Abstract
Background
There have been enumerable studies on the effects of glucagon-like peptide-1 (GLP-1) on satiety and pancreatic islet function, stimulating the advocacy of surgical transposition of the ileum (rich in GLP-1-generating L-cells) higher in the gastrointestinal tract for earlier stimulation. In the Goto-Kakizaki rat with naturally occurring type 2 diabetes, we studied the influence of ileal exclusion (IE) and ileal resection (IR) on blood glucose, hemoglobin A1c (HbA1c), and GLP-1.
Methods
In six control (Ctrl), 10 IE, and 10 IR rats, over 12 weeks of follow-up, we determined blood glucose, HbA1c, and GLP-1.
Results
Two animals in the IE and IR groups did not survive to week 13. Both operated groups weighed more than the Ctrl group at baseline and at 13 weeks; thus, IE and IR did not retard weight gain (p < 0.05). All three groups were equally hyperglycemic at week 13: 255 ± 10.2 Ctrl, 262 ± 11.0 IE, 292 ± 17.8 IR (mg/dl ± SEM). The three groups had statistically identical markedly elevated HbA1c percentages at week 13: 14.7 ± 28 Ctrl, 11.7 ± 3.4 IE, 13.8 ± 3.5 IR (% ± SEM). The end-study GLP-1 values (pM ± SEM) were 5 ± 0.9 Ctrl, 33 ± 8.9 IE, and 25 ± 6.7 IR. P values for intergroup differences were IE vs. Ctrl 0.02, IR vs. Ctrl 0.02, and IE vs. IR 0.59.
Conclusions
Neither IE nor IR resulted in a decrease in the mean GLP-1 level. On the contrary, the exclusion or resection of the L-cell rich ileum raised GLP-1 levels 5- to 6-fold. This increase in the GLP-1 was not associated with the mitigation of hyperglycemia or elevated HbA1c levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There have been enumerable studies published demonstrating the effects of L-cell elaborated glucagon-like peptide-1 (GLP-1) on satiety and pancreatic islet cell function. The hormone works in concert with peptide YY (PYY), the PYY (3–36) form, one augmenting the actions of the other in an interdependent biofeedback loop [1]. GLP-1 and PYY are secreted in increasing amounts as a function of the caloric content of ingested food [2]. Their quantitative response is influenced by the intestinal site of stimulation [3–5], bile acids [6], central neural and vagal mechanisms [7–9], and other hormones (vasoactive intestinal polypeptide [10], gastrin [11]). The hormones centrally stimulate the arcuate nucleus of the hypothalmus, resulting in a reduced sensation of hunger and an increased sensation of satiety [12–14]. GLP-1 is involved in the “ileal brake” phenomena of delayed gastric emptying, delayed mouth to cecum transit time, and a decreased jejunal wave pressure [15–17]. GLP-1 also contributes to the incretin effect, defined as the concentration of the insulin released by oral glucose stimulation that exceeds the insulin concentration elicited by the same amount of intravenous glucose [18]. With respect to circulating glucose control, GLP-1 stimulates glucose-dependent insulin secretion, preinsulin gene expression, β-cell proliferation, and anti-apoptotic pathways and inhibits glucagon release [19, 20].
These effects of GLP-1 have stimulated experimental metabolic/bariatric operations to mitigate type 2 diabetes. Most prominent among them has been ileal transposition higher in the gastrointestinal tract, first advocated by Edward Mason [21] and now practiced, in one form or another, by several surgeons worldwide [22, 23]. Rationale for ileal transposition can be found in several rat experiments [24–26].
We have recently completed a study measuring GLP-1, PYY, and leptin levels after the stimulation of the terminal ileum or cecum by a static infusion of a food hydrolysate in morbidly obese patients undergoing a duodenal switch procedure [27]. We found that direct stimulation of both the human terminal ileum and cecum elicits plasma GLP-1 and PYY elevations and concurrent leptin decreases. The ileal GLP-1 and PYY elevations exceeded those of the cecum; the hydrolysate effect on the PYY plasma concentration was about three-fold than that of the GLP-1. All hormonal changes reached their maximum at 90 to 100 min. It is questionable, therefore, that the translocation of a segment of the ileum by ileal transposition would enhance the immediate postprandial release of GLP-1 and PYY over that obtained by direct stimulation in situ and, thereby, produce earlier satiety. This work, however, does not challenge whatever effect GLP-1 has on type 2 diabetes and how the elaboration of GLP-1 is related to ileal integrity.
We thus undertook a study in an animal model of naturally occurring type 2 diabetes, the Goto-Kakizaki (GK) rat, of the influence on blood glucose levels, hemoglobin A1c (HbA1c), and GLP-1 subsequent to ileal exclusion (IE) and ileal resection (IR).
Methods
Protocol
Phase I—Establishment of surgical and blood drawing techniques and appropriate anesthesia in 10 animals, four Wistar rats and six GK rats.
Phase II—Planned study of 26 GK rats blindly and randomly divided by animal age into three cohorts, namely six control (Ctrl), 10 IE, and 10 IR animals. Each rat was scheduled for 12 weeks of follow-up with no oral intake restrictions. Blood draws at surgery (week 0), at mid-term (week 9), and at the end of the study (week 13), by cecal or tail veins, were obtained for blood glucose levels. Variability in blood draw sites was due to difficulty in obtaining sufficient sample volumes from a single site. Blood draws by cardiac puncture at week 13 at the end of the study were used for blood glucose, HbA1c, and GLP-1 level determinations. In addition, animal weights were recorded throughout the study, and intestinal lengths were measured at autopsy.
Animal Care
The Wistar and GK rats, 9–10 weeks of age, weighing 275–300 g, were obtained from a commercial vendor. The animals were housed in individual cages at a constant temperature (70 °F) with a 12-h day/night light cycle. All animals received standard species-specific chow (Ralston Purina Co., St. Louis, MO or Harlan Teklad, Indianapolis, IN) and water ad libitum. The animals in phase II, after a 1-week acclimatization period, were randomized to three groups as follows: Ctrl, IE, and IR.
For pain relief postoperatively, the rats were given Ketoprofen 5 mg/kg SQ immediately after surgery, followed by Ibuprofen in a 500-ml water bottle at a dose of 15 mg/kg for 3 days. The rats were given sulfa-Trimethoprim elixir in the water bottle at 1 mg/ml for 6 days of the 12-week follow-up. The animals were closely monitored, and any animal in distress was euthanized.
Surgery
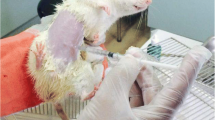
Surgery consisted of either distal IE or distal IR. IE was performed by a side-to-side ileocecal anastomosis using running 6/0 Monocryle suture, approximately 15–20 cm from the ileocecal valve, with ligature closure of the distal ileum with 3/0 Ethibond suture isoperistaltic from the anastomosis. The excluded ileum was retained in the abdominal cavity, its blood supply intact, with egress into the cecum via the ileocecal valve. IR was performed in a similar fashion except for the ligature of the terminal ileum with 3/0 Ethibond at the ileocecal valve and resection of the terminal ileum using multiple 6/0 Ethibond sutures for the ligation of the ileal mesentery. Peritoneal/abdominal wall closure was performed with a running 3/0 Vicryl suture and skin closure with a running 4/0 Vicryl suture. Surgery was performed under a mixture of ketamine (75 mg/kg) and xylazine (10 mg/kg) intra-peritoneal anesthesia.
Termination Euthanasia
At week 13 (12-week follow-up), the animals were anesthetized with the same ketamine/xylazine mixture for cardiac blood draws and then sacrificed by intravenous injection of pentobarbital and phenytoin (1 ml/5–10 kg).
Blood Samples and Analyses
The amounts of blood utilized for analyses were glucose 0.2 ml, HbA1c 0.5 ml, and GLP-1 0.5 ml. Analytical chemistry methods employed were glucose by oxidase biosensor, HbA1c by endpoint reflectance spectrophotometry with direct percent A1c calculation, and GLP-1 by enzyme-linked immunosorbent assay.
Statistics
Minimum sample size was determined by the following:
for a confidence level of 95 % and an expected standard deviation >6.75 % and a difference value >5.5 %. On this basis, a minimum sample size of six animals per group was calculated. Knowing the fragility of the GK animal model, the authors allowed up to 40 % animal loss in the study. Thus, the 20 % actual loss in the IR and IE groups fell within acceptable limits. Group comparisons were performed by Student’s t test.
Results
Study Protocol
Two animals in the IE group and two in the IR group did not survive to week 13. Tail blood draw glucose values were on the average of 23.4 % lower than mesenteric vein samples.
Weight
At week 0, the mean weights (gm ± SEM) for the three groups were Ctrl 350 ± 5.4, IE 371 ± 5.0, and IR 363 ± 5.7. The p values for the differences between groups were IE vs. IR 0.32, IE vs. Ctrl 0.02, and IR vs. Ctrl 0.13. Thus, the six Ctrl animals weighed statistically significantly less than the IE animals at the initiation of the study.
At week 13, the average weights (gm ± SEM) for the three groups were Ctrl 379 ± 10.4, IE 424 ± 5.0, and IR 410 ± 7.9. The p values for the differences between groups were: IE vs. IR 0.15, IE vs. Ctrl 0.01, and IR vs. Ctrl 0.05. Thus, both operated groups weighed statistically significantly more than the non-operated controls, and there was no statistical significant difference in weight between the IE and IR groups.
The average weight gain in the Ctrl was 29 g, in the IE group 53 mg, and in the IR group 47 g. IE or IR surgery, therefore, did not retard weight gain and exceeded the actual average weight gain in the non-operated Ctrl group (p < 0.05).
Small Intestinal Lengths
At week 13, the measured average intestinal length from the pylorus to the ileocecal anastomosis was 73 ± 3.9 (SEM) cm in the IE group and 78 ± 4.0 cm in the IR group, with the average length of the anastomosis to the ileocecal valve measured at 25 ± 3.3 cm in the IE group. The Ctrl group pylorus to ileocecal valve distance averaged 85 ± 2.3 cm.
Blood Glucose
Duplicate values for all blood glucose determinations as well as anatomic sites of blood drawing are given in Table 1. At baseline, blood drawings were made from the tail vein in the Ctrl group and from a mesenteric vein in the IE and IR groups. A calculated correction factor of 23.4 % was used to compensate for the difference in peripheral and central glucose determinations. The mean blood glucose values (mg/dl ± SEM) by tail vein determinations are given in Table 2 and plotted in Fig. 1. The animals in the Ctrl group became progressively more hyperglycemic from week 0 to week 13. The IE and IR animals were hyperglycemic in week 0, markedly dropped their glucose levels in week 9, and regained their preoperative hyperglycemia in week 13. At week 13, the three groups were essentially equally hyperglycemic.
HgA1c
HgA1c levels were determined only at the termination of the study, week 13, by cardiac puncture under anesthesia prior to euthanasia. The value for each animal plus the group means (% ± SEM) are shown in Table 3 and plotted in Fig. 2. The p values for intergroup differences were all NS: IE vs. IR 0.61, IE vs. Ctrl 0.52, and IR vs. Ctrl 0.85. Though certain individual animals maintained HgA1c levels <6 %, the majority of the animals had markedly elevated HgA1c values, in keeping with the group means.
GLP-1
GLP-1 levels were determined only at the termination of the study, week 13, by cardiac puncture under anesthesia prior to euthanasia. The values for each animal plus the group values ± means (pM ± SEM) are shown in Table 4 and plotted in Fig. 3. The p values for intergroup differences were statistically significant for IE vs. Ctrl (p = 0.02) and IR vs. Ctrl (p = 0.02), but not for IE vs. IR (p = 0.59). The mean GLP-1 value for the IE group (33 pM ± 8.9 SEM) was over six-fold that of the Ctrl group (5 pM ± 0.9 SEM). The mean GLP-1 value for the IR group (25 pM ± 6.7 SEM) was five-fold that of the Ctrl group. Neither IE nor IR resulted in a decrease in the mean circulating GLP-1 level but, instead, a marked increase in the mean GLP-1 level occurred.
Discussion
This study questions both the effect of GLP-1 on type 2 diabetes and the role of the ileum per se in glucose homeostasis. Simply stated, if the ileal segment of the intestinal tract plays a role in glucose regulation, and this effect may be enhanced by ileal transposition higher in the intestinal tract, why then do IE and actual IR lead to a marked increase (5–6-fold), and not a decrease, in the circulating GLP-1 level? And if an increase in GLP-1 is beneficial in type 2 diabetes, why did it not affect the hyperglycemia and elevated HbA1c levels in these GK rats?
In this animal study, the operative procedures did not induce weight loss; indeed, weight gain in the IE and IR groups statistically significantly exceeded that in the Ctrl group. This finding may have influenced the study’s results with regard to glucose metabolism and the rat model’s type 2 diabetes.
We purposely studied IR as well as IE since we postulated that the bypassed or excluded ileum might still be stimulated to excrete L-cell-derived GLP-1 by a neurohormonal pathway. When, however, the ileum is excised and there is a five-fold increase in circulating GLP-1, this increased incretin level cannot have been generated from ileal mucosal L-cells. Since the entire gastrointestinal tract is rich in L-cells, with the concentration of L-cells increasing from proximal to distal bowel [2, 28], the increased circulating GLP-1 came from elsewhere in the gut. Possibly, in the absence of the terminal ileum and the ileocecal valve, this site was the now earlier stimulated cecum, which has a marked capacity for GLP-1 elaboration [27]. In any event, the ileum may have a cardinal role in GLP-1 secretion, but this function is not intrinsic to the ileal L-cells and may actually be heightened by the absence of the ileum from the functioning intestinal tract.
Contrary to the general belief that the ileum is a major site of GLP-1 production, we have created in this experiment, in this rat model, a marked increase in circulating GLP-1 by IE or IR. At the same time, having now generated sustained, greatly elevated GLP-1 levels, there was no amelioration of the elevated blood glucose levels or HbA1c. These animals had no benefit with regard to their type 2 diabetes.
This study, however, does not challenge the relationship of GLP-1 and type 2 diabetes in humans, nor does it question a role for the ileum in human hormonal regulation of glucose homeostasis. It does, however, place into question the mechanism for the GLP-1 effect and its elaboration in this rat model. Further, these data raise a serious doubt of the applicability of findings in the GK rat model to humans or, for that matter, any rat model. Rats are relatively inexpensive and easily managed experimental subjects, but rat findings may have little or no bearing on human physiology, biochemistry, and disease.
The postulate that rats are not good models for humans, in particular when the ileum is involved, can be illustrated by the history of the partial ileal bypass operation for hyperlipidemia. In 1964, the first author demonstrated in rabbits and in pigs, and subsequently in humans, that the exclusion of the distal ileum markedly reduced circulating cholesterol levels [29]. The operative mechanism for partial ileal bypass is increased cholesterol and bile acid excretion, resulting in increased cholesterol synthesis and its conversion to bile acids, with increased cholesterol turnover, but a resultant decrease in the cholesterol body pools [30]. This experimental work was repeated by several authors in several different species, including the dog [31], the White Carneau pigeon [32], and the Rhesus monkey [33, 34]—all with comparable results. There was, however, a statement made by the group of Brown and Goldstein, who won the Nobel Prize for their elucidation of the LDL-receptor, that questioned the validity of the partial ileal bypass concept since they could not duplicate our findings in a rat preparation. Apparently, the rat can compensate for the intestinal loss of cholesterol and bile acids by an extraordinary increase in cholesterol synthesis.
The advent of the partial ileal bypass procedure led to the Program on the Surgical Control of the Hyperlipidemias (POSCH) trial, a $65 million dollar NHLBI investigator-initiated, four institutions, secondary intervention, randomized controlled trial, which was the first statistically significant study to show the clinical and radiographic efficacy of lowering the plasma cholesterol, in particular the LDL-cholesterol fraction [35]. POSCH outcomes included the statistically significant reduction of the combined endpoint of death and recurrent myocardial infarction, occurrence of peripheral vascular disease, serial coronary arteriography atherosclerotic progression with actual significant lesion regression, and overall mortality [35–37]. The increase in life expectancy in the partial ileal bypass intervention group over the control group was seen to persist for over 25 years [38]. All this may not have come to pass if the initial animal investigations were carried out in the rat.
In summary, in the type 2 diabetic GK rat, IE and IR raised the circulating GLP-1 concentration 5- to 6-fold. This increase in GLP-1 was not associated with the mitigation of hyperglycemia or elevated HbA1c levels. These outcomes may not have translational relevance to human responses.
References
Naslund E, Bogefors J, Skogar S, et al. GLP-1 slows solid gastric emptying and inhibits insulin, glucagon, and PYY release in humans. Am J Physiol Regul Integr Comp Physiol. 1999;277:R910–6.
Adrian TE, Ferre G-L, Bacarese-Hamilton AJ, et al. Human distribution and release of a putative new gut hormone, peptide YY. Gastroenterology. 1985;89:1070–7.
Greeley Jr GH, Hashimoto T, Izukura M, et al. A comparison of intraduodenally and intracolonically administered nutrients on the release of peptide-YY in the dog. Endocrinology. 1989;125:1761–5.
Zhang T, Brubaker PL, Thompson JC, et al. Characterization of peptide-YY release in response to intracolonic infusion of amino acids. Endocrinology. 1993;132:553–7.
Aponte GW, Fink AS, Meyer JH, et al. Regional distribution and release of peptide YY with fatty acids of different chain length. Am J Physiol. 1985;249:G745–50.
Adrian TE, Ballantyne GH, Longo WE, et al. Deoxycholate is an important releaser of peptide YY and enteroglucagon from the human colon. Gut. 1993;34:1219–24.
Onaga T, Zabielski R, Kato S. Multiple regulation of peptide YY secretion in the digestive tract. Peptides. 2002;23:279–90.
Zhang T, Uchida T, Gomez G, et al. Neural regulation of peptide YY secretion. Regul Pept. 1993;48:321–8.
Rudnicki M, Rigel DF, McFadden DW. Vagal cooling blocks circulating neuropeptide Y (NPY), peptide YY (PYY), and pancreatic polypeptide (PP) release. J Surg Res. 1991;51:40–5.
Ballantyne GH, Goldenring JR, Savoca PE, et al. Cyclic AMP-mediated release of peptide YY (PYY) from the isolated perfused rabbit distal colon. Regul Pept. 1993;47:117–26.
Greeley Jr GH, Jeng YJ, Gomez G, et al. Evidence for regulation of peptide-YY release by the proximal gut. Endocrinology. 1989;124:1438–43.
Hernandez EJ, Whitcomb DC, Vigna SR, et al. Saturable binding of circulating peptide YY in the dorsal vagal complex of rats. Am J Physiol Gastrointest Liver Physiol. 1994;226:G511–6.
Druce MR, Small CJ, Bloom SR. Minireview: Gut peptides regulating satiety. Endocrinology. 2004;145:2660–5.
Korner J, Leibel RL. To eat or not to eat—how the gut talks to the brain. N Engl J Med. 2003;349:926–8.
Savage AP, Adrian TE, Carolan G, et al. Effects of peptide YY (PYY) on mouth to caecum intestinal transit time and on the rate of gastric emptying in healthy volunteers. Gut. 1987;28:166–70.
Spiller RC, Trotman IF, Adrian TE, et al. Further characterization of the ‘ileal brake’ reflex in man—effect of ileal infusion of partial digests of fat, protein, and starch on jejunal motility and release of neurotensin, enteroglucagon, and peptide YY. Gut. 1988;29:1042–51.
Spiller RC, Trotman IF, Higgins BE, et al. The ileal brake—inhibition of jejunal motility after ileal fat perfusion in man. Gut. 1984;25:365–74.
Tolhurst G, Reimann F, Gribble FM. Nutritional regulation of glucagon-like peptide-1 secretion. J Physiol. 2009;587:27–32.
Lim GE, Brubaker PL. Glucagon-like peptide 1 secretion by the L-cell. The view from within. Diabetes. 2006;55:S70–7.
Drucker DJ. The biology of incretin hormones. Cell Metab. 2006;3:153–65.
Mason EE. Ileal transposition and enteroglucagon/GLP-1 in obesity (and diabetic?) surgery. Obes Surg. 1999;9:223–8.
Gagner M. Surgical treatment of nonseverely obese patients with type 2 diabetes mellitus: sleeve gastrectomy with ileal transposition (SGIT) is the same as the neuroendocrine brake (NEB) procedure or ileal interposition associated with sleeve gastrectomy (II-SG), but ileal interposition with diverted sleeve gastrectomy (II-DSG) is the same as duodenal switch. Surg Endosc. 2001;25:655–6.
DePaula AL, Stival AR, DePaula CC, et al. Surgical treatment of type 2 diabetes in patients with BMI below 35: mid-term outcomes of the laparoscopic ileal interposition associated with a sleeve gastrectomy in 202 consecutive cases. J Gastrointest Surg. 2012;16:967–76.
Wang TT, Hu SY, Gao HD, et al. Ileal transposition controls diabetes as well as modified duodenal jejunal bypass with better lipid lowering in a nonobese rat model of type II diabetes by increasing GLP-1. Ann Surg. 2008;247:968–75.
Tsuchiga T, Kalogeris TJ, Tso P. Ileal transposition into the upper jejunum affects lipid and bile salt absorption in rats. Am J Physiol. 1996;271:G681–91.
Strader AD, Vahl TP, Jandacek RJ, et al. Weight loss through ileal transposition is accompanied by increased ileal hormone secretion and synthesis in rats. Am J Physiol Endocrinol Metab. 2005;288:E447–53.
Buchwald H, Dorman RB, Rasmus NF, Michalek VN, Landvik NM, Ikramuddin S. Effects on GLP-1, PYY, and leptin by direct stimulation of terminal ileum and cecum in humans: implications for ileal transposition. Surg Obes Relat Dis 2014. doi:10.1016/j.soard.2014.01.032.
Nilsson O, Bilchik AJ, Goldenring JR, et al. Distribution and immunocytochemical colocalization of peptide YY and enteroglucagon in endocrine cells of the rabbit colon. Endocrinology. 1991;129:139–48.
Buchwald H. Lowering of cholesterol absorption and blood levels by ileal exclusion: experimental basis and preliminary clinical report. Circulation. 1964;29:713–20.
Moore RB, Frantz Jr ID, Buchwald H. Changes in cholesterol pool size, turnover rate, and fecal bile acid and sterol excretion after partial ileal bypass in hypercholesterolemic patients. Surgery. 1969;65:98–108.
Scott Jr HW, Stephenson Jr SE, Younger R, et al. Prevention of experimental atherosclerosis by ileal bypass: 20 % cholesterol diet and I-131 induced hypothyroidism in dogs. Ann Surg. 1966;163:795–807.
Gomes MM, Kottke BA, Bernatz P, et al. Effect of ileal bypass on aortic atherosclerosis of white Carneau pigeons. Surgery. 1971;70:353–8.
Shepard GH, Wimberly JE, Younger RK, et al. Effects of bypass of the distal third of the small intestine on experimental hypercholesterolemia and atherosclerosis in rhesus monkeys. Surg Forum. 1968;19:302.
Scott Jr HW, Stephenson Jr SE, Hayes CW, et al. Effects of bypass of the distal fourth of small intestine on experimental hypercholesterolemia and atherosclerosis in rhesus monkeys. Surg Gynecol Obstet. 1967;125:3–12.
Buchwald H, Varco RL, Matts JP, et al. Effect of partial ileal bypass surgery on mortality and morbidity from coronary heart disease in patients with hypercholesterolemia. Report of the Program on the Surgical Control of the Hyperlipidemias (POSCH). N Engl J Med. 1990;323:946–55.
Buchwald H, Matts JP, Fitch LL, et al. Changes in sequential coronary arteriograms and subsequent coronary events. JAMA. 1992;268:1429–33.
Buchwald H, Campos CT, Varco RL, et al. Effective lipid modification by partial ileal bypass reduced long-term coronary heart disease mortality and morbidity: five-year posttrial follow-up report from the POSCH. Arch Intern Med. 1998;158:1253–61.
Buchwald H, Rudser KD, Williams SE, et al. Overall mortality, incremental life expectancy, and cause of death at 25-years in the Program on the Surgical Control of the Hyperlipidemias (POSCH). Ann Surg. 2010;251(6):1034–40.
Acknwledgments
Funded by a grant from the Robert and Katherine Goodale Chair in Minimally Invasive Surgery, Department of Surgery, University of Minnesota.
Conflict of Interest
Henry Buchwald, Hector J. Menchaca, Van N. Michalek, and Nestor T. Bertin Suguitani have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buchwald, H., Menchaca, H.J., Michalek, V.N. et al. Ileal Effect on Blood Glucose, HbA1c, and GLP-1 in Goto-Kakizaki Rats. OBES SURG 24, 1954–1960 (2014). https://doi.org/10.1007/s11695-014-1307-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1307-x