expert Panel Consensus Statement [5] showed 90 % of the panelists in agreement that LSG is both valid as a stand-alone procedure and as a bridge to reduce perioperative risk in patients who are considered high risk and morbidly obese. In terms of outcome, combined data from 12,799 LSG procedures showed an average length of hospital stay of 2.5 days (SD = 0.93), a conversion rate of 1.05 % (SD = 1.85), a 1.06 % leak rate, and a 0.35 % stricture rate, with a postoperative gastroesophageal reflux rate of 12.11 % (SD = 8.97) [5]. Consequently, LSG has been proposed as an effective alternative to laparoscopic Roux-en-Y gastric bypass and is associated with a relatively shorter operating time and fewer complications, with comparable clinical outcomes [4, 19–24]. Many other studies have demonstrated that LSG is a safe and feasible technique resulting in a short operating time and short length of hospitalization [25]. Still, postoperative complications associated with LSG have been reported, including leaks and bleeding [26]. Long-term risks include strictures and gastroesophageal reflux [27]. Of note, there have been many recent technologic advances in new staples and new reinforcing materials that could serve to increase the safety of this procedure.
Robotic technology has also been proven to be effective in very complex abdominal cases such as Whipple procedures and extended pancreatectomies [28], liver resections [29], and achalasia [30]. It has also proven useful in revision surgeries or in patients with previous abdominal surgeries, when lyses of adhesions and a precise dissection are required [31]. Initially, the robotic approach was used in the bariatric field for biliopancreatic diversion with duodenal switch, as described by Sudan and colleagues in 2007 [32], and for gastric bypass where the leak rate and conversion to open rate was 0 % [33–36].
According to Romero et al. [37], the ability to control these factors using the robot has led to decreased postoperative complications. It is also important to note, however, that robotic-assisted sleeve gastrectomy (RASG) is also associated with an increase in cost and/or time involved with the procedure [37, 38].
Many reports have been published in the literature comparing the robotic sleeve gastrectomy approach with the laparoscopic approach and have shown better results with the RASG. The objective of this study is to report our technique and outcomes associated with the minimally invasive sleeve gastrectomy.
Materials and Methods
This study is a retrospective review of a prospectively maintained database with 409 patients who underwent either a laparoscopic or robot-assisted sleeve gastrectomy by two board certified surgeons at the University of Illinois Hospital and Health Sciences System between January 2008 and December 2013. This study was conducted under Institutional Review Board approval. Two experienced laparoscopic surgeons with over 400 laparoscopic bariatric procedures performed the surgeries.
All patients met the standard eligibility criteria for bariatric surgery. Specifically, following the National Institutes of Health criteria, patients had either a body mass index (BMI) greater than 35 kg/m2 with weight loss recalcitrant to nonsurgical measures with two or more comorbidities or a BMI ≥40 kg/m2 with no comorbidities [39]. Data obtained from the electronic medical records (EMR) of the University of Illinois Hospital and Health Sciences System included age, gender, height, weight, BMI, date of birth, date and type of surgery, length of surgical procedure, size of bougie used, length of hospitalization, postoperative complications, and % excess weight loss (% EWL) at 3, 6, 9, 12, 18, 24, 36, and >36 months. Data on comorbidities including hypertension, type 2 diabetes, gastroesophageal reflux disease (GERD), dyslipidemia, and sleep apnea were also obtained via the EMR.
At the beginning of our experience, patients with BMI over 50 kg/m2 were selected to undergo a robotic approach. Later in our experience, patients with BMI <50 kg/m2 were also included according to surgeons’ preferences.
Preoperative Evaluation
Patients received a bariatric preoperative evaluation and were evaluated by the bariatric surgery team to determine eligibility. Cardiologists, pulmonologists, and endocrinologists were involved if patients presented with any pertinent risk factors.
Laparoscopic Surgical Technique
For the laparoscopic approach, trocars were placed as shown in Fig. 1. The short gastric vessels were divided 5 cm from the pylorus, all the way up to the gastroesophageal junction using the laparoscopic vessel sealing Caiman® device (Aesculap Inc, Center Valley, PA). Once the greater curvature was completely mobilized, a 36-, 38-, or 40-French bougie was introduced to tailor the sleeve. The size of the bougie was based on the surgeon’s level of experience and preference. Next, the stomach was transected and disconnected from the greater curvature starting 6 cm from the pylorus and using multiple staples reloads. The stapler reloads were reinforced using Gore Seamguard® (WL Gore & Associates Inc, Flagstaff, AZ). Finally, an upper gastrointestinal endoscopy was performed in order to control stricture, intragastric bleeding, and leaks.
Robot-Assisted Surgical Technique
For the robotic approach, trocars were placed as shown in Fig. 2. The initial steps for setting up the RASG were similar to the LSG approach. The robot was docked cranially. Using the robotic harmonic shears, the vascular supply of the greater curvature of stomach was taken down starting about 5 cm from the pylorus and all the way up to the left crus. Once the greater curvature was completely mobilized, a 40-French bougie was introduced to tailor the sleeve. It was the surgeon’s preference to use a 40-French bougie in the robotic approach. Next, the stomach was transected and disconnected from the greater curvature, starting 6 cm from the pylorus using multiple staples reloads. The stapler reloads were reinforced using Gore Seamguard®. An upper gastrointestinal endoscopy was also performed in this approach, in order to rule out stricture, intragastric bleeding, and leaks.
Postoperative Management
Patients started mobilization within a few hours of the procedures. On postoperative day 1, an oral tolerance trial was performed and most patients were discharged on postoperative day 2.
Statistical Analysis
Data analyses was conducted using SPSS 19.0 (IBM, SPSS Statistics). Comparisons between the groups were performed using Student’s t test for continuous variables and Fischer’s test for discrete variables. Confidence intervals were set at 95 %, and a two-sided p value of <0.05 was considered statistically significant.
Results
Demographics and Medical Characteristics
As described in Table 1, data was collected from 339 women (83.7 %) and 70 men (16.3 %). The mean age was 41 years (range 18–70). There was no statistical difference between the two groups in terms of age (p = 0.656), but there was a significant difference in gender between the groups (p < 0.5). In terms of comorbidities, 50.6 % of patients had hypertension, 34.7 % had type 2 diabetes, 32.2 % had sleep apnea, 21.7 % had GERD, 21.5 % had dyslipidemia, 17.95 % had asthma, and 7.45 % had hypothyroidism. Patient demographics were similar between the two groups (2.66 vs. 2.62, respectively; p = 0.864). Of those patients with a BMI >50 kg/m2, 48 underwent RASG and 169 underwent LSG.
Perioperative and Postoperative Results
Table 2 summarizes the perioperative and postoperative results. There were 105 RASG and 304 LSG procedures performed. The mean operative time in the RASG group was longer than the LSG group (110.6 min vs. 84.1 min), which was statistically significant (p < 0.05). With regard to bougie sizes, a 40-French bougie was used in 99 % of the RASG procedures, while in the LSG group, either 36- or 38-French bougies were used in 88.8 % of the cases (Table 2). As it relates to %EWL, for those who had a 40-Fr bougie used, the mean %EWL at 24 months follow-up was 43 %; while those who had a 36- or 38-French bougie used, the mean %EWL was 61 % (p < 0.05). At 36 and >36 months follow-up, the %EWL was significantly greater for the 36–38-Fr bougie group (Table 5).
Comparing % EWL at different times follow-up with patients using only 40-Fr bougie in the robotic versus laparoscopic approach, there were no significant differences between both groups (Table 6).
A hiatal hernia repair was performed in the LSG group in 45.7 % of patients as compared to 7.6 % in the RASG. This was statistically significant (p < 0.01) (Table 2). Hiatal hernia repair was not performed systematically; it was performed according to surgeons’ preferences.
In the patients classified as super obese (BMI >50 kg/m2), the mean operative time (OR) was shorter for the RASG (129 min vs. 143 min), although it was not statistically significant (Table 3). There were two complications in the laparoscopic group: one patient who presented with intraoperative bleeding that required an emergency splenectomy and another patient who had a suture leak on postoperative day 5 that required reoperation, drainage, and a stent placement. The patient recovered without any further consequences. The robotic group had no complications. The mortality rate in both groups was 0 % (Table 3). There was no significant difference in length of hospital stay. The robotic group’s stay was half a day shorter than the laparoscopic group (2.44 vs. 3.07; p > 0.62) (Table 2). Finally, no differences were noted in terms of %EWL and BMI at 3 months, 6 months, 9 months, 1 year, 2 years, and 3 years between the two groups. The mean BMI decrease was similar in both groups (Table 4) (Fig. 3).
Discussion
While LSG has long been considered a low-risk procedure with good results in terms of weight loss and comorbidity improvements, robotic surgery is gaining popularity in the bariatric and other fields. The robot was initially used for gastric bypass and biliopancreatic diversion, resulting in 0 % conversion and leak rates [35, 40]. It has more recently been used for sleeve gastrectomy.
RASG is particularly advantageous in the super morbidly obese cohort [15, 41, 42] and in patients with previous and extensive surgeries such as liver transplant [16], as reported by Elli and colleagues who demonstrated a better approach to adhesiolysis using the robot. Still, there is no clear identification of the best indications for use of the robotic system. In our experience with two similar groups of patients (LSG vs. RASG), we found that in the robotic group, there were no leaks, conversions, or postoperative complications, while in the laparoscopic group, there were no conversions, no mortality, and a low postoperative complication rate of 0.65 %.
Romero and colleagues compared their robotic experience (134 cases) with previously published data from 3148 LSG cases and found decreased complication rates for their robotic group. Specifically, they reported a leak rate of 0 % compared to 1.97 % in the LSG group (p = 0.101), a stricture rate of 0 % compared to 0.43 % in the LSG group (p = 0.447), a bleeding rate of 0.70 % compared to 1.21 % in the LSG group (p = 0.594), and a mortality rate of 0 % compared to 0.10 % in the LSG group (p = 0.714) [37]. It is important to note, however, that this was in part due to the sample sizes compared. In our experience and that of Romero et al., the number of patients is significantly higher for the LSG group, which may partially explain the higher numbers of complications in that group.
The operative time also appears to be a factor directly related to use of the robotic approach. In our sample, there was a significant difference in the mean operating time between the RASG and LSG (110.67 and 84.18 min, respectively). Our mean operative time was 110.67 min which is longer than that reported by other authors, including Vilallonga (108 min) [43], Romero (106 min) [37], and Diamantis (95.5 min) [42]. The robotic system also requires more instrumentation, specialized nursing, and larger operating rooms.
In the laparoscopic group, the mean operating time was 84.18 min which is shorter than that reported by Trastulli (106.5 min) [44] and Vilallonga (96.18 min) [43], even when taking patients with associated procedures into consideration (hiatal hernia in 45.7 % of LSG cases). It is also important to mention that the prevalence of hiatal hernia in the morbidly obese is nearly 40 % [45], suggesting that surgeons should evaluate whether patients need to have a hiatal hernia repair at the same time of sleeve gastrectomy, particularly if the patient has previous GERD symptoms [46–48]. In the robotic group, another factor that could explain a longer operative time was related to the fact that it was used as a surgical training model, clinical fellows and residents were involved in performing the operation partially or completely increasing times.
Romero et al. [37] reported a length of stay in the robotic group of 2.2 days compared to 3.3 days in the systematic review (p = <0.005). Other groups have reported lengths of stay of 4 days [42] while other studies make no mention of stay [15, 49]. In our study, we found a difference of only half day shorter in the robotic group’s length of stay. Also in our study, the mean %EWL was similar in both groups. In the robotic group, the mean %EWL at 1 year was 48.89 % versus 52.23 % in the laparoscopic group (Table 4). These results are similar to Romero et al. [37] who reported a 57.2 % EWL at 12 months post-surgery.
Interestingly, different bougie sizes were used for each group and did seem to play a role in determining %EWL (Table 5). In the robotic group, a 40-French bougie was used while in the laparoscopic group, either a 36- or 38-French bougie was used. There were no significant differences between the two groups during the first 2 years of follow-up; however, long-term results after 2 years have shown statistical differences between the different bougie sizes in terms of %EWL (Table 5). The differences between 40-Fr bougies and 38- or 36-Fr bougies in %EWL started at 24 months follow-up. This is the time when the major differences in %EWL are reached with smaller bougie (i.e., at 24, 36, and >36 months follow-up smaller bougies have greater %EWL compared to the 40-Fr bougie group). Considering only patients using 40-Fr bougie, there were no significant differences in %EWL comparing robotic versus laparoscopic approach (Table 6)
This is an important result to consider because there is currently no consensus as to which bougie size is best for sleeve gastrectomy, regardless of approach [50]. Parikh et al. [51] reported no differences in %EWL at 36 months follow-up among patients who had different size bougies used during their procedures. Likewise, other authors [50] have reported no difference in %EWL among bougie sizes, though they did report that bougies 40-French and larger were associated with a leak rate of 0.92 %, as compared to 2.67 % for smaller bougies [49, 50]. In this study, there was no difference in leak rate among the different bougie sizes used.
As described by Vilallonga and Markar [43, 52] the cost of the robotic procedure is higher than the laparoscopic procedure, though cost was not a variable that was measured in this study.
Lastly, the mean operative time in the RASG group was shorter for the super obese patients than for those in the laparoscopic group, though it was not a statistical difference (129 vs. 143 min). In our experience, the robot seems to be useful for patients who were classified as super obese, with BMI >50 kg/m2, by decreasing the “torque effect” and technical limitations of a thick abdominal wall.
Conclusion
In conclusion, the results from this study reveal that there is no clear clinical advantage for RASG versus LSG. It is also associated to longer operative time in the RASG.
Future studies would be valuable using larger sample sizes to compare the effectiveness and long-term outcomes of the RASG procedure.
References
Gill TP, Antipatis VJ, James WP. The global epidemic of obesity. Asia Pac J Clin Nutr. 1999;8(1):75–81.
Kelly T, Yang W, Chen CS, et al. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond). 2008;32(9):1431–7.
Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity among adults: United States, 2011–2012. NCHS Data Brief. 2013;(131):1–8.
Chopra A, Chao E, Etkin Y, et al. Laparoscopic sleeve gastrectomy for obesity: can it be considered a definitive procedure? Surg Endosc. 2012;26(3):831–7.
Rosenthal RJ, International Sleeve Gastrectomy Expert Panel, Diaz AA, et al. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8(1):8–19.
Kashyap SR, Gatmaitan P, Brethauer S, et al. Bariatric surgery for type 2 diabetes: weighing the impact for obese patients. Cleve Clin J Med. 2010;77(7):468–76.
Fischer L, Hildebrandt C, Bruckner T, et al. Excessive weight loss after sleeve gastrectomy: a systematic review. Obes Surg. 2012;22(5):721–31.
Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Langeveld M, de Vries JH. [The mediocre results of dieting]. Ned Tijdschr Geneeskd. 2013;157(29):A6017.
Switzer NJ, Mangat HS, Karmali S. Current trends in obesity: body composition assessment, weight regulation, and emerging techniques in managing severe obesity. J Interv Gastroenterol. 2013;3(1):34–6.
Amorim Adegboye AR, Linne YM. Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst Rev. 2013;7, CD005627.
Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA. 2014;311(1):74–86.
Kissler HJ, Settmacher U. Bariatric surgery to treat obesity. Semin Nephrol. 2013;33(1):75–89.
Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f5934.
Ayloo S, Buchs NC, Addeo P, et al. Robot-assisted sleeve gastrectomy for super-morbidly obese patients. J Laparoendosc Adv Surg Tech A. 2011;21(4):295–9.
Elli EF, Masrur MA, Giulianotti PC. Robotic sleeve gastrectomy after liver transplantation. Surg Obes Relat Dis. 2013;9(1):e20–2.
Sammour T, Hill AG, Singh P, et al. Laparoscopic sleeve gastrectomy as a single-stage bariatric procedure. Obes Surg. 2010;20(3):271–5.
Mognol P, Chosidow D, Marmuse JP. Laparoscopic sleeve gastrectomy (LSG): review of a new bariatric procedure and initial results. Surg Technol Int. 2006;15:47–52.
Guzmán S, Manrique M, Raddatz A, et al. Results of bariatric surgery. Experience over 18 years. Rev Med Chil. 2013;141(5):553–61.
Peterli R, Borbély Y, Kern B, et al. Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg. 2013;258(5):690–5.
Daskalakis M, Weiner RA. Sleeve gastrectomy as a single-stage bariatric operation: indications and limitations. Obes Facts. 2009;2 Suppl 1:8–10.
Sabbagh C, Verhaeghe P, Dhahri A, et al. Two-year results on morbidity, weight loss and quality of life of sleeve gastrectomy as first procedure, sleeve gastrectomy after failure of gastric banding and gastric banding. Obes Surg. 2010;20(6):679–84.
Quesada BM, Roff HE, Kohan G, et al. Laparoscopic sleeve gastrectomy as an alternative to gastric bypass in patients with multiple intraabdominal adhesions. Obes Surg. 2008;18(5):566–8.
Sánchez-Santos R, Ruiz de Gordejuela AG, Gómez N, et al. [Factors associated with morbidity and mortality after gastric bypass. Alternatives for risk reduction: sleeve gastrectomy]. Cir Esp. 2006;80(2):90–5.
Vidal P, Ramón JM, Goday A, et al. Laparoscopic gastric bypass versus laparoscopic sleeve gastrectomy as a definitive surgical procedure for morbid obesity. Mid-term results. Obes Surg. 2013;23(3):292–9.
Mittermair R, Sucher R, Perathoner A. Results and complications after laparoscopic sleeve gastrectomy. Surg Today. 2013.
Rawlins L, Rawlins MP, Brown CC, et al. Sleeve gastrectomy: 5-year outcomes of a single institution. Surg Obes Relat Dis. 2013;9(1):21–5.
Giulianotti PC, Addeo P, Buchs NC, et al. Robotic extended pancreatectomy with vascular resection for locally advanced pancreatic tumors. Pancreas. 2011;40(8):1264–70.
Milone L, Daskalaki D, Fernandes E, et al. State of the art in robotic hepatobiliary surgery. World J Surg. 2013;37(12):2747–55.
Horgan S, Galvani C, Gorodner MV, et al. Robotic-assisted Heller myotomy versus laparoscopic Heller myotomy for the treatment of esophageal achalasia: multicenter study. J Gastrointest Surg. 2005;9(8):1020–9. discussion 1029–30.
Buchs NC, Pugin F, Azagury DE, et al. Robotic revisional bariatric surgery: a comparative study with laparoscopic and open surgery. Int J Med Robot. 2013. doi:10.1002/rcs.1549.
Sudan R, Puri V, Sudan D. Robotically assisted biliary pancreatic diversion with a duodenal switch: a new technique. Surg Endosc. 2007;21(5):729–33.
Ayloo SM, Addeo P, Buchs NC, et al. Robot-assisted versus laparoscopic Roux-en-Y gastric bypass: is there a difference in outcomes? World J Surg. 2011;35(3):637–42.
Snyder BE, Wilson T, Leong BY, et al. Robotic-assisted Roux-en-Y Gastric bypass: minimizing morbidity and mortality. Obes Surg. 2010;20(3):265–70.
Ayloo SM, Addeo P, Shah G, et al. Robot-assisted hybrid laparoscopic Roux-en-Y gastric bypass: surgical technique and early outcomes. J Laparoendosc Adv Surg Tech A. 2010;20(10):847–50.
Tieu K, Allison N, Snyder B, et al. Robotic-assisted Roux-en-Y gastric bypass: update from 2 high-volume centers. Surg Obes Relat Dis. 2013;9(2):284–8.
Romero RJ, Kosanovic R, Rabaza JR, et al. Robotic sleeve gastrectomy: experience of 134 cases and comparison with a systematic review of the laparoscopic approach. Obes Surg. 2013;23(11):1743–52.
Hagen ME, Pugin F, Chassot G, et al. Reducing cost of surgery by avoiding complications: the model of robotic Roux-en-Y gastric bypass. Obes Surg. 2012;22(1):52–61.
Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–9.
Myers SR, McGuirl J, Wang J. Robot-assisted versus laparoscopic gastric bypass: comparison of short-term outcomes. Obes Surg. 2013;23(4):467–73.
Cirocchi R, Boselli C, Santoro A, et al. Current status of robotic bariatric surgery: a systematic review. BMC Surg. 2013;13(1):53.
Diamantis T, Alexandrou A, Nikiteas N, et al. Initial experience with robotic sleeve gastrectomy for morbid obesity. Obes Surg. 2011;21(8):1172–9.
Vilallonga R, Fort JM, Caubet E, et al. Robotic sleeve gastrectomy versus laparoscopic sleeve gastrectomy: a comparative study with 200 patients. Obes Surg. 2013;23(10):1501–7.
Trastulli S, Desiderio J, Guarino S, et al. Laparoscopic sleeve gastrectomy compared with other bariatric surgical procedures: a systematic review of randomized trials. Surg Obes Relat Dis. 2013;9(5):816–29.
Che F, Nguyen B, Cohen A, et al. Prevalence of hiatal hernia in the morbidly obese. Surg Obes Relat Dis. 2013;9(6):920–4. doi:10.1016/j.soard.2013.03.013.
Daes J, Jimenez ME, Said N, et al. Laparoscopic sleeve gastrectomy: symptoms of gastroesophageal reflux can be reduced by changes in surgical technique. Obes Surg. 2012;22(12):1874–9.
Soricelli E, Casella G, Rizzello M, et al. Initial experience with laparoscopic crural closure in the management of hiatal hernia in obese patients undergoing sleeve gastrectomy. Obes Surg. 2010;20(8):1149–53.
Korwar V, Peters M, Adjepong S, et al. Laparoscopic hiatus hernia repair and simultaneous sleeve gastrectomy: a novel approach in the treatment of gastroesophageal reflux disease associated with morbid obesity. J Laparoendosc Adv Surg Tech A. 2009;19(6):761–3.
Abdalla RZ, Garcia RB, Luca CR, et al. Brazilian experience in obesity surgery robot-assisted. Arq Bras Cir Dig. 2012;25(1):33–5.
Yuval JB, Mintz Y, Cohen MJ, et al. The effects of bougie caliber on leaks and excess weight loss following laparoscopic sleeve gastrectomy. Is there an ideal bougie size? Obes Surg. 2013;23(10):1685–91.
Parikh M, Issa R, McCrillis A, et al. Surgical strategies that may decrease leak after laparoscopic sleeve gastrectomy: a systematic review and meta-analysis of 9991 cases. Ann Surg. 2013;257(2):231–7.
Markar SR, Penna M, Hashemi M. Robotic bariatric surgery: bypass, band and sleeve. Where are we now? And what is the future? Minerva Gastroenterol Dietol. 2012;58(3):181–90.
Acknowledgments
We thank our bariatric research team for guidance and patience.
Conflict of Interest
No grant funding was obtained for this study. The authors declare that they have no conflict of interest pertinent to the study.
Statement of Informed Consent
Informed consent for surgery was obtained from all individual participants included in the study before they underwent the procedure. As this is a retrospective analysis, formal consent is not required and an exempt application was approved by Institutional Review Board.
Statement of Human Rights
For this type of retrospective study, formal consent is not required and an exempt application was approved by Institutional Review Board.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elli, E., Gonzalez-Heredia, R., Sarvepalli, S. et al. Laparoscopic and Robotic Sleeve Gastrectomy: Short- and Long-Term Results. OBES SURG 25, 967–974 (2015). https://doi.org/10.1007/s11695-014-1499-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1499-0