Abstract
Introduction
Poor adherence reduces the potential benefits of osteoporosis therapy, lowering gains in bone mineral density resulting in increased risk of fractures.
Aim
To compare prescribing and adherence patterns of anti-osteoporotic medications in patients admitted to an urban teaching hospital in Ireland with a fragility type fracture to patients admitted to a rural hospital in the North Western region.
Methodology
We identified all patients >55 years admitted to Sligo General Hospital between 2005 and 2008 with a fragility fracture (N = 744) using the hospital in-patient enquiry system (HIPE). The medical card number of those patients eligible for the primary care reimbursement services scheme (PCRS) facilitated the linkage of the HSE-PCRS scheme database to the HIPE database which enabled a study to identify persistence rates of patients prescribed osteoporosis therapy after discharge. The results were compared to the findings of a similar study carried out in St. James’s Hospital, Dublin.
Results
The 12 months post-fracture prescribing increased from 11.0 % (95 % CI 9.6, 12.4) in 2005 to 47 % (95 % CI 43.6, 50.3) in 2008 in the urban setting and from 25 % (95 % CI 21.5, 28.9) to 39 % (95 % CI 34.5, 42.7) in the rural setting. Adherence levels to osteoporosis medications at 12 months post-initiation of therapy was <50 % in both study groups. Patients on less frequent dosing regimes were better adherers.
Conclusion
The proportion of patients being discharged on anti-osteoporosis medications post-fragility fracture increased between 2005 and 2008 in both patient groups. Sub-optimal adherence levels to osteoporosis medications continue to be a major concern.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The management of osteoporosis has become a major health problem worldwide. At least one in three women over 50 years of age, and one in five men, will suffer an osteoporotic fracture in their remaining lifetime [1]. Fragility fractures which are a direct result of osteoporosis give rise to significant morbidity and mortality, resulting in reductions in quality of life and increased and largely preventable expenditure on already budgetary constraint health care systems [2, 3]. Figures derived from the International Osteoporosis Foundation estimate that approximately 300,000 people over the age of 50 years have osteoporosis in Ireland. This figure accounts for 25 % of this population and with an increasing elderly population and longer life expectancy these figures are set to increase. Furthermore, a recent study by McGowan et al. [4] identified that the absolute numbers of hospitalisations in Ireland for fragility type fractures increased by 11 % in women and 15 % in men between 2000 and 2009. The results of an Irish Burden of Illness Study demonstrated that fall-related injuries in the elderly are projected to cost the Irish Health care system alone approximately €2,043 million in 2030 [5].
Over the last decade, there has been a considerable increase in the availability of new pharmacological agents for the management of osteoporosis. The efficacy of these products in reducing the risk of fracture is most evident in patients with established osteoporosis [6]. Despite the availability of proven cost-effective pharmacotherapy for managing osteoporosis, studies are continuing to show that post-fracture treatment with anti-osteoporosis medications remains suboptimal [7–10]. Furthermore, in more recent years, the issue of non-adherence with drug therapy particularly in chronic asymptomatic diseases, such as osteoporosis, further compromises the clinical and economic effects of the management of these patients. Several studies have identified that adherence to treatments in patients with osteoporosis continues to be poor, despite the availability of an increasing number of products with longer dosing regimes [11–13]. These studies have concluded that between 50 and 75 % of patients who were initiated anti-osteoporosis medications have discontinued their medications within 12 months of commencement. It is well recognised that poor adherence reduces the potential benefits of osteoporosis therapy, lowering gains in bone mineral density resulting in increased risk of fragility fractures [14]. In recent times, there have also been a number of studies published which have estimated the potential clinical and/or economic implications of poor adherence to osteoporosis medications [15–18].
According to the Report of the National Steering Group on the Prevention of Falls in Older People and the Prevention and Management of Osteoporosis throughout Life, “Current fall prevention services and bone health services appear to have developed in an ad hoc manner in Ireland. They are often championed by an individual health professional. While these efforts are to be applauded this approach is not sustainable. The challenge is to develop a structured, multidisciplinary, integrated strategy that addresses the needs of the population in a responsive, meaningful manner” [5]. The issue of poor adherence to osteoporosis medications was not referred to in this report. The Bone Health Clinics in the present study are part of a comprehensive Bone Health Service in the largest teaching hospital in Ireland and in a rural setting in The North West of Ireland. Both services were initiated in 2004/2005 and each covers a catchment area of approximately 250–300,000 people. All patients who present to the hospitals with classical fragility type fractures, such as hip and colles’ fracture are assessed using a dual-energy X-ray absorptiometry (DXA) scan. Furthermore, patients can be assessed for the presence of vertebral fractures using vertebral morphometry in all referrals for DXA. The clinics provide a service to other specialities in the hospitals, such as rheumatology and gastroenterology, as well as serving the local primary care physicians. Patients who have had a fracture are identified from the orthogeriatric ward rounds and also from the fracture clinics. Patients who may be at risk of sustaining a fracture are also referred to the clinics. Both clinics provide specialised bone biochemistry, a clinical nurse specialist assessment of falls and fracture risk, advice and subsequently a medical consultation. All physicians within both primary secondary and tertiary care have open access to refer patients to these clinics.
Aims
Using a linked database of hospitalisation and prescribing data, the aims of this study were to
-
1.
Examine the trends in prescribing of anti-osteoporosis medications in patients discharged from SGH in the North Western Region of Ireland for treatment of a fragility type fracture prior to and subsequent to their discharge between 2005 and 2008.
-
2.
Compare the results of this study to the prescribing in patients discharged from the largest urban teaching hospital in Ireland.
-
3.
Compare the adherence and persistence rates to osteoporosis medications of patients in the two different geographical areas of the country in the 24 months post-discharge.
-
4.
Examine the factors associated with prescribing of these therapies and medication adherence following discharge.
Methods
The hospital in-patient enquiry system
Data on hospital admissions for fracture were obtained from the local hospital in-patient enquiry system (HIPE) from Sligo General Hospital, which serves a catchment area of approximately 250,000 people in the North Western Region of Ireland. HIPE data are the only source of morbidity data available nationally for acute hospital services in Ireland. All acute public hospitals participate in HIPE reporting on over 1.3 million records annually. Data cover approximately 96 % of all admissions to a hospital. HIPE is a computer-based discharge abstracting system designed to collect demographic, clinical and administrative data on discharges and deaths from acute general hospitals nationally. The information from HIPE data used in this study is as follows: dates of admission and discharge, date of birth, sex, medical card status, and diagnosis (principal and secondary). The most important aspect of this process is the coding of the diagnoses and procedures performed using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Each HIPE discharge record represents details of one admission, and there may be more than one admission, in any given year. There were no risk-factor data available from this database. By identifying the specific codes for fractures, we examined data on all patients who were admitted to hospital for treatment of both typical and atypical osteoporotic type fractures between 2005 and 2008. A list of all fracture types included in the analyses based on ICD-10 coding can be found in “Appendix”. Patients who had sustained a fracture as a direct result of severe trauma, such as a road traffic accident, were excluded from the study. Only fractures sustained as a result of minimal trauma (defined as a fall from standing height or less, or a similar degree of injury) were included.
The HSE-PCRS pharmacy database
The health service executive primary care reimbursement services (HSE-PCRS; formerly known as the GMS medical services scheme) provide free health services under the general medical services (GMS) scheme which includes the provision of prescription medications. The eligibility for this scheme is means tested for those under 70 years of age and free for all those aged 70 or older. The scheme is over-represented by females and socioeconomically deprived and elderly persons, and covers approximately 33 % of the total population in Ireland, approximately 1.2 million individuals but accounts for approximately 70 % of all medications prescribed. The HSE-PCRS database records details on all prescriptions dispensed by pharmacists throughout Ireland for claims purposes from the GMS scheme. While clinical diagnosis is not recorded, full details on medications dispensed are recorded in the database using the WHO anatomical therapeutic chemical (ATC) classification system. Demographic details such as age and gender are also available in the database. The prescription database has been used widely for research purposes in Ireland. All prescription data on the main types of anti-osteoporosis treatments such as bisphosphonates and combinations of same along with strontium ranelate (Protelos)—ATC code M05B—in patients ≥55 years from 2006 to 2009 were included in the analyses.
Linking HIPE data to HSE-PCRS prescription data
Each patient eligible for the HSE-PCRS medical card scheme has a unique number. This information is recorded by the hospital administration at the time of admission, but at present it is not released to the national HIPE data. Linkage of the Sligo General Hospital HIPE data to the HSE-PCRS prescribing database was, therefore, possible and enabled a longitudinal study of patients who sustained an osteoporotic type fracture to include their medical management before and after discharge. The type of information gathered included the drug prescribed and dose and the number of patients admitted for treatment of subsequent fractures. It was also possible to identify whether the patients were on treatment or prophylaxis for osteoporosis prior to their admission as well as after their discharge. Permissions were obtained from the hospital’s ethics committee and chief executive’s office and the HSE-PCRS for linkage of the HIPE database. The linkage was made via the unique card number where available and was possible for 92 % of the study cohort. Once the linkage was completed, all unique identifiers were removed from the merged data set.
Statistical methods
Prescribing of anti-osteoporosis therapies was considered in the 12 months pre- and up to 24 months post-discharge. At the patient level, this refers to the follow-up time that prescribing was assessed after the fracture. In relation to the proportion of anti-osteoporosis medications prescribed to those with fractures, this was calculated as (number of fracture patients receiving anti-osteoporotic type medications)/(number of patients admitted to hospital with a fracture). Descriptive analysis on the medications prescribed in the study cohort with fractures before and after discharge is presented in the form of percentages and 95 % CIs for categorical data and mean ± SD for continuous normal data. Factors associated with prescribing of anti-osteoporotic medications post-fracture (age, gender, type of fracture, year of admission for fracture, prescribing pre-fracture) were examined univariately using Chi square tests. Any factors significant at the p < 0.10 level were included in a logistic model to examine the significant predictors of prescribing of anti-osteoporotic drugs after discharge. Adjusted odds ratios (OR) and 95 % CIs are presented. Longer-term prescribing trends were examined to determine when patients were commenced on their anti-osteoporotic type medications after discharge. SAS (SAS Institute Inc, Cary, NC, USA, v9.1) statistical software was used for analysis. Significance at p < 0.05 is assumed.
Persistence
All formulations were considered, including daily, weekly and monthly administration. Persistence refers to the proportion of those patients still receiving therapy at different periods after initiation (e.g. 6, 12, 18, 24, 30 and 36 months). A refill gap, or a break in the prescription refill, of 5 weeks was used to assess persistence. Persistence in all users (prevalent) and new users (incident) cases were considered. New users were defined as those not having received a prescription for the anti-osteoporosis therapy in the 6 months prior to the study.
Results
The data on approximately 79 % (821) of patients admitted to SJH and 85 % (744) of patients admitted to SGH ≥55 years who had sustained an osteoporotic type fracture during the study period were successfully linked to the HSE-PCRS prescribing database. Linkage of the datasets was not possible for a number of patients for the following reasons: invalid patient record number, no evidence of receiving a prescription and incorrect medical card numbers.
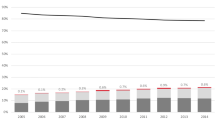
Pre-fracture treatment increased in the SGH group from 15.2 % in 2005 to 16.5 % by 2008, while post-fracture prescribing increased from 31.3 % in 2005 to 43.3 % in 2008. In comparison, pre-treatment in patients from St. James’s Hospital increased from 2.6 % in 2005 to 10.6 % by 2008 while post-fracture prescribing increased from 11 % in 2005 to 47 % in 2008 as illustrated in Fig. 1.
Seventy-six percent of patients overall were women, and the mean age of the study group was 78.14 (SD 9.53) years. Approximately, 65 % were ≥75 years of age, with 25 % > 85 years. There was little change in the numbers of patients >55 years admitted to both hospitals each year for management of a fracture during the study period. In the urban group, females were twice as likely to be prescribed anti-osteoporosis medications post-fracture whereas in the rural group females were four times more likely to be prescribed these medications as illustrated in Table 1. In the rural group, patients with a hip fracture were two and a half times more likely to be prescribed anti-osteoporosis medications than patients with a vertebral fracture attending the same service. Patients in the urban group with a hip fracture were 0.84 times more likely to be prescribed anti-osteoporosis medications than patients with a vertebral fracture over the study period. In the urban group, the 65 to 69-year age group was 10 times more likely than the 55 to 59-year age group to be prescribed anti-osteoporosis medications post-fracture. In the rural group, however, the 65 to 69-year age group was 1.8 times more likely than the 55 to 59-year age group to be prescribed these medications.
The persistence to medications post-fracture in those prescribed therapy was 64.9 % at 6 months and 47.8. % at 12 months in the urban group and 64.8 % at 6 months and 50 % at 12 months in the rural group as illustrated in Table 2. The differences here were not statistically significant. In the urban group, only 28.6 % of hip fracture patients prescribed therapies were persistent at 12 months in contrast to the rural group, where 50 % of the patients continued to be persistent at 12 months. Persistence did not vary with gender. Patients, however, who were prescribed the less frequent dosing regimes were more persistent than patients on more frequent dosing regimes. The difference in persistence between both study groups was not statistically significant.
Discussion
The current study has shown that the prescribing of anti-osteoporosis medications post-fracture has increased significantly since 2005 in both the urban and rural study populations. There was no statistically significant difference in the adherence to oral anti-osteoporosis medications between the urban and rural cohort at 6 and 12 months post-initiation of therapy. Overall adherence was found to be less than 50 % in both study groups at 12 months. While adherence improved with the less frequent dosing regimes in both study populations this was not statistically significant. In the urban study group, the 55 to 64-year age group was shown to be significantly poorer adherers. This is interesting in light of the fact that the recent Irish study by McGowan et al. [4] identified that between 2000 and 2009, the absolute numbers of all osteoporotic type fractures increased by 12 % in females and by 15 % in males, while the absolute numbers of hip fractures increased by 7 % in women and by 20 % in men. The age-specific rates, however, for hip fractures decreased in all age groups with the exception of the 55 to 59-year age group which showed an increase of 4.1 % (p = 0.023) within the study period. This age group was found to be the poorest adherers to anti-osteoporosis medications in the present study. The study by McGowan et al. also identified that assuming stable age-standardised incidence rates from 2009 over the next 20 years, the number of all types of osteoporotic type fractures is projected to increase by 79 % and the number of hip fractures is expected to increase by 88 % by 2025 unless adequate measures are put in place to successfully treat osteoporosis.
It has been estimated that approximately 50 % of the benefits of anti-osteoporosis medications seen in the clinical trials are lost to poor adherence resulting in a doubling of the cost per quality-adjusted life-year gained (QALY) from these medications [19]. It is now also well accepted that strategies to improve compliance and persistence with osteoporosis medications are urgently needed. Improving medication adherence is, however, a complex issue and present efforts across various chronic asymptomatic diseases have not shown significant improvements [20, 21]. A Systematic Review and Literature Appraisal by the ISPOR Medication Adherence & Persistence Special Interest Group [22, 23] concluded that additional research was needed to identify the impact of specific pharmacological treatments on patient medication adherence, especially since improving medication adherence may represent a cost-effective way of allocating resources. The working group also concluded that understanding the reasons for poor adherence, the preferences of patients for osteoporosis treatments and involving patients into clinical decision-making may also contribute to improve medication adherence.
There have been a number of studies carried out to examine both patients and providers perceptions of factors affecting adherence to osteoporosis medications [24, 25]. The study by Inversen et al. [25] identified that factors which contributed to poor adherence were lack of a full understanding of osteoporosis, dissatisfaction with their doctor visits, side effects of the drugs and difficulty in remembering instructions for taking the prescribed medications. Physicians identified patients’ lack of knowledge, structural barriers, side effects of the medications, and the inability to monitor patients’ adherence to their medications as barriers to adherence.
A 2005 survey, carried out on behalf of the International Osteoporosis Foundation (IOF), aimed to understand the reasons why women with osteoporosis do not stay on treatment. The adherence gap: Why osteoporosis patients don’t continue with treatment [26] was a five country European survey involving 500 physicians (primary care physicians and rheumatologists) and 502 women with postmenopausal osteoporosis. It showed that 34 % of women interviewed either did not know what the benefits of their medication were or wrongly thought there were no benefits at all. Drawbacks of treatment identified by women were predominantly related to inconvenience and side effects.
Viewpoints about treatments may differ between physicians and patients, making it difficult to achieve consensus about the best treatment. Open discussion is required if patients’ preferences are to be used to make decisions effectively [27, 28]. In recent years, several anti-osteoporosis medication options that include choices on timing of treatment, choice of product and dosing regime, routes and timing of administration have become available. Understanding patient’s preferences for osteoporosis treatments and involving patients into decision-making related to their own medical care may contribute to optimising treatment selection and consequently improve adherence. Patients increasingly want to be informed by their doctors, and be active in clinical decision-making. The patient’s perspective is becoming increasingly important in health care policy decisions. Over the last decade, discrete choice experiments (DCEs) have been increasingly used to identify collective preferences of various patient groups in health care [29]. This approach suggests that patient’s preferences are determined by the levels of different attributes [30]. DCEs can contribute to what are important attributes to provide knowledge on what the patient with a specific disease prefers and what the patient experiences. However, one cannot rely solely on collective-level approaches to identify individual patient preferences. By providing patients with a number of alternative options and their outcomes, and involving them in decision making, patient decision aids have been shown to improve patient’s satisfaction and the outcome of medical care [6, 31].
One limitation of this study is that patients on parathyroid hormone (PTH) or intravenous bisphosphonates were not included in the study. The HSE-PCRS scheme only contained information on the oral osteoporosis medications reimbursed under this scheme at the time the study was carried out. It was not possible, therefore, to identify if the patients who ceased their medications were prescribed I/V therapy. Based on the findings of a previously published study [32], approximately 10 % of patients prescribed anti-osteoporosis medications receive I/V bisphosphonates.
Conclusion
This study has demonstrated a dramatic increase in the prescribing of osteoporosis medications to patients admitted to an urban and rural hospital for treatment of a fragility fracture between 2005 and 2008. Similar, however, to the findings of other studies, treatment continues to be suboptimal. Furthermore, adherence levels to osteoporosis medications at 12 months post - initiation of therapy was less than 50 % in both study groups. The results of this study identified that adherence to anti-osteoporosis medications was not influenced by geographical location or by the type of service available.
References
Kanis JA, Johnell O, Oden A et al (2000) Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int 11(8):669–674
Johnell O, Kanis JA, Oden A et al (2004) Mortality after osteoporotic fractures. Osteoporos Int 15(1):38–42 (Epub 2003 Oct 30)
Lips P, Van Schoor NM (2005) Quality of life in patients with osteoporosis. Osteoporos Int 16(5):447–455 (Epub 2004 Dec 18)
McGowan B, Casey MC, Silke C et al (2012) Hospitalizations for fracture and associated costs between 2000 and 2009 in Ireland: a trend analysis. Osteoporos Int 24(3):849–857. doi:10.1007/s00198-012-2032-8 (Epub 2012 May 26)
Report of the National Steering Group on the Prevention of Falls in Older People and the Prevention and Management of Osteoporosis throughout Life (2008). Strategy to Prevent Falls and Fractures in Ireland’s Ageing Population. 2008 January. Available from URL: http://www.hse.ie/eng/services/Publications/services/Older/Strategy_to_Prevent_Falls_and_Fractures_in_Ireland%E2%80%99s_Ageing_Population_-_Full_report.pdf, Accessed 20 May 2012
Kanis JA, McCloskey EV, Johansson H et al (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24(1):23–57. doi:10.1007/s00198-012-2074-y (Epub 2012 Oct 19)
Elliott-Gibson V, Bogoch ER, Jamal SA et al (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int 15(10):767–778 (Epub 2004 Jul 16)
Fleurence RL, Iglesias CP, Torgerson DJ (2006) Economic evaluations of interventions for the prevention and treatment of osteoporosis: a structured review of the literature. Osteoporos Int 17(1):29–40 (Epub 2005 Jun 25)
Rabenda V, Vanoverloop J, Fabri V et al (2008) Low incidence of anti-osteoporosis treatment after hip fracture. J Bone Joint Surg Am. 90(10):2142–2148. doi:10.2106/JBJS.G.00864
Zethraeus N, Borgstrom F, Strom O et al (2007) Cost-effectiveness of the treatment and prevention of osteoporosis-a review of the literature and a reference model. Osteoporos Int 38(6):922–928 (Epub 2005 Dec 5)
Huybrechts KF, Ishak KJ, Caro JJ (2006) Assessment of compliance with osteoporosis treatment and its consequences in a managed care population. Bone 38(6):922–928 (Epub 2005 Dec 5)
Imaz I, Zegarra P, Gonzalez-Enriquez J et al (2010) Poor bisphosphonate adherence for treatment of osteoporosis increases fracture risk: systematic review and meta-analysis. Osteoporos Int 21(11):1943–1951. doi:10.1007/s00198-009-1134-4 (Epub 2009 Dec 5)
Rabenda V, Hiligsmann M, Reginster J-Y (2009) Poor adherence to oral bisphosphonate treatment and its consequences: a review of the evidence. Expert Opin Pharmacother 10(14):2303–2315. doi:10.1517/14656560903140533
Siris ES, Selby PL, Saag KG et al (2009) Impact of osteoporosis treatment adherence on fracture rates in North America and Europe. Am J Med 122(2 Suppl):S3–S13. doi:10.1016/j.amjmed.2008.12.002
Danese MD, Badamgarav E, Bauer DC (2009) Effect of adherence on lifetime fractures in osteoporotic women treated with daily and weekly bisphosphonates. J Bone Miner Res 24(11):1819–1826. doi:10.1359/jbmr.090506
Hiligsmann M, Rabenda V, Bruyere O et al (2010) The clinical and economic burden of non-adherence with oral bisphosphonates in osteoporotic patients. Health Policy 96(2):170–177. doi:10.1016/j.healthpol.2010.01.014 (Epub 2010 Feb 13)
Hiligsmann M, Rabenda V, Gathon HJ et al (2010) Potential clinical and economic impact of nonadherence with osteoporosis medications. Calcif Tissue Int 86(3):202–210
Landfeldt E, Lundkvist J, Strom O (2011) The societal burden of poor persistence to treatment of osteoporosis in Sweden. Bone 48(2):380–388. doi:10.1016/j.bone.2010.09.012 (Epub 2010 Sep 17)
Hiligsmann M, McGowan B, Bennett K et al (2012) The clinical and economic burden of poor adherence and persistence with osteoporosis medications in Ireland. Value Health 15(5):604–612. doi:10.1016/j.jval.2012.02.001 (Epub 2012 Apr 11)
Haynes RB, Ackloo E, Sahota N et al (2008) Interventions for enhancing medication adherence. Cochrane Database Syst Rev 16(2):CD000011. doi:10.1002/14651858.CD000011.pub3
McDonald HP, Garg AX, Haynes RB (2002) Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA 288(22):2868–2879
Hiligsmann M, Ravenda V, Bruyere O et al (2010) The clinical and economic burden of non-adherence with oral bisphosphonates in osteoporotic patients. Health Policy 96(2):170–177. doi:10.1016/j.healthpol.2010.01.014 (Epub 2010 Feb 13)
Patrick AR, Schousboe JT, Losina E et al (2011) The economics of improving medication adherence in osteoporosis: validation and application of a simulation model. J Clin Endocrinol Metab 96(9):2762–2770. doi:10.1210/jc.2011-0575 (Epub 2011 Jul 6)
Copher C, Buzinec P, Zarotsky V et al (2010) Physician perception of patient adherence to osteoporosis medications from pharmacy claims. Curr Med Res Opin 26(4):777–785. doi:10.1185/03007990903579171
Iversen MD, Vora RR, Servi A et al (2011) Factors affecting adherence to osteoporosis medications: a focus group approach examining viewpoints of patients and providers. J Geriatr Phys Ther 34(2):72–81. doi:10.1097/JPT.0b013e3181ff03b4
International Osteoporosis Foundation (2005) The adherence gap: why osteoporosis patients don’t continue with treatment. www.iofbonehealthorg/download/ostefound/filemanager/publications/pdf/adherence_gap_reportpdf, Accessed 26 May 2012
Elwyn G, Edwards A, Britten N (2003) What information do patients need about medicines? “Doing prescribing”: how doctors can be more effective. BMJ 327(7419):864–867
Lewis DK, Robinson J, Wilkinson E (2003) Factors involved in deciding to start preventive treatment: qualitative study of clinicians’ and lay people’s attitudes. BMJ 327(7419):841
Louviere JJ, Islam T (2008) A comparison of importance weights and willingness-to-pay measures derived from choice-based conjoint, constant sum scales and best-worst scaling. J Bus Res 61(9):903–911
Elwyn G, O’Connor A, Stacey D et al (2006) Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ 333(7565):417 (Epub 2006 Aug 14)
Elwyn G, Kreuwel I, Durand MA et al (2011) How to develop web-based decision support interventions for patients: a process map. Patient Educ Couns 82(2):260–265. doi:10.1016/j.pec.2010.04.034 (Epub 2010 Jun 2)
McGowan B, Bennett K, Marry J, Walsh JB, Casey MC (2012) Patient profile in a bone health and osteoporosis prevention service in Ireland. IJMS 181(4):511–515. doi:10.1007/s11845-012-0806-9 (Epub 2012 Feb 29)
Acknowledgments
We would like to thank the Health Services Executive-Primary Care Reimbursement Service (HSE-PCRS) for providing the prescribing data for the present study and the Hospital In-Patient Enquiry (HIPE) units in both St. James’s hospital and Sligo Regional Hospital for providing the discharge fracture data.
Conflict of interest
The authors of this article have “no competing interests”.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 3.
Rights and permissions
About this article
Cite this article
McGowan, B., Bennett, K., Casey, M.C. et al. Comparison of prescribing and adherence patterns of anti-osteoporotic medications post-admission for fragility type fracture in an urban teaching hospital and a rural teaching hospital in Ireland between 2005 and 2008. Ir J Med Sci 182, 601–608 (2013). https://doi.org/10.1007/s11845-013-0935-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-013-0935-9