Abstract
Introduction
Vertebral fractures (VF) are the most common osteoporotic fracture. They are associated with significant morbidity and mortality and are an important predictor of future fractures. The epidemiology of VF in Ireland is limited and a greater understanding of their scale and impact is needed. Therefore, we conducted a systematic review of publications on osteoporotic VF in Ireland.
Methods
Systematic searches were conducted using PubMed, Medline, Embase, Scopus and Cochrane electronic databases to identify eligible publications from Ireland addressing osteoporotic VF.
Results
Twenty studies met the inclusion criteria out of 1558 citations. All studies were published since 2000. Data was obtained on 182,771 patients with fractures. Nine studies included more than 100 subjects and three included more than 1000. Females accounted for 70% with an overall mean age of 65.2 years (30–94). There was significant heterogeneity in study design, methods and outcome measures including the following: use of administrative claims data on public hospital admissions, surgical and medical interventions, the impact of a fracture liaison service and the osteoporosis economic burden. The prevalence of VF was difficult to ascertain due to definitions used and differences in the study populations. Only two studies systematically reviewed spine imaging using blinded assessors and validated diagnostic criteria to assess the prevalence of fractures in patient cohorts.
Conclusions
Several studies show that VF are common when addressed systematically and the prevalence may be rising. However, there is a deficit of large studies systematically addressing the epidemiology and their importance in Ireland.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Osteoporosis is a significant global public health issue. One in three post-menopausal women and one in five men over the age of 50 will sustain an osteoporotic fracture in their lifetime equating to 9 million fractures per year worldwide [1, 2]. Treatment to prevent fractures in those with low bone mineral density and a prior fragility fracture is particularly effective. Unfortunately, the majority of individuals who sustain fractures are never diagnosed with osteoporosis or receive treatment for their underlying bone disease [3]. A recent world report suggests Ireland has the sixth highest rate of hip fractures worldwide, while data on other fracture types are less common [4]. Others have shown a continuous increase in the absolute numbers of major osteoporotic fractures in Ireland requiring hospitalisation, with an increase of 30% between 2000 and 2014 and a 43% increase in number of bed days. If age-standardised fracture rates remain stable, hospitalisations for osteoporotic fractures are projected to increase by 150% to 31,605 admissions in 2046 [5].
The spine is the most common osteoporotic fracture site. All vertebral fractures (VF) are associated with significant morbidity, particularly clinical fractures [6]. There is up to an eightfold increased risk in mortality following the fracture which appears to be independent of age, sex and co-morbidities [7, 8]. Left untreated, VF can progress to involve multiple levels of the thoracolumbar spine with potential for spinal instability, disabling pain and polypharmacy. Kyphotic deformities may be complicated by a loss of equilibrium, a predisposition to future falls, restrictive lung disease, dysphagia and loss of independence and result in a significant financial burden [9]. VF are an important predictor of future fractures and should trigger assessment for secondary prevention [10]. However, only one-third are diagnosed at the time of occurrence and thus, many opportunities for intervention are missed [11].
Recent reviews of the global epidemiology of VF show considerable variation between gender, ages and regions [11, 12]. The prevalence and incidence of VF varies considerably between studies, ranging from 5 to 64% [13, 14]. Data from the USA shows that VF account for more than 18% of hospital fragility fracture admissions which is second only to hip fracture and length of hospital stay is similar to hip fractures [15]. In Ireland, published studies that have used national public hospital administrative claims data have suggested that VF only account for 5% of hospitalised fragility fractures and 6% of outpatient fractures which contrasts with other epidemiological studies [5, 14,15,16].
Empirical evidence from our institution shows many spine fractures are under-reported, not coded as a diagnosis in hospital discharge summaries, and follow-up is sporadic. A greater understanding of the scale and impact is needed to guide future resource management in a financially constrained health care system. Therefore, we conducted a systematic review of published literature on osteoporotic VF in Ireland to gain a better understanding of the epidemiology, impact and cost.
Methods
This systematic review was carried out in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [17].
Selection criteria
We performed a systematic literature search to identify all interventional and observational studies addressing osteoporotic VF pertaining to Ireland and Northern Ireland. We restricted the eligible studies to full-text original articles, i.e. excluding review articles, case reports, letters and editorials. We excluded non-human data, paediatric data, non-Irish data, non-osteoporotic fractures and studies that only included bone mineral density data (rather than data on VF). No language limitations were imposed. We included multi-centre studies that included Irish data.
Search strategy
Systematic searches using PubMed, Medline, Embase, Scopus and Cochrane databases were carried out from inception to November 2018. In addition, we hand searched references from eligible studies to identify further studies for inclusion. The search strategy is outlined in Table 1. The Medical Subject Headings (MeSH) and keywords included (“vertebra*” OR “spine” OR “spinal” OR “lumbar” OR “thoracic” OR “thoracolumbar” OR “cervical”) AND (“fracture” OR “fractures”) AND (“osteoporosis” OR “fragility” OR “osteopenia”) AND (“Ireland” OR “Northern Ireland” OR “Irish”).
Data abstraction
The results generated from the search were screened for inclusion by title and abstract. The full text was assessed if required to make the decision (see Fig. 1 for flow chart for eligible studies). Any disagreements were resolved by discussion or upon consultation with the senior author if necessary. Data was extracted independently by the authors. The items for extraction included the following study characteristics: study design and duration, number of participants, age, sex, number with VF, diagnostic criteria for VF (clinical or morphometric), number prescribed anti-osteoporotic treatment, number who underwent surgical intervention for VF, reported co-morbidities, hospitalisation rates and economic analysis carried out (Table 2).
Results
Characteristics of included studies
Using the search strategy as outlined in Table 1, we obtained 1558 citations, 20 of which met our inclusion criteria. All were observational research published since 2000. There was significant heterogeneity in terms of design and reported outcomes, thereby rendering a meta-analysis inappropriate. Descriptive characteristics of included studies are summarised in Table 3, with a summary of interventions and outcomes included in Table 4.
Patient characteristics
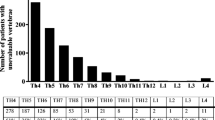
Data was obtained on 182,771 patients with fractures. Nine studies included more than 100 subjects and three studies included more than 1000 subjects. Seventy percent of participants were female with an overall mean age of 65.2 years (30–94). Fractures were defined morphometrically in nine studies and clinically (according to ICD-10, self-reported or not described) in eleven. There was a wide variation in the reported prevalence of VF ranging from 2.7 to 87% due to differences in included participants and ascertainment methods. Generally, the prevalence appeared to significantly increase after 60 years and peak after 70 years amongst patients presenting to osteoporosis services [18]. For the studies that provided information on fragility fracture subtype proportions (n = 181,050), spine fractures accounted for 5.5%, hip fractures 34.5%, radial fractures 18%, humerus 5.5% and others accounted for 36.5% [2, 5, 19,20,21].
Three studies provided descriptive information on patients (n = 385) assessed by osteoporosis/fracture liaison services and discussed potential benefits these services provide [18,19,20]. Identified risk factors in the patient cohorts include the following: a history of previous fracture (11–50%), vitamin D deficiency (49–66%), smoking history (25–37%), excess alcohol intake (4–30%), glucocorticoid intake (7–19%), history of falls (8–13%), previous hysterectomy (7%), anti-epileptic medication intake (7%) and a diagnosis of rheumatoid arthritis (4%). One author included information on further laboratory investigations for 37 male patients showing 14% (5) had positive coeliac antibody screens, 14% (5) had elevated parathyroid hormone levels and 27% (10) had low testosterone results [20].
Mohammed et al. showed a VF prevalence of 13% (77/603) amongst a cohort of patients with rheumatoid arthritis (RA) aged 40 years and older assessed by vertebral fracture assessment (VFA) imaging [22]. The majority of these fractures were classified as moderate-severe by blinded trained musculoskeletal radiologists. Forty percent of these patients did not meet T-score criteria for osteoporosis on DXA. Significant associations included older age, duration of RA, ACPA positivity, elevated markers of disease activity and a DXA classification of osteoporosis [22].
Diagnostic imaging for vertebral fractures
Two studies systematically examined VF using VFA images of patients attending osteoporosis and rheumatology services using blinded assessors and validated diagnostic criteria (Genant semi-quantitative method) to assess the prevalence of fractures [22, 23]. McGuinness et al. compared the use of lateral vertebral assessment (LVA) to diagnose VF with standard lateral spine radiographs amongst patients attending an osteoporosis clinic who had symptoms suggestive of a recent vertebral fracture including new back pain, height loss or a recent fall. A total of 95 participants were included, all of whom had T-scores less than − 2.5.The prevalence of VF amongst this pre-selected cohort was 87% (83/95), ranging from 0 to 9 fractures, 82% of which were grade 2 or 3. Overall agreement between the two methods was acceptable (weighted kappa 0.82, 95% CI 0.72, 0.92). There were no false positives with (LVA); however, 20 fractures on radiographs could not be visualised on LVA. Mohammed reported the prevalence of VF amongst a cohort of RA patients with using LVA imaging, as noted above [22]. Forty-one percent of this cohort had T-scores less than or equal to − 2.5. Twenty-seven percent of subjects had two or more fractures, and the majority were located in the lumbar spine (68%). Fracture severity was mild (grade 1) in 31%, moderate (grade 2) in 55% and severe (grade 3) in 14%.
Osteoporosis medication prescribing and adherence
Data from the National Primary Care Reimbursement Services (PCRS) scheme show prescribing of pharmacological therapy for osteoporosis increased significantly between 2001 and 2011, in particular following hospitalisation for osteoporotic fracture [2, 24]. The proportion of Irish adults who were on treatment has increased prior to fracture (3 to 11%) while post-hospitalisation for fracture, it has increased from 11 to 47% [25]. In this study, less than 5% of patients had VF, and prescription of medication did not differ between fracture types. However, a treatment gap still exists, estimated to be between 20 and 26% for those at high fracture risk [2]. Adherence rates to osteoporosis medication are less than 50% at 1 year [24].
Surgical management of osteoporotic vertebral fractures
Four case series studies addressing surgical interventions, i.e. kyphoplasty [26, 27] and vertebroplasty [28, 29], for VF were identified. They included patients with VF secondary to osteoporosis and other causes, e.g. malignancy and trauma. The kyphoplasty studies solely examined the impact of patient positioning on restoring vertebral height by showing a significant improvement in mean anterior vertebral height differences and Cobb angle. The vertebroplasty studies examined the impact of the procedure on pain levels and mobility showing a significant reduction of pain, a cessation or reduction of opioid use [29] and improved self-reported mobility outcomes following vertebroplasty [28]. Details were limited, the sample sizes were small (range 8–149) and no control groups were included.
Economic evaluation of the osteoporotic burden
Multiple country-specific reports on the economic burden of osteoporosis were published by the International Osteoporosis Foundation in 2013 [2]. The report on Ireland described the clinical and economic burden of osteoporosis in 2010 by incorporating available data on fracture incidence and associated costs into a model in conjunction with the European Federation of Pharmaceutical Industry Associations. The investigators defined the population at risk as being those aged 50 years or older who met the World Health Organization diagnostic criteria (T-score less than − 2.5) for osteoporosis equating to 170,000 individuals during 2010. They estimated 18,000 incident fractures occurred in Ireland during this period, including 2700 VF (15%), accounting for an expenditure of €223 million and 6100 in lost quality-adjusted life years (QALYs). When osteoporosis expenditure was combined with the value for QALY lost (2 × gross domestic product), osteoporosis costs totalled to €650 million in Ireland in 2010. Direct “first-year costs” following fracture amounted to €125 million, subsequent-year costs amounted to €62 million and preventative osteoporosis treatment costs equated to €35 million. Interestingly, expenditure on osteoporosis pharmacotherapy treatment only amounted to 15.8% of the overall total costs. Hip fractures were the most expensive fragility fractures (€105 million), followed by “other” fractures (€72 million), spine (€8 million) and forearm fractures (€3 million) [2].
Data from Irish Public Hospitals has shown that there is an average of 478 VF hospital admissions per year, equating to 3674 bed days based on data from 2000 to 2014. However, there has been over a 150% increase in the number of women hospitalised with VF in 2014 compared with 2000 and a 20% increase in male admissions. The mean duration of hospital admission for VF has increased from 12 days for women and 11 days for men to 17 and 19 days respectively over this time period. Assuming the mean cost for VF admissions from 2003 to 2008, then the mean cost in 2014 was €2.1 million for men and €3.5 million for women accounting for longer admission durations. Overall, we know that hospitalisations for fragility fractures are on the rise. By 2046, expenditure is projected to increase to €304 million compared with €118 million in 2014 and 58% of the affected patients are anticipated to be 80 years or older [5, 30].
Other studies
Two studies from the Department of Mechanical and Biomedical Engineering at NUI Galway examined vertebral trabecular bone loss using simulation models [31, 32]. McDonnell et al. show vertebral trabecular bone is at greater risk of loss from wedge action loading (combination of compression and flexure loading) compared with uni-axial compression loading [31], and horizontal trabeculae may be at greatest risk of damage from strain adaptive resorption [32].
Discussion
This is the first systematic review that examined the literature on osteoporotic spine fractures in Ireland. Overall, they appear to be increasing in incidence and cost but it is probable that many remain undiagnosed and are not being captured and their importance is under-recognised. We found that there is a lack of studies addressing this area and the available data is heterogeneous which limits the inferences that can be made. More formal studies are needed to better understand the incidence, prevalence, effect on patients and their long-term outcome and cost to patients and society. The deficit in data reflects the current situation of osteoporotic spine care in Ireland where streamlined multi-disciplinary care for investigation and management of VF or a national database does not exist. This is in contrast to hip fractures despite spine accounting for a higher proportion of total fragility fractures and their near-equal significance [11, 33]. The National Hip Fracture Care Pathway introduced by the Health Service Executive (HSE) in tandem with the establishment of the Irish Hip Fracture Database (IHFD) has significantly improved patient care for thousands of individuals admitted with hip fractures in Ireland per year [34]. A similar care pathway is greatly needed for vertebral fractures to highlight their significance and to address the confusion that often arises around investigations, management and service access.
We had a clear objective prior to conducting this systematic review and used appropriate pre-defined inclusion and exclusion criteria with a reproducible protocol. We searched multiple different electronic databases and reference lists of relevant articles in order to identify studies that would be potentially eligible for inclusion, but it is possible we did not identify all eligible studies. Due to the limited number of studies that met our inclusion criteria and their heterogeneity, we were unable to perform a meta-analysis and a robust quantitative analysis.
We found a wide range of vertebral fracture prevalence in Ireland, from less than 5% amongst hospitalised populations to almost 90% in older patients with low BMD in whom a fracture was suspected. VF tend to be under-recognised compared with other fragility fractures for several reasons. Firstly, many are asymptomatic and studies suggest only one in three present clinically [11]. However, others have shown even “radiographic” fractures are associated with morbidity, are important for predicting future fracture and are associated with mortality which exceeds hip fracture [6,7,8, 35]. Multi-national studies show the majority do not occur following a fall, unlike non-vertebral fractures [36]. Patients presenting with suggestive symptoms are sometimes dismissed and not imaged, or may delay or not seek medical attention. Fractures often go unreported on imaging preformed for other reasons, possibly due to inattentional blindness [37]. When fractures are recognised, reports may contain ambiguous terminology such as “wedging”, “loss of height” and “end-plate depression”, and consequently, the referring clinician may not realise there is an actual fracture. Finally, the only large sample data for Ireland contains data reported from public hospital admissions. This data is a conservative estimate for two main reasons: (a) only 59% of recorded emergency admissions have a discharge diagnosis and our own audits show that under-reporting is a significant problem and (b) this data does not include patients seen and managed in other facilities or in outpatient clinics [38].
Despite the limited availability of data, we found evidence that the overall number of VF may be increasing and is particularly high in some populations and the numbers are greater when imaging is formally scrutinised for fractures using agreed criteria. The evidence suggests that VF are more common in older Irish adults, those with low BMD or those with co-morbidities such as rheumatoid arthritis. There appears to be a trend for greater prescription use amongst people deemed high risk for fracture or following hospitalisation for fragility fracture. However, there is very limited data on medication adherence and compliance. In addition, we do not have clear evidence of the true rates of osteoporosis diagnosis and treatment rates specifically following VF. We did not find observational studies specifically addressing the incidence of VF, patients’ pre-morbid status, mortality or long-term outcomes including patient perceptions and quality of life. There is limited data addressing the overall economic cost for Irish people with VF but the estimates are concerning and are probably a significant underestimation. While we know the overall osteoporosis poses a high economic burden in this jurisdiction, we have not been able to fully address the true impact and importance of VF in this study.
Conclusion
In summary, there is a large deficit of large studies addressing the epidemiology of osteoporotic fractures in Ireland, in particular vertebral. Several studies show that VF are common when addressed systematically and the prevalence may be rising. Published studies are heterogeneous making inferences difficult. This deficit must be rectified to improve our understanding of the burden of VF in Ireland and enable more effective service planning for fracture prevention and management.
References
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. https://doi.org/10.1007/s11657-013-0136-1
the EU review panel of the IOF, Svedbom A, Hernlund E et al (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8. https://doi.org/10.1007/s11657-013-0137-0
Freedman KB, Kaplan FS, Bilker WB et al (2000) Treatment of osteoporosis: are physicians missing an opportunity? J Bone Joint Surg Am 82-A:1063–1070
International Osteoporosis Foundation (2017) IOF Compendium of Osteoporosis
Kelly MA, McGowan B, McKenna MJ et al (2018) Emerging trends in hospitalisation for fragility fractures in Ireland. Ir J Med Sci 187(1971):601–608. https://doi.org/10.1007/s11845-018-1743-z
Nevitt MC (2000) Effect of alendronate on limited-activity days and bed-disability days caused by Back pain in postmenopausal women with existing vertebral fractures. Arch Intern Med 160:77–85. https://doi.org/10.1001/archinte.160.1.77
Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D (2000) Risk of mortality following clinical fractures. Osteoporos Int 11:556–561. https://doi.org/10.1007/s001980070075
Lau E, Ong K, Kurtz S et al (2008) Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am 90:1479–1486. https://doi.org/10.2106/JBJS.G.00675
Al-Sari UA, Tobias J, Clark E (2016) Health-related quality of life in older people with osteoporotic vertebral fractures: a systematic review and meta-analysis. Osteoporos Int 27:2891–2900. https://doi.org/10.1007/s00198-016-3648-x
Cosman F, Krege JH, Looker AC, Schousboe JT, Fan B, Sarafrazi Isfahani N, Shepherd JA, Krohn KD, Steiger P, Wilson KE, Genant HK (2017) Spine fracture prevalence in a nationally representative sample of US women and men aged ≥40 years: results from the National Health and Nutrition Examination Survey (NHANES) 2013-2014. Osteoporos Int 28:1857–1866. https://doi.org/10.1007/s00198-017-3948-9
Schousboe JT (2016) Epidemiology of vertebral fractures. J Clin Densitom 19:8–22. https://doi.org/10.1016/j.jocd.2015.08.004
Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G (2017) Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 28:1531–1542. https://doi.org/10.1007/s00198-017-3909-3
Fink HA, Litwack-Harrison S, Ensrud KE, Shen J, Schousboe JT, Cawthon PM, Cauley JA, Lane NE, Taylor BC, Barrett-Connor E, Kado DM, Cummings SR, Marshall LM, Osteoporotic Fractures in Men (MrOS) Study Group (2017) Association of Incident, clinically undiagnosed radiographic vertebral fractures with follow-up Back pain symptoms in older men: the Osteoporotic Fractures in Men (MrOS) Study: association of undiagnosed VF with follow-up back pain in older MEN. J Bone Miner Res 32:2263–2268. https://doi.org/10.1002/jbmr.3215
Kendler DL, Marin F, Zerbini CAF, Russo LA, Greenspan SL, Zikan V, Bagur A, Malouf-Sierra J, Lakatos P, Fahrleitner-Pammer A, Lespessailles E, Minisola S, Body JJ, Geusens P, Möricke R, López-Romero P (2018) Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 391:230–240. https://doi.org/10.1016/S0140-6736(17)32137-2
Singer A, Exuzides A, Spangler L et al (2015) Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc 90:53–62. https://doi.org/10.1016/j.mayocp.2014.09.011
Armstrong C, Heaney F, Kearns SR, Curtin W, McCabe JP, Murphy CG, Delaney MF, Carey JJ (2017) A nurse-led fracture liaison service has potential to maximise the diagnosis and treatment of osteoporosis: results of the hoof project. Osteoporos Int 28:S489. https://doi.org/10.1007/s00198-017-3950-2
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269 W64
McGowan B, Bennett K, Marry J, Walsh JB, Casey MC (2012) Patient profile in a bone health and osteoporosis prevention service in Ireland. Ir J Med Sci 181:511–515. https://doi.org/10.1007/s11845-012-0806-9
Ahmed M, Durcan L, O’Beirne J et al (2012) Fracture liaison service in a non-regional orthopaedic clinic--a cost-effective service. Ir Med J 105(24):26–27
Wright S, Beringer T, Taggart H, Keegan D, Kelly J, Whithead E, McKane R, McNally C, McQuilken M, Finch M (2006) A study of male patients with forearm fracture in Northern Ireland. Clin Rheumatol 26:191–195. https://doi.org/10.1007/s10067-006-0261-y
Beringer T, Heyburn G, Finch M et al (2006) Prevalence of vitamin D inadequacy in Belfast following fragility fracture. Curr Med Res Opin 22:101–105. https://doi.org/10.1185/030079906X80332
Mohammad A, Lohan D, Bergin D, Mooney S, Newell J, O’Donnell M, Coughlan RJ, Carey JJ (2014) The prevalence of vertebral fracture on vertebral fracture assessment imaging in a large cohort of patients with rheumatoid arthritis. Rheumatology 53:821–827. https://doi.org/10.1093/rheumatology/ket353
McGuinness B, Stewart S, Taggart H (2009) How useful is dual energy lateral vertebral assessment in a clinic setting? Ulster Med J 78:34–36
McGowan B, Bennett K, Casey MC, Doherty J, Silke C, Whelan B (2013) Comparison of prescribing and adherence patterns of anti-osteoporotic medications post-admission for fragility type fracture in an urban teaching hospital and a rural teaching hospital in Ireland between 2005 and 2008. Ir J Med Sci 182:601–608. https://doi.org/10.1007/s11845-013-0935-9
McGowan BM, Bennett K, Marry J et al (2011) Primary-care prescribing of anti-osteoporotic-type medications following hospitalisation for fractures. Eur J Clin Pharmacol 67:301–308. https://doi.org/10.1007/s00228-010-0942-y
Cawley DT, Sexton P, Murphy T, McCabe JP (2011) Optimal patient positioning for ligamentotaxis during balloon kyphoplasty of the thoracolumbar and lumbar spine. J Clin Neurosci 18:834–836. https://doi.org/10.1016/j.jocn.2010.10.009
Ng JP, Cawley DT, Beecher SM, Baker JF, McCabe J (2016) The reverse Thomas position for thoracolumbar fracture height restoration: relative contribution of patient positioning in percutaneous balloon kyphoplasty for acute vertebral compressions. Int J Spine Surg 10:21. https://doi.org/10.14444/3021
O’Brien J, Brennan D, Taylor D et al (2006) Percutaneous vertebroplasty--initial clinical experience in osteoporotic and myelomatous compression fractures. Ir J Med Sci 175:50–53
Kevane B, Ryder DQ, Gilligan O (2009) Percutaneous vertebroplasty in osteoporosis, myeloma and Langerhans’ cell histiocytosis. Ir Med J 102:212–215
McGowan B, Casey MC, Silke C, Whelan B, Bennett K (2013) Hospitalisations for fracture and associated costs between 2000 and 2009 in Ireland: a trend analysis. Osteoporos Int 24:849–857. https://doi.org/10.1007/s00198-012-2032-8
McDonnell P, Harrison N, McHugh PE (2010) Investigation of the failure behaviour of vertebral trabecular architectures under uni-axial compression and wedge action loading conditions. Med Eng Phys 32:569–576. https://doi.org/10.1016/j.medengphy.2010.02.005
Mc Donnell P, Harrison N, Liebschner MAK, Mc Hugh PE (2009) Simulation of vertebral trabecular bone loss using voxel finite element analysis. J Biomech 42:2789–2796. https://doi.org/10.1016/j.jbiomech.2009.07.038
Weycker D, Li X, Barron R, Bornheimer R, Chandler D (2016) Hospitalizations for osteoporosis-related fractures: economic costs and clinical outcomes. Bone Rep 5:186–191. https://doi.org/10.1016/j.bonr.2016.07.005
National Office of Clinical Audit (2018) Irish Hip Fracture Database National Report 2017
Lindsay R, Silverman SL, Cooper C et al (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323
Costa AG, Wyman A, Siris ES, Watts NB, Silverman S, Saag KG, Roux C, Rossini M, Pfeilschifter J, Nieves JW, Netelenbos JC, March L, LaCroix A, Hooven FH, Greenspan SL, Gehlbach SH, Díez-Pérez A, Cooper C, Compston JE, Chapurlat RD, Boonen S, Anderson FA Jr, Adachi JD, Adami S (2013) When, where and how osteoporosis-associated fractures occur: an analysis from the Global Longitudinal Study of Osteoporosis in Women (GLOW). PLoS One 8:e83306. https://doi.org/10.1371/journal.pone.0083306
Gehlbach SH, Bigelow C, Heimisdottir M et al (2000) Recognition of vertebral fracture in a clinical setting. Osteoporos Int 11:577–582. https://doi.org/10.1007/s001980070078
Healthcare Pricing Office, Health Service Executive (2017) Activity in acute public hospitals in Ireland. Annu Rep 2016. http://www.hpo.ie/latest_hipe_nprs_reports/HIPE_2017/HIPE_Report_2017.pdf
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
JJC has received speaker fees from Eli Lilly, Amgen, UCB, Pfizer, Hospira and Celltrion. He has received travel support from Roche, Amgen, Eli Lilly, MSD and UCB and grant and educational support from Amgen, UCB, Eli Lilly, Abbvie, MSD and the Irish Society for Rheumatology. He has served on several committees for and is past-President of the International Society for Clinical Densitometry, is a member of the Committee for Scientific affairs for the International Osteoporosis Foundation and is a founding member of and current president of the Irish DXA Society. EMC, AI, RS, MK, CA, FH and DB, JPMC declare that they have no conflict of interest to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McCabe, E., Ibrahim, A., Singh, R. et al. A systematic review of the Irish osteoporotic vertebral fracture literature. Arch Osteoporos 15, 34 (2020). https://doi.org/10.1007/s11657-020-0704-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-020-0704-0