Abstract
Summary
In the past 10 years after implementation, the orthogeriatric treatment model led in general to consistent outcomes for 1555 older adults in terms of most of the complications and mortality. Surgery was more often delayed to 24–48 h after arrival at the hospital, while the length of hospital stay shortened.
Introduction
Since 1 April 2008, patients aged ≥ 70 years presenting themselves with a hip fracture at Ziekenhuisgroep Twente (ZGT) have been treated according to the orthogeriatric treatment model. The aim of this study was to investigate if outcomes of the orthogeriatric treatment model are consistent over the first 10 years after implementation.
Methods
Between 1 April 2008 and 31 December 2016, patients aged ≥ 70 years who were surgically treated at ZGT for a hip fracture were included and divided into three periods equally distributed in time. Patient characteristics, in-hospital logistics, complications, and mortality data were compared between the three periods.
Results
A total of 1555 patients were included. There was a shift in the surgical treatment for the fractured neck of femur from dynamic hip screw/cannulated screws to hemiarthroplasty (p < 0.001). Surgery within 24 h after arrival to the hospital decreased (p < 0.001), while surgery within 48 h stayed the same (p = 0.085). Length of hospital stay significantly decreased over time (p < 0.001). Complication rates were consistent except for the number of postoperative anemia, delirium, and urinary tract infections. Mortality rates did not change over the years.
Conclusions
The orthogeriatric treatment model leads in general to consistent outcomes concerning mortality and most of the complications, except for postoperative anemia, delirium, and urinary tract infections. Inconsistent complication rates were influenced by altered diagnosis and treatment protocols. Length of hospital stay reduced, while time to surgery was more often delayed to 24–48 h. Monitoring clinical outcomes of the orthogeriatric treatment model over time is recommended in order to optimize and maintain the quality of care for this frail patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are common, affecting 1.5 million people per year worldwide. Due to the aging of population, hip fractures are expected to increase to approximately 6.3 million per year by 2050 [1]. Most hip fracture patients are characterized by older age, multiple comorbidities, and functional and cognitive impairment. The prognosis of a hip fracture is poor. One-year mortality can be up to 36%. Only 50% of the patients who were able to function independently in performing basic activities of daily living (ADL) before the fracture regain independence in performing ADL at 6 months after surgery [2,3,4].
In April 2008, the Centre for Geriatric Traumatology (CvGT) was founded at Ziekenhuisgroep Twente (ZGT) location Almelo in order to optimize the quality of care for this frail population. It was the first center in the Netherlands with an integrated orthogeriatric treatment model. Three years later, the treatment model was also implemented at the other location of the hospital. The treatment model is characterized by rapid surgical management, intensive co-management by the geriatrician, and the use of multidisciplinary clinical pathways, starting at the emergency department (ED) up to the outpatient clinic. Besides focusing on trauma surgery, these pathways focus on other age-related aspects such as limiting the risk of developing delirium, comorbidity, nutritional status, osteoporosis, and prevention of falls. One of the most important features of this treatment model is the proactive attitude on preventing patients from adverse events.
Earlier research of Folbert et al. has shown that the implementation of the orthogeriatric treatment model at ZGT was associated with a reduction in complications, length of stay, re-admissions, in-hospital mortality, and 1-year mortality [5, 6]. These studies describe the unfavorable patient profile of our population. Age, comorbidities, osteoporosis, and dementia make that the elderly hip fracture patient is more frail than the elderly patient without a hip fracture [7]. The concept of frailty is a geriatric syndrome characterized by the age-associated decline in physiological reserve and function across multi-organ systems, leading into increased vulnerability for adverse health outcomes [8].
Nowadays, we are 10 years after the implementation of the orthogeriatric treatment model. Although there are a number of papers published about outcomes of the orthogeriatric treatment for older adults with hip fractures in comparison to usual care, literature about the consistency of the outcome of the treatment model after the implementation phase is scarce [6, 9,10,11,12,13]. The aim of this study was to evaluate the consistency of the orthogeriatric treatment model over the past 10 years, in terms of in-hospital logistics, postoperative complications and mortality. This could be useful in order to evaluate the quality of care given to this patient population, change treatment protocols if needed, and share experiences for benchmarking with other hospitals.
Methods
Study design
Between 1 April 2008 and 31 December 2016, all patients with the diagnostic treatment code “218 Femur, proximal (+collum)” treated at both locations of ZGT were included. Patients younger than 70 years, patients without a hip fracture, and patients not surgical treated in ZGT were excluded. Other exclusion criteria were preoperative mortality, pathological or periprosthetic fracture, referral to the orthopedic service for total hip arthroplasty and patients not treated according to the orthogeriatric treatment model. Patients who were not treaded according the orthogeriatric treatment model were those who were admitted to a department where the treatment model was not yet implemented. Included patients were divided into three periods, equally distributed in time based on date of admission: P1 (April 2008–February 2011), P2 (March 2011–January 2014), and P3 (February 2014–December 2016). In the first period, the orthogeriatric treatment model was only implemented at location A. Location H started with the implementation at the second period, taking the experiences of the health care professionals of location A into account. In the first period (P1), patients treated at location A were included; at the second and third period (P2 and P3), patients from both locations were included.
Setting
The integrated orthogeriatric treatment model at ZGT was characterized by early geriatric co-management starting at the admission to the ED. At the ED, most hip fractures were diagnosed using radiographs, consisting of an anteroposterior and a lateral projection of the hip. Blood tests, a chest radiograph, and an electrocardiography were taken for pre-operative assessment. The patient was admitted to the CvGT as fast as possible. The geriatrician was called by the physician at the ED and visited the patient at the ED or CvGT. Comprehensive geriatric assessment was performed to identify geriatric conditions and to develop a personalized treatment plan. Hip fracture surgery was performed as fast as safely possible. In the CvGT, the patient was daily visited by a resident surgery (RS), a nurse practitioner (NP), or a physician assistant (PA) specialized in trauma surgery. The treatment was evaluated in a daily meeting between the RS/NP/PA and the geriatrician. During admission, a medication review, osteoporosis status, possible causes of falls, and nutritional status took place. A multidisciplinary meeting was held twice a week, in which a trauma surgeon, a geriatrician, a dietician, a physiotherapist and an elderly care physician were present. The aim was to have the patients ready for discharge within 5 days after surgery.
Data collection
In this study, the patient characteristics registered at baseline were age, gender, American Society of Anesthesiologist physical status classification (ASA score) [14], Charlson Comorbidity Index (CCI score) [15], pre-fracture living, fracture type, surgical treatment, hemoglobin level at admission, anemia at admission (defined as hemoglobin levels < 7.45 mmol/l in female and < 8.07 mmol/l in male [16]), dementia, history of osteoporosis, the Barthel Index (at admission and at discharge), and the Parker Mobility Score (PMS) [17]. The ASA score is an assessment of a patient’s overall health before the surgery, scored by anesthesiologists [14]. The CCI score contains 19 weighted comorbidities predictive for the 1-year mortality, including diabetes with diabetic complications, congestive heart failure, peripheral vascular disease, chronic pulmonary disease, mild and severe liver disease, hemiplegia, renal disease, leukemia, lymphoma, metastatic tumor, and acquired immunodeficiency syndrome [15]. The Barthel Index measures independence in activity of daily living (ADL) at admission and at discharge, with a total score ranging from 0 (fully dependent in ADL) to 20 (fully independent in ADL) [17]. The PMS measures the mobility level before fracture at admission, with a total score ranging from 0 (no walking ability) to 9 (fully independent walking ability) [18, 19].
The following complications were registered prospectively using the clinical care pathway: postoperative anemia, arrhythmia, cerebrovascular accident, delirium, heart failure, myocardial infarction, pneumonia, pulmonary embolism, renal failure, urinary tract infection, reoperation, and mortality (see Appendix 1 for definitions of complications). Mortality data have been obtained from the municipal death registry and was documented in time intervals: in-hospital mortality, and mortality within 30 days, 1 year, and 3 years after hip fracture surgery. Data of the 3-year survival of the third period (P3) was not yet available. To scrutinize the in-hospital logistics, length of stay at the ED, time to surgery after arrival to the hospital, and length of hospital stay were registered.
Statistical analysis
Categorical variables are described as number with corresponding percentages. Continuous variables are described as mean with standard deviation (SD), or in case of non-parametric data as median with interquartile range (IQR). Differences in baseline characteristics, logistic outcomes, complications, and mortality were tested between the three different periods using a chi-square test (Fisher’s exact tests if appropriate) for categorical data and a one-way ANOVA with a Tukey’s post hoc test, or a Kruskal-Wallis test for continuous data. Survival analysis was performed using Kaplan-Meier analysis. Three-year survival rates were described in percentages with 95% confidence intervals (CI). Comparison of the survival distribution was performed using the log rank test. A p < 0.05 was regarded as being statistically significant. All statistical analyses were carried out using the Statistical Package for the Social Sciences version 23 (SPSS Inc., Chicago, USA).
Results
Patient characteristics
A total of 2938 patients with a hip fracture were registered, of which 2082 patients were 70 years or older and underwent a surgical procedure for hip fracture in ZGT. A total of 527 patients were excluded as a consequence of preoperative mortality, pathological or periprosthetic fracture, total hip arthroplasty placement, double cases, or patients not treated according the orthogeriatric treatment model of the CvGT (Fig. 1). Of the 1555 patients included, 385 patients were admitted during the first period (P1: April 2008–February 2011), and respectively, 589 and 581 were admitted during the second (P2: March 2011–January 2014) and third period (P3: February 2014–December 2016).
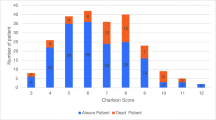
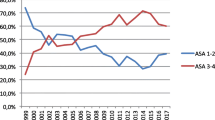
Seventy-two percent (n = 1118) of the included patients were female. The mean age was 83.1 years (SD 6.4 years). There was no difference in age (p = 0.106) or gender (p = 0.094) between the three periods. Sixty-eight percent of the included patients (n = 1038) had an ASA score of ≥ 3. Patients in the first and second period had a significantly higher ASA score in comparison to the patients in the third period (ASA ≥ 3: P1 = 81.2%, P2 = 71.5%, P3 = 53.3%, p < 0.001). There was a shift in the surgical treatment of the fractured neck of femur from dynamic hip screw (DHS)/cannulated screws to hemiarthroplasty (p < 0.001). Other baseline characteristics were not different between the three periods presented (Table 1).
In-hospital logistics
In-hospital logistics are presented in Table 2. The length of stay at the emergency department decreased significantly over the years (p = 0.020). Surgery within 24 h after arrival to the hospital decreased (P1 = 72.9%, P2 = 73.8%, P3 = 64.7%, p < 0.001), whereas surgery within 48 h after arrival to the hospital did not change over the periods (p = 0.085): 96.2% of all the patients underwent surgery within 48 h after arrival to the hospital. Length of hospital stay in days significantly decreased over time (median (IQR): P1 = 9.8 (6.0–15.8), 7.9 (5.9–11.0), 6.9 (5.9–8.9), p < 0.001).
Complications
Complications, mortality, and 3-year survival are presented in Table 3. The number of arrhythmia, cerebrovascular accident, heart failure, myocardial infarction, pneumonia, pulmonary embolism, and renal failure was not different between the periods. The number of postoperative anemia was comparable for the first (15.8%) and second period (19.4%), but significantly increased in the third period (25.2%) (chi-square post hoc test: P1 versus P3, p = 0.001; P2 versus P3, p = 0.017). Type of surgery was significantly associated with postoperative anemia (anemia per type of surgery: dynamic hip screw (DHS)/cannulated screws 7.0%, hemiarthroplasty 19.4%, proximal femur nail antirotation (PFN) 29.9%, p < 0.001). There was no difference in postoperative anemia per period per type of surgery. The number of urinary tract infections significantly decreased over the time (P1 = 10.1%, P2 = 8.3%, P3 = 4.3%, (p = 0.001)). There was a difference in number of observed delirium over period (P1 = 28.1%, P2 = 22.9%, P3 = 31.5%, p = 0.004). The prevalence of delirium significantly increased in P3 in comparison to P2 (chi-square post hoc test: p = 0.001), but no differences were found between P1 and P2 or P1 and P3 (chi-square post hoc test respectively p = 0.070 and p = 0.253). There was a significant association between the complications postoperative anemia and observed delirium (26.3% (n = 112) anemia in patients with a delirium, 18.5% (209) anemia without a delirium, p = 0.001). The number of reoperations and the reason for reoperation within 60 days after surgery did not differ between the three periods. Deep wound infection as reason for reoperation did not change over period (chi-square post hoc test, p = 0.293).
Mortality
The overall in-hospital mortality was 5.0% (n = 77), and the 30-day mortality was 8.0% (n = 124). Over periods, there was no difference in in-hospital mortality or 30-day mortality. Also, the 1-year mortality did not change over period (P1 = 25.2%, P2 = 23.4%, P3 = 22.5%; p = 0.635). The 3-year survival in the first period of 51% (95% CI 45–56%) was comparable with the 3-year survival of 56% in the second period (95% CI 52–60%, p = 0.262) (Fig. 2).
Discussion
The aim of this study was to investigate if the outcomes of the orthogeriatric treatment model are consistent over the first 10 years after its implementation. Our results show in general consistent outcomes in terms of mortality and most of the complications, except for postoperative anemia, delirium, and urinary tract infection. This study is one of the few studies concerning the consistency of care and the long-term outcomes of the orthogeriatric treatment model [20].
We found that there was no difference in mortality over the first 10 years after the implementation. The mortality observed is comparable with mortality rates of 2.3–13.9% in-hospital mortality, 3.3–17.2% 30-day mortality, and 5.9–50.0% 1-year mortality mentioned in earlier studies [2, 3].
Most of the complication rates were also consistent over time. The inconsistent complication rates found were probably influenced by altered diagnosis and treatment protocols. For instance, the diagnosis urinary tract infection was based upon urine sediment analysis in the first years. However, the diagnostic value of urine sediment analysis in patients with a catheter pointed out to be limited as a result of contamination. Therefore, pretreatment positive urine culture was considered as the golden standard in the last years. As a consequence, the number of urinary tract infection following the definition given in Appendix 1 decreased. The increased number of postoperative anemia in the third period is a consequence of the altered treatment for fractured neck of femur, as can be expected due to more perioperative blood loss in patients undergoing a hemiarthroplasty [21, 22]. It is important to realize that the altered treatment has led to an increase of postoperative anemia, because anemia could also lead to an increase of other complications. Therefore, the use of tranexamic acid to reduce the total blood loss might be a next step in further optimizing the care for elderly hip fracture patients [23].
The number of postoperative anemia was highest in patients treated with PFN. This is in line with previous studies that have shown that intramedullary fixation devices made a higher incidence of blood transfusions, probably due to the type of fracture (extracapsular) and the opening of the medullary cavity and proximal reaming [24,25,26,27]. In our study, the number of postoperative anemia in patients treated with PFN was consistent over time. However, the hemoglobin level before surgery tended to be lower, and the number of preoperative anemia tended to be higher in the third period; there was no significant difference found over period in these patient characteristics. For this reason, it was not possible to find a relationship between a preoperative low hemoglobin level and/or anemia and postoperative.
The percentage observed delirium increased in the last period. We found a significant relationship between the complications postoperative anemia and observed delirium which is in line with the results of Blandfort et al., who found that a higher postoperative hemoglobin level after hip fracture surgery reduced the risk of delirium [28]. Despite the trend of lower mean hemoglobin level at admission and increase in prevalent anemia, there was no significant difference over the period. Therefore, it is not possible in our study to find a relation between prevalent anemia or hemoglobin level at admission and postoperative delirium. The relatively low percentage of delirium found in the second period could be a consequence of the start of the treatment model at location H, where the health care professionals were not yet as well educated as they were at location A. This may have led to a less frequently diagnosed delirium. Earlier studies have shown that delirium is often misdiagnosed due to lack of knowledge and awareness in nurses and doctors [29]. In our study, health care professionals were educated over time. Early recognition and diagnosis through growing geriatric expertise within the various disciplines contributed to the increase in number of diagnosed cases of delirium. A recommendation that could be made for the future is to put even more focus on diagnosing delirium.
Overall, the exact number of postoperative anemia (20.6%) and urinary tract infections (7.3%) is relatively low in comparison to wide range presented in previous studies (anemia 24–44%, urinary tract infections 12–61%) [30, 31]. The incidence of delirium (27.4%) is comparable to previous studies (13–56%) [30, 32].
The in-hospital logistics were inconsistent over time. The length of stay at the ED reduced. Patients had to wait longer for surgery, and fewer patients were treated within 24 h after arrival at the hospital. This might be partly a result of the introduction of the direct oral anticoagulants, which has to be omitted during 48 h before hip fracture surgery can take place [33]. Other reason may be a lower threshold for delaying surgery in order to achieve a better medical condition of the patient to reduce the risk of perioperative complications (e.g., in case of a pneumonia) or limited capacity of operating rooms. Surgical treatment within 48 h should be pursued following the national guidelines and the guidelines of the American Academy of Orthopedic Surgeons (AAOS), because there is no evidence for fewer complications when performing surgery within 24 h [34, 35]. In our study, the number of patient treated within 48 h was consistent over time.
The length of hospital stay decreased significantly, which is mostly a result of the agreements made with the nursing homes in order to shorten waiting time until transfer to geriatric rehabilitation departments. Over time, the patient characteristics did not change, except for the ASA score. The decreased percentage of patients with ASA ≥ 3 suggests that the patient’s overall health nowadays is better before the surgery, but it could also be influenced by inconsistency of grading the ASA score between anesthesiologists that has been demonstrated in multiple studies before [14]. Another changed baseline characteristics was the type of surgery. We found strong evidence supporting hemiarthroplasty for patients with displaced femoral neck fractures which led to a shift in the surgical treatment of the fractured neck of femur from dynamic hip screw (DHS)/cannulated screws towards hemiarthroplasty over the years [34].
Since the implementation of the CvGT, we collect data for process monitoring, quality assessment, and research. Due to the aging population, the number of hip fractures is expected to increase. Much work has been done to optimize the treatment of this vulnerable elderly group. It might be worthwhile to use the results of this study for benchmarking with other hospitals and for national and international research into long-term effectiveness.
In our perspective, recommendations for future research would be to investigate the economic effect of the orthogeriatric comanagement, the effects of the use of direct oral anticoagulants on the outcome of hip fracture patients, the prevention of the most common complications (e.g., postoperative anemia, delirium, and pneumonia), and the evaluation of patient-reported outcome measurements.
Strengths and weaknesses analysis
One of the strengths of this study is that it is one of the few studies concerning the long-term outcomes of the orthogeriatric treatment. It is the first study in the Netherlands presenting the consistency of care in the first 10 years after implementation of the orthogeriatric treatment model, with a large study population. This study shows valuable insights in logistics and the outcomes that can be used for optimizing care.
A limitation of the study is selection bias, because the fittest elderly were treated with a total hip prosthesis and are excluded in this series. Overestimation of the favorable results seems therefore unlikely. Other points of criticism are the lack of literature to compare the study results with the missing data on the impact of a hip fracture on quality of life and the patient perspective.
Conclusion
The orthogeriatric treatment model for older adults with a hip fracture led in general to consistent outcomes in the 10 years after implementation in terms of mortality and most of the complications, except for postoperative anemia, delirium, and urinary tract infection. Length of hospital stay shortened, while surgery is more often delayed to 24–48 h after arrival at the hospital. Monitoring clinical outcomes of the orthogeriatric treatment model over time is recommended in order to optimize and maintain the quality of care for this frail patient population.
References
Cheng SY, Levy AR, Lefaivre KA, Guy P, Kuramoto L, Sobolev B (2011) Geographic trends in incidence of hip fractures: a comprehensive literature review. Osteoporos Int 22:2575–2586. https://doi.org/10.1007/s00198-011-1596-z
Forni S, Pieralli F, Sergi A, Lorini C, Bonaccorsi G, Vannucci A (2016) Mortality after hip fracture in the elderly: the role of a multidisciplinary approach and time to surgery in a retrospective observational study on 23,973 patients. Arch Gerontol Geriatr 66:13–17. https://doi.org/10.1016/j.archger.2016.04.014
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650. https://doi.org/10.1007/s00198-009-0920-3
Jamal Sepah Y, Umer M, Khan A, Ullah Khan Niazi A (2010) Functional outcome, mortality and in-hospital complications of operative treatment in elderly patients with hip fractures in the developing world. Int Orthop 34:431–435. https://doi.org/10.1007/s00264-009-0803-4
Folbert ECE, Smit RS, van der Velde D, Regtuijt EMM, Klaren MH, Hegeman JHH (2012) Geriatric fracture center: a multidisciplinary treatment approach for older patients with a hip fracture improved quality of clinical care and short-term treatment outcomes. Geriatr Orthop Surg Rehabil 3:59–67. https://doi.org/10.1177/2151458512444288
Folbert EC, Hegeman JH, Vermeer M, Regtuijt EM, van der Velde D, ten Duis HJ, Slaets JP (2017) Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos Int 28:269–277. https://doi.org/10.1007/s00198-016-3711-7
Auais M, Morin S, Nadeau L, Finch L, Mayo N (2013) Changes in frailty-related characteristics of the hip fracture population and their implications for healthcare services: evidence from Quebec, Canada. Osteoporos Int 24:2713–2724. https://doi.org/10.1007/s00198-013-2390-x
Leng S, Chen X, Mao G (2014) Frailty syndrome: an overview. Clin Interv Aging 9:433. https://doi.org/10.2147/CIA.S45300
Grigoryan KV, Javedan H, Rudolph JL (2014) Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma 28:e49–e55. https://doi.org/10.1097/BOT.0b013e3182a5a045
Flikweert ER, Izaks GJ, Knobben BA et al (2014) The development of a comprehensive multidisciplinary care pathway for patients with a hip fracture: design and results of a clinical trial. BMC Musculoskelet Disord 15:188. https://doi.org/10.1186/1471-2474-15-188
Prestmo A, Hagen G, Sletvold O, Helbostad JL, Thingstad P, Taraldsen K, Lydersen S, Halsteinli V, Saltnes T, Lamb SE, Johnsen LG, Saltvedt I (2015) Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet 385:1623–1633. https://doi.org/10.1016/S0140-6736(14)62409-0
Kammerlander C, Roth T, Friedman SM, Suhm N, Luger TJ, Kammerlander-Knauer U, Krappinger D, Blauth M (2010) Ortho-geriatric service—a literature review comparing different models. Osteoporos Int 21:637–646. https://doi.org/10.1007/s00198-010-1396-x
Kates SL (2016) Hip fracture programs: are they effective? Injury 47:S25–S27. https://doi.org/10.1016/S0020-1383(16)30006-7
Daabiss M (2011) American Society of Anaesthesiologists physical status classification. Indian J Anaesth 55:111–115. https://doi.org/10.4103/0019-5049.79879
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Blanc B, Finch CA, Hallberg L et al (1968) Nutritional anaemias. Report of a WHO scientific group. World Health Organ Tech Rep Ser 405:1–40
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Parker MJ, Palmer CR (1993) A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br 75:797–798
Kristensen MT, Foss NB, Ekdahl C, Kehlet H (2010) Prefracture functional level evaluated by the new mobility score predicts in-hospital outcome after hip fracture surgery. Acta Orthop 81:296–302. https://doi.org/10.3109/17453674.2010.487240
Lau TW, Fang C, Leung F (2017) The effectiveness of a multidisciplinary hip fracture care model in improving the clinical outcome and the average cost of manpower. Osteoporos Int 28:791–798. https://doi.org/10.1007/s00198-016-3845-7
de Palma L, Torcianti M, Meco L, Catalani A, Marinelli M (2013) Operative delay and mortality in elderly patients with hip fracture: an observational study. Eur J Orthop Surg Traumatol 28:1–6. https://doi.org/10.1007/s00590-013-1241-y
Sciard D, Cattano D, Hussain M, Rosenstein A (2011) Perioperative management of proximal hip fractures in the elderly: the surgeon and the anesthesiologist. Minerva Anesthesiol 77:715–722
Baskaran D, Rahman S, Salmasi Y, Froghi S, Berber O, George M (2018) Effect of tranexamic acid use on blood loss and thromboembolic risk in hip fracture surgery: systematic review and meta-analysis. HIP Int 28:3–10. https://doi.org/10.5301/hipint.5000556
Hou G, Zhou F, Tian Y, Ji H, Zhang Z, Guo Y, Lv Y (2014) Predicting the need for blood transfusions in elderly patients with pertrochanteric femoral fractures. Injury 45:1932–1937. https://doi.org/10.1016/j.injury.2014.08.033
Adunsky A, Lichtenstein A, Mizrahi E et al (2003) Blood transfusion requirements in elderly hip fracture patients. Arch Gerontol Geriatr 36(1):75–81. https://doi.org/10.1016/S0167-4943(02)00059-6
Foss NB, Kehlet H (2006) Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br 88–B:1053–1059. https://doi.org/10.1302/0301-620X.88B8.17534
Kadar A, Chechik O, Steinberg E, Reider E, Sternheim A (2013) Predicting the need for blood transfusion in patients with hip fractures. Int Orthop 37:693–700. https://doi.org/10.1007/s00264-013-1795-7
Blandfort S, Gregersen M, Borris LC, Damsgaard EM (2017) Blood transfusion strategy and risk of postoperative delirium in nursing homes residents with hip fracture. A post hoc analysis based on the TRIFE randomized controlled trial. Aging Clin Exp Res 29:459–466. https://doi.org/10.1007/s40520-016-0587-5
Schuurmans MJ, Duursma SA, Shortridge-Baggett LM (2008) Early recognition of delirium: review of the literature. J Clin Nurs 10:721–729. https://doi.org/10.1111/j.1365-2702.2001.00548.x
Carpintero P, Caeiro JR, Carpintero R et al (2014) Complications of hip fractures: a review. World J Orthop. https://doi.org/10.5312/wjo.v5.i4.402
Bliemel C, Buecking B, Hack J, Aigner R, Eschbach DA, Ruchholtz S, Oberkircher L (2017) Urinary tract infection in patients with hip fracture: an underestimated event? Geriatr Gerontol Int 17:2369–2375. https://doi.org/10.1111/ggi.13077
Oh ES, Li M, Fafowora TM, Inouye SK, Chen CH, Rosman LM, Lyketsos CG, Sieber FE, Puhan MA (2015) Preoperative risk factors for postoperative delirium following hip fracture repair: a systematic review HHS public access. Int J Geriatr Psychiatry 30:900–910. https://doi.org/10.1002/gps.4233
Yassa R, Khalfaoui MY, Hujazi I et al (2017) Management of anticoagulation in hip fractures: a pragmatic approach. EFORT Open Rev 2:394–402. https://doi.org/10.1302/2058-5241.2.160083
American Academy of Orthopeadic Surgeons Guideline: Management of hip fractures in the elderly (2014) https://www.aaos.org/Reasearch/guidelines/HipFxGuideline_rev.pdf. Accessed 13 Oct 2018
Richtlijn proximale femurfracturen (2016) https://richtlijnendatabase.nl/richtlijn/prixmale_femurfracturen/proximale_femurfracturen_-_startpagina.html. Accessed 13 Oct 2018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
ESM 1
(DOCX 69 kb)
Rights and permissions
About this article
Cite this article
Nijmeijer, W.S., Folbert, E.C., Vermeer, M. et al. The consistency of care for older patients with a hip fracture: are the results of the integrated orthogeriatric treatment model of the Centre of Geriatric Traumatology consistent 10 years after implementation?. Arch Osteoporos 13, 131 (2018). https://doi.org/10.1007/s11657-018-0550-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0550-5