Abstract
Background
The request to lose weight is expanding not only in obese and morbidly obese patients but also in overweight patients affected by co-morbidities as diabetes and hypertension and who do not tolerate diet regimen or lifestyle changes. The aim of this study is a multicenter evaluation of outcomes of intragastric balloon in overweight patients.
Methods
Patients (BMI 27–30 kg/m2) treated with a BioEnterics Intragastric Balloon (BIB) between 1996 and 2010 were extracted from the database of the participating centres in Rome (Italy), Liège (Belgium) and Madrid (Spain). Primary endpoints were the efficacy and safety at 6 and 42 months from balloon positioning. Secondary endpoints included resolution of co-morbidities.
Results
A total of 261 patients were included in this study. The most common indication for balloon placement was a psychological disorder (54 %). Mean body mass index (BMI) fell from 28.6 ± 0.4 at baseline to 25.4 ± 2.6 kg/m2 at 6 months and to 27.0 ± 3.1 kg/m2 at 3 years from BIB removal. The mean %EWL was 55.6 % at 6 months and 29.1 % at 3 years. Forty-seven patients (18 %) had complications associated with placement of the intragastric balloon (leak = 28, intolerance = 14, duodenal ulcer = 2, gastritis = 1, oesophagitis = 1, duodenal polyps = 1). The rate of patients with hypertension decreased from 29 % at baseline to 16 % at 3 years. Diabetes decreased from 15 to 10 %, dyslipidaemia decreased from 20 to 18 %, hypercholesterolaemia decreased from 32 to 21 % and osteoarthropathy decreased from 25 to 13 %.
Conclusions
The intragastric balloon is safe and effective in overweight patients, helping to reduce progression to obesity and decreasing the prevalence of a number of important co-morbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization estimates that there are more than 1 billion overweight adults worldwide, 300 million of whom are defined as clinically obese with a body mass index (BMI) >30 kg/m2 [1]. Approximately 700 million adults have a BMI between 25 and 30 kg/m2. Overweight and obesity are increasing globally and represent a major contribution to the burden of chronic disease and disability [2]. Excess weight poses a significant risk for serious and chronic diseases, including type 2 diabetes, cardiovascular disease, hypertension and stroke, as well as certain forms of cancer [1, 3–9]. Conservative estimates of the economic costs of obesity and overweight in developed countries are between 2 and 7 % of total health costs [2].
Extensive evidence links excessive body weight and overall mortality. A prospective 10-year follow-up of more than 60,000 middle-aged men and women showed that the risk of death compared with normal-weight people was two- to-threefold greater among those who were obese at the age of 50 years and 20–40 % greater among those who were overweight [3].
The aim of this study is the evaluation of safety and efficacy of intragastric balloon in overweight patients affected by one or more co-morbidities.
Methods
Patients were selected according to the National Institutes of Health criteria and guidelines for obesity surgery [10]. BioEnterics Intragastric Balloon (BIB—Allergan, Irvine, CA, USA) was placed in all cases. Patients were independently evaluated by a team made up of internist, dietician and psychologist for pre-positioning selection. They were extracted from the database of the participating centres in Rome (Italy), Liège (Belgium) and Madrid (Spain). The period considered was between 1996 and 2010. Inclusion criteria were: BMI 27–30, previous failure of dietary measures and the presence of at least one of the following co-morbidities at the time of BIB placement: hypertension (blood pressure >140/90 mmHg), diabetes (fasting glycaemia >120–130 mg/dl; HbA1c > 9 %), respiratory disorders (sleep apnoea and/or tachypnoea after little physical activity), osteoarthropathy (subjective reduction of physical activity due to joint pain), dyslipidaemia (LDL cholesterol >250 mg/dL; triglycerides >250 mg/dl) and psychological disorders (anxiety assessed with SF-36).
All enrolled patients had not received weight loss treatments for at least 8 months before placement of the intragastric balloon.
BIB placement was performed under conscious or unconscious sedation [11]. Balloon inflation, using between 300 and 700 ml of saline solution and methylene blue, was carried out under direct endoscopic vision.
Results are expressed as mean ± standard deviation for numerical variables and absolute numbers. Statistical analysis was done by means of Student’s t-test for numerical variables and χ 2 test or Fisher’s exact test for categorical variables. P < 0.05 was considered significant.
Study Endpoints
Patients’ weight, BMI and co-morbidities were recorded prior to placement of the intragastric balloon and at 6 months (time of removal of balloon) and 3 years of follow-up after BIB removal. Complications during and after balloon placement were also recorded. Patient satisfaction was assessed with a ten-point scale (1 = very unsatisfied, 10 = very satisfied).
Details of post-BIB dietary management and surgical procedures were recorded.
The primary endpoints of the study were the evaluation of weight loss parameters: BMI, %BMI loss (%BMIL), %excess weight loss (%EWL) and complications evaluated at 6 months and 3 years of follow-up. Secondary endpoints included resolution of co-morbidities according to the following cutoff: hypertension: 120–130 mmHg, diabetes: fasting glycaemia <110 mg/dL; HbA1c < 6 %, respiratory disorders: absence of symptoms, osteoarthropathy: absence of pain, dyslipidaemia: LDL cholesterol <200 mg/dL; triglycerides <200 mg/dL and psychological disorders according to SF-36.
Results
Baseline Characteristics
From the three centres, 261 patients (32 M/ 229 F) were included in this study. Of these, 73 were treated in 1996–2000, 25 in 2001–2003 and 163 in 2004–2010. The baseline characteristics of these patients are reported in Table 1. The indications for intragastric balloon positioning are reported in Table 2.
In Liège, of the 219 eligible patients, 121 patients (five male, 116 female) had evaluable data at the 3-year follow-up and were included in the analysis. Of these 121 patients, 73 were treated in 1996–2000, 25 in 2001–2003 and 23 in 2004–2010. Indications for an intragastric balloon were: psychological disorders (68 patients), dyslipidaemia (49), hypercholesterolaemia (42), hypertension (37), diabetes (31), osteoarthropathy (31) and respiratory disease (2).
In Madrid, all 101 (21 male, 80 female) eligible patients had evaluable data at the 3-year follow-up and were included in the analysis. All 101 patients were treated in 2004–2008. Indications for an intragastric balloon were: psychological disorders (47 patients), hypercholesterolaemia (37), hypertension (25), osteoarthropathy (24), diabetes (5) and respiratory disease (one).
In Rome, all 39 (five male, 34 female) eligible patients had evaluable data at the 3-year follow-up and were included in the analysis. All 39 patients were treated in 2004–2008. Indications for an intragastric balloon were: psychological disorders (27 patients), hypertension (13), osteoarthropathy (11), hypercholesterolaemia (five), diabetes (three) and dyslipidaemia (two).
Primary Endpoints
Weight Loss
In the total sample, mean BMI decreased from 28.6 ± 0.4 before intragastric balloon placement to 25.6 ± 2.6 at the time of removal of the balloon (6 months) (p < 0.05) and to 27.0 ± 3.1 at 3-year follow-up. Mean %BMI loss was 11.5 ± 9.0 and 6.1 ± 10.4 % at 6 months and 3-year follow-up, respectively. The mean excess weight loss was 55.6 ± 58.8 % at 6 months and 29.1 ± 60.3 % at 3 years. Data from the three individual centres are summarised in Table 1.
Complications
A total of 47 out of 261 (18 %) patients had complications associated with placement of the intragastric balloon. Twenty-eight patients had a leak: 26 in Liège (three after 2001, none after 2004) and two in Rome (one after 5 months post-placement). Fifteen patients were psychologically intolerant to BIB (11 in Liège, two in Madrid, two in Rome). In addition, in Madrid, two patients had a duodenal ulcer, one had gastritis, one had oesophagitis and one had duodenal polyps.
Co-morbidities
In the total sample, the rate of patients with hypertension decreased from 29 % (baseline) to 14 % at 6 months and 16 % at 3 years. The rate of patients with diabetes decreased from 15 to 8 % at 6 months and 10 % at 3 years. The rate with dyslipidaemia decreased from 20 to 18 % at both 6 months and 3 years, and the rate with hypercholesterolaemia decreased from 32 to 21 % at 6 months and 3 years. The rate with osteoarthropathy decreased from 25 to 12 % at 6 months and 13 % at 3 years. Respiratory and psychological disorders decreased from 1 and 54 % at baseline, respectively, to 0 and 13 % at 6 months. Data from the individual centres are summarised in Table 2.
Post-BIB Management
In the total sample, 172 (66 %) patients followed a dietician’s plan after removal of the intragastric balloon. Of these, 132 (77 %) followed between one and three diets, 17 (10 %) followed four to six diets and 20 (12 %) followed more than six diets. Forty (15 %) patients had post-BIB surgery. Of these, 28 patients had a gastric band (LapBand; between 4 months and 7 years after removal of the balloon), five had gastric bypass procedures (9 months to 7 years after removal), three had sleeve gastrectomy (1–3 years after removal) and four had vertical banded gastroplasty (2–4 years after removal). In addition, 25 (10 %) patients had aesthetic/plastic surgical procedures after BIB removal. Of these, 14 had abdominoplasty, six had breast augmentation and five had liposuction. Table 3 shows the data for the individual centres.
Patient Satisfaction
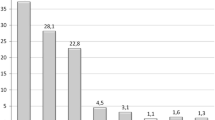
Figure 1 summarises the patient satisfaction scores in the three centres and overall. The majority of patients (52 %) reported a satisfaction score of between 5 and 8 out of 10. When asked whether the intragastric balloon treatment had changed their approach to their disease, 177/261 (68 %) patients said that it had. The figures for the individual centres were 78/121 (64 %) in Liège, 71/101 (70 %) in Madrid and 28/39 (72 %) in Rome. The overall rate of unsatisfied patients (score 1–4) was 8.0 %.
Discussion
The BioEnterics Intragastric Balloon system can be used as a temporary weight loss measure in patients with a BMI of 27 or over. It is inserted endoscopically into the stomach and filled with saline, which causes it to expand into a spherical shape that partially fills the stomach and induces satiety. The device can be left in place for a maximum of 6 months and should be used in combination with a long-term supervised diet and lifestyle modification programme [12–14]. In fact, after 1 year from intragastric balloon removal, almost all patients reach their initial weight if they were left without a following bariatric surgical procedure, or a supervised diet and behavioural regimen, with strict follow-up [15–17]. The rate of patients with %EWL > 25 % is 30 % if patients are compliant to a diet and behavioural regimen [17].
The BIB system has been shown to be safe and effective. In an Italian crossover study in 32 obese patients, mean BMI decreased by 5.8 with BIB and by 0.4 with a sham treatment in the first 3-month period; following crossover, BMI decreases in the second 3 months were 5.1 with BIB and 1.1 with sham [16]. The patients experienced transient gastrointestinal symptoms, such as nausea and vomiting, after their procedure, but no serious complications were seen. In a Brazilian study including 483 obese patients who received an intragastric balloon, 323 completed 6 months of follow-up and 85 completed 1 year of follow-up [12]. The mean weight reduction at 6 months was 15.2 kg and the mean decrease in BMI was 5.2. After 1 year, patients had maintained 90 % of the BMI reduction seen at 6 months. Two patients experienced balloon impaction and one experienced spontaneous deflation. A retrospective study of 260 patients in Italy treated with an intragastric balloon plus eating behaviour counselling or with a structured diet plan found a significantly greater weight loss with BIB than with diet after 6 months (BMI decrease, 6.1 versus 2.5) [17].
A clinical experience with the BIB system in more than 2,500 patients in Italy showed an average BMI loss of 4.9 ± 12.7 kg/m2, with a complication rate of 2.8 %; balloon rupture occurred in 0.36 %. Pre-operative co-morbidities were diagnosed in 56.4 % of patients; these were resolved in 44.3 % of cases and improved in a further 44.8 % [13].
In one centre in Madrid, Spain, 714 consecutive patients treated with BIB in 2005–2007 had a mean BMI loss of 6.5 ± 12.7 after 6 months. The overall complication rate was 4.1 %. Co-morbidities were resolved in 64 (40 %) of the 162 patients with one or more pre-operative co-morbidities diagnosed [14].
The cited studies were carried out in obese patients with high BMI (mean BMIs of 35–45). Given the risks associated with lower degrees of excess weight and the lack of treatment options for overweight patients, the aim of this study was to review the use of the intragastric balloon in overweight patients (BMI between 27 and 30) affected by one or more co-morbidity. The objectives were to evaluate the efficacy of a single balloon treatment in preventing progression from overweight to obesity and to evaluate its effect on weight management in these patients.
The Nurses’ Health Study found an increased relative risk of death during 16 years of follow-up, even at quite modest levels of overweight, among women who had never smoked—odds ratios versus BMI <19 were 1.3 for BMI 25–26.9, 1.6 for BMI 27–28.9 and 2.1 for BMI 29–31.9 [4].
Most people with type 2 diabetes are overweight (about 75 %), and prospective population studies confirm a close relationship between overweight and risk of developing type 2 diabetes [5]. The Nurses’ Cohort Study—a 14-year study of more than 100,000 women aged 30 to 55 years—found that, after adjustment for age, BMI was the dominant predictor of the risk of type 2 diabetes. Compared with a BMI below 22, there was an eightfold increase in risk for type 2 diabetes at a BMI of 25–26.9, a 16-fold increase at BMI 27–28.9 and a 28-fold increase at BMI 29–30.9 [6]. Similar findings have been reported in men, with an increased risk of type 2 diabetes for all BMI levels of 24 and above; a BMI of 27 at age 21 years increased the risk of type 2 diabetes by more than sixfold [7].
In addition to diabetes, several other cardiovascular risk factors are influenced by overweight, including hypertension, dyslipidaemia and haemostatic factors [5]. In the Framingham Heart Study, body weight—independent of several traditional risk factors—was directly related to the development of congestive cardiac failure, and the risk of coronary heart disease (CHD) increased with body weight in both men and women [8]. In the Nurses’ Cohort Study, the relative risk of CHD compared with a BMI <21 was 2.1 for a BMI of 25–28.9 and 3.6 for a BMI >29 [9].
Overweight and obesity are also associated with cerebrovascular disease, as well as with a wide range of respiratory, gastrointestinal and metabolic disorders [5]. Cancers that are more common in overweight and obese people include those of the breast, endometrium, cervix and prostate [5]. The significant health risks and healthcare burden associated with overweight and obesity clearly begin at relatively low BMI and increase with increasing weight. This demonstrates the importance of patients’ weight management very early in the progression of the disease, both to reduce the health risks associated with overweight and to prevent progression to obesity. Dietary, lifestyle, pharmacological, psychological and surgical interventions all have a potential role in the treatment of overweight and obesity. Treatment options are, however, lacking for overweight people who have failed to lose weight with dietary and other approaches and whose BMI is not high enough to indicate surgical intervention.
In this sample of 261 overweight patients in three European centres, placement of an intragastric balloon resulted in a mean %BMI loss of 11.5 % and a mean %EWL of 58.8 % at the time of balloon removal (6 months). More than half of these losses were sustained at 3-year follow-up from BIB removal. The intragastric balloon was associated with a low complication rate and high rates of patient satisfaction and resolution of co-morbidities.
The finding that many patients maintained the weight loss achieved by the 6-month balloon treatment in the medium term (42 months) suggests that BIB can be used, in combination with other treatments, as part of a strategy for preventing the progression of overweight to obesity. One explanation for the efficacy of the intragastric balloon in these patients may be that disordered alimentary behaviours and co-morbidities are not as deeply rooted in overweight patients as in obese patients and may have greater potential for reversal.
In addition, BIB is a repeatable treatment. In fact, an Italian study found better post-intervention weight loss in patients who received two consecutive intragastric balloon treatments compared with those who followed a 7-month diet programme after removal of the balloon [18]. In a clinical experience in Spain, 112/174 patients received a second BIB (usually 1 month after the removal of the first one), and these patients continued to lose weight [14].
Dietary and other behavioural interventions have repeatedly been shown to have limited efficacy in overweight and obese people. In the 1980s, a US study found that a combination of very low calorie diet and behavioural therapy was significantly more effective than either intervention alone at the end of the intervention (6 months) and after 1 year. However, after 5 years, a majority of patients in all three groups had returned to their pre-treatment weight [19]. A recent study of a Web-based diet and physical activity programme found that the 12-month intervention improved the diet and activity behaviours of overweight and obese men, but weight loss occurred only for those with the highest adherence [20]. A systematic review of multicomponent weight management programmes (diet, exercise and behaviour therapy) in overweight and obese adults, including 12 randomised controlled trials, concluded that weight changes were small and weight regain was common in those studies that measured it [21].
The low complication rate and the absence of complications associated with intragastric balloon placement in this study are important, especially as the patients involved were overweight rather than clinically obese. Patient satisfaction with the treatment was high, with only 15 % of patients scoring 3/10 or below and 37 % scoring 8/10 or above. We found that the satisfaction level is lowering together with the weight increase postoperatively or post-gastric balloon removal in BMI > 35 patients. This observation was not confirmed in overweight patients maybe because these patients were not so scared by morbid weight and co-morbidities. To clarify and understand this observation, more dedicated studies in this field are needed.
The intragastric balloon positioning is recommended for temporary use in patients with BMI > 35 kg/m2. After its removal, usually a high rate of patients would regain the initial weight during the following months. It has been showed as good procedure to improve the co-morbidities, lower the ASA score and ameliorate the laparoscopic surgical field prior to the following surgical bariatric procedure. The role of intragastric balloon in overweight patients is not clearly stated because of a lack of wide experience on this field. In fact, overweight patients with 27–30 BMI are a large and important group of population who are usually left out of the bariatric treatment algorithm as they are often considered to have lower mortality risk as compared to the clinically obese populations.
One of the major reasons for promoting weight loss in overweight patients is to reduce the likelihood of weight-related co-morbidities, with excess weight known to increase the risk for type 2 diabetes, cardiovascular disease, hypertension and stroke and certain forms of cancer [1–9]. A significant linear relationship exists between body weight and both hypertension and diabetes, making control of excess body weight important for their prevention and treatment [22]. Apart from calorie restriction obtained through the procedure, improvement of insulin resistance and insulin sensitivity (mainly related to weight loss) also contributes to better glycaemic control among obese diabetic patients undergoing bariatric surgery [22].
A weight loss of 5 kg has been shown to reduce the risk of women developing type 2 diabetes by at least 50 % [6]. Also in women, a weight loss of more than 9 kg was associated with about 25 % reduction in all-cause cardiovascular and cancer mortality [23]. A 10-kg weight loss reduces systolic blood pressure by 10 mmHg and diastolic blood pressure by 20 mmHg as well as decreases total cholesterol by 10 %, LDL cholesterol by 15 % and triglycerides by 30 % [5].
Mean weight losses in this study were over 5 kg at 6 months in all three centres (>10 kg in Madrid) and were still over 5 kg at 3 years after balloon removal in two of the centres (4.68 kg in Liège). The rates of diabetes, hypertension, dyslipidaemia and osteoarthropathy were all one third to one half lower at 3 years after the intragastric balloon treatment compared with baseline.
Conclusion
The BioEnterics Intragastric Balloon system is safe and effective in treating overweight patients with BMI 27–30. This is a useful tool for clinicians to prevent progression to obesity and reduce important co-morbidities associated with excess weight and may have implications for the future management of overweight patients.
References
World Health Organization. Factsheet: obesity and overweight. http://www.who.int/hpr/NPH/docs/gs_obesity.pdf.
Seidell JC. The impact of obesity on health status: some implications for health care costs. Int J Obesity. 1996;19 Suppl 6:S13–6.
Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–78.
Manson JE, Willett WC, Stampfer MJ, et al. Body weight and mortality among women. N Engl J Med. 1995;333:677–85.
Jung RT. Obesity as a disease. Br Med Bull. 1997;53:307–21.
Colditz GA, Willett WC, Rotnitsky A, et al. Weight gain as a risk factor for clinical diabetes in women. Arch Intern Med. 1995;122:481–6.
Chan JM, Rimm EB, Colditz GA, et al. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994;17:961–9.
Hubert HB, Feinleib M, McNamara PM, et al. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67:968–77.
Willet WC, Manson JE, Stampfer MJ, et al. Weight, weight change, and coronary heart disease in women. JAMA. 1995;273:461–5.
NIH Conference. Gastrointestinal surgery for severe obesity. Consensus development conference panel. Ann Intern Med. 1991;115:956–61.
Messina T, Genco A, Favaro R, et al. Intragastric balloon positioning and removal: sedation or general anesthesia? Surg Endosc. 2011;25:3811–4.
Sallet JA, Marchesini JB, Paiva DS, et al. Brazilian multicenter study of the intragastric balloon. Obes Surg. 2004;14:991–8.
Genco A, Bruni T, Doldi SB, et al. BioEnterics Intragastric Balloon: the Italian experience with 2,515 patients. Obes Surg. 2005;15:1161–4.
Lopez-Nava G, Rubio MA, Prados S, et al. BioEnterics® Intragastric Balloon (BIB®): single ambulatory center Spanish experience with 714 consecutive patients treated with one or two consecutive balloons. Obes Surg. 2011;21:5–9.
Angrisani L, Lorenzo M, Borrelli V, et al. Is bariatric surgery necessary after intragastric balloon treatment? Obes Surg. 2006;16:1135–7.
Genco A, Cipriano M, Bacci V, et al. BioEnterics Intragastric Balloon (BIB): a short-term, double-blind, randomised, controlled, crossover study on weight reduction in morbidly obese patients. Int J Obes. 2006;30:129–33.
Genco A, Balducci S, Bacci V, et al. Intragastric balloon or diet alone? A retrospective evaluation. Obes Surg. 2008;18:989–92.
Genco A, Cipriano M, Bacci V, et al. Intragastric balloon followed by diet vs intragastric balloon followed by another balloon: a prospective study on 100 patients. Obes Surg. 2010;20:1496–500.
Wadden TA, Sternberg JA, Letizia KA, et al. Treatment of obesity by a very low calorie diet, behaviour therapy, and their combination: a five-year perspective. Int J Obes. 1989;13 Suppl 2:39–46.
Patrick K, Calfas KJ, Norman GJ, et al. Outcomes of a 12-month web-based intervention for overweight and obese men. Ann Behav Med. 2011;42(3):391–401.
Loveman E, Frampton GK, Shepherd J, et al. The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: a systematic review. Health Technol Assess. 2011;15(2):1–182.
Pappachan JM, Chacko EC, Arunagirinathan G, et al. Management of hypertension and diabetes in obesity: non-pharmacological measures. Int J Hypertens. 2011;3:98–105.
Williamson DF, Pamuk E, Thun M, et al. Prospective study of intentional weight loss and mortality in never-smoking overweight US white women aged 40–64 years. Am J Epidemiol. 1995;141:1128–41.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Genco, A., López-Nava, G., Wahlen, C. et al. Multi-Centre European Experience with Intragastric Balloon in Overweight Populations: 13 Years of Experience. OBES SURG 23, 515–521 (2013). https://doi.org/10.1007/s11695-012-0829-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0829-3