Abstract
Background
Surgical resection with negative margins is the treatment of choice for adrenocortical carcinoma (ACC). This study was undertaken to determine factors associated with negative resection margins.
Methods
National Cancer Database was queried from 2010 to 2016 to identify patients with AJCC/ENSAT Stage I–III ACC who underwent adrenalectomy. Patient, tumor, facility, and operative characteristics were compared by margin status (positive—PM or negative—NM) and operative approach (open—OA, laparoscopic—LA, or robotic—RA). Multivariable logistic regression was used to identify factors associated with PM.
Results
Eight hundred and eighty-one patients were identified, of which 18.4% had PM and 81.6% had NM. Patients with advanced pathologic T stage and pathologic N1 stage were more likely to have PM (vs. NM) (T3, 49.7% vs. 24.8%, p < 0.01; T4, 26.2% vs. 10.0%, p < 0.01; N1, 6.7% vs. 3.5%, p < 0.01). Patients undergoing OA (vs. LA and RA) were more likely to have advanced clinical T stage (T4, 16.6% vs. 5.7% vs. 7.8%, p < 0.01) and larger tumors (> 6 cm, 84.6% vs. 64.1% vs. 62.3%, p < 0.01). High-volume centers (≥ 5 cases) were more likely to utilize OA. Patients undergoing LA (vs. RA) were more likely to require conversion to open (20.3% vs. 7.8%, p = 0.011). On multivariable analysis, factors associated with higher odds of PM included T3 disease (OR 7.02, 95% CI 2.66–18.55), T4 disease (OR 10.22, 95% CI 3.66–28.53), and LA (OR 1.99, 95% CI 1.28–3.09). High-volume centers were associated with lower odds of PM (OR 0.67, 95% CI 0.45–0.98). There was no significant difference in margin status between OA and RA (OR 1.44, 95% CI 0.71–2.90).
Conclusion
Centers with higher ACC case volumes have lower odds of PM and utilize OA more often. LA is associated with higher odds of PM, whereas RA is not. These factors should be considered when planning the operative approach for ACC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adrenocortical carcinoma (ACC) is a rare and aggressive endocrine malignancy with a poor prognosis. It has an annual incidence of 200 cases per year and a 5-year survival rate of 15–44% [1, 2]. The standard of care for patients as recommended by the American Joint Committee on Cancer (AJCC) and the European Network for the Study of Adrenal Tumors (ENSAT) Stage I–III ACC (no evidence of distant metastases) is adrenalectomy with R0 resection, as it is the only therapy that is potentially curative [3,4,5]. This often entails en bloc resection of adjacent involved organs for locally advanced disease.
The National Comprehensive Cancer Network (NCCN) recommends open adrenalectomy as the standard of care for ACC. These guidelines state that it is important to “achieve negative margins and avoid breaching the tumor capsule,” and cite an “increased risk for local recurrence and peritoneal spread when done laparoscopically,” although this may be biased by comparing the early surgeon’s experience with laparoscopic vs. open adrenalectomy [6,7,8,9].
Although laparoscopic adrenalectomies for ACC have been associated with unfavorable outcomes, robotic adrenalectomies for ACC have not been assessed in the literature. The goal of our study was to use a national registry of cancer patients to identify risk factors for positive margin status after adrenalectomy for ACC, specifically focusing on operative approach and institutional operative experience.
Methods
The National Cancer Database (NCDB) is a clinical oncology database sponsored by the American College of Surgeons and the American Cancer Society. It captures data from more than 1,500 Commission on Cancer (CoC)-accredited facilities and represents over 70 percent of newly diagnosed cancer cases nationwide. These facilities are categorized as “Community Cancer Program” (CCP), “Comprehensive Community Cancer Program” (CCCP), “Academic/Research Program” (ARP), and “Integrated Network Cancer Program” (INCP) by the CoC. CCPs treat 100–500 newly diagnosed cancer cases each year and may refer out a portion of diagnostic or treatment procedures. CCCPs treat 500 or more newly diagnosed cancer cases each year and provide a full range of diagnostic and treatment services on-site or by referral. ARPs treat 500 or more newly diagnosed cancer cases each year and participate in postgraduate medical education in at least four specialties. INCPs are organizations with multiple facilities that provide integrated cancer care and comprehensive services. For this study, CCPs and CCCPs were classified jointly as “Community” institutions, and ARPs and INCPs were classified jointly as “Academic” institutions.
The National Cancer Database (NCDB) was queried from 2010 to 2016 for all patients with the International Classification of Diseases, 10th edition, Clinical Modification (ICD-10-CM) diagnosis code for malignant neoplasm of the cortex of the adrenal gland (C74.0) with the ICD for Oncology, 3rd edition (ICD-O-3) histology code for adrenal cortical carcinoma (8370) who underwent an adrenalectomy. Only patients with ACC as the primary/only cancer were included (North American Association of Central Cancer Registries #560, code 00 or 01). Patients whose treatment was not performed at the treating facility were excluded from the study (NAACCR #610, code 00). Patients with AJCC or ENSAT Stage IV disease, i.e., metastatic (M1) disease, and those who underwent neoadjuvant systemic therapy were also excluded. Operative approach was only available from 2010 and onward, thus patients undergoing adrenalectomy from 2004 to 2009 were excluded.
Data regarding patient age, gender, race/ethnicity, Charlson–Deyo score, insurance status, location, and income quartile were obtained. Tumor characteristics including clinical and pathologic T and N stages, tumor size, and laterality were assessed. Data regarding operative approach (open—OA, laparoscopic—LA, or robotic—RA) and conversion rates were obtained. Additionally, facilities were stratified by case volume over the entire study period. Prior studies have defined “high-volume” as the facilities in 75th to 90th percentile for case volume [10, 11]. In this study, a facility performing 5 cases over the entire study period corresponded to the 85th percentile for facility case volume. Thus, the facilities were stratified into two groups: 1–4 cases in the entire study period, classified as low volume, and 5 or more cases in the entire study period, classified as high volume.
Patient, tumor, facility, and operative characteristics were compared by operative approach and margin status (positive—PM or negative—NM). Variables were described as median (interquartile ratio) for nonparametric continuous variables and n (%) for categorical variables. Univariate analysis was performed with the Mann–Whitney U test for nonparametric continuous variables and Pearson’s Chi-squared test for categorical variables. Statistically significant variables on univariate analysis and variables associated with operative approach and experience were used in a backward stepwise logistic regression to identify independent factors associated with PM. The regression model’s goodness of fit was tested with the Hosmer–Lemeshow test and the C statistic. In the Hosmer–Lemeshow test, p value greater than 0.05 signifies that the model fits the observed data. The C statistic represents the area under the receiver-operating curve (ROC).
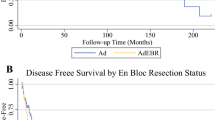
Overall survival was compared between patients with PM and NM using the Kaplan–Meier estimate, using the log-rank test to assess for statistical significance. Subgroup analysis by T stage and margin status for overall survival was also performed using the Kaplan–Meier estimate.
Results
A total of 881 patients with AJCC or ENSAT Stage I–III ACC who underwent surgical resection without neoadjuvant therapy were identified (Table 1). The majority of cases were performed at Academic centers (70%), and approximately half of the cases (48.9%) were performed at high-volume centers. There were 407 low-volume centers: 119 centers performed 1 case, 111 centers performed 2 cases, 88 centers performed 3 cases, and 89 centers performed 4 cases in the entire study period. The majority of cases were performed via OA (65%), followed by LA (26.2%) and RA (8.7%). OA rates decreased from 72.9% of all cases in 2010 to 64.4% of all cases in 2016. LA rates remained similar over time, from 22.1% in 2010 to 21.2% in 2016. RA rates increased over time, from 5.0% in 2010 to 14.4% in 2014 (Fig. 1). In Academic centers from 2010 to 2016, OA decreased from 75.0 to 70.2%, LA decreased from 19.6 to 18.1%, and RA increased from 5.4 to 11.7%, respectively. In Community centers from 2010 to 2016, OA decreased from 70.2 to 51.4%, LA increased from 25.5 to 29.7%, and RA increased from 4.3 to 18.9%, respectively.
Patient demographics, tumor characteristics, and operative outcomes between OA, LA, and RA were compared (Table 1). Patients undergoing OA (vs. LA and RA) had fewer comorbidities (Charlson–Deyo Score 2, 2.8% vs. 4.8% vs. 5.2%; Charlson–Deyo Score 3, 1.0% vs. 2.6% vs. 3.9%, p = 0.022) and were less likely to live in the highest income neighborhoods (31.8% vs. 42.4% vs. 41.6% p = 0.006). Patients undergoing OA (vs. LA and RA) were more likely to receive treatment at an Academic center (72.6% vs. 67.0% vs. 59.2%, p = 0.029) or at a high-volume center (52.9% vs. 45.0% vs. 31.2%, p = 0.013). There were no differences in age, sex, race, or insurance status between the groups.
There were no differences in tumor laterality between the groups. Patients undergoing OA (vs. LA and RA) were more likely to have advanced pathologic T stage (T4, 16.6% vs. 5.7% vs. 7.8%, p < 0.01) and tumors greater than 6 cm in size (84.6% vs. 64.1% vs. 62.3%, p < 0.01). The rates of PM for OA, LA, and RA on univariate analysis were not statistically different, at 16.8%, 22.5%, and 18.6%, respectively (p = 0.186). Patients undergoing LA (vs. RA) were more likely to require conversion to open (20.3% vs. 7.8%, p = 0.011). PM was present in 18.5% of LA who did not convert to open and 29.8% of LA who converted to open (p = 0.09). PM was present in 12.7% of RA who did not convert to open and 66.7% of RA who converted to open (p < 0.01).
Patient demographics, tumor characteristics, treatment regimen, and operative outcomes were compared between the PM and NM cohorts (Table 2). Overall, PM was reported in 149 (18.4%) patients and NM was reported in 659 (81.6%) patients (Table 2). There was no significant difference in margin status by demographic factors, such as age, gender, race, Charlson–Deyo score, or insurance status. Patients with PM were more likely to have advanced T stage (pT3, 49.7% vs. 24.8%, p < 0.01; pT4, 26.2% vs. 10.0%, p < 0.01). There was no significant difference in margin status by tumor size, laterality, operative approach, or case volume. Patients with PM (vs. NM) were more likely to get adjuvant chemotherapy (42.3% vs. 33.1%, p < 0.01) and radiation therapy (39.6% vs. 15.8%, p = 0.033).
On multivariate analysis, factors associated with higher odds of PM included pT3 disease (OR 7.02, 95% CI 2.66–18.55), pT4 disease (OR 10.22, 95% CI 3.66–28.53), and LA (compared to OA) (OR 1.99, 95% CI 1.28–3.09) (Table 3). The odds of PM were similar for RA compared to OA (OR 1.44, 95% CI 0.71–2.91). High-volume centers were associated with lower odds of PM (OR 0.67, 95% CI 0.45–0/98). The model fits the observed data well as tested using the C statistic (C = 0.759) and the Hosmer–Lemeshow test (p = 0.801).
Overall survival was significantly shorter for patients with PM vs. NM (25.4 vs. 78.2 months, p < 0.01) (Fig. 2a). This significant difference between survival with PM vs. NM was upheld throughout all stratification schema, including: 1) by T stage (T1, 46.7 vs. 106.1 months, p < 0.01; T2, 85.4 vs. 101.9 months, p < 0.01; T3, 64.7 vs. 74.1 months, p < 0.01; T4, 24.3 vs. 33.2 months, p < 0.01) (Fig. 2b), 2), by operative approach (OA, 22.5 vs. 70.8 months, p < 0.01; LA, 16.5 vs. 81.8 months, p < 0.01; RA, undefined vs. undefined, p = 0.045) (Fig. 2c), and 3), and by case volume (1–4 cases, 24.6 vs. 71.0 months, p < 0.01; 5 or more cases, 25.5 vs. 84.5 months, p < 0.01) (Fig. 2d).
Discussion
The treatment of choice for non-metastatic ACC is complete surgical resection with R0 margins. Current guidelines recommend OA in order to minimize the risk of tumor spillage and positive margin status, both of which are associated with higher rates of locoregional recurrence and worse survival [9, 12]. In our study, the proportion of patients with ACC undergoing LA or RA increased over time. Patients undergoing OA were more likely to have tumors > 6 cm in size and extra-adrenal extension with invasion into surrounding organs (pathologic T4) and were more likely to be performed at Academic or high-volume centers, as compared to patients undergoing LA and RA, both of which raise the possibility of selection bias and emphasize the need for appropriate patient selection for surgical approach. On univariate analysis, rates of PM were similar between OA, LA, and RA. However, after adjusting for tumor size, pathologic T stage, and center experience with ACC, LA was associated with higher odds of PM compared to OA, while RA was not. Our study provides preliminary data suggesting that RA can be safely performed without a higher risk of PM with careful patient selection.
To our knowledge, this is the first study in the literature that evaluates differences between robotic, laparoscopic, and open approaches for ACC. Reports on RA are mostly limited to case series describing the technical aspects and outcomes for benign adrenal disease [13,14,15]. Studies on ACC typically group robotic surgery with laparoscopic surgery together as “minimally invasive surgery” or exclude robotic surgery altogether [16, 17]. Our study shows that RA is not associated with a higher risk of PM compared to OA for ACC.
Why was LA associated with higher odds of PM in our study, while RA was not? The NCDB does not contain enough details on surgical technique to answer this question. However, other studies in the literature have compared differences in technique for performing an adrenalectomy between RA and LA which may explain this difference. For example, Gokceimam et al. compared intraoperative video recordings of 30 LA to 30 RA and found significantly superior metrics of surgical flow and economy of motion for RA, even when stratified by tumor size [18]. These included detailed measures, such as operative time, quality of camera control, instrument movement, tissue trauma from traction, quality of tumor dissection, range of movement around the tumor, and bleeding. Another study from the same group found lower rates of microcapsular disruption with RA compared to reported rates in the literature for LA [19]. These studies suggest that RA may offer technical advantages over LA. In our study, LA was associated with a significantly higher rate of conversion to open compared to RA. Interestingly, LA requiring conversion to open resulted in a slightly higher but nonsignificant difference in the rate of PM, while RA requiring conversion to open resulted in a significantly higher rate of PM. A recent study by Delozier et al. also identified conversion to open in minimally invasive surgery (MIS) as a prognostic factor for poor survival, although the rates of PM were not statistically significantly increased in this population [20]. Their study did not specifically assess differences between robotic and laparoscopic approaches and instead grouped these two approaches together as MIS. A similar study on risk factors for PM for ACC by Skertich et al. included metastatic ACC in their analysis and found that extra-adrenal extension (T3/T4) and distant metastases were associated with incomplete resection [21]. They found no difference in rates of PM by surgical approach on univariate analysis. However, like Delozier et al., they combined robotic surgery with laparoscopic surgery and did not perform multivariate analyses to adjust for tumor size or pathologic T stage [20, 21].
Our study also evaluates the impact of operative volume on rates of PM. The top 15% of hospitals by case volume—corresponding to 5 or more cases over the entire study period—account for nearly half of the total operative volume in the nation and an even larger share of patients with T4 ACC undergoing adrenalectomy (52.5%). These high-volume centers were associated with significantly lower odds of PM. In contrast, low-volume centers, of which 119 performed 1 case, 111 performed 2 cases, and 88 performed 3 cases over seven years, had higher odds of PM. This finding is consistent with other single-institution studies which have shown that treatment at high-volume centers is associated with higher rates of operative management, higher utilization of adjuvant therapy, and improved outcomes for ACC [10, 22]. Our study suggests that patients with ACC may be better served by referrals to regional high-volume centers with more experience managing ACC.
Based on our findings, surgeons should cautiously approach patients with large, irregular tumors concerning for ACC, especially those with extra-adrenal extension, as these factors represent the strongest risk factors for PM. These patients may be best served with an open approach. Although our multivariable regression does show that the odds of PM are similar between RA and OA, independent of tumor size, it is still important to note that RA were more likely be performed on smaller tumors with lower T stages in our study.
If a surgeon finds an unexpectedly challenging case during LA or RA, several techniques can help surgeons identify safe dissection planes to maintain negative margins. For example, indocyanine green has been used to delineate the vascular anatomy of adrenal neoplasms and enhance the contrast between tumor and normal tissue [23,24,25]. Intraoperative ultrasound has also been used to identify key structures and safe plane of dissections, resulting in lower rates of complications and conversion to open [26]. A hand-assist port may provide additional tactile feedback over laparoscopy alone; however, this is generally very rarely utilized in practice. These adjuncts should not delay conversion to open if indicated.
Our study has some important limitations related to the retrospective nature of a national registry. The NCDB does not accurately describe clinically significant factors that may affect margin status, such as the extent of extra-adrenal invasion into adjacent organs. Details regarding operative approach are only available from 2010 and onward, which reduces the sample size of the study. The NCDB does not differentiate between transabdominal vs. retroperitoneal approaches, nor does it differentiate between surgeons who perform hand-assisted laparoscopy and those who stay completely laparoscopic, which may confound the outcomes assessed in our study. The sample size for RA was small (n = 77) in comparison to that of OA and LA, although to our knowledge, this is the largest study on RA for ACC in the literature. Most importantly, the data are susceptible to bias. In many cases, the diagnosis of ACC is not known preoperatively, and this may affect the operative approach, especially for smaller tumors. In addition, surgeons may be less inclined to perform minimally invasive adrenalectomies on larger tumors with extra-adrenal extension, leading to selection bias. Finally, the database also lacks information on recurrence rates and disease-free survival, which are important measures for oncologic outcomes. Overall, the limitations of the NCDB and the rarity of the disease stress the importance of establishing multi-institutional collaboratives to prospectively study the surgical treatment of adrenocortical carcinoma.
Conclusion
Laparoscopic adrenalectomy for ACC is associated with higher odds of positive margin status and conversion to open. Robotic and open adrenalectomies had similar odds of positive margins, although most robotic adrenalectomies were performed on smaller tumors, and the sample size for robotic operations was low. Centers with higher case volumes for ACC are more likely to utilize open surgery in the management of ACC and have lower odds of positive margin status. These factors should be considered when planning the operative approach for ACC.
References
Ayala-Ramirez M, Jasim S, Feng L, Ejaz S, Deniz F, Busaidy N, Waguespack SG, Naing A, Sircar K, Wood CG, Pagliaro L, Jimenez C, Vassilopoulou-Sellin R, Habra MA (2013) Adrenocortical carcinoma: clinical outcomes and prognosis of 330 patients at a tertiary care center. Eur J Endocrinol 169:891–899
Kebebew E, Reiff E, Duh QY, Clark OH, McMillan A (2006) Extent of disease at presentation and outcome for adrenocortical carcinoma: have we made progress? World J Surg 30:872–878
Schulick RD, Brennan MF (1999) Long-term survival after complete resection and repeat resection in patients with adrenocortical carcinoma. Ann Surg Oncol 6:719–726
Icard P, Goudet P, Charpenay C, Andreassian B, Carnaille B, Chapuis Y, Cougard P, Henry JF, Proye C (2001) Adrenocortical carcinomas: surgical trends and results of a 253-patient series from the French Association of Endocrine Surgeons study group. World J Surg 25:891–897
Tella SH, Kommalapati A, Yaturu S, Kebebew E (2018) Predictors of survival in adrenocortical carcinoma: an analysis from the National Cancer Database. J Clin Endocrinol Metab 103:3566–3573
Gonzalez RJ, Shapiro S, Sarlis N, Vassilopoulou-Sellin R, Perrier ND, Evans DB, Lee JE (2005) Laparoscopic resection of adrenal cortical carcinoma: a cautionary note. J Surgery 138:1078–1085
Leboulleux S, Deandreis D, Al Ghuzlan A, Aupérin A, Goéré D, Dromain C, Elias D, Caillou B, Travagli JP, De Baere T, Lumbroso J, Young J, Schlumberger M, Baudin E (2010) Adrenocortical carcinoma: is the surgical approach a risk factor of peritoneal carcinomatosis? Eur J Endocrinol 162:1147–1153
Miller BS, Ammori JB, Gauger PG, Broome JT, Hammer GD, Doherty GM (2010) Laparoscopic resection is inappropriate in patients with known or suspected adrenocortical carcinoma. World J Surg 34:1380–1385
National Comprehensive Cancer Network Neuroendocrine and Adrenal Tumors (Version 2.2020).
Gratian L, Pura J, Dinan M, Reed S, Scheri R, Roman S, Sosa JA (2014) Treatment patterns and outcomes for patients with adrenocortical carcinoma associated with hospital case volume in the United States. Ann Surg Oncol 21:3509–3514
Park HS, Roman SA, Sosa JA (2009) Outcomes from 3144 adrenalectomies in the United States: which matters more, surgeon volume or specialty? Arch Surg 144:1060–1067
Margonis GA, Kim Y, Prescott JD, Tran TB, Postlewait LM, Maithel SK, Wang TS, Evans DB, Hatzaras I, Shenoy R, Phay JE, Keplinger K, Fields RC, Jin LX, Weber SM, Salem A, Sicklick JK, Gad S, Yopp AC, Mansour JC, Duh QY, Seiser N, Solorzano CC, Kiernan CM, Votanopoulos KI, Levine EA, Poultsides GA, Pawlik TM (2016) Adrenocortical carcinoma: impact of surgical margin status on long-term outcomes. Ann Surg Oncol 23:134–141
Brunaud L, Ayav A, Zarnegar R, Rouers A, Klein M, Boissel P, Bresler L (2008) Prospective evaluation of 100 robotic-assisted unilateral adrenalectomies. Surgery 144:995–1001
Agcaoglu O, Aliyev S, Karabulut K, Siperstein A, Berber E (2012) Robotic vs laparoscopic posterior retroperitoneal adrenalectomy. Arch Surg 147:272–275
Hupe MC, Imkamp F, Merseburger AS (2017) Minimally invasive approaches to adrenal tumors: an up-to-date summary including patient position and port placement of laparoscopic, retroperitoneoscopic, robot-assisted, and single-site adrenalectomy. Curr Opin Urol 27:56–61
Autorino R, Bove P, De Sio M, Miano R, Micali S, Cindolo L, Greco F, Nicholas J, Fiori C, Bianchi G, Kim FJ, Porpiglia F (2016) Open versus laparoscopic adrenalectomy for adrenocortical carcinoma: a meta-analysis of surgical and oncological outcomes. Ann Surg Oncol 23:1195–1202
Hu X, Yang W-X, Shao Y-X, Dou W-C, Xiong S-C, Li X (2020) Minimally invasive versus open adrenalectomy in patients with adrenocortical carcinoma: a meta-analysis. Ann Surg Oncol 27:3858–3869
Gokceimam M, Akbulut S, Erten O, Kahramangil B, Kim YS, Li P, Berber E (2021) An intra-operative video comparison of laparoscopic versus robotic transabdominal lateral adrenalectomy. Int J Med Robot Comput Assist Surg 17:e2203
Gokceimam M, Kahramangil B, Akbulut S, Erten O, Berber E (2021) Robotic posterior retroperitoneal adrenalectomy: patient selection and long-term outcomes. Ann Surg Oncol 28:7497–7505
Delozier OM, Stiles ZE, Deschner BW, Drake JA, Deneve JL, Glazer ES, Tsao MW, Yakoub D, Dickson PV (2021) Implications of conversion during attempted minimally invasive adrenalectomy for adrenocortical carcinoma. Ann Surg Oncol 28:492–501
Skertich NJ, Tierney JF, Chivukula SV, Babazadeh NT, Hertl M, Poirier J, Keutgen XM (2020) Risk factors associated with positive resection margins in patients with adrenocortical carcinoma. Am J Surg 220:932–937
Dickson PV, Kim L, Yen TWF, Yang A, Grubbs EG, Patel D, Solorzano CC (2018) Adjuvant and neoadjuvant therapy, treatment for advanced disease, and genetic considerations for adrenocortical carcinoma: an update from the SSO endocrine and head and neck disease site working group. Ann Surg Oncol 25:3453–3459
DeLong JC, Chakedis JM, Hosseini A, Kelly KJ, Horgan S, Bouvet M (2015) Indocyanine green (ICG) fluorescence-guided laparoscopic adrenalectomy. J Surg Oncol 112:650–653
Lerchenberger M, Gündogar U, Al Arabi N, Gallwas JKS, Stepp H, Hallfeldt KKJ, Ladurner R (2020) Indocyanine green fluorescence imaging during partial adrenalectomy. Surg Endosc 34:2050–2055
Arora E, Bhandarwar A, Wagh A, Gandhi S, Patel C, Gupta S, Talwar G, Agarwal J, Rathore J, Chatnalkar S (2018) Role of indo-cyanine green (ICG) fluorescence in laparoscopic adrenalectomy: a retrospective review of 55 Cases. Surg Endosc 32:4649–4657
Sebastian M, Rudnicki J (2020) Recommendation for laparoscopic ultrasound guided laparoscopic left lateral transabdominal adrenalectomy. Gland Surg 9:689–694
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Tseng, Diperi, Gonsalves, Chen, Ben-Shlomo, Shouhed, Phillips, Burch, and Jain have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tseng, J., Diperi, T., Gonsalves, N. et al. Operative approach and case volume are associated with negative resection margins for adrenocortical carcinoma. Surg Endosc 36, 9288–9296 (2022). https://doi.org/10.1007/s00464-022-09167-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09167-0