ABSTRACT
BACKGROUND
International medical graduates (IMGs) have substantial representation among primary care physicians in the USA and consistently report lower career satisfaction compared with US medical graduates (USMGs). Low career satisfaction has adverse consequences on physician recruitment and retention.
OBJECTIVE
This study aims to identify factors that may account for or explain lower rates of career satisfaction in IMGs compared with USMGs.
DESIGN
Using data from the 2008 Health Tracking Physician Survey, a nationally representative survey, we examined the association between IMG status and career satisfaction among primary care physicians. We used multivariable logistic regression modeling to adjust for a broad range of potential explanatory factors and physician characteristics.
PARTICIPANTS
The study participants comprise primary care physicians who reported at least 20 h a week of direct patient care activities (N = 1,890).
MAIN MEASURES
The main measures include respondents’ overall satisfaction with their careers in medicine.
KEY RESULTS
IMGs were statistically significantly less likely than USMGs to report career satisfaction (75.7% vs. 82.3%; p = 0.005). This difference persisted after adjusting for physician characteristics and variables describing the practice environment (adjusted odds ratio = 0.62; 95% confidence interval, 0.43–0.90). Pediatricians (vs. internists) and those who earned $200,001–250,000 (vs. <$100,000) or >$250,000 were more likely to report career satisfaction, while solo practitioners and those who reported being unable to provide high-quality patient care were less likely to report career satisfaction.
CONCLUSIONS
After adjusting for a number of variables previously shown to have an impact on career satisfaction, we were unable to identify additional factors that could account for or explain differences in career satisfaction between IMGs and USMGs. In light of the central role of IMGs in primary care, the potential impact of poorer satisfaction among IMGs may be substantial. Improved understanding of the causes of this differential satisfaction is important to appropriately support the primary care physician workforce.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Primary care is a cornerstone for developing a cost-effective, high-quality healthcare system that reduces health disparities.1–3 International medical graduates (IMGs), defined as physicians who did not attend medical school in the USA or Canada, comprise more than a quarter of the primary care physician workforce in the USA.4 The majority of IMGs are primary care physicians and approximately two thirds of IMGs practice in non-urban primary care shortage areas.5 IMGs also provide a substantial proportion of care to vulnerable populations.6
Although IMGs report lower rates of career satisfaction compared with US medical graduates (USMGs),6–9 little is known about factors that may account for this lower satisfaction. Studies have shown that physician specialty,8,10 professional autonomy,7,9,11 and compensation 7–9 are associated with overall physician satisfaction. However, prior studies of career satisfaction have not further examined these factors to determine whether they may explain lower career satisfaction rates among IMGs. Lower rates of career satisfaction among IMGs are concerning given the potential impact on the patients they serve and the health systems in which they provide care. Prior work indicates that dissatisfied physicians report greater intent to leave their current practice12–14 and that high physician turnover can result in disruption of patient care while being costly to physician practices.15 In primary care alone, a shortage of 45,000 physicians is expected by 2020.1 In light of these predicted shortages, issues related to career satisfaction are particularly relevant.
A thorough understanding of career satisfaction is vital for developing effective policies and practices to support and maintain an increasingly diverse physician workforce. Thus, using data from the 2008 Health Tracking Physician Survey (HTPS), we sought to identify factors that may account for lower rates of career satisfaction in IMGs compared with USMGs among primary care physicians.
METHODS
Data Source
We utilized the restricted data set from the 2008 HTPS,16 a nationally representative self-administered mail survey of licensed US physicians providing at least 20 h/week of direct patient care, conducted by the Center for Studying Health System Change. The HTPS sampling frame was drawn from the American Medical Association master file including all active, nonfederal, office-, and hospital-based physicians. The sampling strategy was based on classical stratified random sampling design with proportional allocation.16
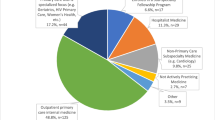
A total of 4,720 physicians completed the 2008 survey with a weighted response rate of 62%. We limited our analysis to physicians who reported that they were primary care providers (internal medicine, family/general practice and pediatrics), which resulted in a final sample of 1,890 physicians.
Dependent Variable: Physician Career Satisfaction
Physicians were asked the following: “Thinking very generally about your satisfaction with your overall career in medicine, would you say that you are currently very dissatisfied, somewhat dissatisfied, neither satisfied nor dissatisfied, somewhat satisfied, or very satisfied?” We created a binary variable for assessing satisfaction, with those answering “somewhat satisfied” or “very satisfied” coded as “satisfied” and those answering “neither satisfied nor dissatisfied”, “somewhat dissatisfied” or “very dissatisfied” coded as “not satisfied”.
Independent Variable
The primary independent variable was IMG status which assessed the country where a physician attended medical school. The survey response choices were: “USA,” “Canada,” “Puerto Rico,” and “Others”. Those responding “USA,” “Canada,” and “Puerto Rico” were classified as USMGs while those responding “Others” were classified as “IMG.”
Covariates
Variables that could potentially explain or account for differences in career satisfaction between IMGs and USMGs were classified into two domains—physician characteristics and practice environment. Specific covariates were selected based on existing literature suggesting that physician specialty,8,10 professional autonomy,7,9,11 and compensation 7–9 are associated with career satisfaction. Additionally, prior work from our group on the workplace experiences of IMGs 17 suggested that factors such as communication difficulties and challenges in navigating healthcare systems may have an impact on career satisfaction. Variables related to these domains were included where available.
Physician characteristics included gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific Islander and others), physician age, specialty (internal medicine, family medicine/general practice, and pediatrics), and board certification in primary specialty (yes/no).
Practice environment variables provided a description of a physician’s practice environment, including their ability to access services for their patients. This included respondents’ reported income from the practice of medicine in the prior year (<$100,000, $100,001–150,000, $150,001–200,000, $200,001–250,000, and ≥$250,001), metropolitan statistical area of practice (large metropolitan (population, ≥1 million) or adjacent, small metropolitan (population, <1 million) or adjacent, and non-metropolitan (population, <250,000 with an average population of approximately 23,800)), whether respondents were solo practitioners (yes/no), the percent of practice revenue from Medicare and Medicaid, and hours spent in medically related activities in the last week. Respondents’ ability to obtain a variety of patient services was assessed through a series of questions with yes/no responses: referrals to high-quality specialists, non-emergency hospital admissions, high-quality outpatient mental health services, and interpreter services for non-English speaking patients. Respondents were asked if they believed they had adequate time to spend with patients during office visits and whether they believed they were able to provide high-quality care to all patients. Responses were characterized as agree (comprising those who agreed somewhat and those who agreed strongly) versus disagree (comprising those who disagreed somewhat and those who disagreed strongly). Finally, respondents were asked whether they had communication difficulties with patients due to language and whether insurance companies rejected their care decisions. Responses were dichotomized as “problem” (comprising those reporting major or minor problems) and “not a problem” (comprising those who did not report problems).
Statistical Analysis
We compared differences in physician characteristics and practice environment variables between IMGs and USMGs using t tests for continuous variables and χ 2 tests for categorical variables. We then used logistic regression to model the unadjusted and adjusted associations between the independent variables and career satisfaction. The logistic regression modeling proceeded in three steps. First, we examined the unadjusted effect of IMG status on the likelihood of career satisfaction. Second, we sequentially added the two groups of independent variables (physician characteristics and practice environment variables) to help identify potential explanatory factors. Finally, all variables included in the final model were tested individually for interactions with IMG status. This allowed us to determine whether the effects of any included variables on career satisfaction differed between IMGs and USMGs.
In order to account for effects arising from unequal probability sampling, differential survey response, stratification and clustering, we used weighting and survey analysis procedures in SAS version 9.2 and SUDAAN.18 Statistical significance was set at α = 0.05.
RESULTS
In Table 1, we present a description of the sample, stratified by IMG status. In total, 24.2% of respondents were IMGs. About half (49.2%) of IMGs in our sample self-identified as Asian or Pacific Islander while the majority (82.2%) of USMGs self-identified as non-Hispanic white. When compared with USMGs, IMGs were older, more likely to report lower income, less likely to report being board certified, more likely to report practicing in large metropolitan areas, more likely to report being solo practitioners and derived a greater percentage of their practice revenue from both Medicare and Medicaid.
IMGs and USMGs did not differ significantly with respect to gender, reported communication difficulties with patients, adequate time to spend with patients, perceived ability to provide high-quality care, insurance rejections of care decisions, hours spent in medically related activities per week, or ability to obtain specialist referrals.
Overall, 80.5% of respondents reported being satisfied with their careers. However, the proportion of physicians reporting satisfaction was significantly lower among IMGs compared with USMGs (75.7% vs. 82.3%, p = 0.005; unadjusted odds ratio (OR) = 0.67; 95% CI, 0.52–0.87). Table 2 presents results for both unadjusted and adjusted models. After adjusting for physician characteristics, IMG status remained significantly associated with lower likelihood of reporting career satisfaction (OR = 0.59; 95% CI, 0.43–0.81). The negative effect of IMG status persisted after additionally controlling for variables related to the practice environment (OR = 0.62; 95% CI, 0.43–0.90).
In the fully adjusted model, pediatricians (vs. internists) (adjusted OR, 1.65; 95% CI, 1.01–2.72) and those whose reported income was $200,001–250,000 (vs. <$100,000) (adjusted OR, 2.68; 95% CI, 1.48–4.85) or ≥$250,001 (adjusted OR, 2.56; 95% CI, 1.39–4.73) were significantly more likely to report career satisfaction. Solo practitioners (adjusted OR, 0.56; 95% CI, 0.40–0.78), those who reported not having adequate time to spend with patients (adjusted OR, 0.36; 95% CI, 0.26–0.48) and those who reported being unable to provide high-quality care to patients (adjusted OR, 0.44; 95% CI, 0.32–0.61) were significantly less likely to report career satisfaction.
Finally, after testing each variable in the fully adjusted model individually for interactions with IMG status, no significant interactions were found.
COMMENT
In this nationally representative sample of primary care physicians, IMGs were less likely than USMGs to report career satisfaction. More importantly, this difference remained even after adjusting for a broad range of potential explanatory factors, including physician characteristics and variables related to the practice environment. Although IMGs and USMGs differed with respect to the distribution of several potential explanatory factors, the lack of significant interactions indicates that none of the variables had a differential effect on career satisfaction based on IMG status.
This study adds to the literature in several important ways. It builds on prior work by including a broad range of explanatory variables, many of which have been associated with career satisfaction in prior studies.7–11 Although the difference in career satisfaction between IMGs and USMGs is modest in this study, it is statistically significant and consistent with findings of previous studies.6,8 This modest but persistent difference is meaningful because IMGs comprise approximately 25% of the total US physician workforce, with an important role in primary care and care for vulnerable populations. In light of the impact of low career satisfaction on physician recruitment, physician retention and patient satisfaction,11–13 systematic persistence of lower career satisfaction among this group of physicians may have negative effects on the health of their patients and the overall health of the communities in which IMGs work. These issues may be of particular consequence when considered in the context of predicted physician shortages, rising healthcare costs, and the growing healthcare needs of an increasingly diverse patient population.
Addition of the race/ethnicity variable to the model had a small but negative confounding effect on the relationship between IMG status and career satisfaction. This finding warrants further exploration. Almost half (49.2%) of IMGs in this sample self-identified as Asian/Pacific Islander, compared with just 6.8% of USMGs. Asian/Pacific Islander physicians were also somewhat more likely to report career satisfaction, though this finding was not statistically significant. Thus, controlling for race/ethnicity had the effect of removing the influence of a large group of physicians who tend to report slightly greater career satisfaction. Although country of origin data are not available in HTPS, more than 25% of IMGs in the USA originate from the Indian sub-continent.19 Two important factors may contribute to their increased career satisfaction. First, most countries in South Asia utilize English as their language of medical education. Therefore, language and perhaps some cultural customs may be less foreign to this group of physicians. Second, given the large numbers and long history of physicians from South Asia, newcomers from this region may be more likely to find existing support networks both formal and informal.20 Future work is needed to evaluate the importance of such support structures and the role they might play in mitigating differences in career satisfaction.
Our findings suggest that additional domains of experience may contribute in important ways to differences in career satisfaction between IMGs and USMGs. These domains, previously explored using qualitative methods,17 may include the impact of discrimination in the workplace, stresses of being an “outsider” and lack of appropriate supportive structures in the workplace. Existing work indicates that IMGs are more likely than USMGs to report experiences of discrimination in the workplace.21 In addition, IMGs have reported both linguistic and cultural barriers to providing patient care.22 Finally, nearly half of IMGs practice primary care,5 although many have previously trained in other specialties and may have had well-established careers in their home countries. This lack of available career opportunities in IMGs’ initial specialty of interest as well as the impact of the change in status from established physician to trainee may have an important effect on career satisfaction. None of these factors is captured in currently available quantitative data, yet they may have an important role in shaping career satisfaction. Future work should seek to elucidate these additional domains, particularly how they affect the relationship between IMG status and career satisfaction.
Our findings should be considered in light of several limitations. First, although the career satisfaction measure in the HTPS survey was derived from a validated career satisfaction measure developed by the Society of General Internal Medicine Career Satisfaction Study Group 23,24 the specific measure used in HTPS/CTS has not been clearly validated. In spite of this limitation, the career satisfaction measure used in HTPS is the same as that used in all seven rounds of the CTS survey, allowing for consistency in career satisfaction assessment across studies. Additionally, both CTS and HTPS data are frequently used, particularly in examining issues related to career satisfaction.6,7,11,25 The Physician Worklife Study 26,27 utilized a 38-item instrument to measure global job, career and specialty satisfaction. This approach, while more complex, also allows for greater nuance in distinguishing the various aspects of satisfaction. Future work may seek to develop and validate a measure for career satisfaction that includes more detail than the single question variable currently used, but is less cumbersome than a 38-item instrument. Second, there are a number of factors that may contribute to career satisfaction that were not measured in this survey. Although this is a limitation of these data, this study did include a broad range of factors previously found to be associated with career satisfaction. Finally, although IMGs are often treated as a homogeneous group, there is great diversity within this group, which often cannot be discerned using survey data. For example, recent work indicates potentially important differences between US citizens who attend medical school abroad (US IMGs) and foreign nationals who are new immigrants to the USA (foreign-born IMGs);28 however, the level of detail in the HTPS did not allow us to distinguish between these groups. Future studies may seek to better understand differences in career satisfaction between US IMGs and foreign-born IMGs.
Despite these limitations, the study has several notable strengths. First, all variables included in the model were chosen based on prior literature in the field,7–11 as well as evidence from our own qualitative study of IMG experiences in the USA.17 Second, we used the most recent nationally representative data source available, and the career satisfaction measure is the same one used in all seven rounds of the CTS and two existing rounds of the HTPS. Finally, although prior work describes differences in career satisfaction between IMGs and USMGs, this is the first study to examine the potential role of a comprehensive set of factors with the explicit objective of trying to explain observed differences.
Given the central role of IMGs in primary care in the US healthcare system, particularly for vulnerable populations, a comprehensive understanding of factors contributing to career satisfaction is important for the development and maintenance of a functional physician workforce that can care for our increasingly diverse patient population. Although significant efforts have been directed to recruiting new individuals into the primary care workforce, the retention of those in whom the US healthcare system has already invested time and resources is also of paramount importance. This will be difficult to achieve without an ability to effectively assess diverse aspects of workplace experiences and their effects on career satisfaction.
References
US Department of Health and Human Services. Healthy people, 2010: understanding and improving health, 2nd Ed. Washington, DC: US Government Printing Office; November 2000.
Starfield B. Primary care in the United States. Int J Health Serv. 1986;16(2):179–198.
Institute of Medicine. Primary care: America’s health in a new era. Washington, DC: Institute of Medicine; 1996.
American Medical Association IMG Section. International medical graduates: contemporary challenges and opportunities. Chicago, IL: American Medical Association; 2010.
Hing E, Lin S. Role of international medical graduates providing office-based medical care: United States, 2005–2006. NCHS Data Brief. Feb 2009(13):1–8.
Morris AL, Phillips RL, Fryer GE, Jr., Green LA, Mullan F. International medical graduates in family medicine in the United States of America: an exploration of professional characteristics and attitudes. Hum Resour Health. 2006;4:17.
Stoddard JJ, Hargraves JL, Reed M, Vratil A. Managed care, professional autonomy, and income: effects on physician career satisfaction. J Gen Intern Med. Oct 2001;16(10):675–684.
Leigh JP, Kravitz RL, Schembri M, Samuels SJ, Mobley S. Physician career satisfaction across specialties. Arch Intern Med. Jul 22 2002;162(14):1577–1584.
Pagan JA, Balasubramanian L, Pauly MV. Physicians’ career satisfaction, quality of care and patients’ trust: the role of community uninsurance. Health Econ Policy Law. Oct 2007;2(Pt 4):347–362.
Leigh JP, Tancredi DJ, Kravitz RL. Physician career satisfaction within specialties. BMC Health Serv Res. 2009;9:166.
Landon BE, Reschovsky J, Blumenthal D. Changes in career satisfaction among primary care and specialist physicians, 1997–2001. Jama. Jan 22–29 2003;289(4):442–449.
Landon BE, Aseltine R, Jr., Shaul JA, Miller Y, Auerbach BA, Cleary PD. Evolving dissatisfaction among primary care physicians. Am J Manag Care. Oct 2002;8(10):890–901.
Landon BE, Reschovsky JD, Pham HH, Blumenthal D. Leaving medicine: the consequences of physician dissatisfaction. Med Care. Mar 2006;44(3):234–242.
Buchbinder SB, Wilson M, Melick CF, Powe NR. Primary care physician job satisfaction and turnover. Am J Manag Care. Jul 2001;7(7):701–713.
Buchbinder SB, Wilson M, Melick CF, Powe NR. Estimates of costs of primary care physician turnover. Am J Manag Care. Nov 1999;5(11):1431–1438.
Association of American Medical Colleges. Physician shortages to worsen without increases in residency training. Chicago, IL: AAMC; 2010.
Chen P, Nunez-Smith M, Bernheim S, Berg D, Gozu A, Curry LA. Professional experiences of international medical graduates in primary care. J Gen Intern Med. 2010;25(9):947–953.
Center for Studying Health System Change. 2008 health tracking physician survey restricted use file: user’s guide. Washington, DC: Center for Studying Health System Change; January 2010 2009.
American Medical Association. International Medical Graduates in American Medicine. American Medical Association; 2010.
American Association of Physicians of Indian Origin. AAPI Clinical Observership Program. http://aapiusa.org/education/observership.aspx. Accessed July 2011.
Baldwin DC, Jr., Daugherty SR, Rowley BD. Racial and ethnic discrimination during residency: results of a national survey. Acad Med. Oct 1994;69(10 Suppl):S19-21.
Fiscella K, Roman-Diaz M, Lue BH, Botelho R, Frankel R. ‘Being a foreigner, I may be punished if I make a small mistake’: assessing transcultural experiences in caring for patients. Fam Pract. Apr 1997;14(2):112–116.
Reed VA, Jernstedt GC, McCormick TR. A longitudinal study of determinants of career satisfaction in medical students. Med Educ Online; 2004;9:11. Available from http://www.med-ed-online.org. Accessed July 2011
Konrad TR, Williams ES, Linzer M, McMurray J, Pathman DE, Gerrity M, Schwartz MD, Scheckler WE, Van Kirk J, Rhodes E and Douglas J, for the Society of General Internal Medicine Career Satisfaction Study Group. Measuring Physician Job Satisfaction in a Changing Workplace and a Challenging Environment. Med Care, 1999; 37(11): 1174–1182.
Forrest CB et al. Managed care, primary care, and the patient-practitioner relationship. J Gen Intern Med, 2002. 17(4): p. 270–7.
Williams ES, Konrad TR, Linzer M, McMurray J, Pathman DE, Gerrity M, Schwartz MD, Scheckler WE, Van Kirk J, Rhodes E, and Douglas J for the SGIM Career Satisfaction Study Group. Refining the measurement of physician job satisfaction: results from the Physician Worklife Survey. Med Care 1999;37:1140–1154.
Linzer M, Konrad TR, Douglas J, McMurray JE, Pathman D, Williams ES, Schwartz MD, Gerrity M, Scheckler W, Bigby JA, and Elnora Rhodes for the Society of General Internal Medicine (SGIM) Career Satisfaction Study Group (CSSG). Managed care, time pressure and physician job satisfaction: results from the Physician Worklife Study. J Gen Intern Med 2000;15:441–450.
Norcini JJ, Boulet JR, Dauphinee WD, Opalek A, Krantz ID, Anderson ST. Evaluating the quality of care provided by gradutes of international medical schools. Health Affairs. 2010;29(8):1461–1468.
Acknowledgments
The authors would like to thank Ellyn Boukus from the Center for Studying Health Systems Change, for invaluable technical assistance throughout this study and Corey Pilver, Ph.D., for statistical assistance. Funding and support were provided by the Agency for Healthcare Research and Quality (T32 HS 017589-02T32) and the Robert Wood Johnson Clinical Scholars Program and the Robert Wood Johnson Foundation. Preliminary data from this manuscript were presented at the 2010 Robert Wood Johnson Foundation Clinical Scholars National Meeting, on November 3rd, 2010 in Atlanta, Georgia, the 2011 Association of American Medical Colleges Workforce Conference on May 5, 2011 in National Harbor, Maryland, and at the 2011 National Research Service Award Trainee Research Conference sponsored by the Agency for Healthcare Research and Quality, on June 11, 2011 in Seattle, Washington.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, P.G., Curry, L.A., Nunez-Smith, M. et al. Career Satisfaction in Primary Care: A Comparison of International and US Medical Graduates. J GEN INTERN MED 27, 147–152 (2012). https://doi.org/10.1007/s11606-011-1832-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1832-4