Abstract
Background
The objective of this study was to evaluate the mid-term outcomes of the laparoscopic ileal interposition into the jejunum (JII-SG) or into the duodenum (DII-SG) associated with sleeve gastrectomy for type 2 diabetes mellitus (T2DM) patients with BMI below 35.
Methods
The procedures were performed on 202 consecutive patients. Mean age was 52.2 ± 7.5. Mean duration of T2DM was 9.8 ± 5.2 years. Insulin therapy was used by 41.1%. Dyslipidemia was observed in 78.2%, hypertension in 67.3%, nephropathy in 49.5%, retinopathy in 31.2%, coronary heart disease in 11.9%, and other cardiovascular events in 12.9%.
Results
Mean follow-up was 39.1 months (range, 25–61). Early and late mortality was 0.99% and 1.0%, respectively. Early reoperation was performed in 2.5%. Early and late major complications were 8.4% and 3.5%. Early most frequent complications were pneumonia and ileus. Intestinal obstruction was diagnosed in 1.5%. Mean BMI decreased from 29.7 to 23.5 kg/m2, mean fasting glucose from 202.1 to 112.2 mg/dl, and mean postprandial glucose from 263.3 to 130 mg/dl. Triglycerides diminished from a mean of 273.4 to 110.3 mg/dl and cholesterol from a mean of 204.7 to 160.1 mg/dl. Hypertension was resolved in 87.5%. Mean hemoglobin A1c (HbA1c) decreased from 8.7 to 6.2% after the JII-SG and to 5.9% following the DII-SG. HbA1c below 7% was seen in 89.9% of the patients and below 6.5% in 78.3%. Overall, 86.4% of patients were off antidiabetic medications.
Conclusion
Both JII-SG and DII-SG demonstrated to be safe, effective, and long-lasting alternatives for the treatment of T2DM patients with BMI <35. Beyond glycemic control, other benefits were achieved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) and obesity are predicted to be two of the greatest public health problems of the coming decades globally.1 Most people with diabetes will die or be disabled as a consequence of vascular complications.2
The high cardiovascular (CV) risk that diabetes induces is probably better addressed by approaching not only hyperglycemia but also the usual coexisting risk factors.3 A strategy of intensive glucose control to lower the hemoglobin A1c (HbA1c) value to 6.5% yielded a 10% relative reduction in major macrovascular and microvascular events.4 In another study,5 an intensive glucose control in patients with poorly controlled T2DM had no significant effect on the rates of major CV events, deaths, or microvascular complications. In the ACCORD study, high-risk T2DM patients submitted to intensive therapy to lower HbA1c had an increased mortality and no significantly reduced major CV events, as compared with standard therapy.6
Surgical procedures that induce weight loss lead to the remission of T2DM in the majority of morbidly obese patients.7 The possibility that gastrointestinal surgeries may lead to improvement in glucose homeostasis through mechanisms beyond reduced food intake and weight loss have been extensively explored.8 A recent review of available data in humans concluded that, while caloric restriction or Roux-en-Y gastric bypass (RYGB) leads to gains in insulin sensitivity that is proportionate to the weight loss, biliopancreatic diversion is consistently associated with complete reversal of insulin resistance, occurring before significant weight loss and disproportionate to the weight lost.9
Recently, we demonstrated the effects of laparoscopic ileal interposition into the jejunum (JII-SG) and into the duodenum (DII-SG) associated with a sleeve gastrectomy on the different components of the metabolic syndrome for a population of T2DM patients with body mass index (BMI) lower than 35.10 Although the cellular mechanisms underlying the surgery-induced increase in insulin sensitivity and ß cell function remain speculative, the operation intends to primarily target the pathophysiology of the underlying disease. The first characteristic of the operation is to provide an early contact of ingested nutrients to the interposed distal ileum resulting in an early and significant rise of glucagon-like peptide 1. This corrects the defective early (first-phase) insulin secretion. The second characteristic is the correction of the defective amplification of the late-phase plasma insulin response to glucose by glucose-dependent insulinotropic polypeptide (GIP). Both characteristics were addressed in a recent publication of the hormonal changes before and after ileal interposition with sleeve gastrectomy.11 The third characteristic is the amelioration of insulin resistance. Flatt12 suggested that the most attractive hypotheses for rapid improvement of insulin sensitivity and associated pancreatic beta-cell function are related to surgical ablation of GIP-secreting intestinal K-cells. Another possibility could be related to short-circuiting the enterohepatic bile acid recycling through an early reabsorption of primary bile acids.13 The fourth and fifth characteristics of this operation are related to the resection of part of the stomach in order to provide long-lasting control of obesity, to decrease caloric intake, to accelerate gastric emptying, and to decrease the circulating levels of ghrelin. Based on the above pathophysiology, we assumed the possibility that the DII-SG would give better results in relation to JII-SG as it addresses more aspects of the pathophysiology of the disease. Rubino et al.14 demonstrated that the exclusion of the duodenum promoted improvement in glycemic control based on the foregut theory. The JII-SG encompassed the hindgut theory, while the DII-SG combined both the hindgut and foregut hypotheses. An evidence of the better performance of the DII-SG was provided by a recent publication of diabetic patients with BMI below 30 submitted to the DII-SG. Nearly 95% of the patients achieved an adequate glycemic control (HbA1c < 7%) without antidiabetic medication.15 Moreover, after a prospective randomized controlled study comparing the two versions, it was observed that the DII-SG patients had a better performance compared to the JII-SG at 2 years.16
The primary goal of this study was to evaluate mid-term outcomes of the laparoscopic ileal interposition into the jejunum or into the duodenum associated with sleeve gastrectomy for T2DM patients with BMI below 35.
Methods
This was a retrospective review of our existing diabetic database. According to the current protocol, we identified a total of 202 consecutive diabetic patients with BMI below 35 that were operated from April 2005 to early February 2008. All patients met the criteria of a minimum of 2 years of follow-up to participate in this study and the intermediate outcomes (2–5 years) were analyzed. There was no intention to compare the two versions of ileal interposition associated to sleeve gastrectomy. Both operations were conducted simultaneously. Although we recognized that the clinical presentation and phenotype of patients were not adequate indicators of diabetic severity, patients with longer duration of diabetes, with symptoms and findings suggestive of gastroparesis, low C-peptide levels (<1.5 nmol/l), and high glycemic and HbA1c levels were submitted to the DII-SG. However, the groups were quite comparable regarding age, gender, weight, and BMI. The inclusion criteria included patients who had T2DM for at least 3 years. Associated criteria included documentation of HbA1c > 7.5% for at least 3 months, stable weight [defined as no significant change (>3%) over the 3 months prior to enrollment], and evidence of stable treatment with oral hypoglycemic therapy and or insulin for at least 12 months. Patients were diagnosed according to the American Diabetes Association (ADA) criteria.17 The exclusions involved C-peptide levels below 0.5 nmol/l, positive anti-glutamic acid decarboxylase test, elderly patients (>75 years), previous major upper abdominal surgery, pregnancy, patients with malignant or debilitating diseases, severe pulmonary or cardiac diseases, severe renal disease (glomerular filtration rate below 30 ml/min), taking appetite suppressant medication, eating disorder such as bulimia or binge eating, and obesity due to any other endocrine disorder. Definition of remission of T2DM followed the most recent consensus statement of ADA, although it expressed authors’ opinions and not an official position of ADA.18 Complete remission was defined as a return to “normal” measures of glucose metabolism, HA1c below 6, fasting glucose (FPG) < 100 mg/dl, for at least 1 year, with no active pharmacologic therapy. Prolonged remission was defined as complete remission for at least 5 years duration and finally, partial remission, as HA1c < 6.5%, FPG 100–125 mg/dl for at least 1 year, in the absence of active pharmacologic therapy.
Demographic data, status of diabetes and comorbidities, duration of disease, and medication usage were determined by interview and specific tests. Weight and height were measured and used to calculate BMI. Associated diseases or complications of T2DM were diagnosed in all patients. Dyslipidemia was diagnosed in 78.2% of patients, arterial hypertension in 67.3%, nephropathy (urinary excretion of albumin >30 mcg/min and/or creatinine clearance <80 ml/min) was characterized in 49.5%, retinopathy in 31.2%, neuropathy in 28.2%, gastroesophageal reflux disease (GERD) in 44.6%, urinary lithiasis in 12.4%, coronary heart disease in 11.9%, and other cardiovascular events were documented in 12.9%.
Biochemical markers of T2DM were obtained and included FPG, postprandial plasma glucose (PPG), and HbA1c. Lipid profile was also evaluated.
Technique
Two versions were performed: a segment of ileum interposed up to the jejunum associated with a sleeve gastrectomy or a segment of ileum interposed up to the duodenum associated with a sleeve gastrectomy, diverting the duodenum. The detailed technique19 is described in Fig. 1.
Postoperatively, all patients were monitored four times daily through capillary plasma glucose and were under insulin therapy according to a sliding scale for 1 month. An appropriate and restricted diet was suggested.
Outcome Measures
After 1 month, all antidiabetic medications were discontinued. If necessary, oral hypoglycemic agents were used. Metformin was the first choice. Adjustments were made according to glucose levels. The goal was to have patients with HbA1c below 6.5% without medications. Outcome measures were collected prospectively. Major CV events included myocardial infarction, stroke, death from CV causes, congestive heart failure, arrhythmia, CV surgery, or intervention.
Patient and laboratory evaluations were scheduled every 3 months during the first year after surgery, every 6 months during the second year, and yearly thereafter. The Ethics Committee of the Hospital approved the study, and all subjects gave written informed consent.
Statistical Analysis
The significance level adopted was 5%. The results were expressed in mean, frequency, percentage, minimum, maximum, and standard deviation. The one-way ANOVA for repeated measures was used to verify variations of BMI twice. Logistic regression models were fitted to estimate predictors of success. Stepwise forward selection was used for the regression modeling.
Results
Subject characteristics are presented in Table 1. Overall mean age was 52.2 ± 7.5 years. In the JII-SG group, the mean age was 53 ± 7.4 and was 50.9 ± 7.2 for the DII-SG patients (p = 0.09). The mean percentage of males was 70.8%, with no difference between the JII-SG and DII-SG groups (p = 0.98). Duration of diabetes was greater for the DII-SG group of patients, with a mean of 10.1 ± 4.3 years. In the JII-SG group, patients had diabetes for a mean of 9.1 ± 5.4 years (p = 0.14). Insulin was used by 46.8% of the patients in the DII-SG group and by 36.6% in the JII-SG (p = 0.17).
All the procedures were performed laparoscopically. The ileum was interposed into the jejunum in 125 patients and into the duodenum in 77. Of the 202 patients, 96 (47.5%) underwent an associated procedure, including 21(10.4%) cholecystectomies with cholangiography, 43 (21.3%) adhesiolysis, 17 (8.4%) hiatal hernia repair, 20 (9.9%) liver biopsy, and 1 (0.5%) enterectomy due to Meckel’s diverticulum.
Early and late mortality and major morbidity are listed in Table 2. Early mortality was 0.99%. These two patients underwent the JII-SG. There was one dehiscence from a Meckel’s diverticulectomy. This patient was reoperated but died from abdominal sepsis. The other death was related to an acute renal failure. This patient was discharged from the hospital after 4 days and was readmitted with nausea and severe dehydration 7 days later. Thirty-day major complications were diagnosed in 7.2% of the JII-SG patients and in 10.4% of the DII-SG (p = 0.44). Late mortality (>30 days < 5 years) was 1.0%. One late death occurred in the JII-SG group and the other one in the DII-SG. One death was related to intestinal obstruction and the other to a Guillian–Barrè syndrome in a patient with advanced renal disease. Both early and late mortalities were clearly related to underlying associated diseases, especially renal disease. Late complications were slightly more frequent following the DII-SG (p = 0.06). Late adverse events included: GERD-related symptoms that required medication in 57/28.8%, food intolerance in 9/4.5%, urinary tract infection in 8/4%, diarrhea in 6/3%, gallstone in 24/12.1%, herpes zoster in 1/0.5%, alcoholic cirrhosis in 1/0.5%, urinary lithiasis in 10/5.1%, and seizures in 1/0.5%. Late in the follow-up period, a variety of procedures were performed for different causes, including nephrectomy (adenocarcinoma) in one, prostatectomy in one, cholecystectomy in nine, appendectomy in one, pulmonary lobectomy (breast cancer) in one, scalp reconstruction in one, and inguinal hernia repair in one.
Mean follow-up was 39.1 months, range 25 to 61. There was a similar follow-up for both groups, with 39 ± 9.4 months for the JII-SG and 40 ± 8.4 for the DII-SG (p = 0.14). The mean BMI decreased from 29.7 ± 3.5 kg/m2 preoperatively to 23.5 ± 3.1 kg/m2 (p < 0.0001) postoperatively. The difference was not statistically significant between the two procedures (p = 0.19). The mean BMI decreased from 30.3 ± 3.6 kg/m2 preoperatively to 23.6 ± 3.2 kg/m2 after the JII-SG (p < 0.001) and from 29.6 ± 3.3 to 23.3 ± 2.6 kg/m2 after the II-DSG (p < 0.001). The mean percentage of weight loss was 22.5% of the initial weight. Five patients (2.5%) were underweight (BMI < 18.5 kg/m2), 137 (69.2%) had BMI 18.5–25 kg/m2, and 56 (28.3%) had BMI above 25 kg/m2. The weight loss relative to baseline BMI is demonstrated in Fig. 2.
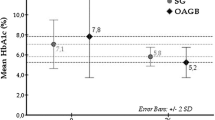
Hemoglobin A1c below 7% was seen in 89.9% of the patients, below 6.5% in 78.3%, and below 6.0% in 60.1% without antidiabetic medication. Overall, the mean HbA1c decreased from 8.7 ± 1.7% to 6.1 ± 1.1% (p < 0.0001). The HbA1c distribution throughout the follow-up period, with respect to patients having normal weight, overweight, and obesity (BMI >30 and <35) and also in relation to the type of operation is illustrated in Fig. 3. After DII-SG, the HbA1c decreased by an average of 2.8% (p < 0.001) and by 2.4% after the JII-SG (p < 0.001). The difference was statistically significant between the two versions (p = 0.001). Mean FPG decreased from 202.1 ± 67.6 to 112.2 ± 30 mg/dl (p < 0.0001). The difference was not statistically significant between the two operations (p = 0.23). Mean postprandial plasma glucose dropped from 263.3 ± 101.5 to 130 ± 45.7 mg/dl (p < 0.0001), with a decrease from 293.5 ± 110.5 to 120.9 ± 42.2 mg/dL (p < 0.01) after the II-DSG and from 237.8 ± 86.8 to 136.2 ± 47.1 mg/dL (p < 0.01) after the JII-SG, Fig. 3. The difference was statistically significant between the two operations (p = 0.04).
Pre- and postoperative glycemic evaluation. HbA 1c glycated hemoglobin, NW normal weight, OW overweight, OB obese. a Overall pre- and postoperative HbA1c evaluation. b Pre- and postoperative HbA1c according to the type of operation. c Pre- and postoperative HbA1c according to the initial BMI. d Pre- and postoperative HbA1c during the follow-up period. e Pre- and postoperative fasting plasma glucose according to the type of operation. f Pre- and postoperative postprandial glucose according to the type of operation. *p = Student’s t test between the pre- and postoperative period
A detailed evaluation of diabetes control and its correlation with preoperative body weight is demonstrated in Table 3. Overall, 86.4% of patients permanently discontinued their preoperative oral hypoglycemic agents and/or insulin. Oral agents were still required in 24 patients (12.1%), with 21 of them using only one medication. Insulin therapy was required in a lower dosage in three patients (1.5%). Preoperatively, the mean daily requirement of insulin was 48.9 units. Postoperatively, this requirement decreased to a mean of 15 units. No patient required more antidiabetic medication in relation to preoperative status. Using logistic regression analysis, different preoperative variables could not predict success, defined as HbA1c below 6.5%, Table 4.
Figure 4 demonstrates lipid profile, hypertension resolution, and pre- and postoperative micro- and macroalbuminuria. Preoperatively, abnormal levels of low-density lipoprotein (LDL) were seen in 55.2% of patients. A LDL < 100 mg/dL, without medication, was achieved by 65.1% of patients. The LDL decreased from a mean of 107.3 ± 37.4 to 90 ± 25.6 mg/dL (p < 0.0001). Postoperatively, normal cholesterol levels (<200 mg/dL) were observed in 93.6%. The mean total cholesterol decreased from 204.7 ± 53.2 to 160.1 ± 28.3 mg/dL (p < 0.0001). Triglycerides decreased from a mean of 273.4 ± 222.2 to 110.3 ± 66.1 mg/dL (p < 0.0001). The triglycerides were lower than 150 mg/dL in 81.8% of patients. High-density lipoprotein (HDL) increased from a mean of 45.5 ± 19.9 to 49.4 ± 13.4 mg/dL (p < 0.0001). Preoperatively, all patients with arterial hypertension were using medication (mean, 1.9 ± 1.2). Postoperatively, the blood pressure had normalized (≤130/≤ 85 mmHg), without medication, in 87.5% of the patients. Overall, CV disease was identified in 50 (24.8%) patients. Postoperatively, six major adverse CV events were diagnosed in five (2.5%) patients. An early myocardial infarction and then angina was observed in one/0.5% patient, angina in two/1.5%, stroke in one/0.5%, and pericardial effusion in one/0.5%. Two of these patients with postoperative CV events had a documented preoperative episode. CV interventions were performed in three/1.5% patients (coronary angioplasty in one, coronary revascularization in one, and coronary stent in one). The mean microalbuminuria decreased from 99.7 ± 193.2 to 37.5 ± 91.5 μg/min after the operations (p < 0.001). Microalbuminuria was diagnosed in 82 (40.6%) patients in the preoperative period. Resolution was achieved in 71.1%. Macroalbuminuria was documented in 14 patients. Postoperatively, 42.9% normalized, 28.6% had microalbuminuria, and 28.6% still had macroalbuminuria. All patients with GFR of 60–89 ml/min had normalized filtration rate (>90 ml/min) in the postoperative period.
Resolution of major associated comorbidities. a Mean pre- and postoperative total cholesterol. b Mean pre- and postoperative triglycerides. c Mean pre- and postoperative HDL cholesterol. d Mean pre- and postoperative LDL cholesterol. e Pre- and postoperative incidence of major associated comorbidities. *p = Student’s t test between the pre- and postoperative period
Discussion
In this report of 2 to 5 years follow-up of 202 consecutive type 2 diabetic patients with BMI < 35 submitted to laparoscopic ileal interposition associated with a sleeve gastrectomy, we showed that 89.9% had HbA1c below 7% without antidiabetic medication, 78.3% of patients had HbA1c below 6.5%, and 60.1% below 6%. The achievements of the Steno-220 study with optimal medical therapy in a very similar patient population resulted in only 17% incidence of patients with HbA1c below 6.5%.
In the present study, sustainability of effect was evident. Similar numbers of HbA1c control were seen at a 7-month follow-up study using these same techniques,21 and repeated in a prospective randomized controlled study at a mean of 2 years follow-up.16. This last study demonstrated that although the difference between the two operations was not statistically significant, the DII-SG provided a greater decrease in the HbA1c level compared to the JII-SG. Due to the findings of this prospective randomized controlled trial, the duodenal version was utilized in more severely diabetic patients in the present study, and again, the DII-SG had a better performance in decreasing HbA1c and controlling postprandial glucose. The anatomical similarity of the DII-SG with the duodenal switch (DS) operation is evident. The DS has the highest rate of resolution of diabetes in morbidly obese patients; however, its long intestinal bypass results in harmful nutritional complications that are avoided by the ileal interposition. So, the possible advantage of the DII-SG in relation to the DS is due to the shorter bypass (only the duodenum and the first 50 cm of the jejunum) that maintains almost the same preoperative intestinal length while stimulating the ileal hormonal secretion as much as the DS. As observed in this study, patients did not have problems of protein malnutrition, fat and vitamins malabsorption as typically seen with the DS operation.
In this study, 86.4% of patients were off antidiabetic medication. Hari Kumar et al.22 reported a series of ten patients with BMI < 35 submitted to the laparoscopic sleeve gastrectomy associated to ileal interposition with a 70% remission rate of T2DM at a 9-month follow-up. Tinoco et al.23 in a mid-term outcome of 30 patients, described an 80% remission rate, and Goel et al.24 demonstrated that after 6 months of operation, 100% of the patients with BMI < 35 submitted to JII-SG had HbA1c below 7%.
In the present series, patients were categorized as a “real world” typical clinical population of moderate to severe T2DM as judged by disease duration and on-treatment values of HbA1c and glucose levels. Early on, we decided to approach T2DM according to the current pathophysiologic knowledge of the disease.
Although the percentage of weight loss is a predictor of remission of diabetes in morbidly obese diabetic patients,25 glucose control was not related to the amount of weight loss in this subset of patients. In this study, mean BMI decreased from 29.7 to 23.5 kg/m2. The operations induced progressively greater weight loss across the normal weight, overweight, and obesity (BMI >30 and <35) groups. It is suggested that patients with T2DM possess adverse CV disease risk factors and have a significant burden of macrovascular disease irrespective of their baseline body weight.26 As indicated by the INTERHEART study, central obesity was a more powerful predictor of CV disease than BMI.27
The concomitant and significant impact on the other components of CV risk was also a relevant finding in this study. Hypertension control was achieved in 87.5% of patients without medication. The benefits of lowering blood pressure have been demonstrated by randomized trials.28 In the present study, the resolution rate of hypercholesterolemia and hypertriglyceridemia was 93.6% and 81.8%, respectively. Lipid management aimed at lowering LDL cholesterol, raising HDL cholesterol, and lowering triglycerides reduced macrovascular disease and mortality in patients with T2DM, particularly in those who had experienced prior CVD events,29 a condition present in 12.9% of the patients in this study.
Our findings demonstrated that the operations could be performed in relative safety. Of the two deaths (0.99%) in the first 30 days after the operation, one was clearly related to the concomitant baseline nephropathy. Of the two late deaths (0.99%), one was related to neurological disease and associated nephropathy. All types of surgeries involve the risk of associated mortality and morbidity, especially in a group of diabetic patients with clinical characteristics such as those presented in this study. Early mortality and morbidity were dealt with in a publication of 454 patients with these techniques.30 During 1988–2000, the annual all-cause mortality rates among T2DM patients were 25.2 per 1,000 person-years compared with 9.5 per 1,000 person-years in those without diabetes in the US population age 35 to 74 years. CV disease mortality in this diabetic population was 11.1 per 1,000 person-years compared to 3.4 per 1,000 person-years in those without diabetes.31
Overall, early 30-day morbidity was 8.4%. The 0.99% leak rate reported in this study is low. A recent position statement on sleeve gastrectomy from the American Society for Metabolic and Bariatric Surgery declared a mean leak rate of 2.2%.32 Late complications were observed in 3.5% of the patients. The observed 1.5% incidence of bowel obstruction resembles that seen with laparoscopic RYGB for morbid obesity, which ranges from 1.5% to 11%.33 Gallstone formation was observed in 12.1% and is a very common finding after weight loss.34
Any comparison between procedures must take into account the patient population, the procedural complexity, associated diseases, and most importantly, the resolution of diabetes and its comorbidities. In a recent mid-term outcome report of the ileal interposition associated with a sleeve gastrectomy performed for regular bariatric patients, the long-term morbidity was 5.9%, with no mortality.35 The use of laparoscopic sleeve gastrectomy (SG) as a sole bariatric procedure has been progressively accepted. Recent reports have shown that sleeve gastrectomy gives similar results in controlling diabetes36 and cardiovascular risk factors37 in an obese population when compared to RYGB.
Malnutrition was not observed. Albumin levels were routinely measured and were always normal. The increased levels of GLP-2 leading to intestinal growth and improvement of nutrient absorption may eventually explain the absence of malnutrition in this series.38 Although a specific measure of quality of life after the operations was not used, the majority of patients reported only mild complaints during the follow-up period and a significant improvement in their daily routine. The most frequent postoperative symptoms were food intolerance and heartburn. Postoperative reflux symptoms were observed in a significant group of patients. A recent report demonstrated that SG produced a significant decrease in lower esophageal sphincter pressure and that the partial resection of the sling fibers during the SG could be related to the increased rates of postoperative GERD.39
We cannot determine whether the favorable survival effect of this operation is related to glucose control or due to any other beneficial effect. We speculate that beyond glycemic control, this type of surgery may eventually impact all-cause mortality as it statistically improves the usual risk variables, like cholesterol, triglycerides, weight, microalbuminuria, and hypertension. It also provided an early and long-lasting control of postprandial glycemia. A relationship between mortality and postprandial glucose is known and is independent of the fasting glucose levels.40 It has also been suggested that postprandial plasma glucose, and not fasting plasma glucose, is associated with cardiovascular disease.41
The sustained effect of the operation could be related to a number of factors, and one of them could be addressing the current pathophysiologic mechanisms of T2DM. The primary objective of this study was not to evaluate the mechanisms by which the surgery influences glucose metabolism, but we speculate that they are probably different from those of other antidiabetic treatments. In a recent publication, we found that the operation induced changes in T2DM by mechanisms independent of weight loss, principally involving restoration of insulin sensitivity and improvement of ß cell function.42 Surprisingly, we could not identify preoperative clinical predictors of success.
The results of this study suggest to the clinician that surgery may be an alternative treatment for diabetic patients at lower BMIs. More objective criteria of disease severity are certainly necessary as this study has also confirmed the superiority of the DII-SG for diabetic patients with greater severity of disease. The good results related to the use of the JII-SG for those with less advanced disease were also confirmed.
In conclusion, after a follow-up of 2 to 5 years, the ileal interposition associated with sleeve gastrectomy has been shown to be a safe, effective, and long-lasting alternative for the treatment of T2DM patients with BMI < 35. Hemoglobin A1c below 7.0% without antidiabetic medications was seen in nearly 90% of the patients, and below 6.5% in 78.5%. It was also observed that besides glycemic control, other benefits were achieved. Future studies should address predictive factors of success and more specific selection criteria.
References
Zimmet P, Alberti KG, Shaw J: Global and societal implications of the diabetes epidemic. Nature 2001;414:782–787.
Moss SE, Klein R, Klein BE. Cause specific mortality in a population-based study of diabetes. Am J Public Health 1991;81:1158–1162.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complication in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853.
The ADVANCE Collaborative Group. Intensive Blood Glucose Control and Vascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 2008;358:2560–2572.
The VADT Investigators. Glucose Control and Vascular Complications in Veterans with Type 2 Diabetes. N Engl J Med 2009;360:129–139.
ACCORD Study Group. Effects of Intensive Glucose Lowering in Type 2 Diabetes. N Engl J Med 2008;358:2545–2559.
Sjostrom L, Lindroos AK, Peltonen M, Torgereson J, Bouchard C, Carlsson B, Dahlgren S, Larsson B, Narbro K, Sjostrom C, Sullivan M, Wedel H: Lifestyle, diabetes and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004;351:2683–2693.
Rubino F, Schauer PR, Kaplan LM, Cummings DE. Metabolic surgery to treat type 2 diabetes: clinical outcomes and mechanisms of action. Ann Rev Med 2010;61:393–411.
Ferrannini E, Mingrone G. Impact of different bariatric surgical procedures on insulin action and beta-cell function in type 2 diabetes. Diabetes Care 2009;32:514–520.
DePaula, AL, Macedo AL, Rassi N, Vencio S, Machado CA, Mota BR, Silva LQ, Halpern A, Schraibman V. Laparoscopic treatment of metabolic syndrome in patients with type 2 diabetes mellitus. Surg Endosc 2008;22:2670–2678.
DePaula AL, Macedo AL, Schraibman V, Mota BR, Vencio S. Hormonal evaluation following laparoscopic treatment of type 2 diabetes mellitus patients with BMI 20–34. Surg Endosc. 2009;23(8):1724–1732.
Flatt PR. Effective surgical treatment of obesity may be mediated by ablation of the lipogenic gut hormone gastric inhibitory polypeptide (GIP): evidence and clinical opportunity for development of new obesity-diabetes drugs? Diab Vasc Dis Res 2007;4:151–153.
Kohli R, Kirby M, Setchell KDR, Jha P, Klustaitis K, Woollett LA, Pfluger PT, Balistreri WF, Tso P, Jandacek RJ, Woods SC, Heubi JE, Tschoep MH, D’Alessio DA, Shroyer NF, Seeley RJ (2010) Intestinal adaptation after ileal interposition surgery increases bile acid recycling and protects against obesity related co-morbidities. Am J Physiol Gastrointest Liver Physiol doi:10.1152/ajpgi.00221.2010.
Rubino F, Forgione A, Cummings DE, Vix M., Gnuli D, Mingrone G, Castagnet M, Marescaux J (2006) The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg 2006; 244:741–749.
DePaula AL, Macedo ALV, Mota BR, Schraibman V. Laparoscopic ileal interposition associated to a diverted sleeve gastrectomy is an effective operation for the treatment of type 2 diabetes mellitus patients with BMI 21–29. Surg Endosc 2009;23:1313–1320.
De Paula AL, Stival AS, Macedo A, Ribamar J, Mancini M, Halpern A, Vencio S. Prospective randomized controlled trial comparing 2 versions of laparoscopic ileal interposition associated with sleeve gastrectomy for patients with type 2 diabetes with BMI 21–34 kg/m2. Surg Obes Relat Dis 2010;6:296–305.
Members of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: James R. Gavin III, MD, PhD (Chair), K.G.M.M. Alberti, MD, Mayer B. Davidson, MD, Ralph A. DeFronzo, MD, Allan Drash, MD, Steven G. Gabbe, MD, Saul Genuth, MD, Maureen I. Harris, PhD, MPH, Richard Kahn, PhD, Harry Keen, MD, FRCP, William C. Knowler, MD, DrPH, Harold Lebovitz, MD, Noel K. Maclaren, MD, Jerry P. Palmer, MD, Philip Raskin, MD, Robert A. Rizza, MD, and Michael P. Stern, MD. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2003; 26:S5–S20.
Buse JB, Caprio S, Cefalu WT, Ceriell A, Del Prato S, Inzuchi SE, Laughlin SM, Phillips II GL, Robertson RP, Rubino F, Kahn R, Kirkman ME. How Do We Define Cure of Diabetes? Reviews/Commentaries/ADA Statements. Consensus Statement. Diabetes Care 2009;32:2133–2135.
DePaula AL, Stival AR, DePaula CC, Halpern A, Vencio S. Impact on dyslipidemia of the laparoscopic ileal interposition associated to sleeve gastrectomy in type 2 diabetic patients. J Gastrointest Surg. 2010 Aug;14(8):1319–25.
Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a Multifactorial Intervention on Mortality in Type 2 Diabetes. N Engl J Med 2008;358:580–591.
DePaula AL, Macedo ALV, Rassi N, Machado CA, Schraibman V, Silva LQ, Halpern H. Laparoscopic treatment of type 2 diabetes mellitus for patients with a body mass index less than 35. Surg Endosc 2008;22:706–716.
Hari Kumar KVS, Ugale S, Gupta N, Naik V, Kumar P, Bhaskar P, Modi KD. Ileal Interposition with Sleeve Gastrectomy for Control of Type 2 Diabetes. Diabetes Technol Ther 2009; 11:785–789.
Tinoco A, El-Kadre L, Aquiar L, Tinoco R, Savassi-Rocha P Short-Term and Mid-Term Control of Type 2 Diabetes Mellitus by Laparoscopic Sleeve Gastrectomy with Ileal Interposition. World J Surg 2011;35(10):2338–2244.
Goel R, Amin P, Goel M, Marik S. Early remission of type 2 diabetes mellitus by laparoscopic ileal transposition with sleeve gastrectomy surgery in 23–35 BMI patients. Int J Diabetes Dev Ctries 2011; 31(2): 91–96.
Dolan K, Hatzifotis M, Newbury L. A comparison of laparoscopic adjustable gastric banding and biliopancreatic diversion in superobesitiy. Obes Surg 2004;14:165–169.
Song SH and Hardisty CA. Type 2 diabetes mellitus: a high-risk condition for cardiovascular disease irrespective of the different degrees of obesity. QJMed 2008;101:875–879.
Salim Yusuf, Steven Hawken, Stephanie Ôunpuu, Tony Dans, Alvaro Avezum, Fernando Lanas, Matthew McQueen, Andrzej Budaj, Prem Pais, John Varigos, Liu Lisheng, on behalf of the INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries: case–control study. Lancet 2004;364:937–952.
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS38. BMJ 1998;317:703–713.
Lindholm LD, Ibsen H, Dahlof B, Devereux RB, Beever G, de Faire U, Fyhrquist F, Julius S, Kjeldsen SE, Kristiansson K, Kederballe-Pedersen O, Niemine MS, Omvik P, Oparil S, Wedel H, Aurup P, Edelman J, Snapin S Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention for Endpoint Reduction in Hypertension Study (LIFE): a randomized trial against atenolol. Lancet 2002;359:1004–1010.
DePaula AL, Stival AR, Halpern A, Vencio S. Thirty-Day Morbidity and Mortality of the Laparoscopic Ileal Interposition Associated with Sleeve Gastrectomy for the Treatment of Type 2 Diabetic Patients with BMI <35: An Analysis of 454 Consecutive Patients. World J of Surg 2011;35:102–108.
Gregg EW, Qiuping G, Cheng YJ, Venkat Narayan KM, Cowie CC. Mortality Trends in Men and Women with Diabetes, 1971 to 2000. Ann Intern Med 2007;147:149–155.
Clinical Issues Committee of the American Society for Metabolic and Bariatric Surgery. Updated Position Statement on Sleeve Gastrectomy as a Bariatric Procedure. Surg Obes Relat Dis 2010; 6:1–5.
Koppman JS, Li C, Gandsas A. Small Bowel Obstruction after Laparoscopic Roux-En-Y Gastric Bypass: A Review of 9,527 Patients. J Am Coll Surg 2008;206:571–584.
Liddle RA, Goldstein RB, Saxton J. Gallstone formation during weight-reduction dieting. Arch Intern Med 1989;149:1750–1753.
DePaula AL, Stival AR, Halpern A, Vencio S. Surgical Treatment of Morbid Obesity: Mid-term Outcomes of the Laparoscopic Ileal Interposition associated to a Sleeve Gastrectomy Obes Surg. 2011; 21(5): 668–675.
Nocca D, Guillaume F, Noel P, Picot MC, Aggarwal R, El Kamel M, Schaub R, de Seguin de Hons C, Renard E, Fabre JM. Impact of laparoscopic sleeve gastrectomy and laparoscopic gastric bypass on HbA1c blood level and pharmacological treatment of type 2 diabetes mellitus in severe or morbidly obese patients. Results of a multicenter prospective study at 1 year. Obes Surg. 2011 Jun;21(6):738–43.
Benaiges D, Goday A, Ramon JM, Hernandez E, Pera M, Cano JF, Obemar Group Laparoscopic sleeve gastrectomy and laparoscopic gastric bypass are equally effective for reduction of cardiovascular risk in severely obese patients at one year of follow-up. Surg Obes Relat Dis 2011;7(5):575–580
Thulesen J, Hartmann B, Kissow H, Jeppesen PB, Orskov C, Holst JJ, Poulsen SS. Intestinal growth adaptation and GLP-2 in rats with ileal-jejunal transposition or small bowel resection. Dig Dis Sci 2001;46:379–88.
Braghetto I, Lanzarini E, Korn O, Valladares H, Molina JC, Henriquez A. Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients. Obes Surg 2010;20:357–362.
The DECODE Study Group on behalf of the European Diabetes Epidemiology Group. Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. Lancet 1999;354:617–621.
Barrett-Connor E, Ferrara A. Isolated postchallenge hyperglycemia and the risk of fatal cardiovascular disease in older women and men: The Rancho Bernardo study. Diabetes Care 1998;21(8):1236–1239.
De Paula AL, Stival AR, Halpern A, Depaula CC, Mari A, Muscelli E, Vencio S, Ferrannini E Improvement in insulin sensitivity and β-cell function following ileal interposition with sleeve gastrectomy in type 2 diabetic patients: potential mechanisms.. J Gastrointest Surg. 2011 Aug;15(8):1344–53
Conflict of interests
The authors attest that there is no conflict of interest to disclose related to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DePaula, A.L., Stival, A.R., DePaula, C.C.L. et al. Surgical Treatment of Type 2 Diabetes in Patients with BMI Below 35: Mid-term Outcomes of the Laparoscopic Ileal Interposition Associated with a Sleeve Gastrectomy in 202 Consecutive Cases. J Gastrointest Surg 16, 967–976 (2012). https://doi.org/10.1007/s11605-011-1807-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1807-0