Abstract
Background and Aims
The impact of gender on the development of chronic ileal pouch disorders following ileal pouch-anal anastomosis (IPAA) has not been evaluated. This study was aimed to assess the association between gender and pouch outcomes.
Methods
Comparisons of long-term pouch outcomes between male and female patients were performed using both univariate and multivariate analyses.
Results
Of all patients enrolled (n = 1564), 881(56.3 %) were males. Male patients were older at the time of inflammatory bowel disease (IBD) diagnosis and pouch construction. The frequencies of neoplasia as the indication for colectomy and significant comorbidity were higher in males, while fewer male patients had IBD-related extra-intestinal manifestations or concurrent autoimmune disorders. There was no significant difference between the genders in other clinicopathological characteristics. More male patients (n = 144, 16.3 %) developed chronic antibiotic-refractory pouchitis (CARP) than females (n = 73, 10.7 %) (P = 0.001). Seventy-four males (8.4 %) had ileal pouch anastomotic sinus versus 22 female patients (3.2 %) (P < 0.001). Multivariate logistic regression analyses confirmed the association between male gender and CARP (odds ratio (OR) 1.64, 95 % confidence interval (CI) 1.21–2.24, P = 0.002) and male gender and ileal pouch anastomotic sinus (OR 2.85, 95 % CI 1.48–5.47, P = 0.002). After a median follow-up of 9.0 (interquartile range 4.0–14.0) years, pouch failed in a total of 126 patients (8.1 %). No significant difference was identified between male and female patients in pouch failure (P = 0.61).
Conclusions
Among the pouch patients referred to our subspecialty Pouch Center, male patients were found to have an increased risk for the CARP and ileal pouch sinus. The pathogenic mechanisms of the association warrant further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA), first described by Parks and Nicholls in 1978,1 has become the surgical procedure of choice for patients with medically refractory ulcerative colitis (UC) or indeterminate colitis (IC), familial adenomatous polyposis (FAP), or a highly selected subset of patients with Crohn’s disease (CD) of the colon. Although IPAA reliably produces excellent functional outcomes as well as an improved patients’ health-related quality of life (QOL),2 – 5 the procedure is technically challenging and adverse postoperative sequelae are common. Previous studies have shown that as high as 60 % of patients undergoing this procedure are likely to experience at least one IPAA-related adverse event.2 , 6.
Our Pouch Center has served as a major tertiary referral center since its establishment in 2002, taking care of patients with complex ileal pouch disorders as well as those with routine pouch cancer surveillance. In 2008, our group proposed a classification of ileal pouch disorders and associated adverse events after restorative proctocolectomy, encompassing irritable pouch syndrome (IPS), acute pouchitis, chronic antibiotic-refractory pouchitis (CARP), cuffitis, CD of the pouch, and pouch procedure-related complications.7 Since then, the management and the risk factors associated with various pouch disorders have been extensively studied. However, the impact of gender on the specific outcomes of IPAA has not been well evaluated. In our clinical practice, we have noticed that the majority of patients with chronic pouchitis or presacral sinus were male. We hypothesized that male patients may be vulnerable to the development of certain pouch disorders. Therefore, we designed this study to systematically assess the impact of gender on the two most challenging pouch disorders, CARP and pouch anastomotic sinus.
Patients and Methods
Patients
This study was approved by the Cleveland Clinic Institutional Review Board (IRB). All eligible ileal pouch patients followed up at our Pouch Center from January 2002 to January 2014 were identified from the IRB-approved registry. Demographics, clinicopathological variables, and ileal pouch disorders and outcomes were all prospectively maintained in the registry. Both paper charts and electronic medical records were carefully reviewed when necessary.
Inclusion and Exclusion Criteria
In order to be included in the study, patients needed to meet all the following inclusion criteria: (1) have an ileal pouch, (2) have regular follow-up at the Pouch Center, and (3) have inflammatory bowel disease (IBD) as underlying diagnosis. Ileal pouch patients with underlying FAP or other bowel diseases were excluded from this study.
Patient Groups
In this study, patients were divided into two groups based on patients’ gender.
Definition of Variables
Demographic and clinicopathological variables were defined as follows: duration of IBD—the time interval from the date of IBD diagnosis (i.e., preoperative diagnosis of UC, IC, or CD) to the date of pouch surgery; active smoking—consumption of more than seven cigarettes per week for at least 6 months prior to the data entry; ex-smoking—cessation of smoking 6 months prior to data entry; family history of IBD—one or more of the first-degree (parents, offspring, or siblings of the index patients) or second-degree relatives who had IBD; extensive colitis—endoscopic, macroscopic, or microscopic disease extending proximal to the splenic flexure; IC—histopathological diagnosis on proctocolectomy specimens that defied a clear distinction between CD and UC; Crohn’s colitis—colitis with granulomas in the absence of related perianal, small bowel, and upper gastrointestinal lesions; extra-intestinal manifestations (EIMs)—including the presence of arthralgia or arthropathy, pyoderma gangrenosum, erythema nodosum, primary sclerosing cholangitis (PSC), IBD-related ocular lesions, and thromboembolic events; autoimmune disorders—adult-onset asthma, type 1 diabetes, rheumatoid arthritis, autoimmune thyroid diseases (including Grave’s disease and Hashimoto’s thyroiditis), psoriasis, systemic lupus erythematosus, autoimmune hemolytic anemia, vitiligo, celiac disease, pernicious anemia, idiopathic thrombocytopenic purpura, and multiple sclerosis; significant comorbidities—congestive heart failure, coronary bypass surgery, chronic obstructive pulmonary diseases, renal stone of insufficiency, non-gastrointestinal cancer, stroke, and liver failure; and the use of anti-tumor necrosis factor (TNF) biologics—the use of infliximab, or adalimumab, or certolizumab pegol for IBD or concurrent autoimmune disorders.
Outcome Measurement
Pouch failure was defined as the requirement for permanent diversion, pouch revision, or pouch excision. Pouch procedure-related complications were defined as conditions which were believed to be attributed to surgical techniques. Those conditions included pouch sinuses, fistulae, anastomotic leak with pelvic abscess, non-CD severe anastomotic or small bowel strictures, efferent or afferent limb syndromes, pouch ischemia, pouch prolapsed, and long or twisted pouch. CARP was defined by a modified Pouchitis Disease Activity Index ≥ 5 points and symptoms lasting 4 weeks or more and failed to respond to a 4-week course of single antibiotic therapy (ciprofloxacin, metronidazole, or tinidazole).8 CD of the pouch was diagnosed based on our previously published criteria,9 i.e., the presence of non-surgery-related perianal fistula or inflammation or ulcerations at the pre-pouch neo-terminal ileum or small bowel in the absence of non-steroidal anti-inflammatory drug (NSAID) use or granulomas on histology. Cuffitis was defined as inflammation of the rectal cuff or anal transitional zone (ATZ) on endoscopy and history without or with minimal concurrent inflammation of the pouch.
Statistical Analysis
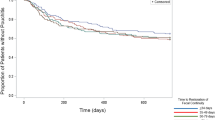
Descriptive statistics were computed for all variables. These included means and standard deviations (SDs) or medians and interquartile ranges (IQRs) for continuous factors and frequencies for categorical factors. Comparisons of the distribution of clinicopathological characteristics between the male and female patients were made by using the two-tailed t test (or Wilcoxon rank sum test as appropriate) for continuous variables and chi-squared test (or the Fisher exact test as appropriate) for categorical variables. The impact of gender on pouch failure was depicted with Kaplan–Meier curves with the log-rank test. Both univariate and multivariate analyses of risk factors associated with the development of ileal pouch disorders were constructed using the logistic regression analysis. P value less than 0.05 was considered statistically significant.
Results
Patient Demographics
A total of 1564 eligible patients were identified from our registry, including 881 (56.3 %) males and 683 (43.7 %) females. Male patients were found to be older at the time of IBD diagnosis (26.8 ± 12.9 vs. 24.3 ± 11.6 years, P < 0.001) and pouch construction (36.7 ± 14.1 vs. 33.8 ± 13.4 years, P < 0.001) than that in their female counterparts (Table 1). The mean body mass index (BMI) at the first Pouch Center visit was 26.1 ± 4.6 kg/m2 for males versus 24.2 ± 5.6 kg/m2 for females (P < 0.001). The frequencies of neoplasia as the indication for colectomy (15.4 vs. 9.7 %, P = 0.001) and significant comorbidity (12.0 vs. 8.1 %, P = 0.01) were higher in males, while fewer male patients had IBD-related EIM (34.0 vs. 41.9 %, P = 0.002) and autoimmune disorders (12.1 vs. 17.3 %, P = 0.004). There was no significant difference in other clinicopathological characteristics between male and female patients (Table 1).
Ileal Pouch Disorders and Pouch Failure
Of all the patients seen at our Pouch Center, 1383 patients (88.4 %) were found to have at least one ileal pouch disorder. The ileal pouch disorders included IPS (n = 199, 12.7 %), acute pouchitis (n = 254, 16.2 %), CARP (n = 217, 13.9 %), cuffitis (n = 143, 9.1 %), CD of the pouch (n = 282, 18.0 %), pouch procedure-related complications (n = 274, 17.5 %), and animus (n = 14, 0.9 %) (Table 2). Comparison analysis showed that more male patients developed CARP than females (16.3 vs. 10.7 %, P = 0.001). Although the overall rate of pouch procedure-related complications was comparable between the two groups (16.5 vs. 18.9 %, P = 0.21), subgroup analyses demonstrated that male patients were more likely to have pouch anastomotic sinus (8.4 vs. 3.2 %, P < 0.001). Male patients less frequently suffered from pouch fistula (1.2 vs. 4.4 %, P < 0.001); however, no significant difference was identified between the two genders in fistula other than PVF (1.2 vs. 2.0 %, P = 0.21). There was no significant difference between male and female patients in other ileal pouch disorders (Table 2).
After a median follow-up of 9.0 (interquartile range 4.0–14.0) years, pouch failed in a total of 126 patients (8.1 %). No significant difference was identified between male (n = 68, 7.7 %) and female (n = 58, 8.5 %) patients in pouch failure (P = 0.58) (Table 2). Similar results were also obtained using the Kaplan–Meier curve analysis (log-rank test, P = 0.61).
Male Gender Is Associated with a Higher Risk for CARP
Univariate logistic regression analysis revealed that male gender was significantly associated with a higher risk for the development of CARP, with an odds ratio (OR) of 1.63 (95 % confidence interval (CI) 1.21–2.21, P = 0.001) (Table 3). Of the clinicopathological variables, other potential risk factors for CARP identified by the univariate analysis included significant comorbidities (P = 0.021), PSC (P < 0.001), non-PSC IBD-related EIM (P = 0.018), autoimmune disorders (P = 0.026), and pouch configurations (P = 0.006) (Table 3). The association between male gender and the risk for CARP was then confirmed by the multivariate logistic regression analysis (OR 1.64, 95 % CI 1.21–2.24, P = 0.002) after adjusting for significant comorbidities, PSC, non-PSC IBD-related EIM, autoimmune disorders, and pouch configurations (Table 4).
Male Gender Is Associated with a Higher Risk for Ileal Pouch Sinus
In the univariate logistic regression analysis, male gender was shown to have a higher risk for ileal pouch anastomotic sinus (OR 2.76, 95 % CI 1.69–4.48, P < 0.001) (Table 3). Univariate analysis demonstrated that other factors associated with the development of ileal pouch sinus were family history of IBD (P = 0.036), preoperative use of anti-TNF biologics (P = 0.02), and the type of anastomosis (P = 0.009) (Table 3). The association between male gender and the risk for ileal pouch anastomotic sinus was then further identified by the multivariate logistic regression analysis after adjusting for family history of IBD, preoperative use of anti-TNF biologics, and the type of anastomosis, with an OR of 2.85 (95 % CI 1.48–5.47) (P = 0.002) (Table 4).
Discussion
Previous studies showed that the clinical and biological behaviors of autoimmune- or inflammatory-related diseases were strongly related to patients’ gender.10 , 11 The gender differences in the presentation and disease course in patients with IBD have also been reported.12 – 14 However, data with respect to the impact of gender on the development of ileal pouch disorders after restorative proctocolectomy were scant in the literature.15 In this large cohort of 1564 patients seen at our Pouch Center, our results revealed that although the pouch failure rate was comparable between male and female patients, male patients had an increased risk for the CARP as well as ileal pouch anastomotic sinus than their female counterparts.
Pouchitis is the most prevalent adverse event in UC patients after IPAA, with a reported cumulative prevalence of 5–59 %.16 – 19 Twenty to 38 % of the patients diagnosed with pouchitis have chronic phenotype which requires long-term courses of antibiotics and other medications.19 In this study, 13.9 % (n = 217) of our patients were diagnosed with CARP and an additional 16.2 % (n = 254) had acute pouchitis. Although IPAA has revolutionized the surgical management of UC patients, pouchitis, especially the chronic type, remains a morbid adverse event, which can significantly compromise patients’ QOL and satisfaction from the operation.20 Several risk factors associated with the development of chronic pouchitis were reported by previous studies. PSC and other EIMs have been repeatedly shown to be risk factors for chronic pouchitis,16 , 21 – 23 as confirmed by the findings in the current study. Other purported risk factors, despite conflicting results, included young age at diagnosis of UC,17 extensive colonic disease,19 , 21 , 22 smoking status,23 – 25 preoperative terminal ileal inflammation,26 and the presence of perinuclear antineutrophil cytoplasmic antibodies.22 , 27 , 28 Possible explanations for this discrepancy were the retrospective design of the studies, different criteria used to diagnose pouchitis, and duration of patient follow-up. In the multivariate analysis, J pouch patients were found to hold a greater risk for CARP than patients with other pouch configurations, which was in line with the results of a recent study from our group.29 Interestingly, a difference in the risk for the development of CARP was also identified between male and female patients, with a higher likelihood leaned to the males. The results from two other previous studies can support our findings. Carraro et al.30 evaluated the histopathology of the ileal pouch mucosa after IPAA (n = 60) and found a significant correlation between severe inflammation and male gender (P = 0.035). In another study of 327 ileal pouch patients, Joelsson and colleagues24 showed that 63/185 (34.1 %) males versus 33/142 (23.2 %) females had at least one episode of pouchitis (P = 0.04); the association between gender and the risk for pouchitis was significant in a multivariate analysis. However, previous studies were not able to divide the pouchitis into acute and chronic types. Our current study showed no difference in the frequency of acute pouchitis between the male and female patients. Male gender is not only a risk factor for CARP but also a risk factor for Clostridium difficile pouchitis31 and recurrent C. difficile pouchitis.32.
Ileal pouch anastomotic sinus featured by a blind-ended track is a less known disease entity. The frequency of ileal pouch sinus in this study was 6.1 % (n = 96), which is consistent with the reported range from 2.8 to 8 % in the literature.33 – 35 The clinical impact of an ileal pouch sinus is significant, as it is one of common causes for pouch failure.33 , 36 , 37 There were no published articles on the risk factors for pouch sinus. In the routine clinical practice at our Pouch Center, we found that the majority of patients with pouch sinus were male. In this study, both univariate and multivariate analyses showed that male gender was significantly associated with a higher risk for the occurrence of ileal pouch anastomotic sinus. One possible explanation for this difference is a narrower pelvis in the males, which makes the surgical procedure, particularly the creation of an anastomosis, technically more challenging than in females.38 The fact that male patients have a higher BMI and shorter mesentery than females may further contribute to the difference in the occurrence of ileal pouch sinus as well as chronic pouchitis. In a study by Akbari and colleagues,33 they demonstrated that 14 (63.6 %) of the 22 patients with ileal pouch sinus were men. A male predominance in ileal pouch sinus patients has also been reported in the previous two studies from our group.39 , 40 Another interesting finding of this study is that patients with a stapled anastomosis were less likely to have ileal pouch anastomotic sinus than those with a handsewn anastomosis. However, this is what we have expected, since our previous study showed that patients undergoing a stapled IPAA had better outcomes, including a lower risk for pouch procedure-related complications, than those undergoing a handsewn IPAA.41.
More importantly, for the first time, we reported that pouch sinus and CARP shared a common risk factor, i.e., the male gender. Therefore, the results may point the pathophysiology behind the two disease conditions, with a common denominator. In our clinical practice, we have increasingly seen male patients with one or both disease conditions. Surgical literatures and clinical operative practice have suggested that male patients typically have a narrower pelvis and/or shorter mesentery, which may increase the risk of anastomotic tension as well as compromise of blood perfusion to pouch tissue, resulting in anastomotic leak/sinus and/or chronic pouchitis, refractory to antibiotic therapy. We believe that tissue ischemia and tissue hypoxia may play an important role in CARP. In fact, hyperbaric oxygen therapy has been successfully used in patients with CARP.42.
Besides CARP and pouch sinus, a difference in the occurrence of pouch fistula between the two genders was also identified in this study, favoring females. This might resulted from the fact that a significant proportion of fistulas in women are PVF. Indeed, 17 (56.7 %) of the 30 female patients with pouch fistulas had PVF, including one that had a history of pouch cutaneous fistula before the diagnosis of PVF. There was no significant difference between the two genders in non-PVF (P = 0.21). In line with these findings, previous data from our group showed that pouch vaginal fistula comprised 46 % of all fistulas in females.15 The association between gender and the risk for pouch fistula was not further investigated in this study. There was no significant difference between male and female patients in other ileal pouch disorders. The reported long-term pouch failure rates from large series in the literature ranged from 3.5 to 15 %.2 , 36 , 43 In agreement with this, ileal pouch failed in a total of 126 patients (8.1 %) after a median follow-up of 9.0 (IQR 4.0–14.0) years in our study. No significant difference in pouch failure rate was identified between the two genders.
Consistent with a previous study of patients for whom the pouch was created at the Cleveland Clinic,15 male patients were shown to be older at the time of IBD diagnosis and pouch construction in this study, further validating the notion that gender has an impact on the disease course in IBD patients. More male patients had significant comorbidities and underwent colectomy due to neoplastic transformation, which might be at least partially explained by their older ages than the female patients. IBD-related EIMs have been reported to occur in 25–40 % of IBD patients,44 , 45 and the frequency in this study was 37.3 %. Interestingly, female patients were found more likely to have EIM than males; similar results were also obtained by previous studies.45 – 47 There might be a common link between IBD-related EIM and other autoimmune disorder. Indeed, a greater proportion of female patients were identified to have autoimmune disorders.48 More than 85 % of patients included in this study had various IPAA-related adverse sequalae, a rate which seemed to be higher than that reported in the literature,2 , 6 but reflected the nature of our Pouch Center as a tertiary referral center mainly looking after patients with complex ileal pouch disorders.
The findings of the current study have several clinical implications. Although the predictors for the chronic pouchitis have been previously evaluated by our group,22 , 25 this study expanded the list and identified male gender as a new risk factor associated with CARP due to the availability of a growing number of patients enrolled in our Pouch Center. This information is valuable to patients as well as practicing colorectal surgeons and gastroenterologists, as it may help to refine the risk calculation and stratification for the development of ileal pouch disorders. However, our result that male and female patients have a comparable long-term pouch survival rate indicates that these ileal pouch disorders can be treated and controlled in most instances. It may also reassure male patients to undergo the IPAA surgery when they are suitable, despite the potential need to be monitored more closely than their female counterparts following the procedure.
There are limitations to our study, particularly relating to the study design. However, the fact that the information employed in the study was from a registry in which data were prospectively accrued strengthened the accuracy of our results. There might have been a referral bias, as all the patients in the current study were seen in the setting of a subspecialty Pouch Center. A careful interpretation of our data was required. We tried to minimize the limitation of referral bias by including all eligible patients (n = 1564), which virtually covered a broad range of disease categories for pouches as well as normal healthy pouches.
In conclusion, among the ileal pouch patients seen at our subspecialty Pouch Center, although the pouch failure rate was comparable between the two genders, male patients were found to have an increased risk for the CARP and ileal pouch sinus than their female counterparts. A more closely follow-up plan might be required for the males following the IPAA procedure.
Abbreviations
- ATZ:
-
Anal transitional zone
- CARP:
-
Chronic antibiotic-refractory pouchitis
- CD:
-
Crohn’s disease
- CI:
-
Confidence interval
- EIMs:
-
Extra-intestinal manifestations
- FAP:
-
Familial adenomatous polyposis
- OR:
-
Odds ratio
- IBD:
-
Inflammatory bowel disease
- IC:
-
Indeterminate colitis
- IPAA:
-
Ileal pouch-anal anastomosis
- IPS:
-
Irritable pouch syndrome
- IQR:
-
Interquartile range
- IRB:
-
The Institutional Review Board
- NSAID:
-
Non-steroidal anti-inflammatory drug
- PSC:
-
Primary sclerosing cholangitis
- PVF:
-
Pouch vaginal fistula
- QOL:
-
Quality of life
- SDs:
-
Standard deviations
- TNF:
-
Tumor necrosis factor
- UC:
-
Ulcerative colitis
References
Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. Br Med J 1978;2:85–8.
Fazio VW, Kiran RP, Remzi FH, et al. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg 2013;257:679–85.
Hahnloser D, Pemberton JH, Wolff BG, et al. The effect of ageing on function and quality of life in ileal pouch patients: a single cohort experience of 409 patients with chronic ulcerative colitis. Ann Surg 2004;240:615–21; discussion 621–3.
Chapman JR, Larson DW, Wolff BG, et al. Ileal pouch-anal anastomosis: does age at the time of surgery affect outcome? Arch Surg 2005;140:534–9; discussion 539–40.
Hahnloser D, Pemberton JH, Wolff BG, et al. Results at up to 20 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Br J Surg 2007;94:333–40.
Fazio VW, Ziv Y, Church JM, et al. Ileal pouch-anal anastomoses complications and function in 1005 patients. Ann Surg 1995;222:120–7.
Shen B, Remzi FH, Lavery IC, et al. A proposed classification of ileal pouch disorders and associated complications after restorative proctocolectomy. Clin Gastroenterol Hepatol 2008;6:145–58; quiz 124.
Shen B, Achkar JP, Connor JT, et al. Modified pouchitis disease activity index: a simplified approach to the diagnosis of pouchitis. Dis Colon Rectum 2003;46:748–53.
Shen B, Fazio VW, Remzi FH, et al. Risk factors for clinical phenotypes of Crohn’s disease of the ileal pouch. Am J Gastroenterol 2006;101:2760–8.
Bouman A, Schipper M, Heineman MJ, et al. Gender difference in the non-specific and specific immune response in humans. Am J Reprod Immunol 2004;52:19–26.
Ortona E, Margutti P, Matarrese P, et al. Redox state, cell death and autoimmune diseases: a gender perspective. Autoimmun Rev 2008;7:579–84.
Gupta N, Bostrom AG, Kirschner BS, et al. Gender differences in presentation and course of disease in pediatric patients with Crohn disease. Pediatrics 2007;120:e1418-25.
Wagtmans MJ, Verspaget HW, Lamers CB, et al. Gender-related differences in the clinical course of Crohn’s disease. Am J Gastroenterol 2001;96:1541–6.
Betteridge JD, Armbruster SP, Maydonovitch C, et al. Inflammatory bowel disease prevalence by age, gender, race, and geographic location in the U.S. military health care population. Inflamm Bowel Dis 2013;19:1421–7.
Rottoli M, Remzi FH, Shen B, et al. Gender of the patient may influence perioperative and long-term complications after restorative proctocolectomy. Colorectal Dis 2012;14:336–41.
Penna C, Dozois R, Tremaine W, et al. Pouchitis after ileal pouch-anal anastomosis for ulcerative colitis occurs with increased frequency in patients with associated primary sclerosing cholangitis. Gut 1996;38:234–9.
Stahlberg D, Gullberg K, Liljeqvist L, et al. Pouchitis following pelvic pouch operation for ulcerative colitis. Incidence, cumulative risk, and risk factors. Dis Colon Rectum 1996;39:1012–8.
Stocchi L, Pemberton JH. Pouch and pouchitis. Gastroenterol Clin North Am 2001;30:223–41.
Hashavia E, Dotan I, Rabau M, et al. Risk factors for chronic pouchitis after ileal pouch-anal anastomosis: a prospective cohort study. Colorectal Dis 2012;14:1365–71.
Turina M, Pennington CJ, Kimberling J, et al. Chronic pouchitis after ileal pouch-anal anastomosis for ulcerative colitis: effect on quality of life. J Gastrointest Surg 2006;10:600–6.
Lipman JM, Kiran RP, Shen B, et al. Perioperative factors during ileal pouch-anal anastomosis predict pouchitis. Dis Colon Rectum 2011;54:311–7.
Achkar JP, Al-Haddad M, Lashner B, et al. Differentiating risk factors for acute and chronic pouchitis. Clin Gastroenterol Hepatol 2005;3:60–6.
Fleshner P, Ippoliti A, Dubinsky M, et al. A prospective multivariate analysis of clinical factors associated with pouchitis after ileal pouch-anal anastomosis. Clin Gastroenterol Hepatol 2007;5:952–8; quiz 887.
Joelsson M, Benoni C, Oresland T. Does smoking influence the risk of pouchitis following ileal pouch anal anastomosis for ulcerative colitis? Scand J Gastroenterol 2006;41:929–33.
Shen B, Fazio VW, Remzi FH, et al. Risk factors for diseases of ileal pouch-anal anastomosis after restorative proctocolectomy for ulcerative colitis. Clin Gastroenterol Hepatol 2006;4:81–9; quiz 2–3.
Schmidt CM, Lazenby AJ, Hendrickson RJ, et al. Preoperative terminal ileal and colonic resection histopathology predicts risk of pouchitis in patients after ileoanal pull-through procedure. Ann Surg 1998;227:654–62; discussion 663–5.
Sandborn WJ, Landers CJ, Tremaine WJ, et al. Antineutrophil cytoplasmic antibody correlates with chronic pouchitis after ileal pouch-anal anastomosis. Am J Gastroenterol 1995;90:740–7.
Fleshner PR, Vasiliauskas EA, Kam LY, et al. High level perinuclear antineutrophil cytoplasmic antibody (pANCA) in ulcerative colitis patients before colectomy predicts the development of chronic pouchitis after ileal pouch-anal anastomosis. Gut 2001;49:671–7.
Mukewar S, Wu X, Lopez R, et al. Comparison of long-term outcomes of S and J pouches and continent ileostomies in ulcerative colitis patients with restorative proctocolectomy-experience in subspecialty pouch center. J Crohns Colitis 2014.
Setti Carraro P, Talbot IC, Nicholls RJ. Long term appraisal of the histological appearances of the ileal reservoir mucosa after restorative proctocolectomy for ulcerative colitis. Gut 1994;35:1721–7.
Shen BO, Jiang ZD, Fazio VW, et al. Clostridium difficile infection in patients with ileal pouch-anal anastomosis. Clin Gastroenterol Hepatol 2008;6:782–8.
Seril DN, Ashburn JH, Lian L, et al. Risk factors and management of refractory or recurrent clostridium difficile infection in ileal pouch patients. Inflamm Bowel Dis 2014;20:2226–33.
Akbari RP, Madoff RD, Parker SC, et al. Anastomotic sinuses after ileoanal pouch construction: incidence, management, and outcome. Dis Colon Rectum 2009;52:452–5.
Nyam DC, Wolff BG, Dozois RR, et al. Does the presence of a pre-ileostomy closure asymptomatic pouch-anastomotic sinus tract affect the success of ileal pouch-anal anastomosis? J Gastrointest Surg 1997;1:274–7.
Whitlow CB, Opelka FG, Gathright JB, et al. Treatment of colorectal and ileoanal anastomotic sinuses. Dis Colon Rectum 1997;40:760–3.
Prudhomme M, Dehni N, Dozois RR, et al. Causes and outcomes of pouch excision after restorative proctocolectomy. Br J Surg 2006;93:82–6.
Fong SS, Chen K, Sim R. Chronic anastomotic sinus after low anterior resection: when can the defunctioning stoma be reversed? Colorectal Dis 2011;13:644–9.
Trencheva K, Morrissey KP, Wells M, et al. Identifying important predictors for anastomotic leak after colon and rectal resection: prospective study on 616 patients. Ann Surg 2013;257:108–13.
Wu XR, Wong RC, Shen B. Endoscopic needle-knife therapy for ileal pouch sinus: a novel approach for the surgical adverse event (with video). Gastrointest Endosc 2013;78:875–85.
Ahmed Ali U, Shen B, Remzi FH, et al. The management of anastomotic pouch sinus after IPAA. Dis Colon Rectum 2012;55:541–8.
Kirat HT, Remzi FH, Kiran RP, et al. Comparison of outcomes after hand-sewn versus stapled ileal pouch-anal anastomosis in 3,109 patients. Surgery 2009;146:723–9; discussion 729–30.
Nyabanga CT, Kulkarni G, Shen B. Hyperbaric oxygen therapy for chronic antibiotic-refractory ischemic pouchitis. Gastroenterol Rep (Oxf) 2015. doi:10.1093/gastro/gov038.
Lepisto A, Luukkonen P, Jarvinen HJ. Cumulative failure rate of ileal pouch-anal anastomosis and quality of life after failure. Dis Colon Rectum 2002;45:1289–94.
Levine JS, Burakoff R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Hepatol (N Y) 2011;7:235–41.
Bernstein CN, Blanchard JF, Rawsthorne P, et al. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol 2001;96:1116–22.
Lakatos L, Pandur T, David G, et al. Association of extraintestinal manifestations of inflammatory bowel disease in a province of western Hungary with disease phenotype: results of a 25-year follow-up study. World J Gastroenterol 2003;9:2300–7.
Jose FA, Garnett EA, Vittinghoff E, et al. Development of extraintestinal manifestations in pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis 2009;15:63–8.
Fairweather D, Frisancho-Kiss S, Rose NR. Sex differences in autoimmune disease from a pathological perspective. Am J Pathol 2008;173:600–9.
Acknowledgments
Author Contributions
XRW and YL contributed to study concept and design, acquisition, analysis and interpretation of data, and drafting of the manuscript. HF contributed data collections and manuscript review. JA, FHR, and BS contributed to study concept and design, analysis and interpretation of data, and critical revision of the manuscript for important intellectual content. BS supervised the study. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Grant Support
This project was partially supported by the Ed and Joey Story Chair (to B.S.).
Conflict of Interest
The authors declared no financial conflict of interest.
Rights and permissions
About this article
Cite this article
Wu, Xr., Ashburn, J., Remzi, F.H. et al. Male Gender Is Associated with a High Risk for Chronic Antibiotic-Refractory Pouchitis and Ileal Pouch Anastomotic Sinus. J Gastrointest Surg 20, 631–639 (2016). https://doi.org/10.1007/s11605-015-2976-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2976-z