Abstract
Obesity is an important modifiable risk factor for musculoskeletal disease. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-compliant systematic review of bariatric surgery on musculoskeletal disease symptoms was performed. One thousand nineteen papers were identified, of which 43 were eligible for data synthesis. There were 79 results across 24 studies pertaining to physical capacity, of which 53 (67 %) demonstrated statistically significant post-operative improvement. There were 75 results across 33 studies pertaining to musculoskeletal pain, of which 42 (56 %) demonstrated a statistically significant post-operative improvement. There were 13 results across 6 studies pertaining to arthritis, of which 5 (38 %) demonstrated a statistically significant post-operative improvement. Bariatric surgery significantly improved musculoskeletal disease symptoms in 39 of the 43 studies. These changes were evident in a follow-up of 1 month to 10 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity, defined as a body mass index (BMI) of greater than 30 kg/m2, has been recognised as a global epidemic for many years [1], with an estimated 315 million adults affected worldwide [2]. This poses a huge health and economic burden, as it is widely established that morbid obesity is a significant risk factor in the development of many chronic diseases. These include coronary artery disease, hypertension, dyslipidaemia and diabetes mellitus [3–5]. Although the effects of obesity (and weight reduction) on these conditions have received the focus of attention in terms of obesity health policy, there are additional significant impacts on psychosocial and musculoskeletal health in the form of arthropathy, musculoskeletal pain, loss of mobility and loss of physical capacity [6–8].
A number of conservative and medical treatments of obesity have previously been recommended, ranging from lifestyle modification to pharmacological therapies, with little success [9–11]. A recent Cochrane review and Health Technology Assessment has demonstrated that surgical management of obesity is clinically more effective than conventional treatment [12, 13].
Obesity is associated with musculoskeletal pain and osteoarthritis, with the lower back and knees most commonly affected. Raised BMI leads to abnormally increased joint loads which in turn alters the structure and composition of articular cartilage [14]. Altered articular cartilage is less able to absorb excess loading forces, which can then lead to deformation of affected joints [15]. Additionally, in obese subjects, skeletal muscle is laden with intramuscular fat which releases systemic and local pro-inflammatory mediators, such as IL-6 and TNF-α. This creates a worsening cycle of local inflammation that, in combination with mechanical factors, leads to a variety of musculoskeletal impairments [16]. These include various pathological phenotypes, such as osteoarthritis and reduced muscle mass, as well as their occupational and lifestyle consequences, such as reduced physical capacity, slower walking speed and musculoskeletal pain [17].
The direct costs of treating obesity and the indirect costs associated with loss of productivity are huge [18]. Recent publications have estimated the direct cost of obesity and related illnesses in the UK at £4.3 billion–£5.1 billion (Euro €5.2 billion–€6.1 billion, US $7.2 billion–$8.5 billion) [19, 20]. The National Institute for Health and Clinical Excellence (NICE) has recently estimated the indirect costs to be UK £2 billion (Euro €2.4 billion, US $3.3 billion) [21]. Similar scales of expenditure are seen elsewhere in the developed world, with an annual total direct and indirect cost of US $139 billion (UK £84 billion, Euro €101 billion) [22] and CDN $4.3 billion (UK £2.3 billion, Euro €2.8 billion, US $3.9 billion) in the USA and Canada, respectively [23].
As obesity is the single most important modifiable risk factor in the progression of osteoarthritis and other musculoskeletal disorders, the impact of bariatric surgery on physical function, and therefore on Health Care Quality of Life (HCQoL) and productivity, may be significant. Bariatric surgery may represent an area of health care reform that can lead to both significant improvements in clinical outcomes and broader economic cost-effectiveness.
In this paper, we aim to provide a systematic review of the impact of bariatric surgery on physical function, musculoskeletal pain and arthritis.
Methodology
This systematic review was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement to improve transparency and completion of our reporting [24]. A study protocol documenting keywords, inclusion and exclusion criteria was produced in advance and agreed by consensus.
Literature Search
A systematic review of the literature was performed using multiple electronic search engines including PubMed, MEDLINE, Ovid and Embase. The search terms, agreed by consensus, are listed as follows:
-
(bariatric OR (weight surgery)) AND mobility
-
(bariatric OR (weight surgery)) AND (((QoL OR (Quality of Life)) AND pain)
-
(bariatric OR (weight surgery)) AND (musculoskeletal)
-
(bariatric OR (weight surgery)) AND arthritis
The search was repeated with the word “weight” replaced with “obesity”, and the results of the two searches were combined.
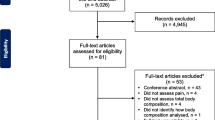
The above terms were generated with the aid of consultant bariatric surgeons with significant experience in surgical academia. The “related” function was used in Pubmed to identify additional papers. References of the articles identified were also searched for by title and, where necessary, abstract review. Relevant systematic reviews’ reference lists were examined, and any relevant papers encountered that were not retrieved in the original database search were also included. Figure 1 provides an overview of search outcomes according to the PRISMA protocol.
Eligibility Criteria and Data Extraction
All peer-reviewed published data that investigated the impact of bariatric surgery on post-operative musculoskeletal pain, arthritis and physical function were considered. The search was restricted to studies published in English, but there were no restrictions on study age, type of study or cohort size.
All papers were reviewed by an author with experience in data extraction and publication of systematic reviews (UE) and were cross checked by a second author (SP). Relevant articles were title and abstract reviewed and, where necessary, also reviewed in full text. Any uncertainty as to inclusion was agreed by consensus.
Inclusion and Exclusion Criteria
To be included in the data analysis, a study had to report a method of determining the impact of bariatric surgery on any of the following outcomes: physical function (including mobility), musculoskeletal pain, arthritis and at any point post-operatively. Studies solely investigating biochemical changes or any other non-musculoskeletal parameter were not included.
In view of our inclusion of all levels of evidence, all papers were scored for quality of evidence in accordance with the original (1989) US Preventive Services Task Force Recommendations instead of the 2011 recommendations. This is because the 1989 guidelines were more objective and provided more subsets of levels of evidence [25].
Data Analysis
Data was extracted from the included studies and tabulated using Microsoft Excel. Due to the heterogeneity of the methods and results of the papers identified and used in this review, it was not possible to perform a quantitative meta-analysis.
All cost figures are provided in the currency originally cited. Equivalent values in other currencies are included in parentheses, calculated at the exchange rate at the time of writing.
Results
Literature Search
The initial search identified 1,019 citations. After removing duplicates, papers not written in English and papers not related to bariatric surgery, 124 papers remained. Of these, 81 did not meet the inclusion criteria detailed above. The final number of papers included in this systematic review was 43 (Fig. 1) [26–68].
Quality of Evidence
All 43 papers were assigned a quality of evidence score in accordance with the original US Preventive Services Task Force Ratings [25]. There were 37 prospective studies and 6 retrospective studies. Of the 37 prospective studies, 3 were randomised controlled trials (level I evidence), 2 were non-randomised controlled trials (II—1), and 10 were prospective cross-sectional trials, including 2 studies that also contained a prospective longitudinal study within it (level II—2 evidence). The remaining 22 studies were prospective longitudinal studies (level II—2 evidence). The largest sample population of the prospective studies was 1,916 and the smallest was 14. The six retrospective studies had sample populations ranging from 15 to 5,502 (level II—3 evidence).
Of the 43 studies in this review, 15 did not use a validated tool to assess the inclusion outcomes. The remaining 28 studies used a variety of 24 different validated outcome tools, with the SF-36 questionnaire the most frequently utilised (15 times) (Table 1).
Outcome Measures
No single study investigated all three outcomes. Of the 43 studies, 22 reported on two outcomes. This also included a paper that did not clearly specify outcomes, but the description in the text was deemed by consensus to meet both mobility and musculoskeletal (MSK) pain [56]. The remaining 21 reported on a single outcome. Musculoskeletal pain was investigated in 33 studies, mobility in 24 studies and arthritis in 6 studies (Table 1).
Mobility
Table 2 refers to all studies that investigated the impact of bariatric surgery on post-operative mobility. Follow-up ranged from 1 month to 10 years. Each component of the relevant outcome questionnaire across the 24 mobility studies was individually deconstructed to provide 79 individual results, listed in chronological order. The authors of four papers did not supply information on statistical significance for 14 of the 79 individual results [33, 40, 44, 56]. Of these 14 results, 1 showed no difference in physical function between open and laparoscopic bariatric surgery groups [40], and the remaining 13 results all showed a tendency to improved mobility or physical function post-operatively [33, 44, 56].
Of the remaining 65 individual results for which the authors confirmed statistical significance, 4 demonstrated a worsening in physical function between 1 and 5 years post-operatively (derived from one study) [32]. Of the remaining 61 results, 3 showed no difference in comparison to population norms [28, 40], 2 showed no difference in physical function scores [26], 1 showed no significant difference between patients in different surgery groups [29], 1 showed a worsening in comparison to population norms [28], and 1 showed a worsening in the surgical group compared to the non-surgical control group [29]. The remaining 53 results all demonstrated significant improvements in physical function.
Pain
Table 3 refers to all studies that investigated the impact of bariatric surgery on post-operative musculoskeletal pain. Follow-up ranged from 1 month to 10 years. Each component of the relevant outcome questionnaire across the 33 musculoskeletal pain studies was individually deconstructed to provide 75 individual results, listed in chronological order. Of the 75 individual results, 42 pertained to a named anatomical region; most commonly the back followed by the knee.
Of these 75 results, the authors did not supply information on statistical significance for 29 of them [31, 35, 38–40, 44, 47, 49, 54–56, 66, 67]. Of these 29 results, 2 had no difference in pain scores [31, 39], and 1 showed a worsening in pain score between 1 and 3 years post-operatively [39]. The remaining 26 results all demonstrated an improvement in pain.
Of the 46 individual results for which the authors provided information on statistical significance, 1 showed no difference in bodily pain 3 months after surgery [26], 1 showed a worsening in pain between 1 and 5 years post-operatively [32], and 2 showed higher pain in the surgical group compared to population norms after 5-year follow-up [28]. The remaining 42 results all confirmed statistically significant improvements in bodily or regional pain up to at least 5 years post-operatively [27, 31, 35–37, 41, 43, 45, 48, 51–53, 57, 58, 60–62, 66, 67].
Arthritis
Six studies in this review investigated the impact of bariatric surgery on arthritis based on author-specified surrogates [34, 42, 46, 50]. These include the following: symptoms of arthritis, reduction in arthritis medication requirements and reduction in symptoms of arthritis based on a questionnaire. One paper retrospectively investigated the incidence of arthroplasty in post-operative groups stratified for rate of weight loss [65]. The individual components of the six studies’ results were deconstructed to provide 13 individual results (Table 4). Follow-up ranged from 1 to 9 years.
Of the 13 individual results, 5 did not include any information on statistical significance [50, 63, 67, 68]. All five individual results showed an improvement in arthritis between 1 and 4 years post-operatively. Further breakdown of one result by Schauer et al. showed that whilst most patients within this study had improved arthritis surrogates at 1 year post-operatively, 2 % actually reported a worsening [63].
Of the remaining eight results that did include data on statistical significance, four demonstrated a significant reduction in arthritis (based on a surrogate marker) between 3 and 5 years post-operatively [34, 42]. One result showed an improvement in symptoms in two surgical groups (low BMI vs control) but no statistically significant intergroup difference [46].
Only two results could possibly be construed as negative. Cremieux et al. reported an increased prevalence of acquired MSK deformity at 3-year follow-up, although the remainder of their results had a tendency towards a reduction in arthritis [34]. Trofa et al. subset analysed their post-operative group in terms of rate of weight loss. They suggested that a rate of weight loss greater than 0.6 kg/m2/month may be a risk factor for joint arthroplasty post-operatively (p < 0.001) [65].
Weight Loss and Procedure Type
Tables 5, 6 and 7 refer to all results listed in ascending order of time to follow-up and, where specified, expanded to include data on the procedure type and rate of weight loss. A total of 112 individual results were listed. Of these, 41 results included data on weight loss obtained at different times to data relating to the outcome measures. Therefore, a linked analysis of weight loss and outcome measures was not possible for these 41 entries.
Of the 112 results, 40 were exclusively gastric band procedures and 62 were non-banded procedures, which included all gastric bypasses, stapled gastroplasties and duodenal switches, and 10 results pertained to studies with a mixture of banded and non-banded procedures.
A variety of tools were used to assess weight loss; however, for sake of clarity, only absolute weight loss (kg), BMI (either proportion change or absolute values), percentage excess weight loss (%EWL) and percentage excess BMI loss (%EBMIL) were listed. The range of change in BMI was −6.3 to −20.86, %EWL 18.4–83.2 and %BMIL 9.3–77.8.
Discussion
The quality of the papers in this review was moderate, with only 5 of the 43 studies being prospective controlled trials, of which only 3 were randomised. However, to our knowledge, this is the most thorough systematic review of this subject matter in the literature. Other notable reviews of musculoskeletal disease outcomes in bariatric surgery patients include the works of Speck et al. [69] and Gill et al. [70], who include 16 and 6 studies in their data syntheses, respectively.
The results of this review are likely to achieve external validity in the developed world, as the majority of the papers were conducted within Europe or North America and covered a wide variety of bariatric procedures.
Fifteen of the 43 studies did not utilise a validated outcome tool, and the remaining 28 studies used a variety of 24 different tools. Of the papers that did use a validated tool, only four papers used the BAROS [39, 44] or Moorehead-Ardelt questionnaire [31, 63] tools created specifically for bariatric surgery patients. Although these questionnaires achieved high validity and compared favourably with other established tools, like the SF-36, the heterogeneity of the results and tools used to generate them made statistical analysis impossible.
The results of the impact of bariatric surgery on physical function are generally positive. Table 3 shows that the improvements in function are seen as early as 1 month post-operatively and sustained for up to 10 years, reflecting bariatric surgery’s position as the most effective and long-lasting weight-reducing method. The results of the paper by Strain et al. did show that the three cohort groups, investigated at the same time and divided into 1-year, 3-year and 5-year follow-up, respectively, showed a worsening physical capacity with prolonged post-operative follow-up. The three studies that demonstrated no worsening in physical function in comparison to population norms may be considered positive results, as any obesity-related impairment had effectively been eliminated. The studies that showed a worse result in comparison to population norms and non-surgical controls, respectively, did not offer absolute intragroup values, and hence, it is impossible to assess the impact of surgery on these cohorts independently. It is possible that these results may have demonstrated a significant intragroup improvement in physical function that may be lost in the authors’ method of reporting.
The pain scores were much more unequivocal, with 68 of the 75 individual results demonstrating an improvement in pain, although 26 of these results did not specify statistical significance. The improvement in pain was reported as early as 1 month and sustained up to 10 years post-operatively. Vincent et al. [26] reported no difference in bodily pain in their cross-sectional study, although the pain score had improved in the cohort undergoing surgery. A similar effect was seen in the study by Lidar et al. [31]. Hooper et al. [36] showed an improvement in the WOMAC pain score in their longitudinal study although this did not achieve statistical significance.
Reporting on arthritis in this review was challenging, as only one of the six studies that listed arthritis as an outcome used a validated tool [63]. It was difficult to determine on what grounds arthritis was evaluated on, and it is likely that clinical surrogates such as pain, stiffness and loss of function may have allowed this section to be discussed under the other outcomes of this review (physical function and pain). Nonetheless, five of the six studies showed a general improvement in arthritis (however assessed) between 1- and 5-year follow-up. To our knowledge, Trofa et al. are unique in the literature by suggesting that a rate of weight loss greater than 0.6 kg/m2/month may be a risk factor for joint arthroplasty post-operatively (p < 0.001). As all 15 of the patients in their study had pre-operative evidence of osteoarthritis, they do not believe that rapid weight loss is a cause for total joint replacement but could be a risk factor for it in view of the improved physical capacity adding additional strain on chronically damaged joints [65].
Mechanisms that contribute to reduced physical capacity include muscle weakness, joint stiffness and pain [71]. Pain is perhaps the most modifiable factor of the three, with muscle weakness and joint stiffness, in particular, reflecting more chronic and permanent obesity-related joint changes. This may explain the trends seen in our review of bariatric surgery significantly improving pain over a 10-year follow-up, with more equivocal improvements in physical function.
The range in weight loss, however assessed, was large. The lowest reductions in BMI related to a number of studies that exclusively assessed gastric band procedures, but this finding was not supported by other measures of weight loss and nor by length to follow-up. Despite modest reductions in weight, these studies still reported improvements in musculoskeletal symptoms. The largest changes in %EWL appeared in the study of Melissas et al. [49], in which a comparison of outcomes was performed between morbidly and super obese subjects. Excluding these extremes, there appeared to be no clear trend in quantifiable weight loss, procedure type and change in musculoskeletal symptoms. The majority of findings in this review supported a sustained improvement in musculoskeletal symptoms following obesity surgery. With no method of standardising weight loss quantification, it was not possible for this review to explore a possible correlation between the rate of weight loss and outcomes in musculoskeletal disease, a concept suggested by Trofa et al. who hypothesised that the rate of weight loss may be a risk factor for arthroplasty.
The global economic cost of obesity is huge, with the direct costs alone reported to represent 2–7 % of the total world health cost. [72] With recent data pointing to a moderate incremental cost per quality-adjusted life year of UK £2,000–£4,000 (US $3,200–$6,400, Euro €2,400– €4,900) [73], the ability for laparoscopic bariatric surgery to pay for itself within 1 year [20] and a reduction in state benefit claims by 75 % after 14 months [74], there is a compelling economic argument for bariatric surgery. Despite an increase in bariatric surgery activity, referral rates in the developed world are likely to be low. A recent national cross-sectional survey revealed that 5.4 % of the non-institutionalised population in England met the referral criteria for bariatric surgery [75], yet surgery rates were estimated to be only a third of the NHS benchmark [76]. An Australian paper in 2009 reported a lower than 1 % surgery rate [77]. An Office of Health Economics report estimated that if 25 % of UK eligible patients received bariatric surgery, there would be a UK £1.45 billion (US $2.3 billion, Euro €1.78 billion) increase to the GDP from increased population productivity and reduction in health costs and state benefits [20]. There is clearly a clinical and economic need to ensure that current referral guidelines are more thoroughly implemented.
Referral guidelines are largely based on the 1991 National Institute of Health criteria, which are practically identical to recently published European and NICE guidelines [78–80]. The referral criteria can be loosely summarised as offering surgery to motivated patients with a BMI >40 kg/m2 or >35 kg/m2 with a serious obesity-related co-morbidity. The NIH guidelines were fashioned from the limited available evidence at the time and equate “patient risk” with BMI and the presence of obesity-related co-morbidity, with little consideration of other patient factors such as age, ethnicity, weight distribution and future risk. None of the guidelines specifically mentions projected improvement in mobility as an influencing factor when referring to bariatric surgery, although the European Guidelines lists “severe joint disease” as an obesity-related disorder [79]. In view of the significant economic gains to be had by mobilising a previously morbidly obese workforce, the concept of factoring in physical capacity alongside current criteria when considering bariatric surgery warrants further exploration.
Several studies in our review expanded their patient selection beyond the standard criteria described in the NIH referral guidelines. Some centres operated on patients with BMI 30–35 kg/m2 [46], the “super obese” [49, 68] and patients with certain co-morbidities, such as cardiac failure [48] and low back pain [51]. These studies showed improved results within the context of musculoskeletal pain and HCQoL. This therefore suggests that not only is there a need for a larger number of obese patients to be referred for surgery in accordance with current guidelines, but there is also scope for the referral criteria to be broadened.
Conclusion
The significant costs of managing obesity can be reduced by bariatric surgery at a small increment in cost per quality-adjusted life year. A proportion of this cost-effectiveness can be attributed to an improvement in physical capacity, although the exact figure is not determinable from our review. Bariatric surgery significantly improved physical function, musculoskeletal pain and arthritis over a period of 10 years in 39 of the 43 studies in our review. The proportion of eligible patients being referred for bariatric surgery is low. This raises the question of whether NICE guidelines should be reviewed to improve referral rate and broaden patient selection.
References
World Health Organization. Obesity: preventing and managing the global epidemic. Geneva: WHO Technical Report Series 894; 2000.
Caterson I, Gill T. Obesity: epidemiology and possible prevention. Pract Res Clin Endocrinol Metab. 2002;16(4):595–610.
Lakka H, Laaksonen D, Lakka T, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288(21):2709–16.
Janssen I, Katzmarzyk P, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–84.
Mokdad A, Ford E, Bowman B, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors. JAMA. 2003;289(1):76–9.
Woo J, Leung J, Kwok T. BMI, body composition, and physical functioning in older adults. Obesity. 2007;15(7):1886–94.
Sternfeld B, Ngo L, Satariano W, et al. Associations of body composition with physical performance and self-reported functional limitation in elderly men and women. Am J Epidemiol. 2002;156(2):110–21.
Stenholm S, Sainio P, Rantanen T, et al. Effect of co-morbidity on the association of high body mass index with walking limitation among men and women aged 55 years and older. Aging Clin Exp Res. 2007;19(4):277–83.
Low AM, Bouldin MC, Sumrall C, et al. A clinician’s approach to medical management of obesity. Am J Med Sci. 2006;331(4):175–82.
Sierra-Johnson J, Wright S, Lopez-Jiminez F, et al. Retaliation of body mass index to fatal and nonfatal cardiovascular events after cardiac rehabilitation. Am J Cardiol. 2005;96(2):211–4.
Over-the-counter weight loss with orlistat? Drugs Ther Bull. 2009;47:125–7.
Colquitt J, Picot J, Loveman E, et al. Surgery for obesity. Cochrane Database Syst Rev. 2009;15(2), CD003641.
Picot J, Jones J, Colquitt J, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13(41):1–190.
Andersen R, Crespo C, Bartlett S, et al. Relationship between body weight gain and significant knee, hip, and back pain in older Americans. Obes Res. 2003;11(10):1159–62.
Hitt H, McMillen R, Thornton-Neaves T, et al. Co-morbidity of obesity and pain in a general population: results from the Southern Pain Prevalence Study. J Pain. 2007;8(5):430–6.
Schranger M, Metter E, Simonsick E, et al. Sarcopenic obesity and inflammation in the InCHIANTI study. J Appl Physiol. 2007;102(3):919–25.
Sowers M, Karvonen-Gutierrez C. The evolving role of obesity in knee osteoarthritis. Curr Opin Rheumatol. 2010;22(5):533–7.
Terranova L, Busetoo L, Vestri A, et al. Bariatric surgery: cost-effectiveness and budget impact. Obes Surg. 2012;22(4):646–53.
Scarborough P, Bhatnagar P, Wickramasinghe K, et al. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: an update to 2006–07 NHS costs. J Public Health. 2011;33(4):527–35.
Office of Health Economics Report: Shredding the pounds. www.rcseng.ac.uk/news/docs/BariatricReport.pdf (2010). Accessed 03 Jan 2014
National Institute for Health and Clinic Excellence UK (NICE). Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children. NICE Clin Guidel. 2006;43.
Levi J, Vinter S, Richardson L, et al. F as in fat: how obesity policies are failing in America. Princeton: Robert Wood Johnson Foundation 2009; 2009.
Katzmarzyk P, Janssen I. The economic costs associated with physical inactivity and obesity in Canada: an update. Can J Appl Physiol. 2004;29(1):90–115.
Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. BMJ. 2009;3(3):e123–30.
Report of the US Preventive Services Task Force. Guide to clinical preventive services, 1989 Appendix A Page 263.
Vincent H, Ben-David K, Conrad B, et al. Rapid changes in gait, musculoskeletal pain, and quality of life after bariatric surgery. Surg Obes Relat Dis. 2012;8(3):346–54.
Schouten R, Wiryasaputra D, van Dielen F, et al. Influence of reoperations on long-term quality of life after restrictive procedures: a prospective study. Obes Surg. 2011;21(7):871–9.
Mathus-Vliegen E. Long-term health and psychosocial outcomes from surgically induced weight loss: results obtained in patients not attending protocolled follow-up visits. Int J Obes (Lond). 2007;31(2):299–307.
Sanchez-Santos R, Del Barrio M, Gonzalez C, et al. Long-term health-related quality of life following gastric bypass: influence of depression. Obes Surg. 2006;16(5):580–5.
Dziurowicz-Kozłowska A, Lisik W, Wierzbicki Z, et al. Health-related quality of life after the surgical treatment of obesity. J Physiol Pharmacol. 2005;56(S6):127–34.
Lidar Z, Behrbalk E, Regev G, et al. Intervertebral disc height changes after weight reduction in morbidly obese patients and its effect on quality of life and radicular and low back pain. Spine (Phila Pa 1976). 2012;37(23):1947–52.
Strain G, Saif T, Gagner M, et al. Cross-sectional review of effects of laparoscopic sleeve gastrectomy at 1, 3, and 5 years. Surg Obes Relat Dis. 2011;7(6):714–9.
Søvik T, Aasheim E, Taha O, et al. Weight loss, cardiovascular risk factors, and quality of life after gastric bypass and duodenal switch: a randomized trial. Ann Intern Med. 2011;155(5):281–91.
Crémieux P, Ledoux S, Cleric C, et al. The impact of bariatric surgery on comorbidities and medication use among obese patients. Obes Surg. 2010;20(7):861–70.
Brancatisano A, Wahlroos S, Brancatisano R. Improvement in comorbid illness after placement of the Swedish Adjustable Gastric Band. Surg Obes Relat Dis. 2008;4(S3):39–46.
Hooper M, Stellato T, Hallowell P, et al. Musculoskeletal findings in obese subjects before and after weight loss following bariatric surgery. Int J Obes (Lond). 2007;31(1):114–20.
Dittmar M, Heintz, Hardt J, et al. Metabolic and psychosocial effects of minimal invasive gastric banding for morbid obesity. Metabolism. 2003;52(12):1551–7.
Melissas J, Volakakis E, Hadjipavlou A. Low-back pain in morbidly obese patients and the effect of weight loss following surgery. Obes Surg. 2003;13(3):389–93.
Schoepel K, Olchowsk IS, Mathis M, et al. Starting a successful bariatric surgical practice in the community hospital setting. Obes Surg. 2001;11(5):559–64.
Nguyen N, Goldman C, Rosenquist C, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234(3):279–89.
Choban P, Onyejekwe J, Burge J, et al. A health status assessment of the impact of weight loss following Roux-en-Y gastric bypass for clinically severe obesity. J Am Coll Surg. 1999;188(5):491–7.
Sampalis J, Sampalis F, Christou N. Impact of bariatric surgery on cardiovascular and musculoskeletal morbidity. Surg Obes Relat Dis. 2006;2(6):587–91.
Peltonen M, Lindroos A, Torgerson J. Musculoskeletal pain in the obese: a comparison with a general population and long-term changes after conventional and surgical obesity treatment. Pain. 2003;104(3):549–57.
Scozzari G, Toppino M, Famiglietti F, et al. 10-year follow-up of laparoscopic vertical banded gastroplasty: good results in selected patients. Ann Surg. 2010;252(5):831–9.
Richette P, Poitou C, Garnero P, et al. Benefits of massive weight loss on symptoms, systemic inflammation and cartilage turnover in obese patients with knee osteoarthritis. Ann Rheum Dis. 2011;70(1):139–44.
Choi J, Digiorgi M, Milone L, et al. Outcomes of laparoscopic adjustable gastric banding in patients with low body mass index. Surg Obes Relat Dis. 2010;6(4):367–71.
McGoey B, Deitel M, Saplys R, et al. Effect of weight loss on musculoskeletal pain in the morbidly obese. J Bone Joint Surg (Br). 1990;72(2):322–3.
Alsabrook G, Goodman HJ, Alexander J. Gastric bypass for morbidly obese patients with established cardiac disease. Obes Surg. 2006;16(10):1272–7.
Melissas J, Christodoulakis M, Schoretsanitis G, et al. Obesity-associated disorders before and after weight reduction by vertical banded gastroplasty in morbidly vs super obese individuals. Obes Surg. 2001;11(4):475–81.
Murr M, Siadati M, Sarr M. Results of bariatric surgery for morbid obesity in patients older than 50 years. Obes Surg. 1995;5(4):399–402.
Khoueir P, Black M, Crookes P, et al. Prospective assessment of axial back pain symptoms before and after bariatric weight reduction surgery. Spine J. 2009;9(6):454–63.
Abu-Abeid S, Wishnitzer N, Szold A, et al. The influence of surgically-induced weight loss on the knee joint. Obes Surg. 2005;15(10):1437–42.
Korenkov M, Shah SS, Sauerland S, et al. Impact of laparoscopic adjustable gastric banding on obesity co-morbidities in the medium- and long-term. Obes Surg. 2007;17(5):679–83.
Magee C, Barry J, Arumugasamy M, et al. Laparoscopic sleeve gastrectomy for high-risk patients: weight loss and comorbidity improvement—short-term results. Obes Surg. 2011;21(5):547–50.
Cottam D, Qureshi F, Mattar S, et al. Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg Endosc. 2006;20(6):859–63.
Zhang N, Maffei A, Cerabona T, et al. Reduction in obesity-related comorbidities: is gastric bypass better than sleeve gastrectomy. Surg Endosc. 2013;27(4):1273–80.
Aftab H, Risstad H, Søvik T, et al. Five-year outcome after gastric bypass for morbid obesity in a Norwegian cohort. Surg Obes Relat Dis. 2014;10(1):71–8.
Julia C, Ciangura C, Capuron L, et al. Quality of life after Roux-en-Y gastric bypass and changes in body mass index and obesity-related comorbidities. Diabetes Metab. 2013;39(2):148–54.
Iossi M, Konstantakos E, Teel D, et al. Musculoskeletal function following bariatric surgery. Obesity. 2013;21(6):1104–10.
Grans R, Warth C, Farah J, et al. Quality of life and prevalence of osteoarticular pain in patients submitted to bariatric surgery. Einstein (Sao Paulo). 2012;10(4):415–21.
Edwards C, Rogers A, Lynch S, et al. The effects of bariatric surgery weight loss on knee pain in patients with osteoarthritis of the knee. Arthritis. 2012;2012:504189. doi:10.1155/2012/504189.
Ahroni J, Montgomery K, Watkins B. Laparoscopic adjustable gastric banding: weight loss, co-morbidities, medication usage and quality of life at one year. Obes Surg. 2005;15(5):641–7.
Schauer P, Ikramuddin S, Gourash W, et al. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 2000;232(4):515–29.
Parvizi J, Trousdale R, Sarr M. Total joint arthroplasty in patients surgically treated for morbid obesity. J Arthroplasty. 2000;15(8):1003–8.
Trofa D, Smith E, Shav V, Shikora S. Total weight loss associated with increased physical activity after bariatric surgery may increase the need for total joint arthroplasty. Surg Obes Relat Dis. 2013; (2):335–9. doi: 10.1016/j.soard.2013.09.011.
James X, Jonathan S, Steven B, et al. The effect of laparoscopic adjustable gastric banding on osteoarthritis and other obesity-related comorbidities. J Obes Weight Loss Ther. 2012. doi:10.4172/2165-7904.1000138.
Peluso L, Vanek V. Efficacy of gastric bypass in the treatment of obesity-related comorbidities. Nutr Clin Pract. 2007;22(1):22–8.
Raftopoulos I, Ercole J, Udekwu A, et al. Outcomes of Roux-en-Y gastric bypass stratified by a body mass index of 70 kg/m2: a comparative analysis of 825 procedures. J Gastrointest Surg. 2005;9(1):44–52.
Speck R, Bond D, Sarwer D, et al. A systematic review of musculoskeletal pain among bariatric surgery patients: implications for physical activity and exercise. Surg Obes Relat Dis. 2013;10(1):161–70.
Gill R, Al-Adra DP, Shi X, et al. The benefits of bariatric surgery in obese patients with hip and knee osteoarthritis: a systematic review. Obes Rev. 2011;12(12):1083–9.
Weaver G, Kuo Y, Raji M, et al. Pain and disability in older Mexican-American adults. J Am Geriatr Soc. 2009;57(6):992–9.
Powers K, Rehrig S, Jones D. Financial impact of obesity and bariatric surgery. Med Clin North Am. 2007;91(3):321–38.
McCartney M. Slimmed down surgery. BMJ. 2010;341:c5499.
Hawkins S, Osborne A, Finlay I, et al. Paid work increases and state benefit decreases after bariatric surgery. Obes Surg. 2007;17(4):434–7.
Ahmad A, Laverty A, Aasheim E, et al. Eligibility for bariatric surgery among adults in England: analysis of a national cross-sectional survey. J R Soc Med Open. 2013;5(1):1–6.
National Institute for Health and Clinical Excellence. Bariatric surgical service for the treatment of people with severe obesity. Commissioning guide, 2007.
Dixon J. Referral for a bariatric surgical consultation: is it time to set a standard of care. Obes Surg. 2009;19(5):641–4.
Hubbard V, Hall W. Gastrointestinal surgery for severe obesity. Obes Surg. 1991;1(3):257–65.
Fried M, Hainer V, Basdevant A. Inter-disciplinary European guidelines on surgery of severe obesity. Int J Obes. 2007;31(4):569–77.
CG43; Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children. NICE Clinical Guidelines. http://publications.nice.org.uk/obesity-cg43. Accessed 12 Jan 2013.
Statement of Informed Consent
For this type of study, formal consent is not required. To our knowledge, all studies included in the data synthesis were compliant with local research ethics guidelines.
Statement of Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest
All authors declare no conflict of interest.
Source Funding
Funding was not required nor requested for the research detailed in the manuscript. All authors declare no source of funding.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-khani, U., Ahmed, A., Hakky, S. et al. The Impact of Obesity Surgery on Musculoskeletal Disease. OBES SURG 24, 2175–2192 (2014). https://doi.org/10.1007/s11695-014-1451-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1451-3