Abstract
Summary
Nonagenarians differ from patients aged 70–79 and 80–89 years in baseline characteristics, complication and mortality rates. Differences increased gradually with age. The results of this study can be used, in combination with the Almelo Hip Fracture Score, to deliver efficiently targeted orthogeriatric treatment to the right patient group.
Purpose
In previous literature, elderly with a hip fracture are frequently defined as ≥ 70 years. However, given the ageing population and the rapidly increasing number of ‘nonagenarians’ (aged ≥ 90 years), the question rises whether this definition is still actual. The aim of this study is to determine whether nonagenarians show differences compared to patients aged 70–79 years and patients aged 80–89 years in terms of patient characteristics, complications and mortality rate.
Methods
From April 2008 until December 2016, hip fracture patients aged ≥ 70 years treated according to our orthogeriatric treatment model were included. Patients were divided into three different groups based on age at admission: 70–79 years, 80–89 years and ≥ 90 years. Patient characteristics, risk of early mortality, complications and outcomes were analysed. Risk factors for 30-day mortality in nonagenarians were determined.
Results
A total of 1587 patients were included: 465 patients aged 70–80 years, 867 patients aged 80–90 years and 255 patients aged ≥ 90 years. Nonagenarians were more often female and had a lower haemoglobin level at admission. Prefracture, they were more often living in a nursing home, were more dependent in activities of daily living and mobility and had a higher risk of early mortality calculated with the Almelo Hip Fracture Score (AHFS). Post-operative, nonagenarians suffer significantly more often from delirium and anaemia. The 30-day mortality and 1-year mortality were significantly higher. Differences increased gradually with age.
Conclusion
Nonagenarians differ from patients aged 70–79 and 80–89 years in baseline characteristics, complication and mortality rates. Differences increased gradually with age. The results of this study can be used, in combination with the Almelo Hip Fracture Score, to deliver efficiently targeted orthogeriatric treatment to the right patient group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The general population is ageing, and due to this, the incidence of hip fractures increases, affecting at this moment 1.5 million people per year worldwide [1,2,3]. In the past decades, geriatric co-management appeared to be inevitable in older patients with a hip fracture [4]. In 2008, the Centre for Geriatric Traumatology (CvGT) was implemented at our hospital. It was the first centre in the Netherlands to implement the integrated orthogeriatric treatment model for elderly with a hip fracture. At the CvGT, all hip fracture patients aged 70 years or older are treated according to this orthogeriatric treatment model, which led to a decrease in complications and mortality [5, 6]. However, given the increasing incidence of hip fractures, the high costs and the limited workforce availability, the question rises if all patients aged 70 years or older should be treated according to the same orthogeriatric treatment model [7]. Targeted orthogeriatric treatment strategy in patient subgroups may contribute to efficiency in hip fracture care and could reduce costs.
With the longer life expectancy, the number of patients aged 90 years or older is also growing. In 2015, there were 16.13 million nonagenarians, which is expected to increase to 76.71 million in 2050 [8]. In line with that, there will likely be a continuing increase in the number of nonagenarians sustaining hip fractures in the coming years. These nonagenarians may require particular orthogeriatric attention because of their advanced age and comorbidities [9]. There have been a few papers written about hip fractures in the extreme elderly [10,11,12,13]. These studies show differences in complication risk and prognosis. However, most studies concern the (non-)operative management and/or outcomes of centenarians and include a low number of patients [14,15,16,17]. Literature regarding targeted orthogeriatric treatment in age subgroups is scarce. A recent study of Liu et al. (2019) showed that superaged patients (80 years or older) could benefit from targeted treatment [18]. The Trondheim hip-fracture trial earlier showed that the effect of comprehensive geriatric care was most pronounced in younger female participants with higher prefracture i-ADL function [19].
The aim of this study is to determine whether nonagenarians show differences compared with patients aged 70–79 years and patients aged 80–89 years in terms of patient characteristics, complications and mortality rate. We hypothesised that there are differences between these age groups that could make a targeted treatment strategy beneficial.
Materials and methods
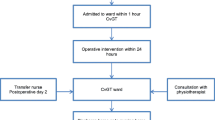
A prospective cohort study was performed among patients treated surgically in the Centre of Geriatric Traumatology of a level 2 trauma centre for non-pathological hip fractures. Between April 2008 and December 2016, all operatively treated patients aged over 70 years were included. Patients with a pathological or periprosthetic fracture and referral to the orthopaedic service (for instance, for total hip arthroplasty) were excluded. Patients who were not treated according the orthogeriatric treatment model were those who were admitted to a department where the treatment model was not yet implemented. Patients were surgically treated with osteosynthese (proximal femur nail anti-rotation, dynamic hip screw or three cannulated screws) or hip hemiarthroplasty.
Study procedure and data collection
Treatment was performed accordingly to our integrated orthogeriatric care model, using a multidisciplinary treatment protocol supported by clinical care pathways [5, 20]. In the Centre of Geriatric Traumatology, uniform data collection and recordings of all patient data were achieved by a standard evaluation according to the clinical pathway for hip fracture patients.
The following patient characteristics were registered: age, gender, American Society of Anaesthesiologists (ASA score) physical status classification [21], dementia, Charlson Comorbidity Index (CCI score) [22], malnutrition, living situation, Parker Mobility Score (PMS) [23], Katz-ADL,, Barthel Index [24], the Almelo Hip Fracture Score (AHFS), haemoglobin level, fracture type, surgery within 24 h after admission, type of surgery and the length of stay.
The ASA score is an assessment of a patient’s overall health before the surgery, scored by anaesthesiologists classification (ASA 1, a normal healthy patient; ASA 2, a patient with mild systemic disease; ASA 3, a patient with severe systemic disease that is not life-threatening; ASA 4, a patient with severe systemic disease that is a constant threat to life) [21]. The CCI score contains 19 weighted comorbidities predictive for the 1-year mortality [22]. Malnutrition was assessed using the Short Nutritional Assessment Questionnaire (SNAQ score) [25]. Malnutrition is scored if the SNAQ score is ≥ 2, based on three weighed questions concerning weight, appetite and supplemental drinks/tube feeding. The PMS measures the mobility level before fracture, with a total score ranging from 0 (no walking ability) to 9 (fully independent walking ability) [23, 26]. The Barthel Index measures independence in activity of daily living (ADL), with a total score ranging from 0 (fully dependent in ADL) to 20 (fully independent in ADL) [24].
The AHFS is a risk score containing weighted 9 risk factors [27]. The score ranges from 3 to 19 points, predicting a risk of early mortality ranging from 0.0 to 68.4%. Cut-off points of AHFS ≤ 9 and AHFS ≥ 13 are used to divide patients into a low-, medium- or high-risk group.
The following complications were registered prospectively using the clinical care pathway: anaemia, arrhythmia, cerebrovascular accident, delirium, heart failure exacerbation, myocardial infarction, pneumonia, urinary tract infection, wound infection, readmission, reoperation, implant dislocation and implant failure. Appendix 1 presents the definitions of the complications. Mortality data have been obtained from the municipal death registry and was documented in time intervals: in-hospital mortality, mortality within 30 days and 1 year after hip fracture surgery. To scrutinise the in-hospital logistics, time to surgery after arrival to the hospital and length of hospital stay were registered.
Patients were subsequently subdivided into three different study groups, based on age 70–79 years, 80–89 years and 90+ years of age (nonagenarians). These groups will be regarded to respectively as group 1, group 2 and group 3 in the remaining of this article.
Statistical analysis
Categorical variables are described as number with corresponding percentages. Continuous variables are described as mean with standard deviation (SD) or in case of non-parametric data as median with interquartile range (IQR). Differences in patient characteristics, complications and mortality were tested between the three different patient groups using chi-squared test (Fisher’s exact tests if appropriate) for categorical data and a one-way ANOVA with a Tukey’s post hoc test or a Kruskal-Wallis test for continuous data.
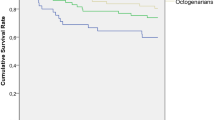
In order to identify a subset of variables that are associated with early mortality following hip fracture surgery in nonagenarians, differences in baseline characteristics and complications between the 30-day mortality and the survival subgroup (within nonagenarians) were tested. Associated variables were described with odds ratio (OR) and 95% confidence interval (95% CI). Level of significance was set at ≤ 0.05 for all analyses. Survival was illustrated using a Kaplan-Meier plot. Data were analysed using the Statistical Package for Social Sciences (SPSS) version 24.0 (SPSS Inc. Chicago, IL).
Results
A total of 2828 patients were admitted to the hospital with a hip fracture during the study period, of which 1587 matched our inclusion criteria (Fig. 1, study inclusion and exclusion criteria). Thirty-two patients were included twice because of a hip fracture on the contralateral side occurred during follow-up. The mean follow-up time was 4 years and 10 months (ranging from 12 to 117 months). Four hundred and sixty-five patients (29.3%) were addressed to group 1, 867 patients (54.6%) were addressed to group 2 and 255 patients (16.1%) were addressed to group 3.
Patient characteristics
Perioperative characteristics are shown in Table 1; post hoc analyses are presented in Table 3. Older patients were significantly more often female (chi-squared post hoc test: group 1 vs group 2, p = 0.010; group 1 vs group 3, p < 0.001; group 2 vs group 3, p = 0.017) and were more often living in a nursing home (chi-squared post hoc tests all p < 0.001). Furthermore, they were more dependent in activities of daily living and mobility (Mann-Whitney U post hoc test Barthel Index all p < 0.001; Katz-ADL group 2 vs group 3 p = 0.019, other p < 0.001; PMS all p < 0.001). Dementia was more often seen in group 2 and 3 than group 1 (chi-squared post hoc test: group 1 vs group 3, p < 0.001; group 1 vs group 2, p < 0.001). A fractured collum femoris was more often seen in group 1 in comparison to group 3 (chi-squared post hoc test: group 1 vs group 3, p = 0.014). Older patients had a significant higher AHFS (p < 0.001). At admission, older age groups had a lower haemoglobin level (Mann-Whitney U post hoc test group 2 vs 3, p = 0.001, other p < 0.001). Group 1 was less often treated with a hemiarthroplasty in comparison to group 2 and 3 (chi-squared post hoc test: group 1 vs group 2 and group 2 vs group 3, p < 0.001).
Complications
Complications in different age groups are illustrated in Table 2. Overall, 49.5% of patients (n = 785) suffered from one or more complication. The number of patients suffering from one or more complications increased with age (chi-squared post hoc test: group 2 vs group 3, p = 0.014; other p < 0.001). Group 2 and 3 had a significant higher number of anaemia needing transfusion and delirium (chi-squared post hoc test anaemia and delirium: group 1 vs group 2 and group 1 vs group 3, p < 0.001). There was a significant association between post-operative delirium and anaemia. Group 1 less often suffered from heart failure than group 3 (chi-squared post hoc test: group 1 vs group 3, p = 0.018). There was no significant difference in other complications.
Reasons for readmission and reoperation
There were no significant differences in the number of readmission or reoperation between the three age groups. Overall, 53 patients (3.3%) were readmitted within 30 days. Reasons for readmissions were deep wound infection (23 patients, 1.4%), failure of PFNA (6 patients, 0.4%), anaemia (3 patients, 0.2%), pneumonia or urinary tract infection (10 patients, 0.7%), luxation of hip hemiarthroplasty (3 patients, 0.2%), wound dehiscence (3 patients, 0.2%) and failure of dynamic hip screw (4 patients, 0.3%). After 30 days, 15 patients (1.5%) needed a reoperation. Reasons for reoperation after 30 days were wound infection (3 patients, 0.2%), failure of PFNA (5 patients, 0.3%), evacuation of haematoma (7 patients, 0.4%), luxation of hemiarthroplasty (2 patients, 0.1%) and failure of dynamic hip screw or avascular femur head necrosis (5 patients, 0.3%).
Mortality
Overall, in-hospital mortality was 3.9% (n = 62), 30-day mortality was 8.0% (n = 127) and 1-year mortality was 23.9% (n = 380). There was a significant difference between the age groups in 30-day mortality and 1-year mortality (both p < 0.001). The 30-day mortality rate in group 1, 2 and 3 was respectively 4.5%, 8.3% and 13.3%. The 1-year mortality rate in group 1, 2 and 3 was respectively 17.0%, 22.5% and 38.4%. The 30-day mortality was increasing with age (chi-squared post hoc test: group 1 vs group 2, p = 0.010; group 1 vs group 3, p < 0.001; group 2 vs group 3, p = 0.016), even as the 1-year mortality (chi-squared post hoc test all p < 0.001). Figure 2 illustrates the significant differences in 1-year survival with 83.0% survival in group 1, 74.0% in group 2 and 61.6% in group 3.
Nonagenarians: risk factors associated with 30-day mortality
Preoperative, univariate analysis revealed that nonagenarians with a living situation in a nursing home had a significantly higher mortality risk within the first 30 days post-operatively compared with nonagenarians who lived on their own (OR 2.23, 95% CI 1.00–4.95, p = 0.045). Dementia was also identified as a univariate preoperative risk factor associated with 30-day mortality (OR 2.17, 95% CI 1.02–4.58, p = 0.043), as well as having two or more comorbidities (OR 3.49, 95% CI 1.56–7.81, p = 0.002), dependency in ADL (OR 3.27, 95% CI 0.96–11.15, p = 0.058) or an ASA score of 3 or 4 (OR 7.95, 95% CI 1.85–34.07, p = 0.005). Perioperative surgery after the first 24 h after admission had a significantly (OR 2.50, 95% CI 1.32–4.72, p = 0.006) negative influence on 30-day survival. Reasons to postpone surgery were oral anticoagulation and admissions with an active pulmonary infection. Type of surgery did not influence 30-day mortality. Post-operative, hospital-acquired pneumonia (OR 4.06, 95% CI 1.65–10.0, p = 0.002) and exacerbation of heart failure (OR 5.76, 95% CI 2.24–14.83, p = 0.001) were univariately associated with 30-day mortality.
Discussion
In the current practice, orthogeriatric hip fracture patients are frequently addressed to as one group (defined as 70 years of age or older). The results of this study are in line with our stated hypotheses that nonagenarians differ from other age groups in terms of patient characteristics, complications and mortality rates. This is an important finding, because this knowledge could contribute to targeting treatment strategy in hip fracture patients that might be beneficial for aiming the best possible care as efficiently as possible.
Multiple baseline differences between the nonagenarians and their relatively younger peers were found. Nonagenarians are more often female, which can be a result of in general longer life expectancy of female [28]. Furthermore, they are more dependent in activities of daily living and mobility and have a lower haemoglobin level at admission. This is an important finding; the AHFS already showed that dependency in mobility and haemoglobin level at admission are independent risk factors for early mortality [27]. Post-operative nonagenarians suffer more often from anaemia and delirium, and there was also a significant relationship between anaemia and delirium. Probably, the lower level of haemoglobin at admission influenced the increased number of post-operative anaemia. This subsequently might have led to a higher incidence of delirium. In addition, advanced age is also a well-known risk factor for delirium [29]. Knowing that these complications are higher in the nonagenarians, extra attention should be given for detection of anaemia at admission and proactive treatment of this condition. Also, preventive measures can be implemented, such as the use of tranexamic acid to reduce the perioperative blood loss and managing delirium risk factors [30].
The overall survival rate found in this study is 74.6% comparable to other literature [31,32,33]. We found that nonagenarians are at the greatest risk of mortality compared to their peers aged 70–89 years. Mortality gradually increased with age. This is in line with the study of Mariconda et al. (2015) who illustrated a worse survival for patients with an advanced age [34]. One of the reasons for the higher mortality rate in the older patients is the a priori lower life expectancy [35]. However, the impact of a hip fracture on mortality cannot be underestimated; nonagenarians without a hip fracture in this period in the Netherlands had a 1-year mortality rate of 26.4%, while the 1-year mortality rate in nonagenarians with a hip fracture in our study is 38.4% [36, 37].
Factors that we have found in this study contributing in the higher risk of 30-day mortality in nonagenarians are as follows: living in a nursing home, dependency based on Katz-ADL, dementia, having two or more comorbidities, ASA score 3 or 4, surgery performed after the first 24 h, post-operative pneumonia and exacerbation of heart failure. As in previous studies, the type of surgery did not influence survival [38]. Other studies illustrated the same risk factors on mortality and added preoperative low haemoglobin, obesity, dialysis and diabetes as an independent risk factor for outcome [33, 34, 39]. These risk factors should be taken into account in planning a treatment strategy. Possible strategies to reduce the risk of mortality in nonagenarians could be striving to perform surgery within the first 24-h, perioperative fluid volume optimization and implement programs to prevent pulmonary complications such as I COUGH [40,41,42].
In this study we questioned if nonagenarians with a hip fracture need a different orthogeriatric treatment strategy, as it might be not necessary to treat all hip fracture patients in the same intensive way. In nonagenarians, who suffer more often from dementia and dependency in ADL and mobility, other treatment goals may be pursued than in younger patients. Furthermore, it is important that intensive geriatric co-management should be applied in the most vulnerable group (e.g. daily consultation of the geriatrician) and less intensive in the relatively vital patients (e.g. one-time consultation). In this way, extra attention then could be given to the patients who need it. Efficiency in hip fracture care is important, given the increasing number of hip fracture patients, limited workforce availability and high costs [2, 43, 44]. Nonetheless, it stands to reason that age alone is not per se the best screening tool for determining the intensity of treatment. For instance, the Trondheim hip-fracture trial earlier showed that the effect of comprehensive geriatric care was most pronounced in younger female participants with higher prefracture i-ADL function [19].
An alternative screening tool to apply a less or more intensive orthogeriatric treatment might be based on a risk model, for instance, by using the AHFS. This score classifies patients in a low-intermediate or high-risk group, based on nine weighted risk factors. The AHFS has an overlap with preoperative risk factors found in the nonagenarians in this study: living in an institution, having two or more comorbidities, ASA score 3 or 4 and cognitive dysfunction. Other risk factors included in the AHFS are as follows: age ≥ 86 years, male gender, low admission serum haemoglobin, having a malignancy in the past 20 years and Parker Mobility Score < 6 [27]. Most of these risk factors are also incorporated in multiple other frailty indices. In practice, patients falling in the low-risk group could get a less intensive orthogeriatric treatment or only if needed (e.g. in case of complications), and patients falling in the high-risk group could get a more intensive orthogeriatric treatment. Future research should be done to investigate if different orthogeriatric treatments in the targeted orthogeriatric patient categories could lead to more efficient care, reduced costs and better outcomes.
Limitations of this study
A limitation of this study is the possible selection bias due to our inclusion criteria: for instance, vital patients treated with a total hip arthroplasty were excluded. Unfortunately, we were not able to perform a multivariate regression analysis in order to identify the independent risk factors for 30-day mortality in the nonagenarians. This was due to a too low numbers of deceased nonagenarians for proper analysis. Besides, we did not analyse the impact of a hip fracture on the quality of life and the patient perspective. This should be part of future studies.
Strengths of this study
This big cohort study with over 1500 orthogeriatric patients is unique in describing three different orthogeriatric age groups and can therefore illustrate the differences in baseline characteristics, complications and prognosis.
In conclusion, this study illustrates that nonagenarians show differences on preoperative characteristics, complications and prognosis, compared to patients aged 70–89 years. Nonagenarians are more often female, living in a nursing home, suffering from dementia and dependent in ADL and mobility. Most of these differences gradually increased with age. Post-operatively, they suffer more often from anaemia and delirium and have a higher risk of 30-day and 1-year mortality. The results of this study can be used, in combination with the AHFS, to deliver efficiently targeted orthogeriatric treatment to the right patient group.
References
Hartholt KA, van Beeck EF, Polinder S, van der Velde N, van Lieshout EMM, Panneman MJM, van der Cammen TJM, Patka P (2011) Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma 71:748–753
Cooper C, Campion G, Melton LJ (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650
Grigoryan KV, Javedan H, Rudolph JL (2014) Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma NIH Public Access 28:e49–e55
Folbert EC, Hegeman JH, Vermeer M, Regtuijt EM, van der Velde D, ten Duis HJ, Slaets JP (2017) Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos Int 28:269–277
Nijmeijer WS, Folbert EC, Vermeer M, Vollenbroek-Hutten MMR, Hegeman JH (2018) The consistency of care for older patients with a hip fracture: are the results of the integrated orthogeriatric treatment model of the Centre of Geriatric Traumatology consistent 10 years after implementation? Arch Osteoporos 13:131
Zielinski SM, Bouwmans CAM, Heetveld MJ, Bhandari M, Patka P, Van Lieshout EMM (2014) The societal costs of femoral neck fracture patients treated with internal fixation. Osteoporos Int 25:875–885
United Nations, Department of Economic and Social Affairs, Population Division PE and PS. World Population Prospects 2019. Population by Age and Sex (thousands) 2015–2050. https://population.un.org/wpp/DataQuery/. Accessed 12 August 2019
Rivoirard R, Chargari C, Trone J, Falk A, Guy J, Eddekaoui H, Lahmar R, Pacaut C, Mery B, Assouline A, Auberdiac P, Moriceau G, Gonthier R, Guillot A, Merrouche Y, Magné N (2014) General management of nonagenarian patients: a review of the literature. Swiss Med Wkly EMH Media 144:w14059
Ooi LH, Wong TH, Toh CL, Wong HP (2005) Hip fractures in nonagenarians—a study on operative and non-operative management. Injury. 36:142–147
Daruwalla ZJ, Wong KL, Malhotra R, Leong KM, Nee PY, Murphy DP (2016) Hip fracture surgery in nonagenarians-the Devil’s advocate? J Am Geriatr Soc 64:210–211
Dick AG, Davenport D, Bansal M, Burch TS, Edwards MR (2017) Hip fractures in centenarians: has care improved in the National Hip Fracture Database Era? Geriatr Orthop Surg Rehabil 8:161–165
Holt G, Smith R, Duncan K, Hutchison J, Gregori A (2008) Outcome after surgery for the treatment of hip fracture in the extremely elderly. J Bone Jt Surg-Am 90:1899–1905
Jennings AG, de Boer P (1999) Should we operate on nonagenarians with hip fractures? Injury 30:169–172
Shabat S, Mann G, Gepstein R, Fredman B, Folman Y, Nyska M (2004) Operative treatment for hip fractures in patients 100 years of age and older: is it justified? J Orthop Trauma 18:431–435
Tarity TD, Smith EB, Dolan K, Rasouli MR, Maltenfort MG (2013) Mortality in centenarians with hip fractures. Orthopedics. 36:e282–e287
Verma R, Rigby AS, Shaw CJ, Mohsen A (2009) Acute care of hip fractures in centenarians—do we need more resources? Injury 40:368–370
Liu Z, Zhang J, He K, Zhang Y, Zhang Y (2019) Optimized clinical practice for superaged patients with hip fracture: significance of damage control and enhanced recovery program. Burns Trauma 7:21
Prestmo A, Saltvedt I, Helbostad JL, Taraldsen K, Thingstad P, Lydersen S, Sletvold O (2016) Who benefits from orthogeriatric treatment? Results from the Trondheim hip-fracture trial. BMC Geriatr BioMed Central 16:49
Folbert EC, Smit R, van der Velde D, Regtuijt EM, Klaren MH, Hegeman JH (2012) Geriatric fracture center: a multidisciplinary treatment approach for older patients with a hip fracture improved quality of clinical care and short-term treatment outcomes. Geriatr Orthop Surg Rehabil SAGE Publications 3:59–67
Daabiss M (2011) American Society of anaesthesiologists physical status classification. Indian J Anaesth Wolters Kluwer -- Medknow Publ 55:111–115
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Parker MJ, Palmer CR (1993) A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg (Br) 75:797–798
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Wijnhoven HAH, Schilp J, van Bokhorst-de van der Schueren MAE, de Vet HCW, Kruizenga HM, Deeg DJH, Ferrucci L, Visser M (2012) Development and validation of criteria for determining undernutrition in community-dwelling older men and women: the short nutritional assessment questionnaire 65+. Clin Nutr NIH Public Access 31:351–358
Kristensen MT, Foss NB, Ekdahl C, Kehlet H (2010) Prefracture functional level evaluated by the new mobility score predicts in-hospital outcome after hip fracture surgery. Acta Orthop 81:296–302
Nijmeijer WS, Folbert EC, Vermeer M, Slaets JP, Hegeman JH (2016) Prediction of early mortality following hip fracture surgery in frail elderly: the Almelo Hip Fracture Score (AHFS). Injury. 47:2138–2143
Nordström P, Thorngren K-G, Hommel Phd A, Ziden Phd L, Anttila S (2018) Effects of geriatric team rehabilitation after hip fracture: meta-analysis of randomized controlled trials. J Am Med Dir Assoc 19(10):840–845
Yang Y, Zhao X, Dong T, Yang Z, Zhang Q, Zhang Y (2017) Risk factors for postoperative delirium following hip fracture repair in elderly patients: a systematic review and meta-analysis. Aging Clin Exp Res 29:115–126
Baskaran D, Rahman S, Salmasi Y, Froghi S, Berber O, George M (2018) Effect of tranexamic acid use on blood loss and thromboembolic risk in hip fracture surgery: systematic review and meta-analysis. HIP Int 28:3–10
Hu F, Jiang C, Shen J, Tang P, Wang Y (2012) Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury Elsevier Ltd 43:676–685
Maxwell MJ, Moran CG, Moppett IK (2008) Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth 101:511–517
Belmont PJ, Garcia EJ, Romano D, Bader JO, Nelson KJ, Schoenfeld AJ (2014) Risk factors for complications and in-hospital mortality following hip fractures: a study using the National Trauma Data Bank. Arch Orthop Trauma Surg 134:597–604
Mariconda M, Costa GG, Cerbasi S, Recano P, Aitanti E, Gambacorta M, Misasi M, Mariconda M, Gambacorta M, Misasi M (2015) The determinants of mortality and morbidity during the year following fracture of the hip. Bone Joint J 97-B(3):383–390
Estimated life expectancy at birth, females - European Health Information Gateway. https://gateway.euro.who.int/en/indicators/hfa_72-1092-estimated-life-expectancy-world-health-report-females/. Accessed 23 August 2019
CBS. StatLine - Overledenen; geslacht, leeftijd, burgerlijke staat, regio. https://opendata.cbs.nl/statline/#/CBS/nl/dataset/03747/table?ts=1568381192468. Accessed 23 August 2019
CBS. StatLine - Bevolking; geslacht, leeftijd en burgerlijke staat. https://opendata.cbs.nl/statline/#/CBS/nl/dataset/7461bev/table?ts=1568381326981. Accessed 23 August 2019
Galler M, Zellner M, Roll C, Bäuml C, Füchtmeier B, Müller F (2018) A prospective study with ten years follow-up of two-hundred patients with proximal femoral fracture. Injury. 49:841–845
Pugely AJ, Martin CT, Gao Y, Klocke NF, Callaghan JJ, Marsh JL (2014) A risk calculator for short-term morbidity and mortality after hip fracture surgery. J Orthop Trauma 28:63–69
Cassidy MR, Rosenkranz P, McCabe K, Rosen JE, McAneny D (2013) I COUGH. JAMA Surg Am Med Assoc 148:740
Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, DeBeer J, Bhandari M (2010) Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. Can Med Assoc J 182:1609–1616
Lewis SR, Butler AR, Brammar A, Nicholson A, Smith AF (2016) Perioperative fluid volume optimization following proximal femoral fracture. Cochrane Database Syst Rev 3:CD003004
Polinder S, Haagsma J, Panneman M, Scholten A, Brugmans M, Van Beeck E (2016) The economic burden of injury: health care and productivity costs of injuries in the Netherlands. Accid Anal Prev Pergamon 93:92–100
Lötters FJB, van den Bergh JP, de Vries F, Rutten-van Mölken MPMH (2016) Current and future incidence and costs of osteoporosis-related fractures in the Netherlands: combining claims data with BMD measurements. Calcif Tissue Int 98:235–243
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix. Definitions of complications
Appendix. Definitions of complications
Anaemia: requiring transfusion based on the transfusion guidelines (CBO, 2007)
Arrhythmia: in comparison with electrocardiogram at admission, with need for treatment
Cerebrovascular accident: hemiparesis of hemiplegia, a CT cerebrum is performed
Delirium: based on the Delirium Observation Screening Scale, score above 3 and geriatrician diagnosis confirmed in medical record
Heart failure: clinical presentation and/or diagnosis confirmed on chest radiograph. Treatment started with diuretics
Myocardial infarction: elektrocardiogram abnormalities suspicious for ischemia and elevated cardiac troponin level
Pneumonia: clinical presentation and/or diagnosis confirmed on chest radiograph. Treatment started with antibiotics
Urinary tract infection: urine sediment with positive WBC and nitrite. Treatment started with antibiotics
Wound infection, superficial: diffuse redness, serous fluid leakage and no fever (RIVM, 2014)
Wound infection, deep: worse than superficial, need for revision
Readmission: admission within the first 30 days after discharge
Reoperation: operation within the first 60 days after initial surgery
Implant dislocation: diagnosis confirmed on XR, need for revision
Implant failure: diagnosis confirmed on XR, need for revision
Rights and permissions
About this article
Cite this article
de Groot, R., Nijmeijer, W.S., Folbert, E.C. et al. ‘Nonagenarians’ with a hip fracture: is a different orthogeriatric treatment strategy necessary?. Arch Osteoporos 15, 19 (2020). https://doi.org/10.1007/s11657-020-0698-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-020-0698-7