Abstract
Background
Elderly patients who undergo major abdominal surgery are potentially at a higher risk of perioperative mortality and postoperative complications. Although laparoscopic surgery has been widely accepted as a less invasive surgical procedure for colorectal diseases, the benefits for elderly patients have not been validated.
Aim
To compare postoperative outcomes and long-term survival between laparoscopic and open colorectal surgery in the elderly population.
Methods
A literature search was electronically performed to identify all studies comparing postoperative outcomes between laparoscopic and open colorectal resections in the elderly population. Primary outcomes were postoperative mortality and complications, and the secondary outcome was long-term survival.
Results
Overall, 30 studies (70,946 patients) met our inclusion criteria. Laparoscopic surgery was significantly associated with a decreased risk of perioperative mortality [odds ratio (OR), 0.55; 95 % confidence interval (CI), 0.45–0.68; P < 0.01] and postoperative complications (OR, 0.55; 95 % CI, 0.48–0.63; P < 0.01) compared with open surgery. There was no significant difference in long-term survival between the two procedures (OR, 0.89; 95 % CI, 0.72–1.07; P = 0.31).
Conclusions
Laparoscopic colorectal surgery in the elderly population has significant advantages in terms of short-term outcomes. Aggressive application of laparoscopic colorectal surgery should be considered for the elderly population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aging has become an important issue worldwide and is expected to rapidly progress within the next 50 years. The proportion of individuals aged >65 years in the total world population has increased to 7.6 % in 2010 from 5.2 % in 1950, and it is expected to increase to 17.6 % in 2060.1 With an increase in life expectancy, the number of elderly patients requiring surgery will also increase. Considering the increasing incidence of colorectal diseases, the frequency of colorectal surgery for elderly patients will increase compared with the previous frequency. Nevertheless, elderly patients are often regarded as high-risk patients because they are more likely to have significant comorbid conditions compared with younger patients.2 Consequently, increasing age itself is also an important risk factor for postoperative morbidity and mortality. Physiologically, aging is associated with a gradual loss of functional reserve capacity, and its effects become most apparent during surgery because it decreases the tolerability for surgical stress in elderly patients.3 It is reported that the 30-day mortality is approximately 6 % for patients aged ≥70 years and that at least 20 % of these patients develop one complication during hospitalization.4 Mortality risk increases by 10 % every year after the age of 70.4 Therefore, there are increasing demands for optimized surgical treatments for elderly patients.
Despite laparoscopic surgery (LPS) being a less invasive procedure and widely accepted surgical method worldwide, there is conflicting evidence regarding the safety and benefits of laparoscopic colorectal surgery in elderly patients. Several previous studies demonstrated that laparoscopic colon resection resulted in decreased postoperative pain, quicker return of bowel function, shorter hospital stay, better cosmesis, and a more rapid return to routine activities.5 – 11 Furthermore, the benefits of LPS are more marked in elderly patients than in younger patients.12 , 13 On the other hand, there are some concerns regarding its application in elderly patients because of physiological concerns such as specialized surgical positions (e.g., the Trendelenburg position) or pneumoperitoneum, which may result in a significant decrease in stroke volume and cardiac output and an increase in cardiac strain.14 In several studies, the risk of cardiorespiratory complications was significantly higher in elderly patients, probably because of an extended surgical duration under prolonged general anesthesia and resultant postoperative atelectasis.4 , 15 , 16
In order to fully consider the application of LPS for elderly patients, the benefits of its decreased invasiveness need to be verified in this age group. The objective of this meta-analysis was to compare postoperative outcomes between LPS and open surgery (OS) in the elderly population. The findings of this study will help the further understanding of various postoperative outcomes from both surgical procedures and facilitate appropriate treatment selection strategies for elderly patients.
Methods
This review was written on the basis of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) statement.17
Literature Search Strategy
PubMed and Cochrane library databases were systematically searched, without language restriction, in October 2014 for manuscripts that compared LPS and OS in the elderly. Our search terms included three main components, colorectal (colorectal OR colon OR colonic OR rectum OR rectal) AND laparoscopy (laparoscopy OR laparoscopic surgery) AND open surgery AND elderly (elderly OR older OR octogenarian).
Inclusion and Exclusion Criteria
Postoperative complications and mortality were defined as primary outcomes in this study, while long-term survival was the secondary outcome. All studies that compared LPS and OS in elderly patients were included. Hand-assisted laparotomy was determined as LPS. Because most of the studies included conversion cases in the LPS group, we determined such cases as LPS cases in accordance with the concept of intention-to-treat. In addition to cohort studies comparing postoperative outcomes, case–control studies in which definitive inclusion and/or exclusion criteria that were presented were also included. The prevalence of postoperative complications (overall, wound infection, anastomotic leakage, pulmonary disease, cardiovascular disease, and mortality) within 30 days after surgery or during hospitalization and reported risk estimates [relative risks, odds ratios (ORs), or hazard ratios (HRs)] and 95 % confidence intervals (CIs) or sufficient data to estimate these were recorded. The length of hospital stay (LOS) after surgery was also recorded. As a secondary outcome, long-term survival data during follow-up were recorded. Studies that only compared young and elderly individuals or those that did not have data for both the LPS and OS groups were excluded. Reviews or meta-analyses were also excluded. All available studies were independently reviewed by two investigators (R.S. and K.O.), and discrepancies were discussed among the authors to achieve an agreement.
Assessment of Methodological Quality and Data Extraction
Data based on the characteristics of the study design, participants, and covariates were extracted together with the postoperative outcomes for the LPS and OS groups. The quality of included studies was independently reviewed by two assessors (R.S. and K.O.) according to the Newcastle–Ottawa Scale (NOS).18 , 19 Scores ranged from 0 (lowest) to 9 (highest). Studies with scores of ≥7 were classified as higher quality studies, while those with scores of <7 were classified as lower quality studies.
Statistical Methods
The pooled ORs and 95 % CIs were calculated, and the outcomes of individual studies were compared using the DerSimonian and Laird random-effects model.20 When one arm of a study contained no events, 0.5 was added to each cell of the 2 × 2 trial table to avoid reducing statistical power. If there was no event in either the LPS or OS groups, the study was discarded from the calculation. Forest plots were constructed for visual display of individual study ORs. Heterogeneity between studies was assessed with the I 2 statistic as a measure of the proportion of total variations in estimates due to heterogeneity, where I 2 values of 25, 50, and 75 % corresponded to cutoff points for low, moderate, and high degrees of heterogeneity, respectively. To assess for publication bias, we tested for funnel plot asymmetry using the regression test by Egger. Subgroup analysis for study characteristics and complication types was performed.
For long-term survival analysis, HR was extracted or computed from each study as an effect size, applying the statistical model described by Tierney et al.21 Meta-regression was employed to assess the influence of key covariates, including year of publication, prospective study, Asian region, sample size, NOS type, definition of elderly age, conversion rate in the LPS group, percentage of females, an American Society of Anesthesiologists score of ≥3, and cancer type, on the generated heterogeneity.
All statistical analyses were performed using Stata version 12 (Stata Corp, College Station, TX, USA). For all comparisons, except those for heterogeneity, statistical significance was defined as P < 0.05, and all tests were two-sided.
Results
Search Process
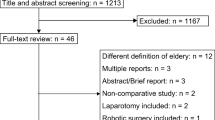
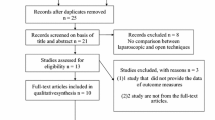
The outline of our search process is shown in Fig. 1; 1138 articles were found through electronic searches and 17 through manual searches. After removing duplicates from the title and abstract search, 1103 studies were excluded. Finally, 52 manuscripts were reviewed in full text, of which 30 met our search criteria. A total of 70,946 patients were included in our study. Details of included studies are listed in Table 1. There were 3 randomized control studies,12 , 13 , 22 3 prospective cohort studies,16 , 23 , 24 20 retrospective studies,7 , 11 , 25 – 42 and 4 case-match control studies.6 , 8 – 10 From the 30 included studies, 13 were classified as higher quality and 17 as lower quality according to the NOS (Table 2).
Short-Term Complications and Mortality
Overall Complications
Of all, 29 studies reported on the short-term complications after surgery and included a total of 42,200 participants, 5,641 of whom underwent LPS and 36,559 of whom underwent OS. The comparison between LPS and OS demonstrated that subjects with LPS had a significantly lower OR of short-term complications (OR, 0.55; 95 % CI, 0.48–0.63; P < 0.01; Fig. 2). Although there was moderate heterogeneity among studies (I 2 = 45.6 %), Egger’s test for funnel plot asymmetry identified no significant publication bias (bias = −0.59, P = 0.10; Supplement 1).
Mortality
To assess the impact of LPS on mortality, 21 studies reporting mortality were identified; The OR was 0.55 (95 % CI, 0.45–0.68; P < 0.01), demonstrating a significant association between LPS and decreased mortality (Fig. 3). Heterogeneity between the included studies was low (I 2 = 11.4 %).
Detailed Complications
The impact of LPS on the incidence of each type of complication is shown in Fig. 4.
Twenty-four studies reported the incidence of wound infection; the OR was 0.51 (95 % CI, 0.39–0.66; P < 0.01), and the heterogeneity between included studies was low (I 2 = 25.0 %). Twenty-two studies reported the incidence of anastomotic leakage; the OR was 0.77 (95 % CI, 0.51–1.16; P = 0.21), and the heterogeneity between included studies was low (I 2 = 9.5 %). Eighteen studies reported the incidence of cardiovascular diseases; the OR was 0.66 (95 % CI, 0.49–0.89; P < 0.01), and the heterogeneity between included studies was low (I 2 = 20.7 %). Twenty-one studies reported the incidence of pneumonia; the OR was 0.63 (95 % CI, 0.46–0.86; P < 0.01), and the heterogeneity between included studies was low (I 2 = 11.7 %). Fourteen studies reported LOS; the standardized mean difference was −0.34 (95 % CI, –0.39 – − 0.30, P < 0.01), and the heterogeneity between included studies was high (I 2 = 86.3 %) (Fig. 5). Therefore, significant associations were found between LPS and a decreased incidence of postoperative wound infection, cardiovascular diseases, pneumonia, and decreased LOS, while associations were not significant for anastomotic leakage. In addition, an association was also found between LPS and decreased LOS.
Subgroup Analysis for Short-Term Complications
Study Design
The impact of study design on OR was assessed; the OR was 0.51 (95 % CI, 0.37–0.70; P < 0.01) for RCTs and 0.55 (95 % CI, 0.47–0.64; P < 0.01) for non-RCTs. The impact of LPS on a decreased incidence of postoperative short-term complications was consistent, regardless of study design (Fig. 6).
Study Quality
The impact of study quality on OR was assessed; the OR was 0.58 (95 % CI, 0.53–0.64; P < 0.01) for higher quality studies and 0.62 (95 % CI, 0.52–0.73; P < 0.01) for lower quality studies. The association of LPS with a decreased incidence of postoperative short-term complications was consistent, regardless of study quality (Fig. 6).
Region
To explore differences in ORs for short-term complications between Western and Asian regions, we categorized all studies into two groups, those published in Western countries and those published in Asian countries. The OR was 0.59 (95 % CI, 0.54–0.64; P < 0.01) for Western countries and 0.60 (95 % CI, 0.48–0.74; P < 0.01) for Asian countries. The association of LPS with a decreased incidence of postoperative short-term complications was consistent, regardless of region (Fig. 6).
Age Definition
The definition of elderly age differed among studies; however, in the present study, the definition of age had no influence on short-term complications. Four studies defined elderly patients as those aged over 65 years; the OR of these studies was 0.60 (95 % CI, 0.53–0.67; P < 0.01). The OR for 17 studies that defined elderly patients as those aged over 70, 71, or 75 years was 0.66 (95 % CI, 0.60–0.78; P < 0.01). The OR of 8 studies that defined elderly patients as those aged over 79 or 80 years was 0.54 (95 % CI, 0.47–0.62; P < 0.01; Fig. 6). These results suggest that OS was a significant risk factor for short-term complications, regardless of age, and was of most relevance for the oldest patients.
Meta-regression Analysis
We explored covariates affecting the heterogeneity of ORs among the included studies. The meta-regression analysis identified year of publication (coefficient, 0.04; 95 % CI, 0.01–0.07; P = 0.02) as a significant source of heterogeneity (Supplement 2). Furthermore, the inclusion of rectal lesions was also shown to have a marginally significant effect as a source of heterogeneity (coefficient, –0.23; 95 % CI, −0.49–0.04; P = 0.09).
Long-Term Survival
To assess the impact of LPS on long-term survival, 3 studies reporting long-term survival were identified. All studies included only patients with colorectal cancer. The HR was 0.89 (95 % CI, 0.72–1.07; P = 0.31), demonstrating no significant association between LPS and long-term survival (Fig. 7). Heterogeneity between the included studies was low (I 2 = 0.0 %).
Discussion
This meta-analysis demonstrated that laparoscopic colorectal surgery for elderly patients has had a clear and positive impact in terms of a significant decrease in postoperative morbidity and mortality compared with conventional open colorectal surgery. Furthermore, this procedure was associated with faster postoperative recovery and the protection of postoperative complications, regardless of the type of postoperative complication. With regard to long-term survival outcomes, there was no significant difference between LPS and OS. Considering the rapidly aging population, an overview of surgical outcomes for elderly patients is useful to understand the intraoperative physiology of elderly patients better and design an age-appropriate treatment plan. Consequently, these findings favor the use of laparoscopic colorectal surgery, even for elderly patients.
One of the difficulties in assessing the outcomes of colorectal surgery in elderly patients is that there is no consistent definition of the elderly patient population in the published series.15 In fact, the definitions of elderly age in included studies varied from 65 to 80 years. In this meta-analysis, subgroup and meta-regression analyses were conducted to evaluate the influence of a variety of definitions of age on postoperative morbidity, showing that it had no significant influence on postoperative morbidity. This finding suggests that the decreased invasiveness of LPS remains an advantage regardless of patient age. In a study including 535 patients, Frasson et al.12 reported that LPS improved the short-term postoperative outcome in patients aged ≥70 years compared with that in patients aged <70 years and concluded that the benefits of LPS are more pronounced in the elderly. These findings therefore favor the aggressive application of laparoscopic surgery in elderly patients.
Although several large randomized control studies have shown the non-inferiority of LPS over OS in terms of long-term survival, this topic remains controversial in elderly patients.43 – 45 This is the first meta-analysis comparing long-term survival between LPS and OS in elderly patients, showing no statistically significant difference between the two procedures. However, this result should be cautiously interpreted because there was a potential imbalance in patient characteristics between LPS and OS; furthermore, no well-designed study has been conducted till date. In elderly patients, surgeons hesitate to perform extended lymphadenectomy, considering the limitations in physical function. Occasionally, elderly patients have greater expectations for a good quality of life than for long-term survival. Investigations assessing the outcomes of better function and improved quality of life will attribute these to appropriate treatment strategies for elderly patients with colorectal cancer.
Recently, Antoniou et al.46 have reported a meta-analysis concluding that LPS has a significant advantage in postoperative morbidity and mortality, consistent with our result. Although they performed sensitivity analysis, the definition of elderly patients, which is considered as one of the critical factors, was not mentioned. Given the appropriate application of LPS, our finding that there is no significant difference among age definitions is useful. In addition, the impact on long-term survival was not discussed. Therefore, our analysis is considered to include more comprehensive and significant result about the benefits of LPS in the elderly.
There are a number of recognized risks of LPS in terms of physiological concerns adherent to postoperative morbidity; increased intraperitoneal pressure caused by pneumoperitoneum, adverse effects of high carbon dioxide levels, and patient positions are all well-known disadvantages of LPS.47 – 49 Although elderly patients are less likely to tolerate these risks because of their limited cardiopulmonary capacity, this meta-analysis demonstrated that these risks are clearly decreased by LPS, probably because of advanced anesthetic improvements and perioperative care.50 Furthermore, serum inflammatory cytokines were reported to be significantly low with LPS, suggesting that LPS can better preserve immune function compared with OS.51 – 53
In a systematic review, the incidence of morbidity and mortality after colorectal cancer surgery was reported to increase with advancing age.54 This finding is considered to be associated with higher comorbidities adherent to surgical risk in elderly patients and indicates the need for optimized perioperative management for elderly patients. A shorter LOS and the lower morbidity rate are important for elderly patients in terms of rapid postoperative recovery of bowel function, oral food intake, and physical activity.7 – 9 , 55 Given that elderly patients are at a high risk of decreased postoperative activities of daily living (ADL), a shorter LOS greatly favors faster ADL recovery by supporting the postoperative rehabilitation of elderly patients and avoiding the risk of postoperative delirium.56
Although significant benefits were shown in this meta-analysis, whether or not LPS is recommended regardless of patient comorbidities remains controversial. There have been recent attempts to determine the surgical indications for elderly patients according to preoperative conditions. Actually, the issue of selection bias is critical and needs more than a passing remark. Only three of the studies included in this analysis were randomized (the numbers of patients enrolled were 727 in RCT and 70,219 in non-RCT). However, even RCT is necessarily not the best way to eliminate selection bias in study of elderly patients, because patients with severe comorbidities are actually excluded. Therefore, a case series study describing these exclusion criteria would be helpful to generalize the conclusions. The Portsmouth Physiologic and Operative Severity Score for the enumeration of Mortality and Morbidity (P-POSSUM) is one of the scoring systems that potentially reflects patient conditions and predicts the risk of postoperative complications.36 Hereafter, a novel guideline not only for surgical indications but also for surgical procedure (i.e., LPS or OS) selection according to the postoperative complication risk is required to achieve the standardization of treatment for elderly patients. Furthermore, because we focused on the benefits of LPS itself, oncological factors such as surgical curability, length of the resected specimen, and number of dissected lymph nodes in cancer patients were not analyzed. The Colorectal Cancer Collaborative Group has reported that older patients with colorectal cancer are more likely to present with later-stage disease compared with their younger counterparts.54 To clarify the oncological accuracy of LPS in elderly patients with colorectal cancer, further studies are required that consider these influencing factors.
In conclusion, this meta-analysis showed significant short-term advantages of LPS in the elderly population. LPS should be aggressively applied for elderly patients. Further studies are required to examine long-term survival compared between LPS and OS in the elderly population.
References
World Population Prospects: the 2012 revision [database online]. United Nations; 2014.
Grailey K, Markar SR, Karthikesalingam A, Aboud R, Ziprin P, Faiz O. Laparoscopic versus open colorectal resection in the elderly population. Surg Endosc. 2013;27:19-30.
Evers BM, Townsend CM, Jr., Thompson JC. Organ physiology of aging. Surg Clin North Am. 1994;74:23-39.
Story DA. Postoperative complications in elderly patients and their significance for long-term prognosis. Curr Opin Anaesthesiol. 2008;21:375-379.
Zucker KA, Pitcher DE, Martin DT, Ford RS. Laparoscopic-assisted colon resection. Surg Endosc. 1994;8:12-17; discussion 18.
Stocchi L, Nelson H, Young-Fadok TM, Larson DR, Ilstrup DM. Safety and advantages of laparoscopic vs. open colectomy in the elderly: matched-control study. Dis Colon Rectum. 2000;43:326-332.
Law WL, Chu KW, Tung PH. Laparoscopic colorectal resection: a safe option for elderly patients. J Am Coll Surg. 2002;195:768-773.
Sklow B, Read T, Birnbaum E, Fry R, Fleshman J. Age and type of procedure influence the choice of patients for laparoscopic colectomy. Surg Endosc. 2003;17:923-929.
Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C. Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum. 2005;48:2070-2075.
Lian L, Kalady M, Geisler D, Kiran RP. Laparoscopic colectomy is safe and leads to a significantly shorter hospital stay for octogenarians. Surg Endosc. 2010;24:2039-2043.
Tan WS, Chew MH, Lim IA, Ng KH, Tang CL, Eu KW. Evaluation of laparoscopic versus open colorectal surgery in elderly patients more than 70 years old: an evaluation of 727 patients. Int J Colorectal Dis. 2012;27:773-780.
Frasson M, Braga M, Vignali A, Zuliani W, Di Carlo V. Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum. 2008;51:296-300.
Allardyce RA, Bagshaw PF, Frampton CM, et al. Australasian Laparoscopic Colon Cancer Study shows that elderly patients may benefit from lower postoperative complication rates following laparoscopic versus open resection. Br J Surg. 2010;97:86-91.
Russo A, Marana E, Viviani D, et al. Diastolic function: the influence of pneumoperitoneum and Trendelenburg positioning during laparoscopic hysterectomy. Eur J Anaesthesiol. 2009;26:923-927.
Chautard J, Alves A, Zalinski S, Bretagnol F, Valleur P, Panis Y. Laparoscopic colorectal surgery in elderly patients: a matched case-control study in 178 patients. J Am Coll Surg. 2008;206:255-260.
Delgado S, Lacy AM, Garcia Valdecasas JC, et al. Could age be an indication for laparoscopic colectomy in colorectal cancer? Surg Endosc. 2000;14:22-26.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605.
Castillo JJ, Dalia S, Pascual SK. Association between red blood cell transfusions and development of non-Hodgkin lymphoma: a meta-analysis of observational studies. Blood. 2010;116:2897-2907.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Fujii S, ishibe A, Ota M, et al. Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients. Surg Endosc. 2013; [Epub ahead of print].
Stewart BT, Stitz RW, Lumley JW. Laparoscopically assisted colorectal surgery in the elderly. Br J Surg. 1999;86:938-941.
Tuech JJ, Pessaux P, Rouge C, Regenet N, Bergamaschi R, Arnaud JP. Laparoscopic vs open colectomy for sigmoid diverticulitis: a prospective comparative study in the elderly. Surg Endosc. 2000;14:1031-1033.
She WH, Poon JTC, Fan JKM, Lo OSH, Law WL. Outcome of laparoscopic colectomy for cancer in elderly patients. Surgical Endoscopy and Other Interventional Techniques. 2013;27:308-312.
Cummings LC, Delaney CP, Cooper GS. Laparoscopic versus open colectomy for colon cancer in an older population: a cohort study. World Journal of Surgical Oncology. 2012;10.
White SI, Wright D, Taylor CJ. A comparison of laparoscopic versus open rectal surgery in 114 consecutive octogenarians. Colorectal Disease. 2012;14:E395-E399.
Altuntas YE, Gezen C, Vural S, Okkabaz N, Kement M, Oncel M. Laparoscopy for sigmoid colon and rectal cancers in septuagenarians: a retrospective, comparative study. Techniques in Coloproctology. 2012;16:213-219.
Issa N, Grassi C, Melki Y, Powsner E, Dreznik Z. Laparoscopic colectomy for carcinoma of the colon in octogenarians. Journal of Gastrointestinal Surgery. 2011;15:2011-2015.
Al-Refaie WB, Parsons HM, Habermann EB, et al. Operative outcomes beyond 30-day mortality: colorectal cancer surgery in oldest old. Ann Surg. 2011;253:947-952.
Pinto RA, Ruiz D, Edden Y, Weiss EG, Nogueras JJ, Wexner SD. How reliable is laparoscopic colorectal surgery compared with laparotomy for octogenarians? Surg Endosc. 2011;25:2692-2698.
Robinson CN, Balentine CJ, Marshall CL, et al. Minimally invasive surgery improves short-term outcomes in elderly colorectal cancer patients. Journal of Surgical Research. 2011;166:182-188.
Tomimaru Y, Ide Y, Murata K. Outcome of laparoscopic surgery for colon cancer in elderly patients. Asian J Endosc Surg. 2011;4:1-6.
Kennedy GD, Rajamanickam V, O'Connor ES, et al. Optimizing surgical care of colon cancer in the older adult population. Annals of Surgery. 2011;253:508-514.
Faiz O, Haji A, Botte A, Clark SK, Darzi AW, Aylin P. Elective colonic surgery for cancer in the elderly: an investigation into postoperative mortality in English NHS hospitals between 1996 and 2007. Colorectal Disease. 2011;13:779-789.
Tei M, Ikeda M, Haraguchi N, et al. Postoperative complications in elderly patients with colorectal cancer comparison of open and laparoscopic surgical procedures. Surgical Laparoscopy Endoscopy & Percutaneous Techniques. 2009;19:488-492.
Akiyoshi T, Kuroyanagi H, Oya M, et al. Short-term outcomes of laparoscopic rectal surgery for primary rectal cancer in elderly patients: is it safe and beneficial? Journal of Gastrointestinal Surgery. 2009;13:1614-1618.
Person B, Cera SM, Sands DR, et al. Do elderly patients benefit from laparoscopic colorectal surgery? Surg Endosc. 2008;22:401-405.
Feng B, Zheng MH, Mao ZH, et al. Clinical advantages of laparoscopic colorectal cancer surgery in the elderly. Aging Clin Exp Res. 2006;18:191-195.
Senagore AJ, Madbouly KM, Fazio VW, Duepree HJ, Brady KM, Delaney CP. Advantages of laparoscopic colectomy in older patients. Arch Surg. 2003;138:252-256.
Miyasaka Y, Mochidome N, Kobayashi K, Ryu S, Akashi Y, Miyoshi A. Efficacy of laparoscopic resection in elderly patients with colorectal cancer. Surg Today. 2013;[Epub ahead of print].
Suto T, Sato T. Evaluation of laparoscopy-assisted surgery in elderly colorectal cancer patients. Nippon Ronen Igakkai Zasshi. 2011;48:655-671.
Green BL, Marshall HC, Collinson F, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100:75-82.
Colon Cancer Laparoscopic or Open Resection Study G, Buunen M, Veldkamp R, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10:44-52.
Fleshman J, Sargent DJ, Green E, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655-662; discussion 662-654.
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Laparoscopic colorectal surgery confers lower mortality in the elderly: a systematic review and meta-analysis of 66,483 patients. Surg Endosc. 2014.
Dhoste K, Lacoste L, Karayan J, Lehuede MS, Thomas D, Fusciardi J. Haemodynamic and ventilatory changes during laparoscopic cholecystectomy in elderly ASA III patients. Can J Anaesth. 1996;43:783-788.
Harris SN, Ballantyne GH, Luther MA, Perrino AC, Jr. Alterations of cardiovascular performance during laparoscopic colectomy: a combined hemodynamic and echocardiographic analysis. Anesth Analg. 1996;83:482-487.
Gebhardt H, Bautz A, Ross M, Loose D, Wulf H, Schaube H. Pathophysiological and clinical aspects of the CO2 pneumoperitoneum (CO2-PP). Surg Endosc. 1997;11:864-867.
Yamamoto S, Watanabe M, Hasegawa H, Baba H, Kitajima M. Short-term surgical outcomes of laparoscopic colonic surgery in octogenarians: a matched case-control study. Surg Laparosc Endosc Percutan Tech. 2003;13:95-100.
Whelan RL, Franklin M, Holubar SD, et al. Postoperative cell mediated immune response is better preserved after laparoscopic vs open colorectal resection in humans. Surg Endosc. 2003;17:972-978.
Wichmann MW, Huttl TP, Winter H, et al. Immunological effects of laparoscopic vs open colorectal surgery: a prospective clinical study. Arch Surg. 2005;140:692-697.
Huang C, Huang R, Jiang T, Huang K, Cao J, Qiu Z. Laparoscopic and open resection for colorectal cancer: an evaluation of cellular immunity. BMC Gastroenterol. 2010;10:127.
Surgery for colorectal cancer in elderly patients: a systematic review. Colorectal Cancer Collaborative Group. Lancet. 2000;356:968-974.
Bo M, Cacello E, Ghiggia F, Corsinovi L, Bosco F. Predictive factors of clinical outcome in older surgical patients. Arch Gerontol Geriatr. 2007;44:215-224.
Ansaloni L, Catena F, Chattat R, et al. Risk factors and incidence of postoperative delirium in elderly patients after elective and emergency surgery. Br J Surg. 2010;97:273-280.
Conflicts of Interest
None declared
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplement 1
Funnel plot of overall postopetrative complications (GIF 105 kb)
Supplement 2
Results of meta-regression analysis (GIF 17 kb)
Rights and permissions
About this article
Cite this article
Seishima, R., Okabayashi, K., Hasegawa, H. et al. Is laparoscopic Colorectal Surgery Beneficial for Elderly Patients? A Systematic Review and Meta-Analysis. J Gastrointest Surg 19, 756–765 (2015). https://doi.org/10.1007/s11605-015-2748-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2748-9