Abstract
Summary
To improve the quality of care and reduce the healthcare costs of elderly patients with a hip fracture, surgeons and geriatricians collaborated intensively due to the special needs of these patients. After treatment at the Centre for Geriatric Traumatology (CvGT), we found a significant decrease in the 1-year mortality rate in frail elderly patients compared to the historical control patients who were treated with standard care.
Introduction
The study aimed to evaluate the effect of an orthogeriatric treatment model on elderly patients with a hip fracture on the 1-year mortality rate and identify associated risk factors.
Methods
This study included patients, aged 70 years and older, who were admitted with a hip fracture and treated in accordance with the integrated orthogeriatric treatment model of the CvGT at the Hospital Group Twente (ZGT) between April 2008 and October 2013. Data registration was carried out by several disciplines using the clinical pathways of the CvGT database. A multivariate logistic regression analysis was used to identify independent risk factors for 1-year mortality. The outcome measures for the 850 patients were compared with those of 535 historical control patients who were managed under standard care between October 2002 and March 2008.
Results
The analysis demonstrated that the 1-year mortality rate was 23.2 % (n = 197) in the CvGT group compared to 35.1 % (n = 188) in the historical control group (p < 0.001). Independent risk factors for 1-year mortality were male gender (odds ratio (OR) 1.68), increasing age (OR 1.06), higher American Society of Anesthesiologists (ASA) score (ASA 3 OR 2.43, ASA 4–5 OR 7.05), higher Charlson Comorbidity Index (CCI) (CCI 1–2 OR 1.46, CCI 3–4 OR 1.59, CCI 5 OR 2.71), malnutrition (OR 2.01), physical limitations in activities of daily living (OR 2.35), and decreasing Barthel Index (BI) (OR 0.96).
Conclusion
After integrated orthogeriatric treatment, a significant decrease was seen in the 1-year mortality rate in the frail elderly patients with a hip fracture compared to the historical control patients who were treated with standard care. The most important risk factors for 1-year mortality were male gender, increasing age, malnutrition, physical limitations, increasing BI, and medical conditions. Awareness of risk factors that affect the 1-year mortality can be useful in optimizing care and outcomes. Orthogeriatric treatment should be standard for elderly patients with hip fractures due to the multidimensional needs of these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to the aging population, the number of hip fractures will increase because of the elevated risk of falling and osteoporosis in the elderly [1–4]. The consequences of a hip fracture are serious. On average, one in three patients die within the first year of sustaining this type of fracture, and in more than half of these patients, their mobility is still limited 1 year after injury [5, 6]. Age-related aspects, such as comorbidity, frailty, and polypharmacy, indicate that treatment is complex. The risks that patients will develop severe complications and loss of function are considerable and often associated with high treatment costs [7].
In Great Britain in the 1960s, geriatric consultations were introduced to improve the care for elderly patients with hip fractures [8]. Following this example, over the last 20 years, surgeons and geriatricians have been working together more intensively, resulting in a variety of treatment models of care. Recently, international guidelines and recommendations have addressed the importance of combined geriatric and surgical treatment as an alternative to traditional treatment.
In 2008, the Geriatric Traumatology Center (CvGT) at Ziekenhuisgroep Twente Almelo-Hengelo (ZGT) was the first center in the Netherlands to implement the integrated orthogeriatric treatment model for elderly patients with a hip fracture. Recent reviews of Kammerlander and Grigoryan and co-workers have shown that there are beneficial effects of integrated orthogeriatric care in comparison with other models [9, 10]. However, empirical data on the efficacy of integrated orthogeriatric care are scarce.
The objective of our study was to analyze the incidence of the 1-year mortality and its risk factors in elderly patients with a hip fracture who have been treated with an integrated orthogeriatric model of care in comparison with patients managed under standard care before the introduction of the CvGT. In order to support future research and benchmarking into this field, we used outcome parameters based on international guidelines and recommendations from an international expert group [11].
Methods
Study design and patients
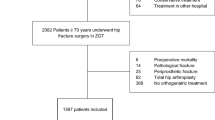
Between April 2008 and October 2013, patients admitted to ZGT were identified for inclusion in this prospective cohort study. Inclusion criteria were hip fracture, aged 70 years and older, and treated in accordance with the integrated orthogeriatric treatment model. Fit patients who were referred to the orthopedic service for total hip replacement because of prefracture suffering from coxarthrosis and those patients with pathological or periprosthetic fractures were excluded, as were the patients who died preoperatively. Informed consent was obtained from all of the individual participants (or a patient proxy). To compare the outcome measures, historical control patients who were managed under standard care in our hospital between October 2002 and March 2008 were used with the same inclusion and exclusion criteria.
Setting
In line with the markers for effective, high-quality, and safe care of the Quality Standard of the Nice Guideline Hip Fractures in Adults, the highlight of the CvGT model is the proactive attitude on preventing patients from adverse events and premature dying, enhancing the quality of life for patients with long-term conditions, helping patients recover following an injury, and ensuring that patients have a positive experience of care in a safe environment [12]. The aim of the introduction of the integrated orthogeriatric treatment model was to prevent complications and loss of function by implementing a proactive approach by means of early geriatric co-management from admission to the emergency department (ED) by following clinical pathways and implementing a multidisciplinary approach. A nurse practitioner or physician’s assistant specialized in trauma surgery made daily visits to the ward under the supervision of a trauma surgeon and geriatrician. For purposes of fall prevention, chronic medication was evaluated, osteoporosis status was investigated, and treatment was started if necessary. A multidisciplinary meeting was held twice a week to discuss the treatment goals, patient progress, and discharge plan. The aim was to have the patients ready for discharge within 5–7 days. Surgery follow-up appointments involved patients attending a multidisciplinary outpatient clinic where they visited a trauma surgeon, physiotherapist, and nurse specialized in osteoporosis (“osteo-physio-trauma outpatient clinic”) (Fig. 1).
Prior to the introduction of the orthogeriatric treatment model, hip fracture patients were treated as “usual” without a standardized multidisciplinary approach, clinical pathway, early geriatric co-management and proactive attitude to prevent complications and loss of function. Various specialties (i.e., internal or pulmonary medicine, cardiology, or urology) were consulted for the management of medical complications as they occurred. Standard data monitoring for quality improvement of the treatment process and research were not used.
Data collection
In the CvGT group, uniform data collection and recordings of all patient data were achieved by a standard evaluation according to the clinical pathway for hip fracture patients. The following patient characteristics were registered at the baseline examination: gender, age, Hospital Safety Management (VMS) frailty score and its separate items (i.e., delirium, prior falling, malnutrition, and physical limitations in activities of daily living [13], previously diagnosed dementia (by a geriatrician/neurologist), American Society of Anesthesiologists Physical Status Classification System (ASA) (classified as 1–2, 3, and 4–5) [14], history of osteoporosis, previous osteoporotic fracture (e.g., wrist, vertebral, or hip fracture), type of fracture, Barthel Index (BI) [15], Parker Mobility Score (PMS) [16], and place of residence. At the baseline examination, comorbidities were scored with the CCI. The CCI categorizes and assigns weights and severities to 19 different patient comorbidities with a predicted 1-year mortality rate for CCI 0 of 12 %, CCI 1–2 of 26 %, CCI 3–4 of 52 %, and CCI 5 or more of 85 % [17].
In line with international guidelines, recommendations, and national quality indicators for the auditing of care [12, 13], the following outcome variables were registered: first, mortality data were checked with the municipal death registry (GBA) and documented in time intervals (i.e., in-hospital mortality, mortality within 30 days, and mortality within 1 year after hip fracture). Furthermore, we registered the length of stay in the ED in minutes, conservative or operative treatment, and type of operation (i.e., osteosynthesis or hemiarthroplasty), time to hip fracture surgery from admission (i.e., within or after 24 h), length of hospital stay in days, and incidence of postoperative surgical and medical (nonsurgical) complications. On discharge, the patients were again scored on the BI and PMS.
For the historical control patients (UC group) data regarding gender, age, type of fracture, ASA score, prefracture living situation, time to surgery, conservative or surgical treatment and type of surgery, and postoperative course complications (if any) were collected retrospectively from the medical records. Mortality data were generated and checked with the GBA. Due to “usual care”, no specific variables for measuring the outcomes of elderly patients with hip fractures were available. See Appendix List of definitions.
Outcomes and statistical analyses
The primary outcome measure was the incidence of 1-year mortality in patients with a hip fracture and identification of associated risk factors. Normally distributed continuous variables were presented as a mean with a standard deviation (SD), not normally distributed continuous variables were presented as a median with an interquartile range (IQR), and categorical variables were presented as a number with a corresponding percentage.
Testing of associations was performed with independent samples T tests or Mann–Whitney U tests as appropriate for continuous variables and by Chi-square tests for between-group comparisons of categorical variables.
To identify a subset of independent variables that were associated with 1-year mortality, a univariate logistic regression analyses was performed. A univariate analysis was performed with gender, age, VMS frailty items (i.e., delirium, falling, physical limitations, and malnutrition), ASA score, dementia, CCI, fracture type, BI score, PMS, and prefracture living situation. The variables with a p value <0.15 were entered in a multivariate logistic regression model. Subsequently, variables with the highest p value were removed step by step until the fit of the model decreased significantly (based on the likelihood ratio test).
One-year mortality rates between the CvGT group and the usual care (UC) group were compared using a Chi-square test. Survival analysis (Kaplan-Meier analysis and Cox proportional hazard regression analysis) were performed to compare the two groups. A p value <0.05 was regarded as being statistically significant. The Statistical Package for the Social Sciences, version 20 (SPSS Inc., Chicago, USA) was used.
Results
Patient characteristics
The baseline characteristics of the CvGT group and the UC group are presented in Table 1. The CvGT patients were older (mean (SD) age 83.0 ± 6.4 years vs. 82.0 ± 6.1 years, p = 0.015), had more severe comorbidities (ASA 3 or higher 78.4 vs. 53.0 %), and had more institutionalized patients in skilled nursing homes prior to admission (15.8 vs. 10.5 %) in comparison with the patients in the UC group.
The majority of patients treated in the CvGT group (97.8 %, n = 831) reported a history of previous falls within 6 months prior to admission. 70.4 % (n = 598) of the CvGT group scored positive on the VMS frailty physical limitations item, 28.4 % (n = 241) scored positive on the VMS frailty delirium item, and 18.9 % (n = 161) scored positive on the VMS frailty malnutrition item. The median (IQR) VMS frailty score was 2.0 (2.0–3.0). In 29.4 % (n = 250) of the CvGT patients, the CCI was 3 or more, and 20.8 % (n = 177) of the patients were suffering from dementia. A total of 12.1 % (n = 103) of the CvGT group had a history of diagnosed osteoporosis, and 15.5 % (n = 132) had experienced a previous osteoporotic fracture. The preoperative median (IQR) BI and PMS were 16.0 (13.0–20.0) and 6.0 (3.0–9.0), respectively (Table 2).
Mortality following hip fracture
In the CvGT group, the 1-year mortality rate was 23.2 % (n = 197) compared to 35.1 % (n = 188) in the UC group (p < 0.001) (Table 1). The survival curve is presented in Fig. 2 (log rank p < 0.001).
The hazard ratio (HR) in the CvGT group compared to the UC group was 0.44 with a 95 % confidence interval (CI) of 0.36–0.54 (p < 0.001), after adjustment for gender, age, ASA score, and prefracture living.
Risk factors for 1-year mortality
In the univariate logistic analysis of the CvGT patients, gender, age, VMS frailty (i.e., delirium, malnutrition, and physical limitations), dementia, ASA score, CCI score, BI, PMS, and prefracture living situation were significantly related to mortality. Multivariate regression analyses revealed that male gender (OR 1.68, 95 % CI 1.13–2.45), increasing age (OR 1.06, 95 % CI 1.02–1.09), higher ASA score (ASA 3 OR 2.43, 95 % CI 1.25–4.74, ASA 4–5, OR 7.05, 95 % CI 3.20–15.52), higher CCI score (CCI 1–2 OR 1.46, 95 % CI 0.83–2.57, CCI 3–4 OR 1.59, 95 % CI 0.85–2.96, CCI 5 OR 2.71, 95 % CI 1.23–5.93), VMS frailty malnutrition (OR 2.01, 95 % CI 1.34–3.02), VMS frailty physical limitations (OR 2.35, 95 % CI 1.32–4.20), and decreasing BI (OR 0.96, 95 % CI 0.92–1.01) were independent risk factors of mortality within 1 year following hip fracture (Table 3). Nagelkerke R 2 was 25 % for this model.
Perioperatively
The treatment details of both patient groups are presented in Table 1. In the CvGT group, 2 % (n = 17) of patients were treated conservatively compared to no patients in the UC group (p < 0.001). Differences between the groups were observed in the use of endoprosthesis (33.6 % in CvGT vs. 26.7 % in UC) and internal fixation for femoral neck fractures (18.6 % in CVGT vs. 25.0 % in UC). Time to surgery was not significantly different between the CvGT group and the UC group (p = 0.259).
Postoperative course and 1-year mortality
A complicated course was found in 53.4 % (n = 454) of the CvGT patients compared to 66.9 % (n = 358) of the patients who were managed with standard care (p < 0.001). We detected a significant association between a complicated course and 1-year mortality in both groups (both p < 0.001). One-year mortality rates in patients with a complicated course were 30.6 % (n = 139) in the CvGT group and 42.2 % (n = 151) in the UC group.
A detailed analysis of complications in the CvGT group revealed that in 454 patients, a total of 788 postoperative complications were diagnosed. Of these complications, 93 % (n = 733) were medical and 7.0 % (n = 55) were surgical. The most common postoperative complications were delirium (24.4 %, n = 207), anemia (16.8 %, n = 143), urinary tract infections (9.8 %, n = 83), pneumonia (8.1 %, n = 69), and heart failure (6.8 %, n = 58) (Table 4).
The patients from the CvGT group were discharged after a median (IQR) length of hospital stay of 8.6 days (5.9–13.2) compared to 10.0 days (7.0–17.0) in the UC group (p < 0.001). In the CvGT group, we observed mean (SD) differences between the preoperative and discharge BI and PMS, which were 5.7 (±3.9) points and 3.3 (±2.4) points, respectively.
Discussion
In the present study, the 1-year mortality rate was 23.2 % in the elderly patients with a hip fracture after integrated orthogeriatric treatment in the CvGT group compared to 35.1 % in the historical control group. We found that integrated orthogeriatric treatment was associated with a reduction in the hospital mortality and long-term mortality rates [10]. These rates were remarkably lower than expected in this vulnerable study population. Relatively few studies have been performed to evaluate the in-hospital mortality and long-term mortality outcomes in elderly hip fracture patients following integrated orthogeriatric treatment in comparison with standard care [18–22]. Our findings are similar to those of Grigoryan et al. [10]
We also found an unfavorable patient profile, which makes the elderly hip fracture patient frailer than the elderly patient without a hip fracture [19, 22, 23]. The concept of frailty is a geriatric syndrome characterized by the age-associated decline in physiological reserve and function across multi-organ systems, leading to increased vulnerability for adverse health outcomes [24]. Frailty has been shown to be a significant predictor of postoperative adverse outcomes in elderly patients [25–28]. Two recent studies have shown that in half of the elderly patients with a hip fracture, frailty, as well as the risk of morbidity, loss of function, and death, increased over time due to the occurrence of frequent falls, osteoporosis, previous osteoporotic fractures, presence of comorbidity, low body mass index, and malnutrition [22, 26]. In our experience, the outcome on the 1-year mortality rate in our study provides a strong argument that elderly patients with a hip fracture require the most optimal possible treatment. Integrated orthogeriatric treatment should be the standard approach with regard to the multidimensional needs of these patients.
Patient characteristics have a great influence on patient outcome [27, 29, 30]. For clinicians, it is relevant to gain insight into the underlying factors that influence the mortality risk following a hip fracture in an attempt to plan effectively for patient care and optimize the quality of care.
Throughout the world, a number of measuring instruments are used for the prognostic scoring of elderly patients with hip fractures who are at risk of adverse outcomes [23]. We identified eight patient characteristics that predict 1-year mortality following hip fracture surgery. The most important risk factors were male gender, increasing age, poor general health (i.e., higher ASA score and CCI of 5 or more), VMS frailty malnutrition and physical limitations, and decreasing BI. However, knowing the risk factors is not the same as having an instrument that is sensitive and specific enough to be useful in clinical practice for stratifying patients. Current models, such as the VMS frailty score, are able to predict the variance in the outcome on a group level; however, these models are not good enough for decisions on an individual level. Perhaps individual prediction is not within reach because of the complexity of the risk factors involved. Because integrated care is not likely to be harmful for anyone, a triage system with good sensitivity and negative predicted value would be the first goal. A future study goal will be to determine the efficacy of a combined triage system with an integrated care pathway.
Due to the recent introduction of the Dutch Health Care Inspectorate’s (IGZ) performance indicator on geriatric co-management in older patients, Dutch policymakers in hospitals and treating professionals are obliged to evaluate and redesign their treatment processes in this area. The introduction of a national database into the healthcare system could make a substantial contribution to this. The most well-known example is Great Britain’s National Hip Fracture Database, where the healthcare system awards suitable remuneration to those hospitals that achieve excellence in the care of hip fractures (i.e., the Best Practice Tariff). Since 2008, the CvGT has been using a database and clinical pathways for process monitoring, quality measurement, and research. Global aging is accelerating, and hip fractures can be expected to increase. Much work is needed to improve the treatment of this vulnerable elderly group. We would like to use our experience with and results from the integrated orthogeriatric treatment model for benchmarking with other hospitals and for national and international research into long-term effectiveness.
Strengths and weaknesses analysis
A strength of this study is that it is the first study in the Netherlands to describe the effectiveness of an integrated orthogeriatric treatment model on 1-year mortality compared to standard care and associated risk factors in elderly patients with a hip fracture. A limitation of study is selection bias because the fittest elderly patients are treated with a total hip prosthesis and are excluded in this series. Overestimating the favorable results would seem unlikely.
Another strength is a good description and analysis of the case mix, such as the VMS frailty scoring system, in relation to 1-year mortality after a hip fracture. In addition, use has been made of specifically defined measuring instruments and outcome measures for the treatment of a representative frail patient population with a follow-up period of 1 year. This means that it can be used for benchmarking and for both national and international research. Points of criticism are the use of data of a historical control group with standard variables instead of a randomized study design. The impact of a hip fracture on the quality of life and the patient perspective were not analyzed. These should be part of future studies. Another research question would be the analysis of the performance of our patients during geriatric rehabilitation in nursing homes following the hip fracture pathway.
Conclusion
After integrated orthogeriatric treatment, a significant decrease was seen in the 1-year mortality rate in frail elderly patients compared to historical control patients treated with standard care. The most important risk factors for 1-year mortality were gender, increasing age, malnutrition, physical limitations, decreasing BI, and medical conditions. Awareness of the risk factors that affect 1-year mortality rate can be useful in an attempt to optimize care and outcomes. Orthogeriatric treatment should be standard for elderly patients with hip fractures due to the multidimensional needs of these patients.
References
Klop C, Welsing PMJ, Leufkens HGM, Elders PJM, Overbeek JA et al (2015) The epidemiology of hip and major osteoporotic fractures in a Dutch population of community-dwelling elderly: implications for the Dutch FRAX® algorithm. PLoS One 10(12), e0143800. doi:10.1371/journal.pone.0143800, eCollection 2015
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733, Epub 2006/09/20
Friedman SM, Mendelson DA (2014) Epidemiology of fragility fractures. Clin Geriatr Med 30(2):175–181, Epub 2014/04/12
Hartholt KA, Oudshoorn C, Zielinski SM et al (2011) The epidemic of hip fractures: are we on the right track? PLoS One 6(7), e22227, Epub 2011/07/30
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20(10):1633–1650, Epub 2009/05/08
Bertram M, Norman R, Kemp L, Vos T (2011) Review of the long-term disability associated with hip fractures. Inj Prev 17(6):365–370, Epub 2011/04/14
Prestmo A, Hagen G, Sletvold O, Helbostad JL, Thingstad P, Taraldsen K et al (2015) Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet (London, England) 385(9978):1623–1633, Epub 2015/02/11
Sabharwal S, Wilson H (2015) Orthogeriatrics in the management of frail older patients with a fragility fracture. Osteoporos Int 26(10):2387–2399
Kammerlander C, Roth T, Friedman SM, Suhm N, Luger TJ, Kammerlander-Knauer U et al (2010) Ortho-geriatric service–a literature review comparing different models. Osteoporosis Int 21(Suppl 4):S637–S646, Epub 2010/11/26
Grigoryan KV, Javedan HMS, Rudolph JLD (2014) Ortho-geriatric care models and outcomes in Hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma 28(3):e49–e55. doi:10.1097/BOT.0b013e3182a5a045
Liem IS, Kammerlander C, Suhm N, Blauth M, Roth T, Gosch M et al (2013) Identifying a standard set of outcome parameters for the evaluation of orthogeriatric co-management for hip fractures. Injury 44(11):1403–1412, Epub 2013/07/25
https://www.nice.org.uk/guidance/cg124. Hip fracture management in adults. Publication date 2011. Accessed 2016, April 09
https://www.vmszorg.nl/themas/kwetsbare-ouderen. Safety Management program Frail elderly scoring system. [webpage] The Hague, 2009. Accessed 2015, December 31
Fitz-Henry J (2011) The ASA, classification and peri-operative risk. Ann R Coll Surg Engl 93(3):185–187, Epub 2011/04/12
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Maryland State Med J 14:61–65
Parker MJ, Palmer CR (1993) A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br Volume 75(5):797–798, Epub 1993/09/01
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383, Epub 1987/01/01
Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J (2005) Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc 53(9):1476–1482, Epub 2005/09/03s
Friedman SM, Mendelson DA, Kates SL, McCann RM (2008) Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc 56(7):1349–1356, Epub 2008/05/28
Khasraghi FA, Christmas C, Lee EJ, Mears SC, Wenz JF Sr (2005) Effectiveness of a multidisciplinary team approach to hip fracture management. J Surg Orthop Adv 4(1):27–31, Epub 2005/03/16
Shyu YI, Liang J, Wu CC, Su JY, Cheng HS, Chou SW et al (2010) Two-year effects of interdisciplinary intervention for hip fracture in older Taiwanese. J Am Geriatr Soc 58(6):1081–1089, Epub 2010/08/21
Auais M, Morin S, Nadeau L, Finch L, Mayo N (2013) Changes in frailty-related characteristics of the hip fracture population and their implications for healthcare services: evidence from Quebec, Canada. Osteoporosis Int 24(10):2713–2724, Epub 2013/06/08
Krishnan M, Beck S, Havelock W, Eeles E, Hubbard RE, Johansen A (2014) Predicting outcome after hip fracture: using a frailty index to integrate comprehensive geriatric assessment results. Age Ageing 43(1):122–126, Epub 2013/07/09
Chen X, Mao G, Leng S (2014) Frailty syndrome: an overview. Clin Interv Aging 9:433–441. doi:10.2147/CIA.S45300
Joseph B, Pandit V, Zangbar P, Kulvatunyou N, Hashmi A, Green DJ et al (2014) Superiority of frailty over age in predicting outcomes among geriatric trauma patients: a prospective analysis. JAMA Surg 149(8):766–772. doi:10.1001/jamasurg.2014.296
Milte R, Crotty M (2014) Musculoskeletal health, frailty and functional decline. Best Pract Res Clin Rheumatol 28(3):395–410. doi:10.1016/j.berh.2014.07.005, Epub 2014 Aug 16
Smith T, Pelpola K, Ball M, Ong A, Myint PK (2014) Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing 43(4):464–471, Epub 2014/06/05
Partridge JS, Harari D, Dhesi JK (2012) Frailty in the older surgical patient: a review. Age Ageing 41(2):142–147, Epub 2012/02/22
Ireland AW, Kelly PJ, Cumming RG (2015) Risk factor profiles for early and delayed mortality after hip fracture: analyses of linked Australian Department of Veterans’ Affairs databases. Injury 46(6):1028–1035, Epub 2015/03/31
Goisser S, Schrader E, Singler K, Bertsch T, Gefeller O, Biber R, et al. Malnutrition according to mini nutritional assessment is associated with severe functional impairment in geriatric patients before and up to 6 months after hip fracture. J Am Med Dir Assoc. 2015. Epub 2015/04/13
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Ellis Folbert states that there has been funding from the Nurse Practitioners Association Research Foundation (OWVS Foundation) for language editing of this manuscript. Ellis Folbert, Han Hegeman, Marloes Vermeer, Marlies Regtuijt, Detlef van der Velde, Henk Jan ten Duis, and Joris Slaets declare that they have no conflict of interest.
Ethical approval
The Medical Ethical Committee of Medisch Spectrum Twente (MST) at Enschede, the Netherlands, declares that this study does not meet the criteria necessary for an assessment by a medical ethical committee according to Dutch law (K15-54).
Appendix
Appendix
Definitions of measuring instruments used
The VMS frailty score was used to screen for frailty on the following items: delirium, falling, physical limitations and malnutrition. Score 0; not frail, maximum score 4; frail on all items.
Preoperative state of health was assessed using the American Society of Anesthesiologists physical status classification system (ASA): ASA 1–2 no or less comorbidity; ASA 3 severe systemic disease requiring medication, limitation of activities; ASA 4 extreme systemic disorder involving a chronic threat to life; ASA 5 extremely ill patient, death expected within 24 h with or without intervention.
We used the Charlson Comorbidity Index (CCI) to estimate the probability of death within 1 year after hip fracture as a reference. This score was first reported in 1987 [16]. The CCI categorizes and assigns weights and severities to 19 different patient comorbidities with a predicted 1-year mortality for CCI 0 of 12 %; CCI 1–2 of 26 %; CCI 3–4 of 52 %; CCI 5 or more of 85 %. At baseline, comorbidities were scored with the CCI and classified in 0, 1–2, 3–4, 5 or >.
The Barthel Index (BI) was used to measure the level of functioning in activities of daily living (ADL): score 0–4 completely dependent on help, 5–9 requires major help, 10–14 requires help but can do a lot independently, 15–19 reasonably to adequately independent, 20 completely independent in ADL.
The Parker Mobility Score (PMS) was used to measure mobility both within and outside the home as well as the ability to undertake activities outdoors. It is a composite score which results in a total score ranging from 0 (unable to mobilize) to 9 (independent).
In this study complications were registered as:
-
1.
Surgical complications; defined as:
-
Superficial site infection: diffuse redness, serous fluid leakage, and no fever. (RIVM, 2014)
-
Deep wound infection; worse than superficial, need for revision.
-
Dislocation of the prosthesis and failure of osteosynthesis: diagnosis confirmed on XR, need for revision.
-
-
2.
Medical complications; defined as:
-
Delirium: based on the Delirium Observation Screening Scale: score above 3, geriatrician diagnosis confirmed in medical record.
-
Anemia: requiring transfusion based on the transfusion guidelines (CBO, 2007)
-
New arrhythmia; in comparison with electrocardiogram at admission, with need for treatment.
-
Cerebrovascular accident; hemiparesis or hemiplegia, a CT cerebrum is performed.
-
Heart failure; clinical presentation, diagnosis confirmed on CXR, started diuretics.
-
Pressure sores; classified as Grade 1 till 4 Braden scale
-
Pulmonary embolism; confirmed with CT-angio.
-
Deep venous thrombosis; confirmed with echo duplex.
-
Myocardial infarction; elektrocardiogram abnormalities suspicious for ischemia and elevated cardiac troponin level.
-
Renal failure; significant decrease GFR in comparison with admission GFR.,
-
Pneumonia; clinical presentation, diagnosis confirmed on CXR, started antibiotics.
-
Urinary retention; retention of 300 mL or more confirmed with bladder scan.
-
Urinary tract infection; urine sediment with positive WBC and nitrite, started antibiotics.
-
Other complications; f.e. phlebitis, n.femoralis paralysis, ileus, electrolyte abnormalities.
-
Rights and permissions
About this article
Cite this article
Folbert, E.C., Hegeman, J.H., Vermeer, M. et al. Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos Int 28, 269–277 (2017). https://doi.org/10.1007/s00198-016-3711-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3711-7