Abstract
Summary
Lower bone mineral density, vitamin D deficiency, lower lean body mass, greater loss of excess weight, and increased bone turnover are complications found after bariatric surgery correlated in the literature with increased risk of fractures. The prevention and treatment of such complications should begin immediately after surgery.
Introduction
The aims of the study were to evaluate bone mass in patients undergoing bariatric surgery by the Wittgrove technique after 1 year of the procedure and correlate it with body composition, weight loss, 25OH vitamin D levels, and markers of bone metabolism.
Methods
The operated group (OG) participated in a clinical consultation; a blood sample taken and a body composition; and bone mineral density assessment by dual energy X-ray absorptiometry (DXA). The results were compared with a control group (CG).
Results
Fifty-six subjects in the OG and 27 in the CG were included. The bone mineral density (BMD), after the surgery, at the lumbar spine (LS) was lower in the OG than in the CG. There was a positive correlation between total body (TB) BMD with 25OHD, body mass index (BMI), and lean mass and an inverse correlation with percentage of excess weight loss (%EWL). Vitamin D deficiency was seen in 60.41 % (OG) and in 16.6 % (CG). PTH was higher in the OG, with secondary hyperparathyroidism in 41.7 %. In 26.5 % and 14.2 % of the OG, ALP and OC levels were above the reference values. In <50 years, elevated values of carboxy-terminal telopeptide (CTX) were found in 66.7 % of patients. A difference was observed in the variation of CTX between 12 and 18 months when compared to over 24 months.
Conclusions
Lower BMD was observed, correlated with lower lean body mass and greater loss of excess weight. Vitamin D deficiency with high prevalence of secondary hyperparathyroidism and high bone turnover was detected. The prevention of bone loss should be initiated in the first months after surgery, which is a period associated with severe muscle loss and increased bone turnover.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has been widely used as a treatment for clinically severe obesity, with Wittgrove and Clark’s Roux-en-Y gastric bypass (RYGB) being one of the most common techniques used. This surgery provides significant reduction in body weight associated with improvement of comorbidities, with numerous proven benefits for health resulting from weight loss. However, despite the improvement of comorbidities, it is known that this procedure can also result in significant nutritional deficiencies in varying degrees of severity. Among them, abnormalities in calcium metabolism and vitamin D occur with frequency [1].
Some authors state that in parallel with weight reduction in approximately 10 % of obese individuals, a reduction of 1 to 2 % of bone mass can occur in various skeletal sites. The bone loss during the weight reduction process may be associated with loss of lean body mass and with an inadequate calcium and protein intake. Thus, there is an influence on the calcium-PTH axis, with increased osteoclastic activity [2].
The aims of this study were to evaluate bone mass in patients at least 1 year after they had undergone bariatric surgery by the Wittgrove and Clark’s technique and to correlate it with body composition, weight loss, use of supplements, 25OH vitamin D levels, and markers of bone metabolism.
Materials and methods
We conducted an observational, cross-sectional, and single-center study at a private practice institute. The study was approved by the Hospital de Clínicas da Univerisdade Federal do Paraná Ethics Committee on Human Research. All patients signed an informed consent. The inclusion criteria consisted of men and women (with regular menstrual cycle) with severe obesity, age ≥25 years, who, 12 months or more prior to participation, had undergone bariatric surgery by the Wittgrove and Clark’s technique performed by one of the three surgeons participating in this study. This is a mixed technique, similar to the Fobi-Capella technique, leaving a gastric pouch of approximately 30 mL, but more rounded, and insulating the entire stomach, the jejunum, and the ileum. This can handle a simple gastro-jejunal loop of 1 m and 40 cm of common food [3]. The exclusion criteria were as follows: patients unable to be contacted or who did not undergo the required exams; patients taking any drug or who had a disease that could interfere with bone metabolism; pregnant or menopausal women; women with any period of amenorrhea; and patients being treated for osteoporosis, except those taking calcium and vitamin D only.
The research protocol was conducted in three phases: first, we performed a survey of the medical records of the patients who had undergone the bariatric surgery by the technique of the study. Individuals who met the inclusion criteria were contacted by telephone or mail and were asked to participate in the second phase of the protocol. This phase consisted of a clinical consultation in which we performed clinical history, application of sun exposure, and lifestyle questionnaire including information about physical activity, alcohol intake, tobacco habits, and the use of multivitamins after the surgical procedure. During the third phase, blood and urine samples were collected and bone mineral density was measured by dual energy X-ray absorptiometry (DXA). Convenience sampling was used for recruiting participants for this study.
The control group (CG) was matched with the surgery group, according to sex, age, race, and body mass index (BMI). Each control was paired with two of the operated group (OG), with accepted age variations up to 2 years and up to two points in BMI. Individuals in the CG underwent the same evaluations as those in the OG, except for bone turnover markers.
Biochemical analysis
Study participants underwent blood sampling after 10 h of fasting. The following tests were performed: total calcium (normal range (NR) 8.8 and 11 mg/dL); phosphorous (NR 2.7 and 4.5 mg/dL); magnesium (NR 1.9 and 2.5 mg/dL); albumin (NR 3.5 and 4.8 g/dL); total alkaline phosphatase by p-nitrophenylphosphate method (NR 53–128 U/L for men between 20–50 years, 56–119 U/L for men above 50 years, and 42–98 U/L for women aged 20–50 years); carboxy-terminal telopeptide (CTX), measured by electrochemiluminescence method (NR 80–320 pg/mL for men aged 20 to 50 years, up to 704 pg/mL for men 50–70 years, and 70–573 pg/mL for premenopausal women over 20 years); osteocalcin by electrochemiluminescence method (NR 24–70 ng/mL for men 18–30 years old, 14–42 ng/mL for men 30–50 years old, 14–46 ng/mL for men 50 to 70 years, and 11 to 43 ng/mL for premenopausal women over 20 years); PTH, by IMMULITE chemiluminescence method (NR 11 to 67 pg/ mL); and calcium/creatinine ratio (NR up to 0.25), for which the patients were instructed to collect the first morning urine in a specific sterile cup.
Serum 25-hydroxyvitamin D (25OHD) levels were measured by chemiluminescence method using the LIAISON® commercial kit and were classified according to the Endocrine Society’s latest guidelines for vitamin D levels: deficiency, below 20 ng/mL; insufficiency, between 21 and 29 mg/mL; and normal, up to 30 ng/mL [4].
Bone mineral density and body composition
Bone mineral density (BMD) and body composition were measured by DXA in a LUNAR DPX NT® model at the Center for Innovative Therapies (CETI), by a trained technician and under researcher monitoring, and the results were evaluated by a single enabled physician. The regions evaluated were total body (TB), lumbar spine (LS) (average of L1–L4), femoral neck (FN), and total femur (TF). The precision coefficients were 1.3 % for LS, 1.28 % for FN, and 0.56 % for TF. The BMD results were expressed as grams per square centimeter and also through Z-scores as determined by the International Society for Clinical Densitometry (ISCD) [5].
The body composition analysis was performed on the same DXA device. Total adipose tissue and total muscle weight, expressed in kilograms and as a percentage, were compared to the National Health and Nutrition Examination Survey (NHANES) data, published in the literature [6].
Assessment of nutritional status
The patient’s weight (kg), without shoes and wearing light clothing, was measured on a digital electronic balance (Toledo do Brasil®) with maximum capacity of 200 kg and an accuracy of 50 g. Height (m) was measured using a Tonelli® brand stadiometer, fixed 50 cm from the floor, with the person in standing position without shoes, back straight, heels together, and arms extended alongside the body.
BMI was determined and classified according to the World Health Organization (WHO) [7]. The weight before surgery was reported by the individuals and subsequently used to calculate the mean percentage of excess weight loss (%EWL), which is the standard in the bariatric surgery nomenclature. This calculation is derived from the following formula: percentage of excess weight loss = (weight loss/excess weight) × 100, where excess weight = total preoperative weight—ideal weight [8].
History of morbidity, family history, life habits, and use of drugs
Participants were asked about previous fractures, osteoporosis family history (mother, grandparents, and/or aunts), smoking, and alcohol intake. The practice of programmed physical activity was classified according to the intensity and frequency of exercises: mild, less than three times per week with practice of 1 h at a time; moderate, three to five times a week, with practice at least 1 h per time; and intense, at least five times per week over 2 h at a time (adapted from Fonseca et al.) [9].
The use of current multivitamins, polyminerals, and medications, including supplementation with vitamin D, was questioned at the time of the interview.
Statistical analysis
The variables selected for statistical analysis were initially submitted to the Shapiro-Wilk test and the Kolmogorov-Smirnov test, which verified the assumption of their symmetrical (normal) distribution. Symmetrical distribution of the variables is presented as mean ± standard deviation (SD), while the asymmetric variables are presented as median, minimum, and maximum values.
For mean comparison, the Kolmogorov-Smirnov test was applied. Fisher’s and chi-square tests were applied for categorical variables. For correlation analysis, the Pearson’s and Spearman’s coefficients were used, which evaluated the association between continuous variables with symmetric and asymmetric distribution, respectively. In addition, multiple linear regression was performed. For all analyses, two-tailed tests with a minimum significance level of 5 % were used.
Results
Characteristics of control and operated groups
Of the total 366 patients at the study center who had undergone bariatric surgery, 76 subjects who had undergone gastroplasty by the Wittgrove and Clark’s technique (RYGB) met the inclusion criteria and were interviewed, while 20 refused to further participate. In total, 83 participants completed the study: 56 subjects in the operated group (OG) and 27 subjects in the control group (CG).
Among the participants of the OG, 47 were women (two of African descent) and nine men (all White). The mean age was 36.4 ± 8.5 years, the mean postoperative BMI was 28.2 ± 4.2 kg/m2, and the mean postoperative time was 33.3 ± 15.8 months. Eight subjects (14.3 %) reported a family history of osteoporosis. Regarding the life habits, 36 (64.3 %) subjects were classified as sedentary, 14 (25 %) as mildly physically active and six (10.7 %) as moderately active. Seventeen patients (30.3 %) reported a smoking history and only one was a current smoker.
The control group (CG) consisted of 20 women (one of African descent) and seven men (all White). The mean age was 36.9 ± 9.6 years and mean BMI was 27.2 ± 4.2 kg/m2. Regarding the life habits, 12 (44.4 %) subjects were sedentary, eight (29.6 %) mildly active, and seven (25.9 %) moderately active. Three (11.1 %) were current smokers and two (7.4 %) reported smoking in the past. Family history of osteoporosis was reported by four (14.8 %) individuals. The general characteristics were not significantly different between the two groups (Table 1).
Supplementation with vitamin D was used by 38 (67.8 %) operated patients for an average of 16.1 ± 11 months after the procedure. The mean dosage used was 423.7 ± 54.2 IU/day. Only one individual used 20,000 IU /week for a period of 3 months. CG patients were not taking vitamin D or any other dietary supplements.
The %EWL of the OG was on average 73.5 ± 19.8 %, considered a satisfactory result. Nine operated patients (16 %) lost less than 50 % of the excess weight. There were significant differences between preoperative (41.8 ± 4.7 kg/m2) and postoperative (28.2 ± 4.2 kg/m2) BMI (p < 0.001) in this group of patients.
Biochemical analysis
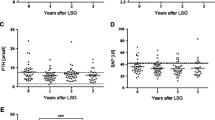
Blood calcium, magnesium, and phosphorus levels were within normal values in both groups. However, the OG had higher serum levels of phosphorus than the control group (p < 0.001) (Table 2). The levels of 25OH vitamin D were lower in patients of the OG compared to the CG (21.3 ± 10.9 vs 32.1 ± 11.8 ng/dL, p < 0.01). Twenty-nine patients in the OG (60.41 %) and three in the CG (16.6 %) had vitamin D deficiency (p < 0.001). However, vitamin D insufficiency was similar between groups, 12 patients (25 %) in the OG and six patients (33.3 %) in the CG (Fig. 1). PTH serum levels were higher in the OG than in the CG (68.1 ± 32.9 vs 39.9 ± 11.9 pg/mL, p < 0.001). Twenty-two patients in the OG (45.8 %) and only one in the CG (5.6 %) had PTH levels above normal values (p < 0.01), and the diagnosis of secondary hyperparathyroidism, with low levels of vitamin D, associated with the elevation of PTH, was found in 41.7 % (20) patients of the OG. There was an inverse correlation between 25OHD and PTH in OG patients (r = −0.41, p = 0.005) and in CG patients (r = −0.61, p = 0.01). No correlation between levels of 25OH vitamin D and BMI, percentage of fat and lean mass, use of multivitamins and polyminerals with %EWL, and sun exposure was observed.
The mean calcium/creatinine ratio was 0.27 ± 0.8, and hypercalciuria was found in three patients (6.3 %) of the OG. The mean serum levels of alkaline phosphatase, osteocalcin, and CTX in the operated women were within the normal range for premenopausal women: 88.5 ± 36.9 U/L, 28.4 ± 11.2 ng/mL, and 532.5 ± 225.3 pg/mL, respectively. In 13 (26.5 %) and seven (14.2 %) patients in the OG, alkaline phosphatase and osteocalcin levels were above the reference values. Fifteen women (37.5 %) had CTX levels above normal, and seven of these had secondary hyperparathyroidism. Among men older than 50 years, the mean values of alkaline phosphatase, osteocalcin, and CTX were within the limits considered normal for their age. However, in individuals under 50 years, elevated values of CTX (945.1 ± 523.8 pg/mL) were found in 66.7 % of patients, suggesting an increased bone resorption (Table 3).
There was a difference in the variation of CTX considering the time after surgery, 12–18 months when compared to over 24 months, (p < 0.05) (Fig. 2). Inverse correlation was observed between the postoperative time with CTX levels (r = −0.37, p = 0.01) and osteocalcin levels (r = −0.3, p = 0.04).
Bone mineral density and body composition
The mean BMD at the LS was significantly lower in the OG than in the CG (1.203 ± 0.15 g/cm2 vs 1.282 ± 0.16 g/cm2, p < 0.05), as well as the Z-score (−0.05 ± 1.19 vs 0.77 ± 1.31 DP, p < 0.05). The BMD measures at the TB, TF, and FN in both groups were similar: TB (OG 1.195 ± 0.01 vs CG 1.226 ± 0.01 g/cm2), TF (OG 1.030 ± 0.13 vs CG 1.081 ± 0.16 g/cm2), and FN (1.039 ± 0, 18 vs 1.042 ± 0.15 g/cm2). A low BMD for chronological age (Z-score < −2.0) was observed at the LS in four individuals of the OG (8 %), but in no one of the CG (p < 0.05).
There was a positive correlation between TB BMD with serum calcium (r = 0.36, p = 0.03), 25OH vitamin D (r = 0.37, p = 0.01), BMI (r = 0.27, p = 0.05), lean mass (kg) (r = 0.48, p = 0.0005), and an inverse correlation with %EWL (r = −0.29, p = 0.04).
No correlation was observed between BMD, time after surgery, and biochemical parameters. In the OG, there was a trend of correlation between BMD at LS and lean body mass (kg) (r = 0.23, p = 0.059). However, in TF BMD, a positive correlation was found with lean body mass (kg) (r = 0.36, p = 0.01) and a negative correlation with %EWL (r = −0.29, p = 0.04).
No differences between body composition parameters were observed in the two groups. The mean percentage of lean body mass (LBM) was 58.9 ± 6.3 % in the OG and 60.1 ± 17.8 % in the CG. The percentage of fat mass (FM) was 36.2 ± 5.8 % in the OG and 36.7 ± 7.9 % in the CG.
In the multiple linear regression analysis, serum calcium, BMI, %EWL, and PTH together explained 65 % of the changes in serum levels of vitamin D in the OG. Indeed, BMI, % of FM, and 25OHD levels explained 41 % of TB BMD and the lumbar spine Z-score was 44 % affected by osteocalcin, alkaline phosphatase, magnesium, 25OHD, vitamin D supplementation, and caffeine (Table 4).
Discussion
The weight loss induced by bariatric surgery reduces complications associated with obesity. A result is considered satisfactory when the %EWL is greater than 50 % [3]. In our study, patients exhibited a high average of %EWL (70 %). However, the rapid weight loss that occurs after surgery may adversely affect bone mass due to increased bone resorption, vitamin D deficiency, reduced lean body mass, and a low absorption of calcium and vitamin D. Some authors state that the loss in bone mass could be attenuated with calcium and vitamin D supplementation [10, 11].
A low bone mass compared with chronological age was seen in 8 % of the operated patients but not in the control group, and the lumbar spine BMD was lower in the operated compared to controls. The trabecular bone is typically more metabolically active, and the spine is rich in trabecular bone in a ratio of 25:75 (cortical/trabecular); so, the loss of bone at this site is compatible with the high turnover observed after bariatric surgery [12]. Abbasi et al. [13] demonstrated osteoporosis in 12.5 % and osteopenia in 39.7 % in a study with 136 patients, mean age 48.34 ± 10.28 years, who had undergone a malabsorptive bariatric surgery 5 years prior. The BMD at all sites was reduced in correlation with the lowest lean mass and weight loss. Similar BMD reduction in spine (−7.4 % ± 6.8 %) and femur (−10.5 % ± 5.6 %) was described in 42 premenopausal women 12 months after Roux-en-Y gastric bypass, correlated with the initial weight and the percentage of weight loss. The greater the weight loss, the greater the reduction in BMD at all sites [14].
Some studies have shown that bone loss after bariatric surgery, associated with loss of weight and lean mass [15, 16], included postmenopausal women, who may have had other risk factors for bone loss. In this study, however, we included only premenopausal women and most men were under 50 years of age.
Clinical risk factors for osteoporosis, such as lack of physical activity, smoking, or family history of osteoporosis, in the linear regression and multivariate analysis, did not influence the BMD, suggesting that in this group, other factors are more important for the bone mass. A review article by Viegas et al. [17] failed to prove, in the same way, that the above-cited factors influence bone mass in this specific population of patients.
The reduction in BMD in young individuals increases the risk of fractures, causing an impact on quality of life and possibly limiting productivity. Two recent studies show that, regardless of age, patients who undergo bariatric surgery are at an increased risk of any fractures of 2.3 times (95 % CI 1.8–2.8) [17, 18]. No patients reported clinical fracture, but we did not evaluate the presence of asymptomatic fractures.
The obese population is at high risk for vitamin D deficiency due to low sunlight exposure, less mobility, over clothing, and inadequate intake of enriched foods, in addition to the greater amounts of vitamin D stored in adipose tissue [19, 20]. BMI, body weight, and fat mass are inversely related to serum 25OHD levels [21]. Thus, several studies demonstrated low levels of vitamin D before bariatric surgery with further worsening with the surgical procedure [22].
Several factors contribute to vitamin D deficiency after the surgery, such as reduced caloric intake, reduction of the gastric volume, and defective absorption resulting from fat malabsorption (delayed mixing of fat with the pancreatic enzymes and biliary salts) in addition to the shortening of the small bowel where absorption occurs. Poor food tolerability, lack of compliance with oral supplementation, preoperative vitamin D status, and reduced 25-hydroxylation in the liver due to steatosis can also contribute to vitamin D deficiency after bariatric surgery [23, 24]. A recently published study showed that preoperative status, long bypass limb length, and African-American race, but not preoperative BMI, are predictors of postoperative vitamin D deficiency [25]. In sum, hypovitaminosis D after bariatric surgery has numerous causes. Much is known about absorption of vitamin D in normal physiology; however, details on absorption after RYGB have yet to be fully elucidated. Consequently, well-designed vitamin D absorption studies comparing different bariatric procedures, while controlling for UVB exposure and dietary vitamin D intake and accounting for the potential contribution from adipose tissue, are needed [26].
Many previous publications reported vitamin D deficiency after bariatric surgery, ranging from 50 to 80 % [27, 28]. Six months after a RYGB procedure, only 9 % of the men and 15 % of the women have adequate levels of vitamin D [29]. Similar to the literature, the OG in this study had a high prevalence of vitamin D deficiency (60.41 %) and insufficiency (25 %) with no correlation with solar exposure. The correlation analysis showed that the lower the levels of 25OHD, the greater the weight loss and the higher the PTH levels. Findings similar to those of Sanchez-Hernandez after Capella’s surgery, 42.2 % deficiency and 37.5 % insufficiency, were inversely correlated with weight loss but not correlated with sun exposure [30]. One reason for the lack of correlation with solar exposure in our study and in the Sanchez-Hernandez et al. study is that other factors such as skin phototypes may also influence the synthesis of vitamin D [31].
Vitamin D supplementation in the patients of our study was far below the dosage recommended and not sufficient to prevent hypocalcemia and hypovitaminosis D. These findings are amply demonstrated in the literature in patients after gastroplasty. Even daily calcium (1800 mg) and vitamin D (1200 IU) supplementation was not able to prevent hypovitaminosis D and secondary hyperparathyroidism [32]. However, the use of large amounts (50.000 IU) by Mahlay et al. [33] preoperatively in patients with vitamin deficiency, followed by 800 IU in the postoperative, reduced the prevalence of 25OHD deficiency from 83 % to 47 %. However, the dosage and duration of supplementation were not enough to reverse 100 % of vitamin D deficiency. These researchers point out the difficulty in the follow-up of bariatric patients, limiting the establishment of studies and adequate supplementation protocols for this group. Another determinant factor for supplemental calcium and vitamin D after bariatric surgery is the need for individualization in the dosage of these nutrients, considering primarily the severity of vitamin D deficiency in each individual [34]. The last guideline of the Endocrine Society recommends for obese patients or patients with disabsortive syndrome a dose 2–3 times greater than that for the general population—at least 6000 to 10.000 IU/day for treating vitamin D deficiency, followed by a dose from 3000 to 6000 IU/day to keep the levels above 30 ng/mL [4].
The complex association between 25OHD, PTH, and obesity has been described in several studies with different techniques and different postoperative times. Deficiency of 25OHD and secondary hyperparathyroidism have been demonstrated both in the first year after surgery and after 5 years of the procedure. A negative correlation was observed between PTH and 25OHD, and a positive one between PTH with BMI and fat mass. The mechanism of this alteration probably occurs by the subcutaneous sequestration of vitamin D by the adipose tissue [35, 36]. The multiple linear regression analysis, reported in this paper, confirms the influence of different variables in BMD and vitamin D levels after bariatric surgery.
Several authors have reported that obesity alone is a risk factor for 25OHD deficiency and secondary hyperparathyroidism, which can worsen after weight reduction in subjects who have undergone bariatric surgery [37–39]. Our study corroborated this fact, since 35.7 % of the operated patients exhibited secondary hyperparathyroidism due to vitamin D deficiency.
We found hypocalcemia in only 14.3 % of the operated group, which is consistent with the literature, since most patients with secondary hyperparathyroidism may have normal levels of blood calcium, a phenomenon usually observed due to the efflux of calcium bone induced by PTH [40]. Diniz et al. [41] evaluated 110 patients undergoing Capella technique Y-Roux and found that 29 % showed elevation of PTH and only one had hypocalcemia.
In the present study, increased bone resorption occurred in 43 % of cases with elevated markers of bone turnover, such as alkaline phosphatase, osteocalcin, and CTX, similarly to the high levels of osteocalcin in 20 % of women after 8 years of bariatric surgery described in the literature [42]. The increase in osteocalcin levels after bariatric surgery is associated with BMD reduction and weight loss [42]. Compared to controls, women after RYGB had higher levels of osteocalcin (68.7 % vs 19 %, p < 0.001), CTX (33.3 % vs 2.4 %, p < 0.001), and alkaline phosphatase, correlated with the PTH levels [43].
The CTX levels in this study correlated inversely with postoperative time, thereby demonstrating that bone resorption is more intense during the first years after the procedure. These findings are consistent with the study of El-Kadre et al. [44], who observed increased bone resorption and PTH levels associated with decreased levels of 25OHD within the first 6 months after RYGB. The increase of CTX in the first year after surgery followed by a partial reduction in the second year was observed by Moreiro et al. Surprisingly, in the same period, there was an increase from 46 to 64 % in the prevalence of secondary hyperparathyroidism, even with calcium (1200 mg) and vitamin D (800 IU) supplementation [45].
The limitation of our study is that we had no previous exam (before surgery) for comparison. Thus, we could not assume that there was a bone loss in the OG, just that it was lower compared with age and the CG. In the same way, the biochemical analysis cannot be compared with preoperative values.
Conclusion
Lower bone mineral density was observed in the OG and was correlated with lower lean body mass and greater loss of excess weight. Also, vitamin D deficiency with high prevalence of secondary hyperparathyroidism and high bone turnover was detected, facts that in the literature are correlated with increased risk of fractures. In spite of this risk being more commonly observed in the late postoperative period (over 2 years), the prevention of bone loss should be initiated in the first months after surgery, which is a period associated with severe muscle loss and increased bone turnover. Planned interventions in the preoperative and postoperative periods to minimize the loss of lean body mass, in addition to individualized calcium and vitamin D supplementation, and periodic monitoring, should be priorities in these individuals.
References
Whitlock KA, Gill RS, Ali T, Shi X, Birch DW, Karmali S (2013) Early outcomes of Roux-en-Y gastric bypass in a publically funded obesity program. ISRN Obes 2013:296597
Riedt CS, Brolin RE, Sherrell RM, Field MP, Shapses SA (2006) True fractional calcium absorption is decreased after Roux-en-Y gastric bypass surgery. Obesity (Silver Spring) 14(11):1940–1948
Wittgrove AC, Clark GW (2000) Laparoscopic gastric bypass, Roux-en-Y- 500 patients: technique and results, with 3–60 month follow-up. Obes Surg 10(3):233–239
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM, Endocrine Society (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96(7):1911–1930
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive summary of the 2013 international society for clinical densitometry position development. Conference on bone densitometry. J Clin Densitom 16(4):455–466
Kelly TL, Wilson KE, Heymsfield SB (2009) Dual energy X-Ray absorptiometry body composition reference values from NHANES. PLoS One 4(9):e7038
Obesity: preventing and managing the global epidemic (2000) Report of a WHO consultation. World Health Organ Tech Rep Ser 894:i-xii, 1–253
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292(14):1724–1737
Fonseca VM, Sichieri R, Veiga (1998) Fatores associados a obesidade em adolescentes. Rev Saude Publica 32(6):541–549
Bowen J, Noakes M, Clifton PM (2004) A high dairy protein, high-calcium diet minimizes bone turnover in overweight adults during weight loss. J Nutr 134(3):568–573
Youssef Y, Richards WO, Sekhar N, Kaiser J, Spagnoli A, Abumrad N, Torquati A (2007) Risk of secondary hyperparathyroidism after laparoscopic gastric bypass surgery in obese women. Surg Endosc 21(8):1393–1396
Clarke B (2008) Normal bone anatomy and physiology. Clin J Am Soc Nephrol 3(Suppl 3):S131–S139
Abbasi AA, Amin M, Smiertka JK, Grunberger G, MacPherson B, Hares M, Lutrzykowski M, Najar A (2007) Abnormalities of vitamin D and calcium metabolism after surgical treatment of morbid obesity: a study of 136 patients. Endocr Pract 13(2):131–136
Carrasco F, Ruz M, Rojas P, Csendes A, Rebolledo A, Codoceo J, Inostroza J, Basfi-Fer K, Papapietro K, Rojas J, Pizarro F, Olivares M (2009) Changes in bone mineral density, body composition and adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg 19(1):41–46
Uebelhart B (2013) Effects of bariatric surgery on bone. Rev Med Suisse 9(390):1251–1255
Brzozowska MM, Sainsbury A, Eisman JA, Baldock PA, Center JR (2013) Bariatric surgery, bone loss, obesity and possible mechanisms. Obes Rev 14(1):52–67
Viégas M, Vasconcelos RS, Neves AP, Diniz ET, Bandeira F (2010) Bariatric surgery and bone metabolism: a systematic review. Arq Bras Endocrinol Metabol 54(2):158–163
Nakamura KM, Haglind EG, Clowes JA, Achenbach SJ, Atkinson EJ, Melton LJ 3rd, Kennel KA (2014) Fracture risk following bariatric surgery: a population-based study. Osteoporos Int 25(1):151–158
García AMJ, López VFJ, Martín CC, Sánchez VP, Cunill JLP (2012) Micronutrientes en cirugía bariátrica. Nutr Hosp 27(2):349–361
Fish E, Beverstein G, Olson D, Reinhardt S, Garren M, Gould J (2010) Vitamin D status of morbidly obese bariatric surgery patients. J Surg Res 164(2):198–202
Gemmel K, Santry HP, Prachand VN, Alverdy JC (2009) Vitamin D deficiency in preoperative bariatric surgery patients. Surg Obes Relat Dis 5(1):54–59
Kremer R, Campbell PP, Reinhardt T, Gilsanz V (2009) Vitamin D status and its relationship to body fat, final height, and peak bone mass in young women. J Clin Endocrinol Metab 94(1):67–73
Kaidar-Person O, Person B, Szomstein S, Rosenthal RJ (2008) Nutritional deficiencies in morbidly obese patients: a new form of malnutrition? Part A: vitamins. Obes Surg 18(7):870–876
Jin J, Stellato TA, Hallowell PT, Schuster M, Graf K, Wilhelm S (2009) Utilization of preoperative patient factors to predict postoperative vitamin D deficiency for patients undergoing gastric bypass. J Gastrointest Surg 13(6):1052–1057
Beckman LM, Earthman CP, Thomas W, Compher CW, Muniz J, Horst RL, Ikramuddin S, Kellogg TA, Sibley SD (2013) Serum 25(OH) vitamin D concentration changes after Roux-en-Y gastric bypass surgery. Obesity (Silver Spring) 21(12):E599–E606
da Rosa CL, Dames Olivieri Saubermann AP, Jacqueline J, Pereira SE, Saboya C, Ramalho A (2013) Routine supplementation does not warrant the nutritional status of vitamin d adequate after gastric bypass Roux-en-Y. Nutr Hosp 28(1):169–172
Toh SY, Zarshenas N, Jorgensen J (2009) Prevalence of nutrient deficiencies in bariatric patients. Nutrition 25(11–12):1150–1156
Gehrer S, Kern B, Peters T, Christoffel-Courtin C, Peterli R (2010) Fewer nutrient deficiencies after laparoscopic sleeve gastrectomy (LSG) than after laparoscopic Roux-Y-gastric bypass (LRYGB)—a prospective study. Obes Surg 20(4):447–453
Duran de Campos C, Dalcanale L, Pajecki D, Garrido AB Jr, Halpern A (2008) Calcium intake and metabolic bone disease after eight years of Roux-en-Y gastric bypass. Obes Surg 18(4):386–390
Sánchez-Hernández J, Ybarra J, Gich I, De Leiva A, Rius X, Rodríguez-Espinosa J, Pérez A (2005) Effects of bariatric surgery on vitamin D status and secondary hyperparathyroidism: a prospective study. Obes Surg 15(10):1389–1395
Cabral MA, Borges CN, Maia JM, Aires CA, Bandeira F (2013) Prevalence of vitamin D deficiency during the summer and its relationship with sun exposure and skin phototype in elderly men living in the tropics. Clin Interv Aging 8:1347–1351
Slater GH, Ren CJ, Siegel N, Williams T, Barr D, Wolfe B, Dolan K, Fielding GA (2004) Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. J Gastrointest Surg 8(1):48–55
Mahlay NF, Verka LG, Thomsen K, Merugu S, Salomone M (2009) Vitamin D status before Roux-en-Y and efficacy of prophylactic and therapeutic doses of vitamin D in patients after Roux-en-Y gastric bypass surgery. Obes Surg 19(5):590–594
Flores L, Osaba MJ, Andreu A, Moizé V, Rodríguez L, Vidal J (2010) Calcium and vitamin D supplementation after gastric bypass should be individualized to improve or avoid hyperparathyroidism. Obes Surg 20(6):738–743
Clare Grace PD, Vincent R, Aylwin SJ (2013) High prevalence of vitamin D insufficiency in a United Kingdom urban morbidly obese population: implications for testing and treatment. Surg Obes Relat Dis 10(2):355–360
Jamal-Allial A, Griffith JL, Tucker KL (2013) The longitudinal association of vitamin D serum concentrations & adiposity phenotype. J Steroid Biochem Mol Biol
Hewitt S, Søvik TT, Aasheim ET, Kristinsson J, Jahnsen J, Birketvedt GS, Bøhmer T, Eriksen EF, Mala T (2013) Secondary hyperparathyroidism, vitamin D sufficiency, and serum calcium 5 years after gastric bypass and duodenal switch. Obes Surg 23(3):384–390
Vasconcelos RS, Viégas M, Marques TF, Diniz ET, Lucena CS, Câmara Neto JB, Bandeira F (2010) Factors associated with secondary hyperparathyroidism in premenopausal women undergoing Roux-en-Y gastric bypass for the treatment of obesity. Arq Bras Endocrinol Metabol 54(2):233–238
Signori C, Zalesin KC, Franklin B, Miller WL, McCullough PA (2010) Effect of gastric bypass on vitamin D and secondary hyperparathyroidism. Obes Surg 20(7):949–952
Ocón Bretón J, Pérez Naranjo S, Gimeno Laborda S, Benito Ruesca P, García Hernández R (2005) Effectiveness and complications of bariatric surgery in the treatment of morbid obesity. Nutr Hosp 20(6):409–414
Diniz Mde F, Diniz MT, Sanches SR, Salgado PP, Valadão MM, Araújo FC, Martins DS, Rocha AL (2004) Elevated serum parathormone after Roux-en-Y gastric bypass. Obes Surg 14(9):1222–1226
Pereira FA, de Castro JA, dos Santos JE, Foss MC, Paula FJ (2007) Impact of marked weight loss induced by bariatric surgery on bone mineral density and remodeling. Braz J Med Biol Res 40(4):509–517
Santos MT, Souza FI, Fonseca FL, Lazaretti-Castro M, Sarni RO (2012) Changes in bone metabolism markers in women after Roux-en-Y gastric bypass. Arq Bras Endocrinol Metabol 56(6):376–382
El-Kadre LJ, Rocha PR, de Almeida Tinoco AC, Tinoco RC (2004) Calcium metabolism in pre- and postmenopausal morbidly obese women at baseline and after laparoscopic Roux-en-Y gastric bypass. Obes Surg 14(8):1062–1066
Moreiro J, Ruiz O, Perez G, Salinas R, Urgeles JR, Riesco M, García-Sanz M (2007) Parathyroid hormone and bone marker levels in patients with morbid obesity before and after biliopancreatic diversion. Obes Surg 17(3):348–354
Conflicts of interest
None.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costa, T.L., Paganotto, M., Radominski, R.B. et al. Calcium metabolism, vitamin D and bone mineral density after bariatric surgery. Osteoporos Int 26, 757–764 (2015). https://doi.org/10.1007/s00198-014-2962-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2962-4