Abstract
Background
The impact of preoperative chemoradiation on postoperative morbidity and mortality of patients with pancreatic adenocarcinoma remains controversial.
Methods
Consecutive pancreatectomies for adenocarcinoma performed between 2011 and 2015 were prospectively monitored for 90 days by using a previously reported surveillance system to determine the association between preoperative chemoradiation and adverse events, pancreatic fistulae, readmissions, and mortality.
Results
Among 209 consecutive patients who underwent pancreatectomy, 159 (76 %) experienced at least one adverse event within 90 postoperative days. Patients who received preoperative chemoradiation (n = 137, 66 %) were more likely to have borderline resectable/locally advanced tumors, to have received induction chemotherapy, and to require vascular resection at pancreatectomy than those who did not receive chemoradiation (all P < 0.05). Nonetheless, there were no significant differences in the rates of severe complications, readmission, or mortality between these groups (all P > 0.05). Among patients who underwent pancreatoduodenectomy, the rate of pancreatic fistula was similar between those who received chemoradiation and those who did not (P = 0.96). In contrast, those who received chemoradiation prior to distal pancreatectomy had a lower rate of pancreatic fistula (P < 0.01).
Conclusion
Preoperative chemoradiation is not associated with an increase in 90-day morbidity or mortality, and it may reduce the rate of pancreatic fistula following distal pancreatectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For patients with localized pancreatic ductal adenocarcinoma (PDAC), chemoradiation directed at the primary tumor and regional lymph nodes prior to pancreatectomy may enhance the physician’s ability to select patients with the appropriate physiology and tumor biology for major surgery, may sterilize malignant adenopathy and oncologically critical surgical margins, may replace viable cancer cells within the primary tumor with fibrotic tissue, and appears to improve local control relative to a therapeutic strategy that employs surgery first.1–3 Further, it may reduce tumor size or the extent of disease, thereby expanding the number of patients with advanced disease who are eligible for potentially curative surgery.4 For these reasons, the administration of preoperative chemoradiation is increasingly recognized in national treatment guidelines and consensus statements as an acceptable treatment alternative for patients with resectable and borderline resectable PDAC.5–7
Multiple single-arm studies of preoperative chemoradiation have demonstrated that it can be safely delivered to patients with PDAC prior to surgery and that it does not prevent the performance of subsequent pancreatectomy.8,9 Yet, utilization of preoperative chemoradiation remains low in the USA, in part because of persistent concerns that the retroperitoneal fibrosis it induces may cause technical difficulties during surgery and because its effects on wound healing may increase the likelihood of postoperative adverse events (AEs).10–12 Indeed, the potential influence of radiation therapy on subsequent perioperative outcomes after proctectomy,13,14 esophagectomy,15,16 and mastectomy17 remains under active investigation. For patients anticipated to undergo pancreatectomy, several studies have suggested that the administration of preoperative radiotherapy either alone or concurrent with sensitizing doses of chemotherapy (e.g., chemoradiation—as is typically administered to patients with PDAC) may be associated with an increased rate of perioperative morbidity18,19 and mortality.11 Although two other studies have identified similar rates of postoperative morbidity and mortality among patients who received preoperative radiation and those who did not,10,20 these studies had significant shortcomings including the inclusion of small numbers of patients who received preoperative radiation and short durations of follow-up. The impact of preoperative chemoradiation on postoperative morbidity and mortality therefore remains poorly characterized.
At the University of Texas MD Anderson Cancer Center, patients diagnosed with PDAC are routinely treated with chemoradiation prior to anticipated pancreatectomy. All patients who undergo pancreatectomy are prospectively monitored for AEs for at least 90 postoperative days by using a previously reported surveillance system.21 Using data from these patients, we compared rates of 90-day adverse events and mortality between patients who did and did not receive chemoradiation prior to pancreatectomy to detect the potential influence of chemoradiation on postoperative morbidity.
Methods
Patient Population
The Institutional Review Board of the University of Texas MD Anderson Cancer Center (MDACC) approved this study of PDAC patients who underwent a pancreatoduodenectomy (PD), distal pancreatectomy (DP), or total pancreatectomy with or without prior chemoradiation. The institution’s prospectively maintained translational pancreatic tumor database was queried, and all patients who underwent pancreatectomy from July 2011 through March 2015 were included. Perioperative care was delivered in a consistent manner during this contemporary period, and most operations were conducted by three pancreatic surgeons.
Data Collection
Clinical data were prospectively collected and maintained by using standardized algorithms similar to those used in the management of large national data sets.22 The following variables were collected from the institution’s translational pancreatic database, which is managed by trained, full-time personnel. Preoperative variables included age, sex, body mass index (BMI), diabetes mellitus and other comorbidities, radiographic tumor stage, serum total bilirubin, serum albumin, presence of absence of a biliary stent, and specifics about the chemotherapy and radiotherapy received. Pre-existing comorbidities were categorized as 0 (none), 1 (mild), 2 (moderate), or 3 (severe) by using the Adult Comorbidity Evaluation-27 index.23 Operative variables included the type of pancreatectomy, vascular resection, operative time, and estimated blood loss (EBL). We used the MDACC clinical staging system to define potentially resectable, borderline resectable (BR), and locally advanced (LA) PDAC.22
Preoperative Therapy
All management decisions were made by members of our Pancreatic Tumor Study Group. Preoperative chemotherapy, chemoradiation, or both sequentially—a strategy consistent with our previously described bias—were generally favored for all patients with PDAC; pancreatectomy was generally offered de novo only to patients who were perceived to have a favorable physiologic profile, a radiographically resectable tumor, and a normal serum level of CA 19-9.24 In the patients who received preoperative chemoradiation, two primary chemoradiation regimens were used: hypofractionated external beam radiotherapy (EBRT) (30 Gy/10 fractions delivered over 2 weeks) or standard EBRT (50.4 Gy/28 fractions delivered over 5.5 weeks) with concurrent sensitizing doses of 5-fluorouracil, capecitabine, or gemcitabine.3 Computed tomography (CT)-based, three-dimensional conformal treatment planning was routinely used.8,9,25 The primary tumor, pancreatoduodenal, portohepatic, superior mesenteric, and celiac axis lymph nodes were typically included in the treatment volume. Margins were 1 cm for microscopic extension, 5 mm for cranial and caudal respiratory motion, and 5 mm for setup error. To reduce duodenal toxicity, portohepatic nodes were not treated in patients receiving standard EBRT if the likelihood of resection was low. Systemic chemotherapy was administered selectively; when systemic chemotherapy and chemoradiation were sequentially administered prior to surgery, induction chemotherapy was delivered prior to chemoradiation. When necessary, biliary decompression was performed, typically with a metal endobiliary stent, prior to the administration of any preoperative therapy.26
Surgical Procedures
Surgical resection was scheduled 6–8 weeks following completion of chemoradiation. In the patients who had undergone PD, a classic or pylorus-preserving PD was performed, which included a periadventitial dissection of the right lateral aspect of the superior mesenteric artery and a lymphadenectomy of lymphatic stations 8a/p, 12a2/b2/p2/c, 13a/b, 14a/b, and 17a/b.1 Reconstruction was always performed with a pancreaticojejunostomy. The type of reconstruction (duct to mucosa or invagination) and the use of pancreatic duct stents were left to the discretion of the operating surgeon. A DP and splenectomy included a lymphadenectomy of stations 10, 11d, 11p, and 18. Vascular resection with reconstruction was performed when the tumor was inseparable from the vena cava, superior mesenteric vein/portal vein, hepatic artery, or celiac trunk.27,28 When the tumor was adherent to adjacent viscera, an en bloc resection was performed. An operative drain was placed routinely; the amylase content of the effluent was measured after the patient was tolerating enteral nutrition and was removed in the absence of evidence for a postoperative pancreatic fistula (POPF). Somatostatin analogs were not used routinely for POPF prophylaxis.
Adverse Event Reporting
A previously reported, standardized surveillance program was used to detect, grade, and report all perioperative AEs.21 A single trained nurse practitioner actively monitored all patients for at least 90 days following pancreatectomy. All predetermined clinical data needed for accurate severity grading were entered into prospectively developed electronic worksheets. All new and existing AEs and associated supporting documentation were audited with the attending surgeon (M.H.G.K.) in real time on a weekly basis; AEs were categorized, validated, graded for severity, and reported for peer review by using the modified Accordion severity grading system. In addition, the severity of delayed gastric emptying (DGE), post-pancreatectomy hemorrhage (PPH), and POPF were graded according to the International Study Group definitions/classifications by using calculators published online by the Pancreas Club (http://pancreasclub.com/calculators/).29–31 All AEs that occurred after discharge from the index admission were rigorously compiled by actively monitoring follow-up clinics and by calling each patient, including a mandatory communication 6–8 weeks after the date of discharge. Subsequent communication with the patient was carried out during an evolving AE.
Statistical Analysis
We compared clinicopathological variables associated with patients who received preoperative chemoradiation and those who did not. Subgroup analyses were performed for patients who underwent PD and DP. To compare variables between cohorts, we used a Mann-Whitney test for quantitative data and a chi-squared or Fisher exact test for categorical data. To evaluate the potential association between chemoradiation and postoperative outcomes, we constructed a logistic regression model. All of the variables listed above were included in the model; variables with a P value <0.15 on univariate analysis were incorporated into the final multivariate model, and a P value <0.05 was considered statistically significant. All statistical analysis was performed by using SPSS, version 23 (IBM, Armonk, NY).
Results
Patient, Preoperative, and Operative Characteristics
Two-hundred and nine patients underwent a pancreatectomy for PDAC during the study period; 137 (66 %) received chemoradiation prior to surgery and 72 (34 %) did not. Among patients who received chemoradiation, 97 (71 %) received an EBRT dose of 50.4 Gy and 35 (26 %) received 30 Gy (Table 1). Compared to patients who did not receive preoperative chemoradiation, patients who received this treatment were more commonly male, had BR or LA cancers, and had received preoperative systemic chemotherapy (all P < 0.05). They were also more likely to require vascular resection, and their operations were longer and associated with a higher median EBL (all P < 0.05).
Postoperative Morbidity and Mortality
One hundred and fifty-nine (76 %) patients experienced at least one AE within 90 postoperative days (Table 2). The rates of all AEs, severe AE (grade 3–5 complications), DGE, PPH, intra-abdominal abscess (IAA), and wound infection among patients who received chemoradiation preoperatively were similar to those who did not (all P > 0.05). However, patients who did receive chemoradiation were less likely to develop a POPF (P < 0.02 for all grades; P < 0.05 for grade B/C). The median length of stay (LOS) (10 days) and 90-day readmission rate (22 %) were no different between the groups. There were no deaths within 90 days of surgery. Furthermore, there was no difference in the rate of overall complications (P = 0.37), severe complications (P = 0.72), or POPF (P = 0.95) between patients who received 30 and 50 Gy of EBRT (data not shown).
Operative Subgroups
Clinicopathologic details of patients who underwent PD and DP are presented in Tables 3 and 4, respectively. Preoperative chemoradiation was administered to 109 patients (67 %) who underwent PD and 25 patients (60 %) who underwent DP. In both subgroups, patients who received chemoradiation were more likely to have BR or LA cancers and to have received systemic chemotherapy than those who did not (P < 0.05). Moreover, at pancreatectomy, patients who received chemoradiation required vascular resection more frequently, had longer median operative times, and had higher median estimated blood loss (all P < 0.05). In both groups, no difference was observed in the rates of AEs, severe AEs, DGE, PPH, IAA, wound infection, LOS, or 90-day readmission between patients who did or did not receive preoperative chemoradiation (all P < 0.05). However, patients who received chemoradiation prior to DP had a lower overall rate of POPF (P < 0.001) and grade B/C POPF (P = 0.01) than patients who did not.
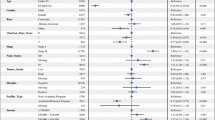
Multivariate Analysis
In a multivariate linear regression analysis of clinical variables, preoperative chemoradiation was not independently associated with the rates of AEs, severe AEs, POPF, or 90-day readmission (data not shown). PD and total pancreatectomy were associated with an increased risk of any AE within 90 days compared with DP (hazard ratio = 2.48, P = 0.04). Moderate/severe comorbidity was associated with an increased rate of POPF compared with less severe comorbidity (hazard ratio = 2.67, P = 0.04). No variables were independently associated with severe AEs or 90-day readmission.
Discussion
In this study, patients who received chemoradiation prior to pancreatectomy had a similar incidence of postoperative AEs, severe AEs, hospital readmissions, and mortality within 90 days as patients who did not. These data suggest that avoiding preoperative irradiation of the surgical field due to fears of postoperative complications is not justified. Our results, combined with existing evidence that preoperative chemoradiation may sterilize regional lymph nodes and soft tissue margins, improve rates of histopathologic response, improve local control following pancreatectomy, and support the use of chemoradiation prior to pancreatectomy in selected patients with PDAC.1–3
Because of our detailed AE surveillance system, the AEs described here include relatively minor—but nonetheless clinically significant—events that might have been missed had data for this analysis come from a retrospective examination of standard clinical documentation. Further, our AE reporting system included AEs that occurred later than 30 days following surgery, which account for up to one third of all postoperative morbidities. These events are not captured by many analyses, including those utilizing data from the National Surgical Quality Improvement Program (NSQIP) database.21,32 Therefore, this study accurately characterizes the significant postoperative morbidity that can be expected following pancreatectomy, whether or not it is preceded by chemoradiation.
In this study, we found similar rates of perioperative morbidity among patients who received chemoradiation prior to pancreatectomy and those who did not. Several prior studies contradict these findings and suggest that preoperative chemoradiation may lead to adverse events or even death following surgery.11,18,19 Our findings do support the conclusions of two other studies, but they have important shortcomings. Specifically, although no difference in 30-day morbidity was noted between patients who did and did not receive preoperative radiation in a recent retrospective analysis of the NSQIP pancreas-specific database conducted by Cooper et al., only a small fraction—100 (6.4 %) of the 1562 patients analyzed in the study—received preoperative radiation of any type.10 And, although a prospective, multiinstitutional, European trial that randomized patients with resectable PDAC either to pancreatectomy alone or to EBRT with concurrent gemcitabine and cisplatin followed by pancreatectomy did not detect a difference in AEs between the two treatment arms, that study was powered to detect overall survival, not morbidity. More importantly, the study was closed to accrual well in advance of meeting its accrual target—only 66 evaluable of 254 planned patients enrolled prior to termination, among whom only 29 received chemoradiation.33 Our study therefore provides additional, important, and timely support for the safety of preoperative chemoradiation, particularly as recent national guidelines assert that preoperative therapy represents an acceptable approach for at least some patients with localized PDAC.6
The fact that we could detect no increase in morbidity in association with preoperative chemoradiation is particularly noteworthy because patients who received chemoradiation presented with relatively anatomically advanced (BR or LA) tumors that required more complex operations to remove (e.g., an increased rate of vascular resection). It is possible that the additional time prior to surgery for patients who underwent chemoradiotherapy is one factor underlying this apparent discrepancy. At the University of Texas MD Anderson Cancer Center, we use the period prior to surgery not only to deliver chemotherapy and/or chemoradiation but also to optimize each patient’s physiologic profile, nutritional status, and treatment for comorbidities. Indeed, patients regularly undergo aggressive optimization of their physiologic and nutritional status under the direction of nutritionists and rehabilitation physicians, a process now undergoing formal evaluation as part of a clinical trial.34 The consequent selection of relatively robust patients who may be particularly tolerant of surgery’s physiologic insults may favorably impact the rate of postoperative morbidity following preoperative therapy.
The fact that the rates of morbidity were similar between groups despite the difference in the magnitude of their associated operations may be further explained by the effect of preoperative chemoradiation on POPF development.35 Patients who develop a POPF are at risk for postoperative infection, hemorrhage, organ failure, readmission, and death.36–41 In our study—and in others—patients who received preoperative chemoradiation had lower rates of both overall POPF and grade B/C POPF than patients who did not, a finding likely attributed to both glandular fibrosis and a decrease in exocrine secretion observed in response to radiotherapy.10,35,42 On subgroup analysis, a difference in the rate of POPF was only observed among patients who underwent DP—not PD. It is quite possible, however, that the absence of a demonstrated protective effect following PD may reflect a type II error related to a low event rate—all patients had the diagnosis of PDAC, and their glands presumably had a dilated pancreatic duct and firm texture. These clinical features would translate into a negligible or low risk of a POPF following PD, irrespective of prior irradiation.43
Although there does not appear to be any association between preoperative chemoradiation and postoperative AEs, many clinicodemographic factors predict morbidity following pancreatectomy. For example, in a randomized, controlled trial comparing pancreaticojejunostomy to pancreaticogastrostomy during PD, Figueras et al.44 found that older age, estimated blood loss >650 ml, POPF, and pancreatic duct size ≤3 mm were associated with severe postoperative complications. In a retrospective review, Baker et al.45 reported that a low BMI, chronic obstructive pulmonary disease, congestive heart failure, neoadjuvant therapy, pylorus preservation, operative time >8 h, and EBL >1.5 L were all associated with grade III–V complications following PD. Using the NSQIP pancreas-specific database, Cooper et al.10 found that older age, lower serum albumin levels, African American race, obesity, chronic obstructive pulmonary disease, biliary stent, vascular resection, soft or unknown gland texture, and total pancreatectomy were associated with postoperative complications. Following DP, predictors of morbidity are similar. In an analysis of the NSQIP database, Kelly et al.46 found that male sex, obesity, neurologic disorders, chronic steroid use, preoperative sepsis, hypoalbuminemia, elevated creatinine, and thrombocytosis predicted 30-day morbidity, and that esophageal varices, neurologic disorders, partially or totally dependent functional status, and high alkaline phosphatase and BUN levels predicted 30-day mortality. In the present study, resection of the pancreatic head with PD or total pancreatectomy was the only factor independently associated with postoperative AEs, and a moderate/severe comorbidity profile was the only factor independently associated with POPF.
Two points regarding the administration of preoperative chemoradiation to patients in this study should be emphasized. First, our center has held a well-reported bias toward this treatment strategy for the past two decades, and we routinely deliver chemoradiation to patients with localized cancer both on and off protocol. Indeed, 137 (66 %) of the 209 patients who underwent pancreatectomy for PDAC received preoperative chemoradiation. In contrast, only 100 (6.4 %) of 1562 patients treated at 43 different hospitals and reported in the NSQIP pancreas-specific database received this treatment.10 Whether the results achieved at MDACC are reproducible in centers with surgeons less experienced in operating following irradiation of the surgical field is unclear. Second, all patients in this study who received chemoradiation did so as the last step of a defined, multidisciplinary treatment program, and all of them underwent a comprehensive staging evaluation 6–8 weeks thereafter in anticipation of pancreatectomy. Given that the administration of preoperative chemoradiation to patients with resectable PDAC remains uncommon nationwide, prior studies that evaluated AEs secondary to chemoradiation followed by pancreatectomy likely included patients with cancers that were initially deemed unresectable, who were treated with palliative intent, and who were subsequently evaluated by a surgeon following a prolonged (and probably unexpected) progression-free interval. To the extent that radiation-induced fibrosis increases over time,2,47 such operations might be associated with increased technical difficulties and possibly AEs.
Our study has additional limitations, foremost among them being its single institution, retrospective design. However, all data concerning AEs were collected prospectively by using the standardized protocol described. Second, patients in this analysis received one of only two primary chemoradiation strategies. Several novel approaches, such as stereotactic body radiation therapy (SBRT), have been developed, and experience with these techniques is increasing.48,49 Whether or not these new strategies would be associated with similar results is unclear. Next, several different regimens of neoadjuvant chemotherapy were used in this cohort of patients, which could potentially introduce bias. However, all patients were treated by using standardized, contemporary perioperative algorithms by a consistent team of surgeons, and overall, the analysis herein of the effects of preoperative adverse events on postoperative outcomes represents the largest and most robust to date. Finally, because our goal was to evaluate perioperative morbidity and mortality, we actively surveyed complications only in the postoperative period. AEs that occurred during chemoradiation were not captured, although we have previously described that these regimens are well-tolerated in prospective clinical trials and that AEs that occur during chemoradiation administration do not prevent subsequent pancreatectomy.8,9,50
Conclusion
In conclusion, the fear of increasing postoperative complications with the administration of preoperative chemoradiation appears unfounded. Rates of 90-day postoperative morbidity and mortality in this study were similar between groups of patients who did and did not receive chemoradiation prior to pancreatectomy, even though patients who received chemoradiation were more likely to have BR or LA tumors, which required more extensive operations to remove. Preoperative chemoradiation also appears to reduce the rate of POPF following DP.
References
Katz MH, Wang H, Balachandran A, Bhosale P, Crane CH, Wang X, Pisters PW, Lee JE, Vauthey JN, Abdalla EK et al: Effect of neoadjuvant chemoradiation and surgical technique on recurrence of localized pancreatic cancer. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract 2012, 16(1):68-78; discussion 78-69.
Chen KT, Devarajan K, Milestone BN, Cooper HS, Denlinger C, Cohen SJ, Meyer JE, Hoffman JP: Neoadjuvant chemoradiation and duration of chemotherapy before surgical resection for pancreatic cancer: does time interval between radiotherapy and surgery matter? Annals of surgical oncology 2014, 21(2):662-669.
Cloyd JM, Crane CH, Koay EJ, Das P, Krishnan S, Prakash L, Snyder RA, Varadhachary GR, Wolff RA, Javle M et al: Impact of hypofractionated and standard fractionated chemoradiation before pancreatoduodenectomy for pancreatic ductal adenocarcinoma. Cancer 2016, 122(17):2671-2679.
Gillen S, Schuster T, Meyer Zum Buschenfelde C, Friess H, Kleeff J: Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS medicine 2010, 7(4):e1000267.
Tempero MA, Malafa MP, Behrman SW, Benson AB, 3rd, Casper ES, Chiorean EG, Chung V, Cohen SJ, Czito B, Engebretson A et al: Pancreatic adenocarcinoma, version 2.2014: featured updates to the NCCN guidelines. Journal of the National Comprehensive Cancer Network: JNCCN 2014, 12(8):1083-1093.
Khorana AA, Mangu PB, Berlin J, Engebretson A, Hong TS, Maitra A, Mohile SG, Mumber M, Schulick R, Shapiro M et al: Potentially Curable Pancreatic Cancer: American Society of Clinical Oncology Clinical Practice Guideline. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2016, 34(21):2541-2556.
Abrams RA, Lowy AM, O’Reilly EM, Wolff RA, Picozzi VJ, Pisters PW: Combined modality treatment of resectable and borderline resectable pancreas cancer: expert consensus statement. Annals of surgical oncology 2009, 16(7):1751-1756.
Evans DB, Varadhachary GR, Crane CH, Sun CC, Lee JE, Pisters PW, Vauthey JN, Wang H, Cleary KR, Staerkel GA et al: Preoperative gemcitabine-based chemoradiation for patients with resectable adenocarcinoma of the pancreatic head. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2008, 26(21):3496-3502.
Varadhachary GR, Wolff RA, Crane CH, Sun CC, Lee JE, Pisters PW, Vauthey JN, Abdalla E, Wang H, Staerkel GA et al: Preoperative gemcitabine and cisplatin followed by gemcitabine-based chemoradiation for resectable adenocarcinoma of the pancreatic head. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 2008, 26(21):3487-3495.
Cooper AB, Parmar AD, Riall TS, Hall BL, Katz MH, Aloia TA, Pitt HA: Does the use of neoadjuvant therapy for pancreatic adenocarcinoma increase postoperative morbidity and mortality rates? Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2015, 19(1):80-86; discussion 86-87.
Laurence JM, Tran PD, Morarji K, Eslick GD, Lam VW, Sandroussi C: A systematic review and meta-analysis of survival and surgical outcomes following neoadjuvant chemoradiotherapy for pancreatic cancer. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2011, 15(11):2059-2069.
Sasson AR, Wetherington RW, Hoffman JP, Ross EA, Cooper H, Meropol NJ, Freedman G, Pingpank JF, Eisenberg BL: Neoadjuvant chemoradiotherapy for adenocarcinoma of the pancreas: analysis of histopathology and outcome. International journal of gastrointestinal cancer 2003, 34(2-3):121-128.
Holubar SD, Brickman RK, Greaves SW, Ivatury SJ: Neoadjuvant Radiotherapy: A Risk Factor for Short-Term Wound Complications after Radical Resection for Rectal Cancer? Journal of the American College of Surgeons 2016, 223(2):291-298.
Milgrom SA, Goodman KA, Nash GM, Paty PB, Guillem JG, Temple LK, Weiser MR, Garcia-Aguilar J: Neoadjuvant radiation therapy prior to total mesorectal excision for rectal cancer is not associated with postoperative complications using current techniques. Annals of surgical oncology 2014, 21(7):2295-2302.
Juloori A, Tucker SL, Komaki R, Liao Z, Correa AM, Swisher SG, Hofstetter WL, Lin SH: Influence of preoperative radiation field on postoperative leak rates in esophageal cancer patients after trimodality therapy. Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer 2014, 9(4):534-540.
Takahata R, Ono S, Tsujimoto H, Hiraki S, Aosasa S, Yamamoto J, Hase K: Preoperative chemoradiation therapy for esophageal cancer is a risk factor for the elevation of high mobility group box-1, leading to an increase in postoperative severe pulmonary complications. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus/ISDE 2016, 29(1):70-78.
Mukai H, Watanabe T, Mitsumori M, Tsuda H, Nakamura S, Masuda N, Yamamoto N, Shibata T, Sato A, Iwata H et al: Final results of a safety and efficacy trial of preoperative sequential chemoradiation therapy for the nonsurgical treatment of early breast cancer: Japan Clinical Oncology Group Study JCOG0306. Oncology 2013, 85(6):336-341.
Allendorf JD, Lauerman M, Bill A, DiGiorgi M, Goetz N, Vakiani E, Remotti H, Schrope B, Sherman W, Hall M et al: Neoadjuvant chemotherapy and radiation for patients with locally unresectable pancreatic adenocarcinoma: feasibility, efficacy, and survival. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2008, 12(1):91-100.
Vento P, Mustonen H, Joensuu T, Karkkainen P, Kivilaakso E, Kiviluoto T: Impact of preoperative chemoradiotherapy on survival in patients with resectable pancreatic cancer. World journal of gastroenterology 2007, 13(21):2945-2951.
Araujo RL, Gaujoux S, Huguet F, Gonen M, D’Angelica MI, DeMatteo RP, Fong Y, Kingham TP, Jarnagin WR, Goodman KA et al: Does pre-operative chemoradiation for initially unresectable or borderline resectable pancreatic adenocarcinoma increase post-operative morbidity? A case-matched analysis. HPB : the official journal of the International Hepato Pancreato Biliary Association 2013, 15(8):574-580.
Schwarz L, Bruno M, Parker NH, Prakash L, Mise Y, Lee JE, Vauthey JN, Aloia TA, Conrad C, Fleming JB et al: Active Surveillance for Adverse Events Within 90 Days: The Standard for Reporting Surgical Outcomes After Pancreatectomy. Annals of surgical oncology 2015, 22(11):3522-3529.
Katz MH, Pisters PW, Evans DB, Sun CC, Lee JE, Fleming JB, Vauthey JN, Abdalla EK, Crane CH, Wolff RA et al: Borderline resectable pancreatic cancer: the importance of this emerging stage of disease. Journal of the American College of Surgeons 2008, 206(5):833-846; discussion 846-838.
Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL, Jr.: Prognostic importance of comorbidity in a hospital-based cancer registry. Jama 2004, 291(20):2441-2447.
Tzeng CW, Fleming JB, Lee JE, Xiao L, Pisters PW, Vauthey JN, Abdalla EK, Wolff RA, Varadhachary GR, Fogelman DR et al: Defined clinical classifications are associated with outcome of patients with anatomically resectable pancreatic adenocarcinoma treated with neoadjuvant therapy. Annals of surgical oncology 2012, 19(6):2045-2053.
25. Cloyd JM CC, Koay EJ, Das P, Krishnan S, Prakash L, Snyder RA, Varadhachary GR, Wolff RA, Javle M, Shroff RT, Fogelman D, Overman M, Wang H, Lee JE, Fleming JB, Katz MHG: Impact of hypofractionated and standard fractionated chemoradiation prior to pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. Cancer 2016.
Pisters PW, Hudec WA, Hess KR, Lee JE, Vauthey JN, Lahoti S, Raijman I, Evans DB: Effect of preoperative biliary decompression on pancreaticoduodenectomy-associated morbidity in 300 consecutive patients. Annals of surgery 2001, 234(1):47-55.
Tseng JF, Raut CP, Lee JE, Pisters PW, Vauthey JN, Abdalla EK, Gomez HF, Sun CC, Crane CH, Wolff RA et al: Pancreaticoduodenectomy with vascular resection: margin status and survival duration. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2004, 8(8):935-949; discussion 949-950.
Katz MH, Lee JE, Pisters PW, Skoracki R, Tamm E, Fleming JB: Retroperitoneal dissection in patients with borderline resectable pancreatic cancer: operative principles and techniques. Journal of the American College of Surgeons 2012, 215(2):e11-18.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW et al: Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007, 142(5):761-768.
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG et al: Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 2007, 142(1):20-25.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M et al: Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005, 138(1):8-13.
Swanson RS, Pezzi CM, Mallin K, Loomis AM, Winchester DP: The 90-day mortality after pancreatectomy for cancer is double the 30-day mortality: more than 20,000 resections from the national cancer data base. Annals of surgical oncology 2014, 21(13):4059-4067.
Golcher H, Brunner TB, Witzigmann H, Marti L, Bechstein WO, Bruns C, Jungnickel H, Schreiber S, Grabenbauer GG, Meyer T et al: Neoadjuvant chemoradiation therapy with gemcitabine/cisplatin and surgery versus immediate surgery in resectable pancreatic cancer: results of the first prospective randomized phase II trial. Strahlentherapie und Onkologie : Organ der Deutschen Rontgengesellschaft [et al] 2015, 191(1):7-16.
Preoperative rehabilitation during neoadjuvant therapy for pancreatic cancer: ClinicalTrials.gov Identifier NCT02295956 [https://clinicaltrials.gov/ct2/show/NCT02295956?term=katz+and+prehabilitation&rank=1]
Lowy AM, Lee JE, Pisters PW, Davidson BS, Fenoglio CJ, Stanford P, Jinnah R, Evans DB: Prospective, randomized trial of octreotide to prevent pancreatic fistula after pancreaticoduodenectomy for malignant disease. Annals of surgery 1997, 226(5):632-641.
36. Vollmer CM, Jr., Sanchez N, Gondek S, McAuliffe J, Kent TS, Christein JD, Callery MP, Pancreatic Surgery Mortality Study G: A root-cause analysis of mortality following major pancreatectomy. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2012, 16(1):89-102; discussion 102-103.
Denbo JW, Orr WS, Zarzaur BL, Behrman SW: Toward defining grade C pancreatic fistula following pancreaticoduodenectomy: incidence, risk factors, management and outcome. HPB : the official journal of the International Hepato Pancreato Biliary Association 2012, 14(9):589-593.
38. Reid-Lombardo KM, Farnell MB, Crippa S, Barnett M, Maupin G, Bassi C, Traverso LW, Pancreatic Anastomotic Leak Study G: Pancreatic anastomotic leakage after pancreaticoduodenectomy in 1,507 patients: a report from the Pancreatic Anastomotic Leak Study Group. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2007, 11(11):1451-1458; discussion 1459.
Wellner UF, Kulemann B, Lapshyn H, Hoeppner J, Sick O, Makowiec F, Bausch D, Hopt UT, Keck T: Postpancreatectomy hemorrhage--incidence, treatment, and risk factors in over 1,000 pancreatic resections. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2014, 18(3):464-475.
McMillan MT, Christein JD, Callery MP, Behrman SW, Drebin JA, Hollis RH, Kent TS, Miller BC, Sprys MH, Watkins AA et al: Comparing the burden of pancreatic fistulas after pancreatoduodenectomy and distal pancreatectomy. Surgery 2016, 159(4):1013-1022.
Fong ZV, Ferrone CR, Thayer SP, Wargo JA, Sahora K, Seefeld KJ, Warshaw AL, Lillemoe KD, Hutter MM, Fernandez-Del Castillo C: Understanding hospital readmissions after pancreaticoduodenectomy: can we prevent them?: a 10-year contemporary experience with 1,173 patients at the Massachusetts General Hospital. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2014, 18(1):137-144; discussion 144-135.
Takahashi H, Ogawa H, Ohigashi H, Gotoh K, Yamada T, Ohue M, Miyashiro I, Noura S, Kishi K, Motoori M et al: Preoperative chemoradiation reduces the risk of pancreatic fistula after distal pancreatectomy for pancreatic adenocarcinoma. Surgery 2011, 150(3):547-556.
Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM, Jr.: A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. Journal of the American College of Surgeons 2013, 216(1):1-14.
Figueras J, Sabater L, Planellas P, Munoz-Forner E, Lopez-Ben S, Falgueras L, Sala-Palau C, Albiol M, Ortega-Serrano J, Castro-Gutierrez E: Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy on the rate and severity of pancreatic fistula after pancreaticoduodenectomy. The British journal of surgery 2013, 100(12):1597-1605.
Baker MS, Sherman KL, Stocker SJ, Hayman AV, Bentrem DJ, Prinz RA, Talamonti MS: Using a modification of the Clavien-Dindo system accounting for readmissions and multiple interventions: defining quality for pancreaticoduodenectomy. Journal of surgical oncology 2014, 110(4):400-406.
Kelly KJ, Greenblatt DY, Wan Y, Rettammel RJ, Winslow E, Cho CS, Weber SM: Risk stratification for distal pancreatectomy utilizing ACS-NSQIP: preoperative factors predict morbidity and mortality. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2011, 15(2):250-259, discussion 259-261.
White RR, Hurwitz HI, Morse MA, Lee C, Anscher MS, Paulson EK, Gottfried MR, Baillie J, Branch MS, Jowell PS et al: Neoadjuvant chemoradiation for localized adenocarcinoma of the pancreas. Annals of surgical oncology 2001, 8(10):758-765.
Mellon EA, Hoffe SE, Springett GM, Frakes JM, Strom TJ, Hodul PJ, Malafa MP, Chuong MD, Shridhar R: Long-term outcomes of induction chemotherapy and neoadjuvant stereotactic body radiotherapy for borderline resectable and locally advanced pancreatic adenocarcinoma. Acta oncologica 2015, 54(7):979-985.
Polistina F, Costantin G, Casamassima F, Francescon P, Guglielmi R, Panizzoni G, Febbraro A, Ambrosino G: Unresectable locally advanced pancreatic cancer: a multimodal treatment using neoadjuvant chemoradiotherapy (gemcitabine plus stereotactic radiosurgery) and subsequent surgical exploration. Annals of surgical oncology 2010, 17(8):2092-2101.
Das P, Wolff RA, Abbruzzese JL, Varadhachary GR, Evans DB, Vauthey JN, Baschnagel A, Delclos ME, Krishnan S, Janjan NA et al: Concurrent capecitabine and upper abdominal radiation therapy is well tolerated. Radiation oncology 2006, 1:41.
Acknowledgments
We thank Ashish Verma, Mano Sundar, and the Translational Pancreatic Tumor Database at the MDACC Department of Surgery. This study was supported by the Various Donor Pancreatic Research Fund at The University of Texas MD Anderson Cancer Center. The University of Texas MD Anderson Cancer Center is supported by the National Institutes of Health through Cancer Center Support Grant P30CA016672.
Authors’ Contributions
All authors/coauthors contributed significantly to the manuscript and fulfilled the requirements for authorship as per the guidelines of the International Committee of Medical Journal Editors (ICMJE).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Denbo, J.W., Bruno, M.L., Cloyd, J.M. et al. Preoperative Chemoradiation for Pancreatic Adenocarcinoma Does Not Increase 90-Day Postoperative Morbidity or Mortality. J Gastrointest Surg 20, 1975–1985 (2016). https://doi.org/10.1007/s11605-016-3286-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3286-9