Abstract
Background
The Bioenterics Intragastric Balloon (BIB) is effective for weight loss. However, comparisons of its effectiveness between groups with different body mass index (BMI) are rare. This study compared the effectiveness of BIB treatment in patients with BMI <32 kg/m2 and those with BMI ≧32 kg/m2 at the time of BIB removal and at 1 year later.
Methods
Between April 2009 and June 2011, 28 obese patients who completed a full course of BIB treatment were enrolled. There are 16 patients with BMI <32 and 12 with BMI ≧32. Patients who lost more than 20 % of excess weight (% EWL) were categorized as responders.
Results
The BMI significantly fell from 32.4 ± 3.7 to 28.5 ± 3.7 kg/m2 (P < 0.01) at the time of BIB removal. All biochemical measurements except for cholesterol level were significantly improved. The median value of %EWL of all patients at BIB removal was 40.1, and 20 patients (71.4 %) were responders. Adherence to dietitian counseling was significantly better in responders than in non-responders (85 vs. 25 %, respectively; P < 0.01). The percentage of responders at 1 year after BIB removal was significantly higher among patients with BMI <32 than those with ≧32 (62.5 vs. 16.7 %, respectively; P = 0.02).
Conclusions
BIB placement can achieve significant weight loss and improvement of co-morbidities in obese patients. Better adherence to dietitian counseling is associated with better response. Patients with BMI <32 maintain better weight loss at 1 year after BIB removal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity carries a significant risk of life-threatening complications, such as heart disease, diabetes, and hypertension, and is one of the major public health problems in both Western and Eastern countries. [1] Although conventional medical treatments using dietary, behavioral, and pharmacologic methods have been effective for short-term weight management, these methods are ineffective for long-term weight control and reduction of co-morbidity. [2] Bariatric surgery is currently the only method for achieving long-term, reliable weight loss for morbidly obese patients. However, surgical procedures are invasive and may lead to a number of complications. [3, 4]
The Bioenterics Intragastric Balloon (BIB), manufactured by BioEnterics Corporation, Carpinteria, CA, USA, has been considered an effective treatment for obesity in Western population. [5, 6] The BIB treats obesity by reducing the volume of the stomach and decreasing food intake in conjunction with a program of new dietary and behavioral routines. The indications of BIB treatment for Asian populations include patients with body mass index (BMI, kg/m2) ≥37, or BMI ≥32, with obesity-related co-morbidities, but do not want to undergo surgery [7] or patients with BMI <32, with obesity-related co-morbidities and failure to lose weight by conventional medical treatments. Although the effects of BIB treatment on Asian populations have been reported in some studies, these reports are still mostly scarce and diverse. [8–11]
The aim of this study was to compare the effectiveness of BIB treatment between patients with BMI <32 and those with BMI ≧32 at the time of BIB removal and at 1 year later. We also attempted to identify factors associated with a better response to BIB treatment.
Materials and Methods
Eligible Patients
Two groups of obese patients were enrolled for BIB placement. First, patients had a BMI ≥ 37, or a BMI ≥ 32, with obesity-related co-morbidities and did not wish to undergo bariatric surgery. A second group of patients had BMI between 27 and 32, with obesity-related co-morbidities and were unable to reduce weight by controlling their diet, behavior modification, or pharmacologic therapy. Contraindications to BIB placement include the following: presence of potentially bleeding lesion of the upper gastrointestinal tract; previous gastric surgery; a large hiatal hernia; administration of aspirin, anti-inflammatory agents, anticoagulants, or steroids; alcoholism or drug addiction; and pregnancy. [6] The study was approved by the Ethical Committee of E-Da Hospital, Kaohsiung, Taiwan.
Intervention
Each individual was evaluated by a multidisciplinary team consisting of dietitians, psychiatrists, endocrinologists, surgeons, and gastroenterologists at the E-Da Hospital. BIB placement was performed under intravenous conscious sedation, and the BIB was inflated under direct vision with a mixture of 500–550 mL saline and 10 mL methylene blue. After full recovery from sedation, the patients were discharged. They were given a proton pump inhibitor for 7 days and antiemetics as needed. Follow-up consultation with a dietician was recommended after BIB placement. Patients were given a structured balanced diet with a caloric intake between 800 and 1,200 kcal/day and were requested to return for follow-up every week for the first 2 weeks, every 2 weeks twice, and then monthly. Patients with psychiatric disorders also had psychiatric treatments as needed. The balloon was routinely removed under endoscopy 6 months after BIB placement. No structured weight maintenance program was conducted after BIB removal. Good adherence to the treatment program was defined as when a patient returned for at least 50 % of scheduled dietician counseling sessions during BIB treatment.
Anthropometric and Biochemical Measurements
Anthropometric and biochemical measurements for all subjects were obtained at the time of BIB placement and removal. Anthropometric measurements obtained included body weight, body height, and waist circumference (WC). BMI was calculated as the weight in kilograms divided by the square of height in meters (kg/m2). Biochemical measurements included blood glucose level, aspartate aminotransferase (AST), alanine aminotransferase, serum cholesterol, triglyceride, high-density lipoprotein (HDL)-cholesterol, and low-density lipoprotein (LDL) -cholesterol levels. Metabolic syndrome was diagnosed according to the recommended criteria. [12] One year after BIB removal, patients were contacted by telephone and reported their current weight.
Classification of Erosive Esophagitis
All endoscopic procedures were performed by the same endoscopist. The endoscopic findings, especially the presence of erosive esophagitis, were recorded for all subjects at the time of BIB placement and removal. Diagnosis and classification of erosive esophagitis was based on the Los Angeles classification, and esophagitis was classified as grade A, B, C, or D. [13]
Definition of Responder
Excess weight (preoperative weight − ideal weight) was calculated as the number of kilograms a patient would need to lose to lower his or her BMI to 23 (the upper healthy limit of normal BMI in Asian patients). [14] Percent excess weight loss (%EWL) was calculated as: (preoperative weight − current weight)/(preoperative weight − ideal weight) × 100. [15] A treatment “responder” was defined as a patient with more than 20 % in %EWL. [16]
Statistical Analysis
For anthropometric and biochemical variables, data were presented as mean ± standard deviation (SD) for normally distributed continuous variables or as median (range) for continuous variables lacking a normal distribution or as percentages for categorical variables. Changes between before BIB placement and after BIB removal were assessed using paired Student's t-test for parametric data, the Wilcoxon signed-rank test for nonparametric data, and McNemar's test for categorical variables. Comparisons between responders and non-responders or between patients with BMI <32 and patients with BMI ≥32 were assessed using Mann–Whitney U-test, chi-square test, or Fisher's exact test when appropriate. A P-value <0.05 indicated a statistically significant difference. All analyses were performed by SPSS 12.0 version for Windows.
Results
Patient Demographics
Between April 2009 and June 2011, a total of 33 consecutive obese patients underwent BIB placement. Five patients (15.2 %) had early BIB removal, including voluntary early removal in two patients and removal in three patients for the following conditions: intractable vomiting, panic attack 1 day after BIB placement, and gastric ulcer with bleeding 5 months after BIB placement. A final group of 28 patients who completed a full course of treatment was enrolled for analysis. The median age of the 28 patients was 31.5 years (range 20–55 years); the group included five men (17.9 %) and 23 women (72.1 %). The number of patients with BMI <32 and BMI ≧ 32 were 16 (57.1 %) and 12 patients (42.9 %), respectively. The median BIB treatment period was 200 days (range 170–225 days). Nine patients (32.1 %) had at least one of the following psychiatric disorders: panic disorder, binge eating disorder, major depressive disorder, and dysthymic disorder.
Changes on Anthropometric and Biochemical Measurements After BIB Placement
All patients had reduced BMI compared to their baseline measurements. As shown in Table 1, the mean BMI and WC significantly fell from 32.4 ± 3.7 and 101.9 ± 8.9 cm to 28.5 ± 3.7 and 90.6 ± 9.3 cm, respectively (P <0.01). All biochemical measurements except for cholesterol level also showed significant improvement. The incidence of metabolic syndrome decreased from 64.3 % to 32.1 % after BIB treatment (P = 0.01).
Factors Associated with Responders to BIB Treatment
The median % EWL of all patients at the time of BIB removal was 40.1 (range 0.94–132.3). Twenty patients (71.4 %) had more than 20 % in EWL and thus were classified as responders. The median % EWL of responders at the time of BIB removal was 54.0 (range 22.7–132.3). To identify factors associated with better response to the BIB treatment, baseline characteristics and adherence to dietician counseling between responders and non-responders were compared. The two groups did not differ in baseline anthropometric and biochemical measurements and presence of psychiatric disorders, but adherence to dietitian counseling was found to be significantly better in responders than in non-responders (85 vs. 25 %, respectively; P < 0.01) (Table 2).
Changes in Anthropometric and Biochemical Measurements Before and After BIB Treatment in Patients with BMI <32 and BMI ≧32
Significant BMI reduction was observed in both groups at the time of BIB removal compared to their baseline measurements. Statistically significant improvement of metabolic parameters was observed in both groups. All biochemical measurements except for AST level and HDL-cholesterol level in patients with BMI <32 and cholesterol level in patients with BMI ≧32 showed significant improvement. The incidence of metabolic syndrome decreased from 56.3 to 31.3 % in patients with BMI <32 and 75.0 to 33.3 % in patients with BMI ≧32 after BIB treatment, but they did not reach statistical significance in both groups (Table 3).
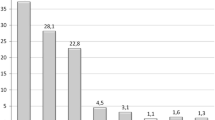
Comparisons of Effectiveness Between Patients with BMIs <32 and BMIs ≧ 32
Patients with BMI ≧32 were younger than those with BMI <32 (39 vs. 27 years, respectively; P < 0.01). At the time of BIB removal, although the reduction in BMI and body weight was higher in patients with BMI ≧32 and median %EWL was higher in patients with BMI <32, they did not reach statistical significance. Responders in the group with BMI <32 and the group with BMI ≧ 32 were 11 (68.8 %) and 9 (75 %), respectively (P = 1.0) (Table 4). Three responders were not enrolled for analysis at 1 year after BIB removal. They included one patient who was pregnant at 6 months after BIB removal and two patients who could not be contacted. Although median %EWL in responders at the time of BIB removal and at 1 year after BIB removal was higher in patients with BMI <32 than those with BMI ≧ 32, it did not reach statistical significance. However, the percentage of responders was significantly higher in patients with BMI <32 than in those with BMI ≧ 32 at 1 year after BIB removal (62.5 vs. 16.7 %, respectively; P = 0.02) (Table 4).
Safety Profile
Three patients had complications, including panic attack, intractable vomiting, and gastric ulcer with bleeding, which resulted in early BIB removal. One patient had Mallory–Weiss syndrome but was successfully treated with proton pump inhibitors and antiemetics. Before BIB placement, only two patients (7.1 %) were found to have erosive esophagitis, and in both cases the esophagitis was scored as grade A. At the time of BIB removal, nine patients (32.1 %) had erosive esophagitis (eight had grade A and one had grade B esophagitis). However, only two patients required proton pump inhibitors for gastroesophageal reflux symptoms during the treatment course.
Discussion
Although BIB has been widely used in the treatment of obesity, the experience in Asia is still limited. Our study confirmed that BIB treatment could result in good weight loss with only minor complications in an Asian population. At the time of BIB removal, our patients achieved a median %EWL of 40.1, which was comparable not only to the %EWL of 32.1 reported from Western countries in one meta-analysis but also to the %EWL of 27 to 45.1 reported from Asian countries. [5, 9–11] In a study of 119 Chinese patients, Mui et al. reported that patients achieved a mean %EWL of 45.1 ± 35.3 at the time of BIB removal. [11] Ohta et al. reported %EWL of 27 ± 9 in 17 Japanese patients and Ganesh et al. reported the mean maximum %EWL of 32.4 in 16 Singapore patients. [9, 10] Moreover, we also found that better adherence to dietitian counseling was associated with better response during BIB treatment. Although weight regain occurred after BIB removal, we found that 1 year after BIB removal, patients with BMI <32 could maintain weight loss better than those with BMI ≧32 could.
Several factors were associated with the treatment outcome. First, dietary and lifestyle modification are the primary treatments for obese people, and Dansinger et al. reported that more frequent dietitian counseling is an independent predictor of greater weight loss in obese patients receiving conventional medical treatment. [17] It is also recommended that BIB treatment should be used in combination with a long-term supervised diet and lifestyle modification program. Our finding that good adherence to dietitian counseling is associated with better response re-emphasizes the importance of supervised diet modification during BIB treatment.
Second, study results have shown that %EWL at the time of BIB removal was significantly higher in patients of lower, compared to higher, BMI categories. [6, 11] Mui et al. reported that BIB produces excellent results in lower-BMI patients. Those authors reported that the mean %EWL in the BMI <30 group, the BMI 30–35 group, the BMI 35–40 group, and the BMI >40 group were 87.0 ± 59.8, 58.3 ± 31.2, 35.1 ± 23.1, and 27.4 ± 17.0 %, respectively. [11] We also found that %EWL at the time of BIB removal was higher in patients with BMI <32 than those with BMI ≧32, but the difference was not significant, which might have resulted from the small sample size.
Third, major psychiatric disorders are thought to be a contraindication to BIB placement. Puglisi et al. also reported that the outcome of BIB treatment appears to be affected by a binge eating pattern in morbidly obese patients. [18] However, although there was a high prevalence of psychiatric disorders in our patients (32.1 %), this factor did not affect treatment outcome. We provided psychiatric treatments for all patients with psychiatric disorders; however, further studies are needed to elucidate whether the psychiatric treatments will affect the outcome of BIB treatment.
Long-term follow-up outcome after BIB removal is another important issue with BIB treatment, and weight regain has been reported in most studies. By using %EWL ≧20 as the cutoff point of responders, Herve et al. reported that percentage of responders and mean %EWL decreased from 74 and 39.8 % at the time of BIB removal to 56 and 26.8 %, respectively, at 1 year after BIB removal. [19] Kotzampassi et al. reported that the percentage of responders was lower as time passed: at the time of removal, the percentage of responders was 83 %. The percentages fell to 53, 27, and 23 % at the 12-, 24-, and 60-month follow-up, respectively. [16]
There is limited Asian data about 1-year follow-up after BIB removal. Ohta et al. reported that four of the eight Japanese patients who were followed for 1 year had % EWLs >20. [10] Although our study showed that the % EWL in responders decreased from 54.0 % at the time of BIB removal to 27.2 % at 1 year after BIB removal, 42.9 % of patients were still categorized as responders at 1 year after BIB removal (compared to 71.4 % at the time of BIB removal). It is worth noting that the percentage of responders at 1 year after BIB removal was significantly higher in patients with BMI <32 than in patients with BMI ≧32 (62.5 vs. 16.7 %, respectively; P = 0.02). These results are consistent with the finding from Herve et al., who reported that the best results were observed in patients who had BMI <30 prior to implantation of the BIB. This implied that BIB treatment for less obese patients might produce a better and more lasting response. Recently, Genco et al. also reported good effectiveness of BIB treatment in 261 overweight patients from three European centers with mean %EWL of 55.6 and 29.1 % at the time of BIB removal and 3 years after BIB removal, respectively. [20] Non-morbidly obese patients make up a large and important part of the population in whom bariatric surgery is not indicated. In the present study, we found that both the body weight and biochemical measurements had significant improvement at the time of BIB removal. Although we did not have the data of changes of co-morbidities after BIB removal, we found that 62.5 % of patients with BMI <32 still had %EWL ≧20 at 1 year after BIB removal. We recommend that BIB might be one alternative for those who have obesity-related co-morbidities and do not respond to conventional medical treatments.
This study not only confirms the effectiveness of BIB treatment but also demonstrates better and longer-lasting responses in less obese Asian patients. However, it may pose some limitations. Firstly, the sample size was small and only 28 patients were enrolled. Secondly, although there were more responders among the group of patients with BMI <32, weight was regained in both groups at 1 year after BIB removal. Moreover, after BIB removal, no dietary counseling was conducted and patients' eating behaviors were not recorded. Thus, the cause–result relationship among BIB placement, changes of patients' eating behaviors, and sustained weight loss remains unclear. A longer period of follow-up and detailed monitoring of the changes in patients' eating behaviors even after BIB removal is mandatory to confirm long-term benefits. Finally, owing to lack of a control group, the efficacy of BIB treatment cannot be compared with other weight reduction methods such as diet or exercise in this study.
Conclusion
BIB placement can help one achieve significant weight loss and improvement of co-morbidities in obese Asian patients. Better adherence to dietitian counseling is associated with a better response. Compared with patients with BMI ≧32, patients with BMI <32 can maintain better weight loss at 1 year after BIB removal. However, weight regain was observed in both groups at 1 year after BIB removal, suggesting that longer follow-up period is necessary to confirm its long-term efficacy.
Abbreviations
- BIB:
-
BioEnterics Intragastric Balloon
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- HDL:
-
High-density lipoprotein
- LDL:
-
low-density lipoprotein
- LA:
-
classification Los Angeles classification
- EWL:
-
Excess weight loss
References
James WP. The epidemiology of obesity: the size of the problem. J Intern Med. 2008;263:336–52.
Delinsky SS, Latner JD, Wilson GT. Binge eating and weight loss in a self-help behavior modification program. Obesity (Silver Spring). 2006;14:1244–9.
Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005;142:547–59.
Goldfeder LB, Ren CJ, Gill JR. Fatal complications of bariatric surgery. Obes Surg. 2006;16:1050–6.
Imaz I, Martinez-Cervell C, Garcia-Alvarez EE, et al. Safety and effectiveness of the intragastric balloon for obesity. A meta-analysis. Obes Surg. 2008;18:841–6.
Dumonceau JM. Evidence-based review of the Bioenterics intragastric balloon for weight loss. Obes Surg. 2008;18:1611–7.
Lee WJ, Wang W. Bariatric surgery: Asia-Pacific perspective. Obes Surg. 2005;15:751–7.
Mui WL, So WY, Yau PY, et al. Intragastric balloon in ethnic obese Chinese: initial experience. Obes Surg. 2006;16:308–13.
Ganesh R, Rao AD, Baladas HG, et al. The Bioenteric Intragastric Balloon (BIB) as a treatment for obesity: poor results in Asian patients. Singap Med J. 2007;48:227–31.
Ohta M, Kitano S, Kai S, et al. Initial Japanese experience with intragastric balloon placement. Obes Surg. 2009;19:791–5.
Mui WL, Ng EK, Tsung BY, et al. Impact on obesity-related illnesses and quality of life following intragastric balloon. Obes Surg. 2010;20:1128–32.
Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–80.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Deitel M, Gawdat K, Melissas J. Reporting weight loss 2007. Obes Surg. 2007;17:565–8.
Kotzampassi K, Grosomanidis V, Papakostas P, et al. 500 intragastric balloons: what happens 5 years thereafter? Obes Surg. 2012;22:896–903.
Dansinger ML, Tatsioni A, Wong JB, et al. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med. 2007;147:41–50.
Puglisi F, Antonucci N, Capuano P, et al. Intragastric balloon and binge eating. Obes Surg. 2007;17:504–9.
Herve J, Wahlen CH, Schaeken A, et al. What becomes of patients one year after the intragastric balloon has been removed? Obes Surg. 2005;15:864–70.
Genco A, Lopez-Nava G, Wahlen C, et al. Multi-centre European experience with intragastric balloon in overweight populations: 13 years of experience. Obes Surg. 2013;23:515–21.
Acknowledgments
This study was supported by a Project of the E-Da Hospital, Grant Number EDAHP101017.
Conflict of Interest
All contributing authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tai, CM., Lin, HY., Yen, YC. et al. Effectiveness of Intragastric Balloon Treatment for Obese Patients: One-Year Follow-up After Balloon Removal. OBES SURG 23, 2068–2074 (2013). https://doi.org/10.1007/s11695-013-1027-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-013-1027-7