Abstract
Background and Objectives
Minimally invasive surgery for adrenocortical carcinoma (ACC) is controversial. We sought to evaluate the perioperative and long-term outcomes following minimally invasive (MIS) and open resection (OA) of ACC in patients treated with curative intent surgery.
Methods
Retrospective data from patients who underwent adrenalectomy for primary ACC at 13 tertiary care cancer centers were analyzed, including demographics, clinicopathological, and operative outcomes. Outcomes following MIS were compared to OA.
Results
A total of 201 patients were evaluated including 47 MIS and 154 OA. There was no difference in utilization of MIS approach among institutions (p = 0.24) or 30-day morbidity (29.3 %, MIS, vs. 30.9 %, OA; p = 0.839). The only preoperatively determined predictor for MIS was smaller tumor size (p < 0.001). There was no difference in rates of intraoperative tumor rupture (p = 0.612) or R0 resection (p = 0.953). Only EBL (p = 0.038) and T stage (p = 0.045) were independent prognostic indicators of overall survival after adjusting for significant factors. The surgical approach was not associated with overall or disease-free survival.
Conclusion
MIS adrenalectomy may be utilized for preoperatively determined ACC ≤ 10.0 cm; however, OA should be utilized for adrenal masses with either preoperative or intraoperative evidence of local invasion or enlarged lymph nodes, regardless of size.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Minimally invasive adrenalectomy (MIS) for primary adrenocortical carcinoma (ACC) remains a highly controversial topic despite the widespread acceptance of minimally invasive techniques among surgeons. The laparoscopic approach to adrenalectomy was first introduced in 1992 and has since been adopted as the preferred approach for resection of benign, functioning, and nonfunctioning adrenal masses.1 A greater number of published series revealing comparable short-term outcomes between MIS and open adrenalectomy (OA) have resulted in increased enthusiasm for MIS for adrenal malignancies; however, these were hindered by small case series and variable duration of follow-up.2 – 6 Despite the demonstrated safety and efficacy of MIS among small- to medium-sized benign lesions (≤6 cm), OA remains to be the procedure of choice for ACC adrenalectomy, which allows for consistent and complete en bloc resection.2 – 6
The two largest comparative series to date of MIS versus OA included 46 laparoscopic cases from the University of Michigan and 30 laparoscopic cases from the Italian Multi-institutional Study.4 , 7 There were no differences in overall survival (OS) and disease-free survival (DFS) between groups in the Italian study, whereas the University of Michigan concluded that OA was superior to the laparoscopic approach due to significantly different positive resection margins, incidence of tumor spillage, improved overall survival among stage II patients, and shorter time to recurrence.4 , 7 The current study includes a large number of MIS adrenalectomies compared to OA.
ACC is a rare and aggressive malignancy afflicting approximately two patients per million per year, accounting for 0.2 % of cancer-related mortality, with 5-year OS rates of 13–58 % following resection.8 – 12 Difficulty in treating most patients is attributed to locally advanced or metastatic disease at the time of presentation. In light of evidence demonstrating chemotherapy and radiation in ACC are largely ineffective, accomplishing a complete oncologic resection (R0) remains the most critical component to curative intent therapy, offering the only opportunity for long-term cure.8 , 11 The early evidence on MIS versus OA offer conflicting outcomes; however, a growing body of evidence reveal comparable short-term outcomes in carefully selected cases of early ACC, while abiding by the principles of oncological resection when performed at high volume centers.2 , 5 , 7 , 9 , 13 – 15 Anecdotal advantages of MIS for ACC include decreased postoperative pain, shorter length of stay, quicker rehabilitation, and fewer complications.6 , 16 MIS has also been correlated with earlier recurrence rates, increased the risk of tumor spillage, or positive margins.7 , 13 As a result, the current guidelines per the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) for resection of ACC dictate the standard treatment should be open surgery with the caveat that if malignancy is unknown preoperatively or if the MIS approach is initiated for suspected early-stage disease, a low threshold for conversion is strongly recommended when there is evidence of invasion, adhesion, or enlarged lymph nodes are seen, as the ideal treatment includes en bloc resection of any involved structures and regional lymphadenectomy.17
In this study, we evaluated the oncologic and long-term survival outcomes of patients treated with MIS or OA in a multi-institutional collaboration among expert academic referral centers in the USA, drawing one of the largest numbers of MIS adrenalectomies reported to date.
Methods
Patients and Data Collection
Demographic, clinicopathological, and perioperative data for all patients who underwent initial curative intent surgery for a diagnosis of adrenocortical carcinoma were collected between 1994 and 2014. Patients were identified from 1 of 13 participating institutions in the US Adrenocortical Carcinoma Group, including the University of Wisconsin, Johns Hopkins Hospital, Stanford University, Vanderbilt University, Emory University, Wake Forest University, Washington University in St. Louis, The Ohio State University, University of California San Francisco, Medical College of Wisconsin, University of Texas Southwestern Medical Center, and New York University. This study included both pediatric and adult populations. Patients diagnosed with metastatic disease and those who underwent reoperation for ACC were excluded from the study. All patient data were collected retrospectively from medical charts. Institutional review board approval was obtained at each participating institution.
Specific demographic, perioperative, and clinicopathological data included age, gender, ASA class, functional tumor status, laterality, EBL, preoperative tumor size, lymph node status, T stage, receipt of neoadjuvant and adjuvant therapies, capsular invasion, lymphatic and venous invasion, and resection margin status. For T stage, two categories were created: (1) lower stage tumors (T1 and T2) and (2) higher stage tumors (T3 and T4). Perioperative complication data were also compared between groups, including in-hospital mortality, mortality within 30 days of operation, any complication within 30 days of operation, Clavien grade, occurrence of abdominal abscess, pancreatic leak, pulmonary embolism, intraoperative tumor rupture, postoperative adrenal insufficiency, reoperation, and readmission. For Clavien grade, two categories were created to define low grades of complications (grades I and II) and high grades of complications (III, IV, and V). The surgical approach was reported as open or MIS. MIS included laparoscopic, hand-assisted, robotic and retroperitoneoscopic approaches to surgery. Open surgery was described as either abdominal, posterior, or thoracoabdominal. Readmission was defined as occurring within 90 days of operation. Disease recurrence was defined as biopsy-proven ACC or imaging reports consistent with or highly suggestive of tumor recurrence.
Predictors of Resection Margin Status
In order to identify factors with potential impact on resection margin status, the surgical approach, preoperative tumor size, age, gender, and BMI were selected as the preoperative factors available for univariable and logistic regression analyses. Three additional patient variables, the surgical era, tumor size category, and size approach, were constructed to account for the potential influences of time throughout the course of the study, and the potential relationship between tumor size and surgical approach on resection margin status. The surgical era was defined as either early, the period between 1994 and 2005, or late, the period from 2006 to 2014. The tumor size overlap was defined as the range of tumor sizes in which both MIS and OA procedures were performed, and only these cases were used for this analysis. This range was then subdivided into three smaller categories to create the tumor size category variable. Tumor size categories were defined as 1 (3.7–7.0 cm), 2 (7.1–10.0 cm), or 3 (10.1–16 cm). The “size-approach” was a combined variable of the tumor size category in association with the surgical approach used (MIS or OA). The purpose of this variable was to incorporate the potential influence of interactions between the size of the tumor in the context of a MIS or open approach. For example, a tumor classified as “2-MIS” is one in which its size was between 7.1 and 10.0 cm and was resected by a MIS approach.
Prognostic Indicators of Overall and Disease-Free Survival
OS and DFS times were computed for all patients starting from the date of operation. DFS was defined as the duration from the time of initial operation to the first documentation of disease recurrence.
Statistical Analyses
Demographic, clinicopathological, and perioperative patient data were stratified according to operative approach (MIS vs. OA). This analysis was conducted under an intention to treat analysis, such that the MIS group was analyzed with the patients that were converted to open surgery. Two additional subgroup analyses were conducted. One analysis evaluated patients within the MIS group alone in order to isolate potential predictors of conversion. Patients who underwent a MIS approach with subsequent conversion to open were compared to patients who underwent a nonconverted MIS approach. A second comparison of nonconverted MIS cases versus OA was also conducted.
Variables with potential correlations were analyzed by the Pearson product–moment correlation coefficient in order to identify the degree of linear dependence between two variables to avoid potential confounding. The variables EBL and operative transfusion were statistically correlated (R > 0.4); therefore, only EBL was included in univariable and multivariable analyses. Other variables with possible collinear relationships included tumor size with EBL and tumor size with T stage, neither of which were correlated. Potential differences between groups were evaluated by χ 2 analyses and Student’s t test where appropriate. Continuous data were reported as medians with ranges. Among the factors that satisfied the inclusion criteria for multivariable analysis, functional tumor status and venous invasion were excluded on the basis of significant missing data (≥75.0 % missing), which presented a significant risk of unreliable estimates.
In the analysis of factors influencing resection margin status, all patients under tumor size category 3 (tumor size range 10.1–16.0 cm, category 3-MIS and category 3-OA) were excluded due to the small number of patients in the 3-MIS group (n = 2). Among the preoperative factors available for analysis, the surgical approach, preoperative tumor size, tumor size category, size-approach, age, gender, BMI, and surgical era were included in univariable analysis. In multivariable logistic regression, factors with p < 0.1 on univariable analyses were included in the model in addition to the size-approach variable.
In survival analyses, patient demographic, perioperative, and clinicopathological data were evaluated for differences between the MIS and open surgery groups using χ 2 and Student’s t tests. Factors with p < 0.1 were assessed for predictive capacity for OS and DFS in univariable and multivariable analyses via a Cox proportional hazards model. OS and DFS were estimated for each group using the methods of Kaplan and Meier. Additionally, propensity score analysis was utilized in order to adjust for preoperative factors thought to impact the choice of surgical approach on OS and DFS. All preoperative factors satisfying p < 0.2 in logistic regression analyses were included in the propensity score as follows: PS = −3.142 + (0.148 × era) − (0.004 × age) − (0.485 × functional tumor status) + (1.234 × gender) + (0.513 × tumor size). One-to-one matching was not possible due to a high degree of missing data; rather, the propensity score was constructed and included with the surgical approach in an adjusted Cox proportional hazards model for OS and DFS. All statistical tests were two-sided, and statistical significance was denoted by p < 0.05. Statistical analyses were performed using SPSS software (version 23.0, IBM SPSS, Chicago, IL).
Results
Demographic and Clinicopathological Characteristics
The original study cohort consisted of 265 cases of adrenalectomy for ACC. Twelve cases were excluded due to unreported approach to surgery, and 52 cases were excluded due to metastatic disease at the time of presentation. A MIS approach was utilized in 47 (23.4 %) of patients. Thus, there were 201 patients across 13 institutions included in this study. Within this group, there were 2 robotic ACC resections, 1 retroperitoneoscopic approach, 3 hand-assisted approaches, and 32 laparoscopic resections. In addition, nine cases were included in the MIS group as an intention to treat analysis due to conversion from laparoscopic to open surgery (19.0 % conversion) (Fig. 1). Thus, there were 38 patients in the nonconverted MIS group and 154 patients in the OA group.
There was no difference among participating institutions in the decision to proceed with a MIS approach to surgery (p = 0.24). The gender distribution, BMI, and ASA classification were comparable between both approaches (Table 1). Utilization of a MIS approach was not associated with tumor laterality, functional tumor status, the era in which the operation was performed, or receipt of neoadjuvant chemotherapy. There were many differences between groups, with MIS patients presenting with smaller tumors (median size 5.5 cm, MIS, vs. 10.9 cm, OA; p < 0.001), lower EBL (100 mL, MIS, vs. 825 mL, OA; p = 0.002), shorter length of stay (median LOS 3 days, MIS, vs. 6 days, OA; p < 0.001), and lower pathologic T stage (75 %, MIS, vs. 44.3 %, OA for T1–T2; p < 0.001). A complete comparison of patient demographic, perioperative, and tumor data between MIS and OA are summarized in Table 1.
In the comparison of nonconverted MIS versus OA, univariable analysis revealed smaller tumor size (median size 5.5 cm, nonconverted MIS, vs. 10.9 cm, OA; p < 0.001), lower EBL (100 mL, nonconverted MIS, vs. 825 mL, OA; p = 0.002), shorter median operative time (156 min, nonconverted MIS, vs. 236 min, OA; p = 0.007), shorter length of stay (2 days, nonconverted MIS, vs. 6 days, OA; p = 0.001), and lower T stage (T1–T2 77.8 %, nonconverted MIS, vs. 44.3 %, OA; p < 0.001) as statistically different in the MIS group.
Perioperative Morbidity and Mortality
There was no difference in 30-day or in-hospital mortality following adrenalectomy (Table 2). There was no difference in 30-day overall morbidity between MIS and open surgery groups (p = 0.839). For patients who experienced postoperative complications, there were no differences in the grade of complication (p = 0.537). There was no difference in the rate of intraoperative tumor rupture (p = 0.612) or necessity for reoperation between groups (p = 0.871). Of note, there were no differences between the overall morbidity (p = 0.669), 30-day mortality (p = 0.563), and in-hospital mortality (p = 0.587) with the era in which the operation was performed. In the subgroup analysis of nonconverted MIS cases compared to OA, there was no difference in the overall 30-day complication rate (25.0 %, nonconverted MIS, vs. 30.9 %, OA; p = 0.669), low grade of complications (71.4 %, nonconverted MIS, vs. 59.6 %, OA; p = 0.694), intraoperative tumor rupture (8.8 %, nonconverted MIS, vs. 9.4 %, OA; p = 0.999), or R0 status (77.0 %, nonconverted MIS, vs. 72.0 %, OA; p = 0.50).
Potential Influences on Resection Margin Status
The tumor size overlap between MIS (including converted cases) and OA cases ranged from 3.7 to 16 cm. On univariable analysis, the early surgical era was significantly associated with higher R1 status (37.5 %, early era, vs. 20.9 %, late era; p = 0.017). Of note, the approach (p = 0.953), preoperative tumor size (p = 0.661), tumor size category (p = 0.792), and size-approach (p = 0.817) were not associated with R1 status. No factors were significantly associated with an impact on R1 status in multivariable analysis (Table 3). Of note, there was no association of type of surgical approach with margin status.
Prognostic Indicators, OS, and DFS Following Resection of ACC
The surgical approach, tumor size, EBL (dL), length of stay, and T stage were included in univariable and multivariable analyses of potential prognostic indicators in OS and DFS. In our analysis, EBL and transfusion were correlated by Pearson coefficient (R = 0.660), whereas EBL and tumor size were not (R = 0.273), nor was T stage and tumor size (p = 0.331). Hence, only EBL was selected in the current analyses. On univariable analysis, significant prognostic factors for OS included tumor size (p = 0.026), EBL (p = 0.002), and T stage (p = 0.003). EBL (p = 0.038) and T stage (p = 0.045) were independently predictive of OS on multivariable analysis (Table 5). Similarly, tumor size (p = 0.043) was significantly associated with DFS on univariable analysis; however, there were no factors that were independently correlated with DFS on multivariable analysis (Table 6). Of note, the era in which the operation was performed had no impact on OS (p = 0.809) or on DFS (p = 0.151).
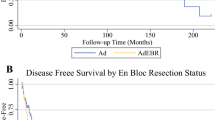
There was no difference in median and 5-year OS between groups (MIS vs. OA 91.0 vs. 53.9 months, and 67.7 vs. 48.6 %, respectively; p = 0.289, Table 4; Fig. 2). In addition, there was no difference in the median and 5-year DFS for patients who underwent MIS versus open surgery (14.3 vs. 9.8 months, and 9.1 vs. to 3.8 % respectively (p = 0.174, Table 4; Fig. 3). Overall disease recurrence rates were comparable between both groups (p = 0.074) (Table 2). On multivariable analysis, after controlling for tumor size, EBL, LOS, and T stage, there was no difference in OS and DFS rates associated with the type of surgical approach (p = 0.239 and p = 0.285, respectively) (Tables 5 and 6; Figs. 2 and 3, respectively). After adjusting for the approach and propensity score in multivariable logistic regression analyses, neither the propensity score nor surgical approach was predictive of OS or DFS (OS: propensity score p = 0.354, approach p = 0.302; DFS: propensity score p = 0.453, approach p = 0.306).
The 5-year disease-free survival for patients who underwent minimally invasive versus open resection for adrenocortical carcinoma. There was no difference in median and 5-year DFS for patients who underwent MIS versus OA (14.3 vs. 9.8 months, and 9.1 vs. to 3.8 %, respectively; p = 0.285). Number at risk (asterisk)
In subgroup analysis of nonconverted MIS cases to OA, univariable analysis revealed EBL (p = 0.008) and T stage (p = 0.002) as predictors for OS; however, no factors were identified for DFS in this cohort. On multivariable analyses, EBL (p = 0.020) was the only independent prognostic factor for OS, and no factors were identified for DFS. There were no differences in median and 5-year OS based on surgical approach (nonconverted MIS vs. OA 90.9 vs. 53.9 months, and 68.9 vs. 48.6 %; p = 0.261). Similarly, there were no differences in the median and 5-year DFS between nonconverted MIS and OA (18.8 vs. 9.8 months, and 11.1 vs. 3.8 %, respectively; p = 0.083).
Predictors of Conversion to Open Surgery
Subgroup analyses of patients who underwent conversion to open surgery from a minimally invasive approach were compared to cases completed using the MIS approach (9 vs. 38 cases, respectively). On univariable analysis, the cases completed using MIS techniques had significantly lower BMI (median 25.5 kg/m2, range 19.0–50.0, nonconverted MIS, vs. 34.0 kg/m2, range 25.4–64.0, converted MIS; p = 0.020), smaller tumor size (median 6.5 cm, range 3.0–15.0, nonconverted MIS, vs. 11.0 cm, range 7.0–15.0, converted MIS; p < 0.001), lower EBL (median 100 mL, range 25–450, nonconverted MIS, vs. 800 mL, range 400–1400, converted MIS; p < 0.001), and shorter operative times (156 min, range 79–318, nonconverted MIS, vs. 358 min, range 205–780, converted MIS; p = 0.001). After adjusting for BMI, tumor size, EBL, and operative time on multivariable analysis, there was no difference in OS and DFS rates associated with the type of surgical approach (p = 0.540 and p = 0.197, respectively).
Discussion
This study represents one of the largest comparative series of the effect of type of surgical approach for ACC. To date, the current literature includes small case series, lacking power to perform adequate case matching2 – 4 , 7 , 11 – 13 , 18 , 19 (Table 7). In this study, there was no difference in R0 status, tumor recurrence, intraoperative tumor rupture, or evidence of microvascular or capsular invasion between MIS and OA. Our findings highlighted EBL and T stage as independent prognostic indicators for OS, but not the surgical approach. Therefore, in these highly selected patients, there was no difference in outcome when MIS techniques were utilized. Notably, there was no difference in overall morbidity or grade of complication. Potential explanations for this finding may be that morbidity is linked to the risk inherent with the need for en bloc resection or the absence of anastomoses that drives surgical complications for other tumor types. The exact reason for the lack of association with between surgical approach and complications is unclear and larger series are required to verify these results.
Our group previously identified independent associations between postoperative complications and decreased OS following resection of various tumors including ACC and gastric carcinoma.15 , 20 Peritoneal carcinomatosis and laparoscopy have been anecdotally correlated; however, our data do not reflect a difference in tumor recurrence between approaches. Earlier underpowered reports have cautioned against laparoscopic adrenalectomy for ACC due to high rates of peritoneal carcinomatosis attributed to violation of the tumor capsule during manipulation.6 , 13 , 21 Although the development of peritoneal carcinomatosis was not studied in this series, our data did not reveal a greater risk of intraoperative tumor rupture within the MIS group, which likely reflects stringent patient selection, smaller tumor size, and increased proficiency of experienced MIS surgeons at participating institutions. Future studies will need to evaluate the presence of peritoneal carcinomatosis following MIS adrenalectomy in order to validate these results.
Our analysis reveals that the approach to surgery does not significantly affect the risk of margin positivity, which is consistent with prior analyses, although smaller tumors were more common in the MIS group.3 , 7 , 18 In order to account for this difference, the size-approach variable, which accounted for the potential interactions of tumor size and approach in the same model, revealed no difference in margin status and tumor size. This is a critical finding, as the importance of achieving a margin-negative resection was reinforced in a large analysis of nearly 4000 patients identified from the National Cancer Data Base, which revealed a clear improvement in survival among margin-negative patients.9
Prior authors have suggested relative contraindications to MIS adrenalectomy, such as prior laparotomy, trauma, or widespread systemic disease.12 , 22 However, others noted none of their laparoscopic cases were converted due to adhesions, even though as many as 69 % of patients had undergone previous surgery.16 Locally advanced disease, widespread systemic disease, and tumor size greater than 10 cm have all been reported to favor the decision to pursue OA in other series.16 , 22 – 24 The conversion rate in the current study was 19.1 %. Other series have reported conversion rates ranging from 7 to 34.2 %; however, these data may also be obscured by small sample sizes and variations establishing comparative groups.19 , 25 After analyzing the nonconverted MIS cases compared to OA, there were no differences in terms of perioperative or survival outcomes. It is important to note that the diagnosis of ACC is often unknown to the surgeon prior to the operation and a significant proportion of adrenal lesions are resected under the premise of reasonable suspicion due to size and imaging characteristics. As a result, the decision to pursue a MIS or OA is chiefly guided by technical feasibility.
Stringent patient selection criteria have long been attributed to the success and safety of MIS adrenalectomy. The sole distinguishing preoperative criterion between the two approaches included smaller tumors in the MIS group. Not surprisingly, this suggests that size carries the greatest impact in decision-making regarding the surgical approach. Low stage tumors (AJCC T1 and T2) were independently predictive of improved survival. For ACC, the tumor, lymph node, and metastasis (TNM) classification proposed by the International Union Against Cancer (UICC) and the American Joint Commission on Cancer (AJCC) has been the most widely used classification and the staging strategy used in this study. However, TNM staging for ACC remains controversial in terms of true prognostic value. The European Network for the Study of Adrenal Tumors (ENSAT) is recognized for its ability to prognostically differentiate between stages II and III and was validated in a large German ACC registry.26 , 27 The Weiss score utilizes tumor pathology to assess prognosis, however is limited by its reliance on inter-rater reproducibility.28 Although neither the ENSAT nor Weiss scoring classifications were available in this study, these staging systems offer additional prognostic insight to ACC survival analyses for future studies.
There are several limitations to this study. The retrospective design limited the analysis, and selection bias was likely. Retrospective data collection also contributed to missing data, which may have led to a misrepresentation of the impact of certain factors on MIS and OA. The limited recurrence data was likely the result of the referral-based practice among participating centers, wherein many patients are followed in the community and thus recurrence data was incomplete. In addition, this series was limited by the rarity of the disease, evidenced by the number of MIS cases available over a 20-year period (n = 47). The diagnosis of ACC was not known prior to surgery. Therefore, the decision-making process for approach may have been driven by other factors, including clinical suspicion and tumor size; thus, these data attest to the technical feasibility of MIS adrenalectomy. There remain inherent differences among centers that could not have been controlled, including protocols of perioperative management, oncologic follow-up, the impact of learning curve among trainees, and slight variations in surgical techniques. Under ideal circumstances, the most effective approach to confirm the findings in this study is a prospective, randomized controlled trial, but this is not realistic due to the rarity of ACC and the infrequency of pre-operative diagnosed ACC.
Despite these limitations, this study represents one of the largest series of MIS ACC resections treated curatively across 13 tertiary care centers in the country, offering a robust illustration of current practice and long-term outcomes in an area of ongoing clinical investigation. For suspected ACC, an open adrenalectomy is recommended in order to ensure a true oncologic resection particularly when there may be concern for invasion. However, a MIS approach may be utilized to patients with tumors ≤ 10 cm, providing the principles of an oncologic resection are followed.
Conclusion
In patients undergoing curative intent resection for ACC, MIS techniques offer comparable surgical and oncologic outcomes to open surgery among highly selected patients with a preoperative tumor size less than or equal to 10.0 cm. There was no difference in OS or DFS based on the surgical approach. The deciding factor in the surgical approach for ACC must be driven by the ability to achieve a complete and appropriate oncologic resection. Open adrenalectomy should be utilized for adrenal masses with either preoperative or intraoperative evidence of local invasion or enlarged lymph nodes, regardless of size.
References
Gagner M, Lacroix A, Prinz RA, et al.: Early experience with laparoscopic approach for adrenalectomy. Surgery 1993;114:1120–1124; discussion 1124–1125.
Donatini G, Caiazzo R, Do Cao C, et al.: Long-term survival after adrenalectomy for stage I/II adrenocortical carcinoma (ACC): a retrospective comparative cohort study of laparoscopic versus open approach. Ann Surg Oncol 2014;21:284–291.
Fossa A, Rosok BI, Kazaryan AM, et al.: Laparoscopic versus open surgery in stage I-III adrenocortical carcinoma -- a retrospective comparison of 32 patients. Acta Oncol 2013;52:1771–1777.
Lombardi CP, Raffaelli M, De Crea C, et al.: Open versus endoscopic adrenalectomy in the treatment of localized (stage I/II) adrenocortical carcinoma: results of a multiinstitutional Italian survey. Surgery 2012;152:1158–1164.
Porpiglia F, Fiori C, Daffara F, et al.: Retrospective evaluation of the outcome of open versus laparoscopic adrenalectomy for stage I and II adrenocortical cancer. Eur Urol 2010;57:873–878.
Autorino R, Bove P, De Sio M, et al.: Open Versus Laparoscopic Adrenalectomy for Adrenocortical Carcinoma: A Meta-analysis of Surgical and Oncological Outcomes. Ann Surg Oncol 2016;23:1195–1202.
Miller BS, Gauger PG, Hammer GD, Doherty GM: Resection of adrenocortical carcinoma is less complete and local recurrence occurs sooner and more often after laparoscopic adrenalectomy than after open adrenalectomy. Surgery 2012;152:1150–1157.
Ranvier GG, Inabnet WB, 3rd: Surgical management of adrenocortical carcinoma. Endocrinol Metab Clin North Am 2015;44:435–452.
Bilimoria KY, Shen WT, Elaraj D, et al.: Adrenocortical carcinoma in the United States: treatment utilization and prognostic factors. Cancer 2008;113:3130–3136.
Schteingart DE, Doherty GM, Gauger PG, et al.: Management of patients with adrenal cancer: recommendations of an international consensus conference. Endocr Relat Cancer 2005;12:667–680.
Mir MC, Klink JC, Guillotreau J, et al.: Comparative outcomes of laparoscopic and open adrenalectomy for adrenocortical carcinoma: single, high-volume center experience. Ann Surg Oncol 2013;20:1456–1461.
Cooper AB, Habra MA, Grubbs EG, et al.: Does laparoscopic adrenalectomy jeopardize oncologic outcomes for patients with adrenocortical carcinoma? Surg Endosc 2013;27:4026–4032.
Gonzalez RJ, Shapiro S, Sarlis N, et al.: Laparoscopic resection of adrenal cortical carcinoma: a cautionary note. Surgery 2005;138:1078–1085; discussion 1085–1076.
Moinzadeh A, Gill IS: Laparoscopic radical adrenalectomy for malignancy in 31 patients. J Urol 2005;173:519–525.
Margonis GA, Amini N, Kim Y, et al.: Incidence of Perioperative Complications Following Resection of Adrenocortical Carcinoma and Its Association with Long-Term Survival. World J Surg 2016;40:706–714.
Cobb WS, Kercher KW, Sing RF, Heniford BT: Laparoscopic adrenalectomy for malignancy. Am J Surg 2005;189:405–411.
Stefanidis D, Goldfarb M, Kercher KW, et al.: SAGES guidelines for minimally invasive treatment of adrenal pathology. Surg Endosc 2013;27:3960–3980.
Miller BS, Ammori JB, Gauger PG, et al.: Laparoscopic resection is inappropriate in patients with known or suspected adrenocortical carcinoma. World J Surg 2010;34:1380–1385.
Brix D, Allolio B, Fenske W, et al.: Laparoscopic versus open adrenalectomy for adrenocortical carcinoma: surgical and oncologic outcome in 152 patients. Eur Urol 2010;58:609–615.
Jin LX, Sanford DE, Squires MH, 3rd, et al.: Interaction of Postoperative Morbidity and Receipt of Adjuvant Therapy on Long-Term Survival After Resection for Gastric Adenocarcinoma: Results From the U.S. Gastric Cancer Collaborative. Ann Surg Oncol 2016.
Leboulleux S, Deandreis D, Al Ghuzlan A, et al.: Adrenocortical carcinoma: is the surgical approach a risk factor of peritoneal carcinomatosis? Eur J Endocrinol 2010;162:1147–1153.
Carnaille B: Adrenocortical carcinoma: which surgical approach? Langenbecks Arch Surg 2012;397:195–199.
Sgourakis G, Lanitis S, Kouloura A, et al.: Laparoscopic versus Open Adrenalectomy for Stage I/II Adrenocortical Carcinoma: Meta-Analysis of Outcomes. J Invest Surg 2015;28:145–152.
Zini L, Porpiglia F, Fassnacht M: Contemporary Management of Adrenocortical Carcinoma. European Urology 2011;60:1055–1065.
Kirshtein B, Yelle JD, Moloo H, Poulin E: Laparoscopic adrenalectomy for adrenal malignancy: a preliminary report comparing the short-term outcomes with open adrenalectomy. J Laparoendosc Adv Surg Tech A 2008;18:42–46.
Fassnacht M, Johanssen S, Quinkler M, et al.: Limited prognostic value of the 2004 International Union Against Cancer staging classification for adrenocortical carcinoma: proposal for a Revised TNM Classification. Cancer 2009;115:243–250.
Beuschlein F, Weigel J, Saeger W, et al.: Major prognostic role of Ki67 in localized adrenocortical carcinoma after complete resection. J Clin Endocrinol Metab 2015;100:841–849.
Weiss LM: Comparative histologic study of 43 metastasizing and nonmetastasizing adrenocortical tumors. Am J Surg Pathol 1984;8:163–169.
Author Contribution
Each author listed in the following manuscript contributed significantly to the concept and/or design of this work in the form of data acquisition, analysis, and interpretation of results. Each author was involved in the drafting or revision of the intellectual content included in this manuscript and provided final approval of the current version. All authors agree to be accountable for the following work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures and Funding Sources
None.
Rights and permissions
About this article
Cite this article
Lee, C.W., Salem, A.I., Schneider, D.F. et al. Minimally Invasive Resection of Adrenocortical Carcinoma: a Multi-Institutional Study of 201 Patients. J Gastrointest Surg 21, 352–362 (2017). https://doi.org/10.1007/s11605-016-3262-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3262-4