Abstract
Summary
Spine fracture prevalence is similar in men and women, increasing from <5 % in those <60 to 11 % in those 70–79 and 18 % in those ≥80 years. Prevalence was higher with age, lower bone mineral density (BMD), and in those meeting criteria for spine imaging. Most subjects with spine fractures were unaware of them.
Introduction
Spine fractures have substantial medical significance but are seldom recognized. This study collected contemporary nationally representative spine fracture prevalence data.
Methods
Cross-sectional analysis of 3330 US adults aged ≥40 years participating in NHANES 2013–2014 with evaluable Vertebral Fracture Assessment (VFA). VFA was graded by semiquantitative measurement. BMD and an osteoporosis questionnaire were collected.
Results
Overall spine fracture prevalence was 5.4 % and similar in men and women. Prevalence increased with age from <5 % in those <60 to 11 % in those 70–79 and 18 % in those ≥80 years. Fractures were more common in non-Hispanic whites and in people with lower body mass index and BMD. Among subjects with spine fracture, 26 % met BMD criteria for osteoporosis. Prevalence was higher in subjects who met National Osteoporosis Foundation (NOF) criteria for spine imaging (14 vs 4.7 %, P < 0.001). Only 8 % of people with a spine fracture diagnosed by VFA had a self-reported fracture, and among those who self-reported a spine fracture, only 21 % were diagnosed with fracture by VFA.
Conclusion
Spine fracture prevalence is similar in women and men and increases with age and lower BMD, although most subjects with spine fracture do not meet BMD criteria for osteoporosis. Since most (>90 %) individuals were unaware of their spine fractures, lateral spine imaging is needed to identify these women and men. Spine fracture prevalence was threefold higher in individuals meeting NOF criteria for spine imaging (∼1 in 7 undergoing VFA). Identifying spine fractures as part of comprehensive risk assessment may improve clinical decision making.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Approximately two million Americans suffered an osteoporosis-related fracture in 2005, and this incidence is projected to increase to more than three million by 2025 [1]. Health care professionals frequently fail to diagnose and treat osteoporosis even after major fractures [2].
The presence of osteoporotic fractures indicates that the skeleton has deteriorated and is unable to sustain day-to-day loads. Clinical and morphometric spine fractures are associated with increased mortality [3], chronic pain, and impaired quality of life [4, 5]. Spine fractures are often the first osteoporotic fractures [6] and are associated with substantially elevated risk for subsequent vertebral [7] and nonvertebral fractures including those of the hip [8]. Accordingly, recognition of these fractures as sentinel events may trigger assessments and interventions that potentially could prevent additional fractures [9–12]. However, spine fractures often do not come to clinical attention at the time of the event and so patients with spine fractures are usually not identified. As a result, criteria for proactive spine imaging with radiography or VFA have recently been recommended by the National Osteoporosis Foundation (NOF). Although these criteria were intended to identify individuals with increased spine fracture prevalence, the prevalence in individuals meeting these criteria is unknown [10].
In the USA, five previous studies have provided prevalence data on spine fractures by lateral spine radiography. These studies were not nationally representative, did not include both men and women or a broad age range, or did not comprehensively discriminate fractures from nonfracture deformities [13–17]. Over a decade ago, the Surgeon General’s Report on Bone Health and Osteoporosis highlighted the need for national-level data on spine fracture prevalence obtained through VFA [9]. Compared to lateral lumbar and thoracic spine radiographs, VFA includes a single image of the spine, has reduced resolution and higher noise, but less projection distortion (parallax) and lower radiation exposure, with nearly comparable accuracy in identifying vertebral fractures [18–25].
The National Health and Nutrition Examination Survey (NHANES) has provided information regarding BMD of US citizens, and the NHANES III database is the reference database for hip BMD [26]. The goals of this study were to define the prevalence of spine fractures in men and women aged ≥40 years using VFA data collected in NHANES 2013–2014, to assess characteristics of subjects with spine fractures, to compare self-report of spine fracture with VFA diagnosis, and to assess prevalence in those meeting NOF spine imaging criteria based on age, BMD, and previous fracture [10].
Methods
Study design and sample
The NHANES is conducted by the National Center for Health Statistics (NCHS) to assess the health and nutritional status of a representative sample of the noninstitutionalized, civilian US population. Details about the plan, operation, and design of the survey are described elsewhere [27]. NHANES participants underwent a home interview followed by assessments at a mobile examination center. All procedures in NHANES 2013–2014 were approved by the NCHS Research Ethics Review Board; written informed consent was obtained from subjects.
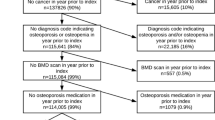
The percentage of subjects aged ≥40 years who came to the mobile examination center relative to the number selected to participate was 61.2 %. Of 3708 adults, 378 (10 %) did not undergo VFA due to pregnancy, body weight > 450 lb (204 kg), history of radiographic contrast material exposure in the past week, or presence of Harrington rod in the spine, or had scans excluded because of movement artifacts. The VFA sample included 3330 subjects.
Assessments
VFA using lateral spine imaging IVA™ mode and BMD of posterior–anterior lumbar spine (LS) and proximal femur with Hologic Discovery® A densitometers (Hologic Inc., Marlborough, MA) were performed in the supine position. BMD was analyzed using APEX™ Version 4.0. Images of T4–L4 were viewed and results were stored using Optasia Medical SpineAnalyzer™ 4.0 software (Cheadle Hulme, UK). Each vertebra was graded using a semiquantitative method [28] by a physician trained by the expert musculoskeletal radiologist (Genant) at the NHANES DXA quality control center at the University of California, San Francisco (UCSF) as normal or mild, moderate, or severe fracture. Spine images of “fracture” cases identified by the UCSF reader were reread by Dr. Genant to confirm the findings; this rereading was limited to putative fracture cases because discrimination of fracture from nonfracture deformity is challenging, whereas discriminating deformity from non-deformity is relatively easy. Of 274 participants initially identified to have a “fracture,” 88 (32 %) were not confirmed; these were mostly mild wedge deformities, without evident endplate or cortical wall displacement, thought to represent deformity related to chronic mechanical loading or degenerative remodeling. As described by Genant et al. in 1993 [28], the readings included inspection for vertebral body height loss and morphology out of step with adjacent vertebrae and for buckling or bowing of the endplates and/or anterior cortical walls. Also, deformities related to degenerative change identified by intact and sometimes sclerotic endplates with accompanying adjacent disc space narrowing were not diagnosed as fractures, and deformities such as Scheuermann’s disease or congenital vertebral fusion were also not diagnosed as fractures [28]. Subject status was defined as “normal” if no fracture was observed and at least 9 of 10 vertebral bodies from T7–L4 were evaluable; T4–T6 were not required to be evaluable since they are not always well visualized and only a small proportion of vertebral fractures occur at these levels [19]. Status was considered “fractured” if a fracture was observed in T4–L4, regardless if there were unevaluable levels elsewhere. Status was “uninterpretable” for participants not meeting above criteria.
Procedures for assessment of BMD of the lumbar spine (LSBMD), total hip (TOTBMD), and femoral neck (FNBMD) have been described elsewhere [29, 30]. LSBMD was calculated as the average of individual lumbar vertebra in subjects with at least two valid vertebrae between L1 and L4 [31]. T-scores were calculated per the 2013 recommendations from the International Society for Clinical Densitometry [31].
Self-reported race/ethnicity and previous fracture history were assessed by questionnaire. Prior low trauma fractures were defined as self-reported fractures that occurred at age ≥50 years due to a fall from standing height or less, a trip/slip, or a fall out of bed (hip, wrist, spine) or at age ≥20 years and not due to severe trauma such as a car accident, hard fall down steps, or from a ladder (fractures other than hip, wrist, spine).
The prevalence of spine fractures in men and women aged ≥50 years was compared in those meeting vs not meeting the following NOF criteria for spine imaging [10]: (a) women aged 65–69 and men aged 70–79 years whose FNBMD, TOTBMD, or LSBMD T-score was ≤ −1.5; (b) women aged ≥70 and men aged ≥80 years whose FNBMD, TOTBMD, or LSBMD T-score was ≤ −1.0; and (c) men and women who reported a prior low trauma fracture that occurred after age ≥50 years. Data on additional conditions that define eligibility for spine imaging, such as glucocorticoid use and historical height loss, were not yet publicly released.
Statistical analyses
Analyses were conducted with PC-SAS (Version 9.3, SAS Institute, Cary, NC) and SUDAAN (Version 11.0.1, Research Triangle Institute, Cary, NC). All analyses used the examination sample weights and accounted for the complex survey design when performing statistical tests. Statistical tests were t tests or chi-square analyses for unadjusted results. For age-adjusted results, age was included as an independent variable in a regression model, and means or proportions for the variable of interest were calculated by group after setting the value for age equal to the average age of the sample being modeled (57 years in the present study).
Because 10 % of the examined sample were not included in the final VFA sample, nonresponse bias analyses were conducted. Excluded respondents were more likely to be older, female, nonwhite, have higher BMI, report their health as fair or poor, and report more sedentary time than respondents in the analytic sample. To examine for potential nonresponse bias, the publicly released examination sample weights were adjusted for item nonresponse by age, sex, and race/Hispanic origin using the PROC WTADJUST procedure in SUDAAN. The sample weights adjusted for nonresponse for these three characteristics resulted in conclusions similar to those when the publicly released sample weights were used.
Results
The VFA sample included 1602 males and 1728 females. The weighted demographic characteristics of the VFA sample reflect those of the noninstitutionalized US population aged ≥40, and mean age was 57 years. Specifically, the race/ethnic composition after applying the sample weights was 71 % non-Hispanic white, 11 % Hispanic, 10 % non-Hispanic black, 5 % non-Hispanic Asian, and 2 % other race. Mean BMI was 29 kg/m2 and mean BMD values were within the normal range (T-score > −1) at FNBMD, TOTBMD, or LSBMD in both genders.
Overall, 5.4 % of US adults aged ≥40 had spine fractures, including 6.2 % of males and 4.6 % of females (Table 1). There was a significant increase in the prevalence of spine fractures by age in both genders (P = 0.03 for all). The prevalence increased from 3–5 % in men and women <60 years old to 16–21 % in those aged ≥80 years. Overall, the prevalence of mild fractures was 2.3 % and of moderate/severe fractures was 3.3 %. The prevalence of moderate/severe fractures was 1.9 % in those aged <65 years and 14.5 % among those ≥80, with similar age-related increases in men and women (Table 2). Among fracture cases, the proportion with moderate/ severe fracture was higher in those aged ≥65 years (66 %; 95 % CI 55–76 %) than in those <65 (51 %; 95 % CI 35–67 %) (P = 0.03; data not shown).
Gender distribution for normal vs fractured adults was similar. Adults with fracture were older, more likely to be non-Hispanic white, had lower BMI and BMD at all sites, and a higher proportion met BMD criteria for osteoporosis (T-score ≤ −2.5) at the LS or FN (26.4 vs 9.9 %) (Table 3). In those ≥65 years old with vertebral fracture, 38 % had osteoporosis in at least one site compared to 14 % of those without fracture, and 22 % had normal BMD at both sites compared to 35 % of the nonfracture population.
Spine status showed fracture in 1 % by both VFA and self-report, 2 % by self-report with normal VFA, and 5 % by VFA diagnosis with no fracture self-report. Only 8 % of those with a VFA diagnosis were aware of their fracture. Furthermore, only 21 % of those who self-reported fracture had a proven VFA diagnosis (Table 4).
Common locations for fractures in both genders were the mid-thoracic region and thoracolumbar junction. Fracture frequency appeared to be similar in men and women at most levels, but fractures appeared to be more common in men at some levels, including T11 and T12 (Fig. 1).
Distribution of fractures at individual vertebra by sex, NHANES 2013–2014 VFA fracture sample (n = 186). The distribution of fractures at each level from T4 through L4 is shown for the 186 subjects found to have one or more vertebral fractures. Results are presented as frequency of fracture at each vertebral level. Note the precision of this information may be low at some levels, and these data are provided to illustrate distribution rather than exact prevalence at each level. As an additional caveat, visualization of T4–T6 was inadequate in some subjects, although only a small proportion of vertebral fractures occur at these levels [19]
The prevalence of spine fracture was higher in subjects meeting NOF criteria for spine imaging overall (14.0 vs 4.7 % in adults not meeting criteria, P < 0.001) and considering men (20.1 vs 5.6 %, P = 0.003) and women (12.4 vs 3.6 %, P < 0.001) separately (Table 5).
Discussion
These data from NHANES 2013–2014 provide the first nationally representative estimates of spine fracture prevalence in US men and women aged ≥40 years. VFA-diagnosed spine fracture prevalence was very low in subjects 40–49 but increased to 11 % in those aged 70–79 and 18 % in those aged ≥80 years. Among fracture cases, a higher proportion of individuals ≥65 years old vs younger adults had fractures of at least moderate severity. Prevalence was similar in men and women. Beyond the association with age, those with vertebral fractures had lower BMI and BMD. Among participants aged ≥65 years with vertebral fractures, the proportion with osteoporosis by BMD criteria was 38 % and the proportion with normal BMD (T-score > −1.0 at both skeletal sites) was 22 %. The Study of Osteoporotic Fractures (SOF) study showed that 58 % of hip fracture patients had osteoporosis at the LS or FN [32]. Thus, among older people with spine or hip fractures, roughly 40–60 % of subjects meet BMD criteria for osteoporosis.
Five previous studies of spine fracture prevalence in the US, all based on lateral spine radiography, have been published [13–17]. The first included women ≥50 years old in Rochester, MN [13]. Prevalence of deformity by quantitative morphometry (QM), a method that does not discriminate fracture from nonfracture deformity, increased from 7.6 % among women aged 50–54 to 45.5 % in women 80–84. The second study included 899 women and 529 men ≥50 years old in Saunders County, NE and also assessed deformity by QM [14]. Prevalence of spine deformity increased with age, from 10 % of women in their 50s to 45 % of women in their 80s and from 29 % of men in their 50s to 39 % of men in their 80s. The SOF included 9575 Caucasian women aged ≥65 years from four metropolitan areas, again using QM, reported prevalence of vertebral deformities to be 20 %, without prevalence reported by age [15]. By a visual semiquantitative methodology, the prevalence of deformity in 704 women and men in the Framingham Study with mean age 53–54 years was 14 % with no effect of age or sex on prevalence, although the authors suggested that some deformities may have been a result of remote trauma, stress, sports, physical activity, or degenerative remodeling, rather than osteoporosis [16]. Finally, in the MrOS Study, prevalence in 5958 men aged ≥65 years from six locations in the US was 12 % by semiquantitative methodology (mildly deformed vertebrae had to have endplate depression or cortical buckling to be considered fractured) [17]. In studies from Canada, Japan, and Europe, spine fracture prevalence rates varied from 4 to 25 %, based on the population age, gender distribution, geography, ascertainment technique, and other factors [7, 8, 33–38].
The methodology for the evaluation of the VFA images was the rigorous semiquantitative method as described by Genant [28]. While this methodology is sometimes mis-applied to include only an assessment of approximate height and shape, the method described by Genant et al. includes evaluation of qualitative features including endplate deformity, buckling of cortices, lack of parallelism of endplates, and loss of vertical continuity of vertebral shape to define fracture and assessment for presence of characteristic nonfracture deformities to rule out fracture [28]. Training slide decks on this methodology are available from the International Osteoporosis Foundation website https://www.iofbonehealth.org/what-we-do/training-and-education/educational-slide-kits/vertebral-fracture-teaching-program. The lower prevalence of spine fractures in this contemporary study may be due to the rigorous methodology for defining fractures, since in most prevalence studies in the USA, visual assessments for degenerative change or nonfracture deformities were conducted incompletely or not at all [13–16]. In some European studies that included a stricter definition of spine fractures, prevalence was more similar to that seen here [8, 37, 39]. Another system for defining spine fracture prevalence called the Algorithm-Based Qualitative (ABQ) method defines spine fracture by presence of endplate depression without consideration of vertebral height reduction with a detailed algorithm for identifying nonfracture deformity [40]. Depending on how the SQ vs ABQ method is implemented by individual readers and investigators, these methods are likely to show different prevalences [22, 41]. In addition to the reading methodology, it is possible that spine fracture prevalence may have declined, similar to the decline in hip fracture since the 1990s [42–44].
We endeavored to rigorously differentiate fractures from nonfracture deformities such as stress and degenerative remodeling. These latter deformities often occur at T7–T8 and T12–L1 where flexion compression force may be maximal and suggest a chronic or intermittent stress-related phenomenon, rather than an acute fracture [45]. Multiple negative consequences have been associated with spine fractures defined by a variety of methodologies, usually by criteria less strict than those in this study [3, 4, 7, 8, 15, 46]. The clinical and prognostic significance of spine fractures by our strict criteria might be even more important. Further studies of the consequences of nonfracture vertebral deformities are warranted.
Over 90 % of subjects with a positive VFA diagnosis did not self-report a fracture, and most subjects who self-reported a fracture did not have a VFA diagnosis. Similarly, in another study, 93 % of subjects with radiographic spine fractures were unaware of the fracture [47]. Vertebral fractures are associated with an increased risk (2–5-fold) for subsequent vertebral and other fractures [46]; indeed, a high proportion (perhaps up to 50 %) of patients with hip fracture have vertebral fractures found on routine spine imaging [48]. The identification of spine fractures as sentinel events could potentially reduce the risk of having subsequent hip or other fracture [9, 10, 12, 49].
The prevalence of vertebral fracture was 14.0 % (one in seven individuals) in individuals meeting NOF criteria for screening spine imaging based on age and BMD or on previous fragility fracture [10], compared to 4.7 % in those not meeting criteria. Thus, the NOF criteria indeed identified subjects with approximately threefold increased prevalence of vertebral fracture. At the time of these analyses, some data from NHANES 2013–2014, such as glucocorticoid use and historical height loss, were not yet publicly available. When this information is available, future analyses may help to refine the NOF screening criteria.
In those aged <50 years, very few of the females but approximately 3.5 % of the males had spine fractures. The cause of fractures in younger males is unknown, although athletic and work-related trauma or repetitive stresses are possible etiologies [34]. Also, some of these subjects may have had glucocorticoid exposure during young adulthood, as glucocorticoids are known to contribute risk for fracture independently of BMD [50]. Future analyses including glucocorticoid use will help address at least one of these possibilities.
This is the first study to assess the prevalence of spine fractures in a nationally representative sample. The study included men and nonwhite groups and a wide range of ages. The study used VFA and strict criteria were utilized for diagnosis. The agreement between VFA performed with a Hologic Discovery A in the supine lateral position, as used in this study, and radiographs has been independently evaluated by two studies including a total of 679 older men and women. The studies found very good agreement with kappas of 0.73 and 0.84 [19, 51]. A large volume of additional data, including multisite BMD assessment and fracture history, were collected. A possible limitation is potential nonresponse bias in the estimates, although results from analyses re-weighted to address nonresponse by age, sex, and race/ethnicity were similar to those obtained when the publicly released sample weights were used, suggesting that nonresponse bias associated with these particular demographic variables is unlikely. Another limitation is lower statistical reliability of some of the estimates as evidenced by wide CI. Finally, institutionalized persons, a group with a high prevalence of osteoporosis [52], were not included.
In conclusion, this study establishes the prevalence of spine fracture by VFA using a rigorous definition of fracture in a nationally representative sample of men and women. The prevalence was lower than in previous US studies which defined fractures less rigorously, suggesting that visual assessment is necessary to evaluate for nonfracture deformities. Spine fracture prevalence was higher with increasing age, lower BMD, or previous fracture. Even so, most subjects with spine fracture did not meet BMD criteria for osteoporosis. Few US citizens (less than 10 %) with documented vertebral fracture were aware of their fracture and those reporting a history of spine fracture usually did not have one. The prevalence of vertebral fracture was threefold higher in individuals who met NOF screening criteria [10] based on age and BMD or on previous fracture; the findings correspond to approximately one fracture case out of every seven subjects meeting screening criteria. Identifying individuals with prevalent vertebral fractures as part of a comprehensive risk assessment may improve clinical decision making.
References
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 22:465–475
Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, Krohn KD (2014) Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res 29:1929–1937
Ensrud KE, Thompson DE, Cauley JA et al (2000) Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. J Am Geriatr Soc 48:241–249
Lips P, Cooper C, Agnusdei D, et al. for the Working Party for Quality of Life of the European Foundation for Osteoporosis et al (1999) Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Osteoporos Int 10:150–160
Nevitt MC, Ettinger B, Black DM, Stone K, Jamal SA, Ensrud K, Segal M, Genant HK, Cummings SR (1998) The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 128:793–800
Sontag A, Krege JH (2010) First fractures among postmenopausal women with osteoporosis. J Bone Miner Metab 28:485–488
Ferrar L, Roux C, Felsenberg D, Glüer CC, Eastell R (2012) Association between incident and baseline vertebral fractures in European women: vertebral fracture assessment in the Osteoporosis and Ultrasound Study (OPUS). Osteoporos Int 23:59–65
McCloskey EV, Vasireddy S, Threlkeld J et al (2008) Vertebral fracture assessment (VFA) with a densitometer predicts future fractures in elderly women unselected for osteoporosis. J Bone Miner Res 23:1561–1568
US Department of Health and Human Services (2004) Bone health and osteoporosis: a report of the surgeon general. US Department of Health and Human Services, Public Health Service, Office of the Surgeon General, Rockville, MD
Cosman F, deBeur SJ, LeBoff MS, et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381
Watts NB, Bilezikian JP, Camacho PM et al (2010) American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of postmenopausal osteoporosis. Endocr Pract 16(suppl 3):1–37
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster J-Y, On behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF) (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Melton LJ III, Lane AW, Cooper C, Eastell R, O’Fallon WM, Riggs BL (1993) Prevalence and incidence of vertebral deformities. Osteoporos Int 3:113–119
Davies KM, Stegman MR, Heaney RP, Recker RR (1996) Prevalence and severity of vertebral fracture: the Saunders County Bone Quality Study. Osteoporos Int 6:160–165
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR (1999) Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res 14:821–828
Samelson EJ, Hannan MT, Zhang Y, Genant HK, Felson DT, Kiel DP (2006) Incidence and risk factors for vertebral fracture in women and men: 25-year follow-up results from the population-based Framingham study. J Bone Miner Res 21:1207–1214
Schousboe JT, Rosen HR, Vokes TJ, Cauley JA, Cummings SR, Nevitt MC, Black DM, Orwoll ES, Kado DM, Ensrud KE, For the Osteoporotic Fractures in Men (MrOS) Study Research Group (2014) Prediction models of prevalent radiographic vertebral fractures among older men. J Clin Densitom 17:449–457
Schousboe JT, Debold CR (2006) Reliability and accuracy of vertebral fracture assessment with densitometry compared to radiography in clinical practice. Osteoporos Int 17:281–289
Hospers IC, van der Laan JG, Zeebregts CJ et al (2009) Vertebral fracture assessment in supine position: comparison by using conventional semiquantitative radiography and visual radiography. Radiology 251:822–828
Fuerst T, Wu C, Genant HK et al (2009) Evaluation of vertebral fracture assessment by dual X-ray absorptiometry in a multicenter setting. Osteoporos Int 20:1199–1205
Damiano J, Kolta S, Porcher R, Tournoux C, Dougados M, Roux C (2006) Diagnosis of vertebral fractures by vertebral fracture assessment. J Clin Densitom 9:66–71
Ferrar L, Jiang G, Schousboe JT, DeBold CR, Eastell R (2008) Algorithm-based qualitative and semiquantitative identification of prevalent vertebral fracture: agreement between different readers, imaging modalities, and diagnostic approaches. J Bone Miner Res 23:417–424
Vokes TJ, Dixon LB, Favus MJ (2003) Clinical utility of dual-energy vertebral assessment (DVA). Osteoporos Int 14:871–878
Rea JA, Li J, Blake GM, Steiger P, Genant HK, Fogelman I (2000) Visual assessment of vertebral deformity by X-ray absorptiometry: a highly predictive method to exclude vertebral deformity. Osteoporos Int 11:660–668
Schousboe JT, Vokes T, Broy SB et al (2008) Vertebral fracture assessment: the 2007 ISCD official positions. J Clin Densitom 11:92–108
Looker AC, Wahner HW, Dunn WL et al (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489
Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J (2013) National health and nutrition examination survey: plan and operations, 1999-2010. Vital Health Stat 1(56):1–37
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Centers for Disease Control and Prevention, National Center for Health Statistics. 2013-2014 Data documentation, codebook, and frequencies: dual-energy X-ray absorptiometry—Spine (DXXSPN_H). https://wwwn.cdc.gov/Nchs/Nhanes/2013–2014/DXXSPN_H.htm. Accessed 2 June 2016
Centers for Disease Control and Prevention, National Center for Health Statistics. 2013-2014 Data documentation, codebook, and frequencies: dual-energy X-ray absorptiometry—femur (DXXFEM_H). https://wwwn.cdc.gov/Nchs/Nhanes/2013–2014/DXXFEM_H.htm. Accessed 2 June 2016
Watts NB, Leslie WD, Foldes AJ, Miller PD (2013) 2013 International Society for Clinical Densitometry position development conference: Task Force on Normative Databases. J Clin Densitom 16:472–481
Wainwright SA, Marshall LM, Ensrud KE et al (2005) Study of Osteoporotic Fractures Research Group. Hip fracture in women without osteoporosis. J Clin Endocrinol Metab 90:2787–2793
Jackson SA, Tenenhouse A, Robertson L, CaMos Study Group (2000) Vertebral fracture definition from population-based data: preliminary results from the Canadian Multicenter Osteoporosis Study (CaMos). Osteoporos Int 11:680–687
O’Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ (1996) The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 11:1010–1018
Middleton ET, Steel SA (2008) Routine versus targeted vertebral fracture assessment for the detection of vertebral fractures. Osteoporos Int 19:1167–1173
Sanfélix-Genovés J, Reig-Molla B, Sanfélix-Gemeno G et al (2010) The population-based prevalence of osteoporotic vertebral fracture and densitometric osteoporosis in postmenopausal women over 50 in Valencia, Spain (the FRAVO Study). Bone 47:610–616
Kanterewicz E, Puigoriol E, García-Barrionuevo J, del Rio L, Casellas M, Peris P, Frodos Research Group (2014) Prevalence of vertebral fractures and minor vertebral deformities evaluated by DXA-assisted vertebral fracture assessment (VFA) in a population-based study of postmenopausal women: the FRODOS study. Osteoporos Int 25:1455–1464
Fujiwara S, Hamaya E, Goto W et al (2011) Vertebral fracture status and the World Health Organization risk factors for predicting osteoporotic fracture risk in Japan. Bone 49:520–525
Ismail AA, Cooper C, Felsenberg D et al (1999) Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. European Vertebral Osteoporosis Study Group. Osteoporos Int 9:206–213
Jiang G, Eastell R, Barrington NA, Ferrar L (2004) Comparison of methods for the visual identification of vertebral fractures. Osteoporos Int 15:887–896
Oei L, Rivandeira F, Ly F, Breda SJ, Zillikens MC, Hoffman A, Utterlinden AG, Krestin GP, Oei EHG (2013) A review of radiological scoring methods of osteoporotic vertebral fractures for clinical and research settings. Eur Radiol 23:476–486
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB (2009) Incidence and mortality of hip fractures in the United States. JAMA 302:1573–1579
Stevens JA, Anne Rudd R (2010) Declining hip fracture rates in the United States. Age Ageing 39:500–503
Wright NC, Saag KG, Curtis JR et al (2012) Recent trends in hip fracture rates by race/ethnicity among older US adults. J Bone Miner Res 27:2325–2332
Yu W, Lin Q, Zhou X, Shao H, Sun P (2014) Reconsideration of the relevance of mild wedge or short vertebral height deformities across a broad age distribution. Osteoporosis Int 25:2609–2615
Siris ES, Genant HK, Laster AJ, Chen P, Misurski DA, Krege JH (2007) Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporosis Int 18:761–770
Krege JH, Wan X, Lentle BC et al (2013) Fracture risk prediction: importance of age, BMD, and spine fracture status. BoneKEy Reports 2:404
Gallacher SJ, Gallagher AP, McQuillian C, Mitchell PJ, Dixon T (2007) The prevalence of vertebral fracture amongst patients presenting with non-vertebral fractures. Osteoporos Int 18:185–192
Siris ES, Adler R, Bilezikian J et al (2014) The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int 25:1439–1443
Van Staa TP, Laan RF, Barton IP et al (2003) Bone density threshold and other predictors of vertebral fracture in patients receiving oral glucocorticoid therapy. Arthritis Rheum 48:3224–3229
Domiciano DS, Figueiredo CP, Lopes JB, Kuroishi ME, Takayama L, Caparbo VF, Fuller P, Menezes PR, Scazufca M, Bonfa E, Pereira RMR (2013) Vertebral fracture assessment by dual X-ray absorptiometry: a valid tool to detect vertebral fractures in community-dwelling older adults in a population-based survey. Arthritis Care & Res 65:809–815
Zimmerman SI, Girman CJ, Buie VC et al (1999) The prevalence of osteoporosis in nursing home residents. Osteoporos Int 9:151–157
Acknowledgements
Financial support for the collection of osteoporosis-related data in NHANES 2013–2014 was provided by Eli Lilly and Company through a grant to the CDC Foundation. Eli Lilly and Company had no role in the collection of the data or the production of the public use datasets. The authors appreciate and acknowledge the contribution of Meng Lian in providing expert vertebral fracture assessment and Barbara Coffey, at Eli Lilly and Company, for manuscript process support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclosure
Dr. Cosman is a consultant to Lilly, Amgen, Merck, Radius, and Tarsa, has received grants (funding and/or medication) from Lilly and Amgen, and is a speaker for Lilly and Amgen. Drs. Krege and Krohn are employees and stockholders of Eli Lilly and Company. Dr. Shepherd has received grants from Amgen, Merck, and Hologic. Dr. Steiger is a stockholder of Optasia Medical. Dr. Wilson is an employee and stockholder of Hologic, Inc. Dr. Genant is a consultant to Lilly, Amgen, Merck, Janssen, Regeneron, Medtronic, AgNovos, BioMarin, Medimune, and BioClinica. Drs. Looker, Schousboe, Fan, and Sarafrazi Isfahani have no financial disclosures.
Conflicts of interest
None.
Additional information
Felicia Cosman and John H. Krege contributed equally.
Required disclaimer
The findings and conclusions in this report are those of the authors and not necessarily those of the Centers for Disease Control and Prevention.
Rights and permissions
About this article
Cite this article
Cosman, F., Krege, J.H., Looker, A.C. et al. Spine fracture prevalence in a nationally representative sample of US women and men aged ≥40 years: results from the National Health and Nutrition Examination Survey (NHANES) 2013-2014. Osteoporos Int 28, 1857–1866 (2017). https://doi.org/10.1007/s00198-017-3948-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-3948-9