Abstract
Purpose
Preoperative chemoradiotherapy (CRT) is a novel, emerging treatment strategy for pancreatic ductal adenocarcinoma (PDAC), but it remains unclear whether post-surgery adjuvant chemotherapy is feasible following preoperative CRT. This retrospective study evaluates the feasibility of adjuvant therapy after preoperative CRT.
Methods
The subjects of this study were 99 consecutive patients who underwent pancreatectomy for PDAC between January, 2007 and February, 2013 in our hospital. Sixty patients received preoperative CRT: as gemcitabine (GEM) and 40 Gy radiation in 28 (G-CRT group), and as GEM, S-1, and 50.4 Gy radiation in 32 (GS-CRT group). We also evaluated 39 patients who underwent surgery alone (SA group). We investigated adjuvant chemotherapy induction and completion rates and the frequency of adverse events rated ≥grade 3, based on Common Terminology Criteria for Adverse Events (version 4.0) in all three groups.
Results
In the G-CRT, GS-CRT, and SA groups, the induction rates were 78 % (22/28), 78 % (25/32), and 72 % (28/39), respectively; completion rates were 86 % (19/22), 88 % (22/25), and 82 % (23/28), respectively; and adverse event frequencies were 36 % (8/22), 28 % (7/25), and 43 % (12/28), respectively. No significant difference was found among the three groups.
Conclusion
Preoperative CRT was demonstrated to be safe and did not compromise the feasibility of adjuvant chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic ductal adenocarcinoma (PDAC) is a lethal disease with a 5-year survival rate of about 6 % [1]. Surgical resection is the only curative treatment, but this is feasible in only 13–20 % of patients. Even when the tumor is completely resected, patients with PDAC have a 5-year survival rate of just 5–20 %. In fact, the median overall survival (OS) after pancreatectomy alone is around 20 months [2, 3]. A recent study showed that the administration of adjuvant chemotherapy following curative resection significantly prolonged both disease-free survival (DFS, +6.7 months) and the 5-year OS rate (20.7 vs. 10.4 %), compared with observation alone [3]. Thus, further development of multidisciplinary treatments is needed urgently.
Preoperative chemoradiotherapy (CRT) has been found to improve the prognosis of patients with PDAC [4–7]. In 2008, Evans et al. [8] reported a median survival time of 34 months for patients with resectable PDAC, who received preoperative CRT. Recent systematic reviews have suggested that preoperative CRT could expand the population of PDAC patients who are eligible to undergo curative surgery [9, 10]. Although preoperative CRT can improve the prognosis of patients with PDAC and expand the indications for curative surgery, there is concern that it may adversely affect the feasibility of adjuvant chemotherapy or the perioperative clinical course, due to accumulation of its toxicity. To address these clinical concerns, we evaluated the feasibility of adjuvant therapy and the perioperative clinical course, in terms of perioperative morbidity, rates of adjuvant therapy induction and completion, and frequency of adverse events during adjuvant therapy, after preoperative CRT.
Methods
Study setting
This study was performed at Osaka University Hospital, Japan, and approved by the local ethics committee (no. 15149).
Patients
The subjects of this retrospective study were 99 consecutive patients with PDAC who underwent pancreatectomy between January, 2007 and February, 2013, in our hospital. Cytological and/or histological evidence of PDAC was confirmed before treatment and all patients provided written informed consent for participation in this study. Patients with resectable PDAC were divided into three groups according to the treatments they received: The G-CRT group (n = 28) received gemcitabine (GEM, 800 mg/m2) and 40 Gy radiation; the GS-CRT group (n = 32) received GEM (600–1000 mg/m2), S-1 (40–80 mg/m2), and 50.4 Gy radiation; and the SA group (n = 39) underwent surgery alone. In the early part of this retrospective investigation period (2007–2009), we focused on recruiting patients with advanced PDAC for preoperative chemoradiation therapy (CRT), and we used G-CRT in this era. We then began to recommend a set of treatments: GS-CRT plus curative resection following adjuvant chemotherapy, for patients even in the early stages because our early study showed a better prognosis with these approaches [8]. In this retrospective investigation, tumors were deemed resectable when they met the following criteria: no distant metastasis; no tumor extension to the hepatic artery, celiac axis, or superior mesenteric artery (SMA); no tumor that extended to the splenic artery unless it was resected with a distal pancreatectomy and a splenic artery resection; no venous involvement, or limited involvement of the superior mesenteric vein (SMV)/portal vein (PV) or inferior vena cava (IVC), which allowed safe resection and reconstruction; and no tumor extension to the splenic vein, unless the tumor could be resected with a distal pancreatectomy and a splenic vein resection. All patients were aged ≤85 years, had an Eastern Cooperative Oncology Group performance status (PS) ≤2, and had organ function adequate to endure preoperative CRT and surgery [11]. Preoperative CRT was not discontinued because of its adverse effects in any patient.
Treatment protocol for preoperative CRT
Preoperative CRT included three-dimensional (3-D) conformal radiotherapy. The G-CRT group received a single course of 40 Gy in 20 fractions over 4 weeks. Systemic gemcitabine (800 mg/m2) was usually started concurrently with radiation and administered weekly. The GS-CRT group received 3-D conformal radiotherapy as a single course of 50.4 Gy in 28 fractions over 5 weeks. Oral S-1 (40–80 mg/m2) and an intravenous infusion of 600–1000 mg/m2 gemcitabine were delivered concurrently with the start of radiation. Radiation was performed as described previously [12, 13]. The clinical target volume was defined as the gross tumor volume with a 5-mm margin, plus the neuroplexus region and local lymph node region. The local lymph node regions included the celiac, superior mesenteric, peripancreatic, portal, and para-aortic regions, for pancreatic head cancers; and the splenic region for pancreatic body and tail cancers. The posterior margin of the target volume extended 1.0 cm posterior to the spinal column, and therefore included the vertebral bodies. The planned target volume included the clinical target volume, with an extra 10-mm margin for possible errors, as well as anatomical boundaries, such as the stomach, duodenum, small intestine, and transverse colon. The radiation field and dose were based on published data on the tolerance of normal tissue to therapeutic irradiation [14, 15].
Surgery
Restaging computed tomography (CT) was performed 1–2 weeks after the completion of preoperative CRT. In cases that did not involve liver metastasis, peritoneal implantation, or direct invasion of the adjacent large arteries, pancreatectomy was performed 3–7 weeks after preoperative CRT completion. When arterial reconstruction was required for curative resection, chemotherapy was given at least 6 months after CRT. When pancreatic tumors involved the PV/SMV, the involved part of the vein was resected together with the pancreas (en bloc resection). All gastrointestinal tract reconstruction procedures, including pancreatojejunostomy, pancreatogastrostomy, hepatic duct jejunostomy, gastrojejunostomy, and jejunojejunostomy, were performed after pancreaticoduodenectomy, but no anastomotic procedure was performed after distal pancreatectomy.
Pathological examination
Pathological examination was performed as described previously [12]. Briefly, human PDAC samples were obtained, with Institutional Review Board approval, and fixed in 10 % formalin for 48 h, embedded in paraffin, and sectioned into 3.5-μm slices. Formalin-fixed, paraffin-embedded tissue sections that included PDAC were deparaffinized, hydrated, and stained with hematoxylin and eosin. These samples were evaluated and diagnosed by an experienced pathologist.
Postoperative adjuvant chemotherapy and follow-up
Postoperative treatment was carried out according to the CONKO-001 study, with follow-up as described previously [3, 12, 16]. Briefly, for adjuvant chemotherapy, patients were treated with intravenous infusions of 800–1000 mg/m2 gemcitabine on days 1, 8, and 15, and then every 4 weeks for six cycles. This adjuvant chemotherapy regimen was started within 8 weeks after surgery, when the PS was ≤2 or there was no evidence of recurrence. To investigate for signs of recurrence, three kinds of examinations were performed every 3 months in the postoperative follow-up: a routine physical examination; laboratory tests, including checking serum levels of tumor markers, CEA and CA19-9; and radiological imaging, including chest X-ray and an abdominal CT [or magnetic resonance imaging (MRI)]. All cases were counted as “complete” when the patient had received at least 60 % of the regulated amount for 6 months.
Evaluation and statistical analysis
Toxicities were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE, version 4.0). Postoperative pancreatic fistulas were graded according to the definition of the International Study Group on Pancreatic Fistula (ISGPF). Postoperative delayed gastric emptying was graded according to the definition from the International Study Group of Pancreatic Surgery (ISGPS) [17, 18]. Data are expressed as mean ± standard deviation. The Chi-squared test and Fisher’s exact test were used for comparing categorical variables, when appropriate. All analyses were conducted with the JMP 11 software program (SAS Institute, Cary, NC, USA) [19]. Significance was defined as a P value of <0.05.
Results
PDAC backgrounds were similar among treatment groups, except in tumor stage
Table 1 summarizes the clinicopathological features of the patients with PDAC at their initial presentation to our department. The administration of preoperative treatment depended on the patient’s condition at that time; therefore, we examined the differences in patient characteristics among the three groups. We found that patients in the preoperative CRT groups had better PS than those in the SA group, but the difference was not significant. There were no significant differences among the groups in age, gender, co-existence of diabetes mellitus, or previous treatment of another cancer. The preoperative CRT groups showed more advanced clinical tumor-stages (cT) than the SA group; however, there were no significant differences in the mean tumor size, location, clinical detection of lymph node infiltration (N-stage), or clinically determined stage, defined by the Union for International Cancer Control (UICC), among the groups.
Table 2 shows the pathological findings of the resected specimens. Interestingly, pathology revealed local invasion that contrasted with the initial clinical findings. More advanced pathological T-stages (pT) were found in specimens resected from the SA group than in those resected from the GS-CRT group. These findings indicated that preoperative CRT was predominantly effective in limiting local tumor invasion.
Preoperative CRT did not affect perioperative complications
Table 3 summarizes the perioperative variables and complications in the three groups. Patients in the preoperative CRT groups had more high-stage locally advanced tumors than those in the SA group and the surgical procedures required were consequently more complicated in the CRT groups. For example, resection with reconstruction of the PV or the IVC was more often required in the G-CRT group than in the SA group. Accordingly, the operation times were longer in the G-CRT group, although there was no significant difference in blood loss between the groups. Surprisingly, performing preoperative CRT did not increase the incidence of perioperative complications, including surgical site infections [20]. Unfortunately, there was one postoperative death in the G-CRT group, from a pseudo-aneurysm rupture secondary to a pancreatic fistula. Despite this, the preoperative CRT groups had a lower incidence of pancreatic fistula than the SA group.
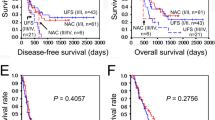
Preoperative CRT did not decrease the rate of completion of adjuvant chemotherapy
Figure 1 shows the postoperative clinical course of patients in each group. All the patients underwent curative resections of PDAC. A larger proportion of patients in the SA group than in the two CRT groups refused post-surgery adjuvant chemotherapy. Similar numbers of patients in the three groups could not undergo adjuvant chemotherapy because early recurrence was detected before adjuvant chemotherapy started. The rates of induction of adjuvant chemotherapy were 78.6 % in the G-CRT group, 78.1 % in the GS-CRT group, and 71.8 % in SA the group, without a significant difference among the three groups (P = 0.208). The rates of completing adjuvant chemotherapy were 86.4 % in the GS-CRT group, 88 % in the GS-CRT group, and 82.1 % in the SA group. Again, these rates were not significantly different among the three groups (P = 0.824). The main reasons for discontinuing adjuvant chemotherapy were recurrence (8 %) and adverse events (6.7 %). Accumulation of the anti-cancer drugs and the radiation dose during preoperative CRT did not affect the completion of adjuvant chemotherapy (Fig. 2).
Flowchart showing the number of patients in each group, at each stage of postoperative treatment (boxes). Right-pointing arrows indicate the number of patients that dropped out and their reasons for not continuing to the next stage. Gemcitabine was given as the adjuvant chemotherapy. CRT chemoradiotherapy, G-CRT gemcitabine and radiation treatment, GS-CRT gemcitabine, S-1, and radiation treatment, SA surgery alone
The total amount of gemcitabine, S-1, and radiation during the preoperative chemoradiotherapy (CRT). CRT chemoradiotherapy, G-CRT gemcitabine and radiation treatment, GS-CRT gemcitabine, S-1, and radiation treatment, Course A patients who completed postoperative adjuvant chemotherapy, Course B patients who discontinued postoperative adjuvant chemotherapy due to early recurrence, Course C patients who discontinued postoperative adjuvant chemotherapy due to its adverse events, Course D patients who refused postoperative adjuvant chemotherapy. Values are expressed as mean ± SD. The postoperative clinical course did not differ among the groups according to a the total amount of gemcitabine given during preoperative CRT to each preoperative CRT group (G-CRT group and GS-CRT group); b the total amount of S-1 given during preoperative CRT to the GS-CRT group; and c the total radiation dose given during preoperative CRT to each preoperative CRT group (G-CRT group and GS-CRT group): course A, course B, course C, and course D
Preoperative CRT did not increase the rates of adverse events during adjuvant chemotherapy
All adverse events during adjuvant chemotherapy were graded with the CTCAE version 4.0, as shown in Table 4. The frequencies of adverse events did not differ among the three groups, except for neutropenia. The SA group had significantly more cases of grade 3 or grade 4 neutropenia than the GS-CRT group.
Discussion
This retrospective study investigated the postoperative influences of two kinds of preoperative CRT treatments for patients with PDAC. In comparing these patient groups with a group of patients who did not receive preoperative CRT, the few differences in underlying tumor characteristics did not affect the rates of perioperative adverse events or the feasibility of adjuvant therapy, which were similar among the three groups. These results showed that preoperative CRT did not adversely affect the clinical course of PDAC surgery.
The only significant difference in the tumor characteristics of patients who received preoperative CRT and those who did not was the extent of local tumor invasion detected clinically. Tumor stages were more advanced in the preoperative CRT groups than in the SA group. In contrast, our pathological findings revealed that local invasion and vascular invasion were more advanced in the SA group than in the preoperative CRT groups. We assumed that these findings indicated a significant reduction in tumor progression, due to the effects of preoperative CRT, as previously reported [21]. These data also showed better local control of PDAC in the GS-CRT group than in the G-CRT group. This may be partly attributable to stronger anti-cancer activity of the combination therapy with gemcitabine and S-1 than gemcitabine alone in patients with unresectable PDAC, as previously described [4, 22–24]. We considered that the combination therapy with gemcitabine and S-1 may be capable of higher performance in the local control of PDAC during preoperative CRT.
Although we found a few differences in tumor characteristics among the treatment groups, they did not affect post-surgery outcomes. Therefore, we compared the perioperative adverse events and the feasibility of adjuvant therapy among the three groups. To investigate whether preoperative CRT would affect perioperative adverse events, we reasoned that if CRT increased the risk of major complications following surgery, then the PDAC prognosis would be exacerbated by the negative effects on the feasibility of postoperative therapy. Previous reports have presented conflicting results on how preoperative CRT affected perioperative variables and complications [21, 25–28]. For example, Laurence et al. [27] suggested that preoperative CRT might increase perioperative complications, whereas others found that preoperative CRT did not increase surgical variables, including the operation time and blood loss [28–30]. In the present study, the G-CRT group required significantly longer operation times than the SA group because the former group included more patients who required resection and reconstruction of the PV or the IVC. However, this difference could be explained by the larger number of more advanced cases in the G-CRT group than in the SA group. Consequently, we concluded that preoperative CRT did not prolong the operation time.
In the present study, there was one postoperative death, in the G-CRT group. This patient died of delayed massive hemorrhage from a pseudo-aneurysm rupture, on POD 97. As the pseudo-aneurysm accompanied a pancreatic fistula, we regarded the death as a complication of pancreatic fistula, because pseudo-aneurysms are rarely related to radiation [31, 32]. Moreover, the rate of pancreatic fistulas tended to be lower in the preoperative CRT groups than in the SA group in this study; a finding consistent with a previous report [33], which showed that radiation reduced pancreatic fistulas by hardening the pancreas with fibrosis. Therefore, we considered that the death in the preoperative CRT group was not related to the preoperative CRT. Another patient, from the GS-CRT group, suffered mild gastritis, which resolved with medication. A previous study also showed that the incidence of radiation-induced gastritis was very low because the stomach was rarely within the treated field [34]. Thus, this investigation showed that preoperative CRT did not increase perioperative adverse events significantly.
The induction and completion rates of postoperative adjuvant chemotherapy after CRT have rarely been reported; thus, we investigated these rates in each group. It remains unclear whether the feasibility of postoperative adjuvant chemotherapy is affected by preoperative CRT. Previous investigators reported rates of adjuvant chemotherapy induction of 30–95 % among patients who received preoperative CRT [30, 35]. White et al. reported that postoperative adjuvant therapy was given to 75 % of patients who did not receive preoperative anti-cancer therapy and to more than 30 % of those who did receive preoperative anti-cancer therapy [35]. In the present study, all three groups had similar adjuvant chemotherapy induction rates and completion rates, although there were no significant differences in dose intensity between patients who completed the adjuvant chemotherapy and those who discontinued adjuvant chemotherapy because of its adverse events (Fig. 2). This suggests that the accumulation of an anti-cancer drug or radiation dose before surgery does not significantly affect the ability to complete adjuvant chemotherapy.
Despite our finding that adjuvant chemotherapy delivery was statistically similar among the groups, both the induction and completion rates were higher in the preoperative CRT groups than in the SA group. Previous studies found that the completion of adjuvant chemotherapy was reduced in the presence of major postoperative complications [28]. As mentioned above, in the present study, preoperative CRT did not change the rate of major complications, which may explain why the adjuvant chemotherapy completion rates were similar in the preoperative CRT groups and the SA group. The different patient characteristics of the groups could also account for the results, as the SA group included more patients with poor PS and none stopped preoperative CRT because of its adverse events. This suggested that there may have been a potential bias in patient selection. Some patients in the SA groups refused adjuvant chemotherapy because of their physical condition, such as general fatigue. It is possible that the preoperative CRT groups comprised a larger proportion of patients who could endure adjuvant chemotherapy. Indeed, the SA group included significantly more cases of grade 3 or grade 4 neutropenia during adjuvant chemotherapy than the GS-CRT group. However, in comparing the dose intensity of preoperative therapy, there were no significant differences between that given to patients who could complete the adjuvant chemotherapy and that of those who discontinued adjuvant chemotherapy because of its adverse events (Fig. 2). This suggests that accumulation of the anti-cancer drug or radiation dose before surgery does not significantly affect the completion of adjuvant chemotherapy.
In conclusion, the present study showed that preoperative CRT was safe, it did not affect the subsequent clinical course, and it did not compromise the feasibility of adjuvant chemotherapy.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Li D, Xie K, Wolff R, Abbruzzese JL. Pancreatic cancer. Lancet. 2004;363:1049–57.
Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310:1473–81.
Ueno H, Kosuge T, Matsuyama Y, Yamamoto J, Nakao A, Egawa S, et al. A randomized phase III trial comparing gemcitabine with surgery-alone in patients with resected pancreatic cancer: Japanese Study Group of Adjuvant Therapy for Pancreatic Cancer. Br J Cancer. 2009;101:908–15.
Chua TC, Saxena A. Preoperative chemoradiation followed by surgical resection for resectable pancreatic cancer: a review of current results. Surg Oncol. 2011;20:161–8.
Artinyan A, Anaya DA, McKenzie S, Ellenhorn JD, Kim J. Neoadjuvant therapy is associated with improved survival in resectable pancreatic adenocarcinoma. Cancer. 2011;117:2044–9.
Paulson AS, Tran Cao HS, Tempero MA, Lowy AM. Therapeutic advances in pancreatic cancer. Gastroenterology. 2013;144:1316–26.
Evans DB, Varadhachary GR, Crane CH, Sun CC, Lee JE, Pisters PW, et al. Preoperative gemcitabine-based chemoradiation for patients with resectable adenocarcinoma of the pancreatic head. J Clin Oncol. 2008;26:3496–502.
Gillen S, Schuster T, Meyer Zum Büschenfelde C, Friess H, Kleeff J. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med. 2010;7:e1000267.
Morganti AG, Massaccesi M, La Torre G, Caravatta L, Piscopo A, Tambaro R, et al. A systematic review of resectability and survival after concurrent chemoradiation in primarily unresectable pancreatic cancer. Ann Surg Oncol. 2010;17:194–205.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
Eguchi H, Nagano H, Tanemura M, Takeda Y, Marubashi S, Kobayashi S, et al. Preoperative chemoradiotherapy, surgery and adjuvant therapy for resectable pancreatic cancer. Hepatogastoroenterology. 2013;60:904–11.
Eguchi H, Nagano H, Kobayashi S, Kawamoto K, Wada H, Hama N, et al. A phase I trial of combination therapy using gemcitabine and S-1 concurrent with full-dose radiation for resectable pancreatic cancer. Cancer Chemother Pharmacol. 2014;73:309–15.
Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1991;21:109–22.
Marks LB, Yorke ED, Jackson A, Ten Haken RK, Constine LS, Eisbruch A, et al. Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys. 2010;76:S10–9.
Iwagami Y, Eguchi H, Wada H, Tomimaru Y, Hama N, Kawamoto K, et al. Implication of peritoneal lavage cytology in resectable left-side pancreatic cancer. Surg Today. 2015;45:444–50.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761–8.
Komatsu H, Egawa S, Motoi F, Morikawa T, Sakata N, Naitoh T, et al. Clinicopathological features and surgical outcomes of adenosquamous carcinoma of the pancreas: a retrospective analysis of patients with resectable stage tumors. Surg Today. 2015;45:297–304.
Shinkawa H, Takemura S, Uenishi T, Sakae M, Ohata K, Urata Y, et al. Nutritional risk index as an independent predictive factor for the development of surgical site infection after pancreaticoduodenectomy. Surg Today. 2013;43:276–83.
Heinrich S, Pestalozzi BC, Schäfer M, Weber A, Bauerfeind P, Knuth A, et al. Prospective phase II trial of neoadjuvant chemotherapy with gemcitabine and cisplatin for resectable adenocarcinoma of the pancreatic head. J Clin Oncol. 2008;26:2526–31.
Nakai Y, Isayama H, Sasaki T, Sasahira N, Ito Y, Kogure H, et al. Impact of S-1 on the survival of patients with advanced pancreatic cancer. Pancreas. 2010;39:989–93.
Nakai Y, Isayama H, Sasaki T, Sasahira N, Tsujino T, Toda N, et al. A multicentre randomised phase II trial of gemcitabine alone vs gemcitabine and S-1 combination therapy in advanced pancreatic cancer: GEMSAP study. Br J Cancer. 2012;106:1934–9.
Schultheis B, Strumberg D, Bergmann L, Graeven U, Hanauske AR, Lipp R, et al. Results of a phase II trial of S-1 as first-line treatment of metastatic pancreatic cancer (CESAR-study group). Invest New Drugs. 2012;30:1184–92.
Sasson AR, Wetherington RW, Hoffman JP, Ross EA, Cooper H, Meropol NJ, et al. Neoadjuvant chemoradiotherapy for adenocarcinoma of the pancreas: analysis of histopathology and outcome. Int J Gastrointest Cancer. 2003;34:121–8.
Cheng TY, Sheth K, White RR, Ueno T, Hung CF, Clary BM, et al. Effect of neoadjuvant chemoradiation on operative mortality and morbidity for pancreaticoduodenectomy. Ann Surg Oncol. 2006;13:66–74.
Laurence JM, Tran PD, Morarji K, Eslick GD, Lam VW, Sandroussi C. A systematic review and meta-analysis of survival and surgical outcomes following neoadjuvant chemoradiotherapy for pancreatic cancer. J Gastrointest Surg. 2011;15:2059–69.
Tzeng CW, Tran Cao HS, Lee JE, Pisters PW, Varadhachary GR, Wolff RA, et al. Treatment sequencing for resectable pancreatic cancer: influence of early metastases and surgical complications on multimodality therapy completion and survival. J Gastrointest Surg. 2014;18:16–24.
Takahashi H, Ogawa H, Ohigashi H, Gotoh K, Yamada T, Ohue M, et al. Preoperative chemoradiation reduces the risk of pancreatic fistula after distal pancreatectomy for pancreatic adenocarcinoma. Surgery. 2011;150:547–56.
Sho M, Akahori T, Tanaka T, Kinoshita S, Tamamoto T, Nomi T, et al. Pathological and clinical impact of neoadjuvant chemoradiotherapy using full-dose gemcitabine and concurrent radiation for resectable pancreatic cancer. J Hepatobiliary Pancreat Sci. 2013;20:197–205.
Schafer M, Heinrich S, Pfammatter T, Clavien PA. Management of delayed major visceral arterial bleeding after pancreatic surgery. HBP (Oxford). 2011;13:132–8.
Murono S, Nakanishi Y, Inoue D, Ozaki K, Kondo S, Wakisaka N, et al. Pseudoaneurysm of the lingual artery after concurrent intra-arterial chemotherapy with radiotherapy for advanced tongue cancer. Head Neck. 2011;33:1230–2.
Ishikawa O, Ohigashi H, Imaoka S, et al. Concomitant benefit of preoperative irradiation in preventing pancreas fistula formation after pancreatoduodenectomy. Arch Surg. 1991;126:885–9.
Shukuwa K, Kume K, Yamasaki M, Yoshikawa I, Otsuki M. Argon plasma coagulation therapy for a hemorrhagic radiation-induced gastritis in patient with pancreatic cancer. Intern Med. 2007;46:975–7.
White RR, Kattan MW, Haney JC, Clary BM, Pappas TN, Tyler DS, et al. Evaluation of preoperative therapy for pancreatic cancer using a prognostic nomogram. Ann Surg Oncol. 2006;13:1485–92.
Acknowledgments
We thank all of those who contributed samples, the surgeons and nursing staff, and the pathologists at Osaka University Hospital, Japan for providing precise pathological diagnoses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hideo Tomihara and his co-authors have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Tomihara, H., Eguchi, H., Yamada, D. et al. Preoperative chemoradiotherapy does not compromise the feasibility of adjuvant chemotherapy for patients with pancreatic ductal adenocarcinoma. Surg Today 47, 218–226 (2017). https://doi.org/10.1007/s00595-016-1405-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-016-1405-6