Abstract
Background
The functional aspects of obesity are increasingly recognised as a significant clinical and public health concern. Whilst there is substantial evidence for the beneficial impact of bariatric surgery on metabolic and cardiovascular disease, there is less understanding of the quantitative effect of bariatric surgery on back pain. The aim of this meta-analysis was to assess the impact of bariatric surgery on back pain in reported studies.
Methods
Medline, Embase, conference proceedings and reference lists were searched for studies assessing quantitative back pain scores both before and after bariatric surgery. The primary outcome was visual analogue score for back pain pre- and post-bariatric surgery. Secondary outcomes were change in BMI, SF-36 quality of life scores and Oswestry Disability Index (ODI) scores. Weighted mean differences (MD) were calculated for continuous outcomes.
Results
Seven studies were included in the analysis of 246 patients undergoing bariatric surgery. Mean study follow-up was between 3 and 24 months. There was a statistically significant reduction in visual analogue score for back pain following bariatric surgery (MD − 3.01; 95% CI − 4.19 to − 1.89; p < 0.001). Bariatric surgery also resulted in statistically significant improvements in BMI, SF-36 score and ODI score.
Conclusions
Bariatric surgery produces significant and quantifiable reductions in back pain. This may be commuted through reductions in axial load or improved quality of life, but further studies will improve understanding and aid preoperative counselling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Global levels of obesity are increasing and constitute a major health concern due to obesity-related disease [1, 2]. The main health consequences related to obesity include type 2 diabetes, cardiovascular disease, musculoskeletal disorders such as osteoarthritis and low back pain, and certain cancers. Metabolic surgery has been shown in multiple randomised trials and meta-analyses to be effective at improving obesity-related comorbidities and improving quality of life [3].
Whilst the focus on comorbidity management for patients with obesity has tended to focus on type 2 diabetes and cardiovascular disease, there is an increasing focus on quality of life and physical functioning [4]. The prevalence of joint and back pain increases progressively with greater BMI [4]. Joint pain symptoms are particularly prevalent in the load-bearing segments of the body, including the low back and lower limbs (ankles, knees, hips) [4, 5]. The incapacitating effect of back pain contributes to worsening of obesity and physical disability which in itself has a negative impact on physical functioning and leads to deterioration of health-related quality of life (QOL) [5]. A number of studies have explored the effect of bariatric surgery, as an obesity treatment, on the occurrence of back pain, but these are all small studies and no quantitative synthesis of this literature has been performed to date.
This article aims to undertake a systematic review and meta-analysis focussing on back pain related to obesity and specifically on the impact that bariatric surgery has on back pain.
Materials and Methods
Search Strategy
An electronic search was performed using the Embase and Medline databases, and the Cochrane Database of Controlled Trials from 1966 to November 2019. The search strategy terms ‘bariatrics’, ‘obesity surgery’, ‘gastric bypass’, ‘gastric sleeve’, ‘Roux-en-Y’, ‘RYGB’, ‘sleeve gastrectomy’ and ‘adjustable gastric band’ and ‘back pain’ were used in combination with the Boolean operator AND or OR. The electronic search was supplemented by a handsearch of published abstracts from meetings of the International Federation for the Surgery of Obesity and Metabolic Disorders, the British Obesity and Metabolic Surgery Society and the American Society for Metabolic and Bariatric Surgery from 1983 to 2019. The bibliography of articles obtained was additionally searched to identify further relevant citations.
Selection Criteria
Abstracts of the citations identified by the search were then reviewed to determine eligibility for inclusion in the meta-analysis by two independent reviewers (IS and ACC). Studies were included if they only included patients aged 18 years or over, where the primary outcome assessed was back pain in patients before and after bariatric surgery. Discrepancies were resolved by consensus and agreement of the wider authorship team. Exclusion criteria included non-English studies where no translation was available, duplicate studies, kin studies, or studies with an incorrect comparator. Full-text articles of all selected abstracts were further reviewed by two reviewers (IS and ACC) using the same criteria, and disputes were resolved by a senior reviewer. Included studies were then assessed for methodological quality and bias using the MINORS tool for non-randomised studies [6].
Data Extraction
Pertinent data was collected from selected trials by one reviewer (IS) and a second reviewer checked for accuracy (ACC). The primary outcome of interest included the mean visual analogue score (VAS) for back pain before and after bariatric surgery. A number rating scale (NRS) was substituted when the VAS was not available. Secondary outcomes included BMI, disability assessment and quality of life. The following patient characteristics were assessed: age, gender, pre- and postoperative measurements for BMI, weight, visual analogue score for back pain, Oswestry disability index and quality of life (QoL) assessment using Short-Form 36 (SF-36).
Statistical Analysis
Categorical variables were reported as frequencies and percentages, and continuous data was expressed as mean ± standard deviation. Meta-analysis was conducted where possible for outcomes relating to back pain in patients before and after bariatric surgery. Outcomes assessed in the meta-analysis were assessed using weighted mean difference (MD). The estimated effects were calculated using Revman 5.3 software obtained from the Cochrane website. Where data was not available in the articles or from the authors, then Cochrane methods for missing data were followed. All pooled outcome measures were determined using the DerSimonian and Laird’s random effects model [7]. Heterogeneity in the results of the trials was assessed using a chi-square test of heterogeneity (significance level P < 0.1) and the I2 measure of inconsistency [8].
Results
Study Selection
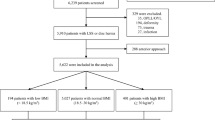
A preliminary database search of the literature yielded 293 articles after duplicates were removed (Fig. 1). After initial screening of titles and abstracts, 16 studies underwent full-text assessment for eligibility. Seven manuscripts met inclusion criteria and were included in the final systematic review. The included manuscripts consisted of seven cohort studies.
Basic Demographics
A total of seven studies [5, 9,10,11,12,13,14] with 246 patients were included (Table 1). In the meta-analysis, there were 206 females (83.7%), the mean age was 42.3 years and the mean follow-up was 11.7 months. There were a variety of operative techniques used including, where recorded, Roux-en-Y gastric bypass (148), sleeve gastrectomy (48) and vertical banded gastroplasty (29). The procedure types in Koulischer et al.’s study for the 47 of 65 patients included were unclear but the operations for the 65 patient group included gastric bypass or mini gastric bypass (60/65; 92%), and sleeve gastrectomy (5/65; 8%). The preoperative mean BMI for the total study population was 46.5 kg/m2. The preoperative mean VAS for back pain was 5.71.
Quality Assessment of Included Studies
Studies were assessed for bias and methodological quality using the MINORS criteria (Table 2). All studies were graded as low–moderate in quality.
Outcomes
Visual Analogue Score for Back Pain
Five studies used the VAS [5, 9, 10, 13, 14] and two studies used the NRS [11, 12] to quantitatively score back pain. Back pain was assessed preoperatively and at a median of 12 months follow-up postoperatively (range 3–24 months). Back pain was shown to be statistically significantly lower following bariatric surgery (Fig. 2) (seven studies [5, 9,10,11,12,13,14]; MD − 3.01; 95% CI − 4.19 to − 1.89; p < 0.001). Heterogeneity was high and statistically significant (I2 = 83%; p < 0.001).
Mean BMI Change
There was a statistically significant reduction in mean BMI following bariatric surgery (Fig. 3) (six studies [9,10,11,12,13,14]; MD − 12.23; 95% CI − 14.07 to − 10.39; p < 0.001). Heterogeneity was moderate but statistically non-significant (I2 = 55%; p = 0.05).
Quality of Life
Four studies reported on SF-36 scores before and after bariatric surgery [5, 9, 11, 12]. There was a statistically significant improvement in SF-36 physical component scores following bariatric surgery (Fig. 4) (four studies [5, 9, 11, 12]; MD 26.46; 95% CI 12.88 to 40.04; p < 0.001). Heterogeneity was high and statistically significant (I2 = 91%; p < 0.001).
Oswestry Disability Index
The impact of bariatric surgery on ODI scores was reported in three studies [9, 10, 12]. There was a statistically significant improvement (reduction) in ODI following bariatric surgery (Fig. 5) (three studies [9, 10, 12]; MD − 9.54; 95% CI − 15.41 to − 3.67; p < 0.001). Heterogeneity was moderately high but non-statistically significant (I2 = 63%; p = 0.07).
Discussion
This is the first meta-analysis addressing the impact of bariatric surgery on back pain in patients with obesity. We identified a total of seven cohort studies with 246 patients who underwent various bariatric procedures including sleeve gastrectomy, Roux-en-Y gastric bypass, duodenal switch, vertical banded gastroplasty and laparoscopic adjustable banding. All studies utilised the VAS or equivalent as an assessment tool for back pain symptoms before and after bariatric surgery.
Results of our meta-analysis revealed that back pain in obese patients was statistically significantly lower following bariatric surgery. This was observed across all seven studies which met the inclusion criteria. The mean change in VAS following bariatric surgery was 3 points. This is equivalent to the minimal clinically important difference for radiofrequency interventions for chronic back pain [15] suggesting a clinically important impact on back pain. Moreover, an improvement of the quality of life was reported in four of the studies based on SF-36 physical component score [5, 9, 11, 12]. Three studies reported a reduction in the Oswestry Disability Index score following bariatric surgery [9, 10, 12].
In exploring the causation of improved back pain following bariatric surgery, some authors have proposed that the overall improvement in wellbeing following metabolic surgery may account for alterations in back pain perception [9] as opposed to mechanical or musculoskeletal changes. Our meta-analysis provides some credence to this hypothesis with a demonstrable improvement in SF-36 physical component quality of life assessment. Alternatively, other groups contend that the improvement in back pain is more exclusively dependent on reduced axial load following post-bariatric intervention weight loss. The mechanisms leading to symptom improvement include changes in spinal biomechanics, a reduction in local inflammatory processes from mechanical loading, decreased muscular fatigue, and off-loading of the intervertebral disc or facet joints [9]. Further studies, incorporating pre- and postoperative spinal imaging, will be required to better understand the mechanism of improvements in back pain noted after bariatric surgery.
Weight loss following lifestyle modifications (change in diet and increase in physical activity) is also likely to have positive effect on back pain symptoms and quality of life. Non-surgical interventions produce less drastic and efficient weight loss over a longer period of time but it is difficult to compare the results [9]. Only Vincent et al. had a comparative non-surgical weight loss control group. They concluded that the bariatric group experienced significant improvement in back pain symptoms in the first 3 months. In contrast, there was no observed weight loss nor reduction in back pain severity in the control group. Some studies suggest that atherosclerosis, which is a common obesity-related condition, has additional consequence in regard to back pain. The four lumbar arteries and median sacral artery supply the lumbar segments and also perfuse the surrounding structures (intervertebral discs, nerve roots, and paraspinal muscles). Atherosclerosis of the abdominal aorta and of the lumbar arteries disrupts perfusion of lumbar structures, potentially resulting in structural degeneration and back pain [16]. Bariatric surgery has been shown to have significant improvements in markers of atherosclerosis and endothelial function [17] which may provide further explanation of the reductions in back pain noted in our study.
This study is not without limitations. Although we conducted an extensive search, the literature surrounding this topic is not broad. Previous studies have focussed more on the impact of bariatric surgery on conditions such as diabetes, cardiovascular disease and various musculoskeletal disorders generally and there is a paucity of studies focussing on back pain. We were able to identify only seven studies, which limits our study’s generalisability. The overall median follow-up was 12 months but three of the studies (Vincent et al., Josbeno et al., Cakir et al.) [5, 11, 14] had follow-up less than 6 months which may not be a sufficient time to observe the durability of the improvement in pain symptoms as well as the long-term effect of obesity surgery [9]. All seven studies were low–moderate in quality as assessed by the MINORS criteria of evidence and relatively small sample size. Finally, some of the surgery performed in the included articles is non-contemporaneous, and therefore, aspects of practice and outcomes may not be relevant to current metabolic surgery.
Despite these limitations, our study is a comprehensive analysis of the impact of bariatric surgery on back pain. It is evident that obesity surgery does have a favourable effect on the intensity of back pain and improves quality of life. Nonetheless, it should be reserved for obese patients with BMI > 35 kg/m2 with serious related comorbidities such as diabetes hypertension, cardiovascular disease and sleep apnoea [18]. Future studies are required to investigate the pathophysiologic mechanisms of development of back pain in obesity and its improvement following bariatric procedures.
References
Wang YC, McPherson K, Marsh T, et al. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–25. https://doi.org/10.1016/S0140-6736(11)60814-3.
Engin AB, Engin A. Obesity and lipotoxicity. 2017;960 https://doi.org/10.1007/978-3-319-48382-5.
Shanti H, Patel AG. Surgery for obesity. Medicine. 2019;47(3):184–7. https://doi.org/10.1016/j.mpmed.2018.12.011.
Andersen RE, Crespo CJ, Bartlett SJ, et al. Relationship between body weight gain and significant knee, hip, and back pain in older Americans. Obes Res. 2003;11(10):1159–62. https://doi.org/10.1038/oby.2003.159.
Vincent HK, Ben-David K, Cendan J, et al. Effects of bariatric surgery on joint pain: a review of emerging evidence. Surg Obes Relat Dis. 2010;6(4):451–60. https://doi.org/10.1016/j.soard.2010.03.284.
Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6. https://doi.org/10.1046/j.1445-2197.2003.02748.x.
Dersimonian; Laird, 9.4.3.1 Random effects (Dersimonian And Laird). Handbook-5-1.Cochrane.Org. [Online]. Available: https://handbook-5-1.cochrane.org/chapter_9/9_4_3_1_random_effects_dersimonian_and_laird_method_for.htm.
Grant J, Hunter A. Measuring inconsistency in knowledgebases. J Intell Inf Syst. 2006;27(2):159–84. https://doi.org/10.1007/s10844-006-2974-4.
Khoueir P, Black MH, Crookes PF, et al. Prospective assessment of axial back pain symptoms before and after bariatric weight reduction surgery. Spine J. 2009;9(6):454–63. https://doi.org/10.1016/j.spinee.2009.02.003.
Melissas J, Kontakis G, Volakakis E, et al. The effect of surgical weight reduction on low back pain. Obes Surg. 2005;15:378–81.
Josbeno DA, Jakicic JM, Hergenroeder A, et al. Physical activity and physical function changes in obese individuals after gastric bypass surgery. Surg Obes Relat Dis. 2010;6(4):361–6. https://doi.org/10.1016/j.soard.2008.08.003.
Koulischer S, Cadière B, Cadière GB, et al. Evolution des douleurs lombaires après chirurgie bariatrique. Rev Med Brux. 2015;36(3):147–51.
Lidar Z, Behrbalk E, Regev GJ, et al. Intervertebral disc height changes after weight reduction in morbidly obese patients and its effect on quality of life and radicular and low back pain. Spine (Phila Pa 1976). 2012;37(23):1947–52. https://doi.org/10.1097/BRS.0b013e31825fab16.
Çakır T, Oruç MT, Aslaner A, et al. The effects of laparoscopic sleeve gastrectomy on head, neck, shoulder, low back and knee pain of female patients. Int J Clin Exp Med. 2015;8(2):2668–73.
Noshchenko A, Lindley EM, Burger EL, et al. What is the clinical relevance of radiographic nonunion after single-level lumbar interbody arthrodesis in degenerative disc disease?: A meta-analysis of the YODA project database. Spine (Phila Pa 1976). 2016;41(1):9–17. https://doi.org/10.1097/BRS.0000000000001113.
Kauppila LI. Atherosclerosis and disc degeneration/low-back pain – a systematic review. J Vasc Surg. 2009;49(6):1629. https://doi.org/10.1016/j.jvs.2009.04.030.
Lupoli R, di Minno MND, Guidone C, et al. Effects of bariatric surgery on markers of subclinical atherosclerosis and endothelial function: a meta-analysis of literature studies. Int J Obes. 2016;40(3):395–402. https://doi.org/10.1038/ijo.2015.187.
Chen R, Takahashi T, Kanda T. Bariatric surgery for morbid obesity [14]. N Engl J Med. 2007;357(11):1159. https://doi.org/10.1093/med/9780199846085.003.0030.
Funding
Mr. Andrew Currie and Professor Christopher Pring are receivers of research grant from Medtronic, outside of the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval Statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Irena Stefanova and Andrew C Currie are considered joint first authors.
Rights and permissions
About this article
Cite this article
Stefanova, I., Currie, A.C., Newton, R.C. et al. A Meta-analysis of the Impact of Bariatric Surgery on Back Pain. OBES SURG 30, 3201–3207 (2020). https://doi.org/10.1007/s11695-020-04713-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04713-y