Abstract
Background
Due to the current increased longevity in the elderly population and the increased size of that population, major abdominal intervention is more frequently performed among octogenarians. This study aimed to compare the surgical and postoperative outcomes of laparoscopic colorectal resections with those of open surgery in the octogenarian population.
Methods
Retrospective analysis based on a prospectively maintained database of octogenarians who underwent laparoscopic or open elective colorectal resections from 2001 to 2008 was performed. Diagnosis, comorbidities, operative data, and early postoperative complications are analyzed in this report.
Results
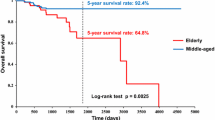
Colon resection was performed for 199 octogenarians, using laparotomy for 116 patients (group 1) and laparoscopic surgery for 83 patients (group 2). The mean age was 84.3 years for the laparotomy patients and 84.7 years for the laparoscopic patients. The American Society of Anesthesiology (ASA) scores was comparable between groups 1 and 2. Colorectal adenoma was the most common indication for surgery in both groups: for 77.6% of the group 1 patients and 54.2% of the group 2 patients. Right colectomy was the most frequently performed operation in group 2: for 57.8% of the group 2 patients and 31% of the group 1 patients (p = 0.0003). Open resections had a higher mean blood loss in both group 1 (286 ml) and group 2 (152 ml) (p = 0.0002), and more patients required intraoperative transfusions (p = 0.005) despite similar operative times. The conversion rate in the laparoscopic group was 25.3%. The patients in the laparoscopic group had less morbidity, both overall and clinically, than the open group (p < 0.05). The median hospital stay was 8 days in group 1 and 6 days in group 2 (p = 0.0065). The rate of major surgical complications was similar in the two groups of patients: 6% in group 1 and 4.8% in group 2. The reoperation rate was 2.6% in group 1 and 3.6% in group 2 (p > 0.05). The mortality rate was 3.4% in group 1 and 2.4% in group 2.
Conclusions
Laparoscopic colorectal resection was effective and safe for octogenarians, with less blood loss and faster postoperative recovery. The morbidity rate is lower than for traditional laparotomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The global life expectancy has dramatically changed over the recent decades. This change is attributed to a variety of reasons such as improved health care and advances in medicine. A 2003 annual report shows that in eastern countries, life expectancy at that time was 79 years for males and 85 for females [1]. In the United States, the elderly population (age >65 years) was 12.4% of the general population in the year 2000. It is predicted that in the year 2050, 86 million people will be part of this group, estimated to be 20.7% of the general population [1].
Laparoscopic colorectal surgery has proved to be a safe and feasible approach associated with a minimized immunologic and inflammatory response [2]. Some authors still do not consider laparoscopic surgery to be an acceptable surgical approach for elderly patients, although it is associated with faster recovery, reduced pain, early return to normal activities, and better cosmesis [3, 4]. Generally, the laparoscopic approach is associated with longer operative times and specific physiologic changes affecting the pulmonary and cardiovascular systems. These factors and existing comorbidities have convinced some surgeons to choose open surgery as opposed to the laparoscopic approach [3, 4].
Published data comparing laparoscopic with open colorectal surgery for the elderly patient are limited [5–12]. To date, several authors have published their colorectal laparoscopic surgical experience with octogenarian patients [5, 7–9]. Therefore, this study aimed to compare the surgical and early postoperative outcomes of laparoscopic colorectal resections with those of open surgery for octogenarians.
Methods
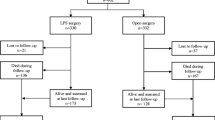
After institutional review board approval, a retrospective analysis based on a prospectively maintained surgical database of consecutive octogenarians who underwent laparoscopic or open colorectal resections from January 2001 to July 2008 was performed. The patients were divided into two groups. Group 1 consisted of the patients who underwent open colorectal resection, and group 2 comprised the patients who underwent laparoscopic colorectal resection.
The exclusion criteria ruled out urgent or emergent procedures, perineal procedures that included resection (such as perineal rectosigmoidectomy), and operations that did not include colon or rectal resection (such as stoma construction). The data evaluated included preoperative patient baseline parameters, surgical variables, and postoperative outcomes within 30 days after surgery. The preoperative parameters analyzed were age, gender, body mass index (BMI), American Society of Anesthesiology (ASA) classification, comorbid state, diagnosis, indication for surgery, and previous abdominal surgeries.
The operative data evaluation included type of procedure performed, operative time in minutes, estimated blood loss (EBL) in milliliters, intraoperative packed red blood cell transfusion, and intraoperative complications. For the laparoscopic cases, the reasons for conversion and the incision length also were obtained. An unplanned incision longer than 7 cm any time during the operation was considered a conversion to laparotomy.
Postoperative analysis included mortality rate, intensive care unit (ICU) stay, hospital length of stay (LOS), time elapsed until the first bowel movement and until toleration of a regular diet, exacerbation of preexisting medical conditions, and minor and major surgical complications. The complications were divided by whether an invasive approach (reoperation or radiologic drainage) was undertaken (major) or not (minor). For the overall analysis, all cases were included, including the converted cases from the laparoscopic group, on an intention-to-treat basis. Afterward, a separate analysis excluding the converted cases was performed to compare successfully completed laparoscopic cases and open cases.
Statistical analysis was performed using GraphPad Prism 2.01 (GraphPad Software, Inc., San Diego, CA, USA). Ordinal and categoric data were analyzed with Fisher’s exact test or unpaired t-test as appropriate. The Mann–Whitney U test was used for variables not distributed normally. Descriptive data were expressed as mean ± standard error of the mean (SEM), as medians and range, or as the number of patients and the percentage. Statistical significance was indicated when the p value was less than 0.05.
Results
During an 8-year period, 199 octogenarian patients underwent elective abdominal colorectal resections at Cleveland Clinic Florida. The oldest patient was 95 years old at the time of the operation. Group 1 (laparotomy) consisted of 116 patients, and group 2 (laparoscopy) had 83 patients. Table 1 presents the demographics of the groups, including the histopathologic assessment.
The incidence of comorbid conditions was high. Only 10.3% of the patients in group 1 (n = 12) and 10.8% of the patients in group 2 (n = 9) had no preexisting comorbidity. The proportion of patients with ASA score 3 or 4 was 69% in the open group (n = 80) and 56.6% in the laparoscopic group (n = 47). Right hemicolectomy was the most commonly performed surgery in both groups of patients, although it was performed for a higher percentage of patients in the laparoscopic group. Abdominoperineal resections were more commonly performed in the laparotomy group (Table 2).
Open surgery was 7.1 min faster than laparoscopic surgery, but the difference between the two groups was not significant. The open resections had a mean EBL 134.5 ml greater than the laparoscopic procedures. A larger proportion of patients in the open group required intraoperative red blood cell transfusions (Table 2).
Intraoperative complications occurred for 6.9% of the patients in group 1 (n = 8) and 4.8% of the patients in group 2 (n = 4). Four splenic injuries, three intestinal injuries, and one intraoperative bleeding occurred in the open group, which resulted in two splenectomies and two small bowel resections. In the laparoscopic group, one splenic injury, two small bowel injuries, and one intraoperative bleeding ensued, resulting in one small bowel resection.
The mean ICU stay did not differ significantly between group 1 (11.9 ± 0.7 days) and group 2 (2.0 ± 0.7 days). The patients in the laparoscopic group had a shorter LOS (median, 6 days; range, 3–54 days) than the patients in the open group (median, 8 days; range, 3–75 days) (p = 0.006). The time required for bowel recovery was similar in the two groups (a median interval of 5 days until the first bowel movement; p = 0.9), whereas the median interval until the first regular meal was 6 days in group 1 and 5 days in group 2 (p = 0.4).
The hospital readmission rate was 13.8% (n = 16) for the open group and 13.2% (n = 11) for the laparoscopic group. The reasons for readmission were related to exacerbation of medical conditions in 13 group 1 patients and 7 group 2 patients.
The surgical complication rates were similar in the two groups (Table 3). On the other hand, the medical complication rates were higher in the laparotomy group than in the laparoscopy group, showing that the medical complications related to the surgical procedure per se were more numerous in the open group (38.8% vs 25.3%; p = 0.03). Open cases resulted in more cardiovascular-, pulmonary-, and urinary-related complications, as shown in Table 3. The overall mortality rate was 3% (n = 6) for the four patients who underwent laparotomy and the two patients who underwent laparoscopy.
The rate of conversion to laparotomy was 25.3% (n = 21). The reasons for conversion were adhesions (47.6%, n = 10), bulky tumors (19%, n = 4), unclear anatomy (14.3%, n = 3), size of the incision (9.5%, n = 2), inability to identify the ureter (4.8%, n = 1), and carcinomatosis (4.8%, n = 1).
The converted cases that were completed without complications demonstrated significant differences in terms of mean operative time (156.2 vs 195.7 min; p = 0.008), mean intraoperative blood loss (129 vs 220 ml; p = 0.005), interval until the first bowel movement (4.5 vs 5.9 days; p = 0.001), interval until toleration of a regular diet (5.1 vs 7.9 days; p < 0.0001), postoperative medical complications (p = 0.02), surgical complications (p = 0.0006), and hospital readmission rate (p = 0.0045).
The operative and postoperative advantages of laparoscopy over laparotomy are analyzed in Table 4. Some added benefits of laparoscopy were fewer surgical, medical, and overall complications, faster recovery, and a smaller incision.
Discussion
Laparoscopic colectomy was not initially accepted widely due to the steep learning curve, extensive use of resources, fear of compromise of oncologic guidelines, and lengthy procedures [3]. This notion has drastically changed over the past decade, and laparoscopy currently is accepted as not only safe and feasible but also superior [3–5]. However, with all the advances in surgical abilities and techniques, some colorectal surgeons still consider age as a relative contraindication to laparoscopy [3–5].
Achievements in controlling, balancing, and minimizing the damaging effects of chronic comorbidities such as hypertension and diabetes as well as cardiovascular, pulmonary, and other chronic diseases have currently made it possible for patients to live a longer life with improved quality. With this increase in life expectancy, an increased incidence of lesions involving the colon and requiring colorectal surgery seems inevitable.
The postoperative morbidity of colorectal resections in elderly patients seems to be associated directly with underlying comorbidity. Previous studies of laparotomy in older patients have shown that mortality was caused primarily by cardiovascular complications and increased morbidity from respiratory problems [11, 12]. Therefore, older patients, who in many cases have comorbid diseases, may benefit from minimally invasive therapy for colorectal and other gastrointestinal diseases. This hypothesis concurs with a report by Law et al. [6], who observed a greater benefit of laparoscopic colorectal resections for patients older than 70 years due to less cardiopulmonary morbidity.
Age alone may not be considered a prognostic factor for gastrointestinal surgery. However, preoperative medical conditions may adversely influence outcome [13, 14]. Cheung et al. [15] analyzed laparoscopic resection for colorectal cancer in octogenarians and found no association between ASA score and postoperative morbidity. Other series have shown significant differences in postoperative morbidity between elderly and younger patients who preoperatively had significantly less medical compromise [8, 11, 16]. In the current study, the proportion of patients with severe medical conditions was high, as shown by the high ASA score in both groups. The protective factor of the minimally invasive therapy became evident by the decreased incidence of postoperative medical complications associated with laparoscopy.
In the current series, right colectomy was the most commonly performed procedure in both groups, although the incidences were higher in the laparoscopy group. Furthermore, abdominoperineal resections were most common in the laparotomy group. These differences could represent a selection bias based on an allocation of more complex surgeries to laparotomy. Other nonmatched studies investigating consecutive surgery series also had reported different procedures between the groups [11, 17].
The proportion of laparoscopic cases during the study period is another important aspect. 41.7% of 199 colorectal resections performed for octogenarians during an 8-year period in the current study were performed by laparoscopy performed by laparoscopy, which represented a higher proportion than reported by Senagore et al. [11] (28.9%) and a proportion similar to that reported by Law et al. [6] (42.2%).
Stoma construction and anastomosis were interrelated in the current study. 67.3% of 55 stomas in the laparotomy group, 67.3% were end stomas, the patients had no anastomosis. This finding is consistent with the higher incidence of absent anastomosis in the laparotomy group (29.3% vs 4.8%). Although the laparoscopic group had more patients with anastomosis, it did not have a higher incidence of major complications due to an intraperitoneal anastomosis.
Previous authors usually reported a shorter operative time for laparotomy [5–8, 10], except for Senagore et al. [11], who showed opposite results. Stocchi et al. [5] observed a significant decrease in the operative time for laparoscopy with increasing experience over time. The current study included similar operative times for both approaches, as previously shown by Person et al. [17] in a prior series at the same institution that used an end point of 65 years.
The analysis of blood loss in the current study favored the minimally invasive approach, as also shown in earlier reports [6, 7, 11]. Vignali et al. [7] confirmed greater blood loss associated with laparotomy, as substantiated with more patients needing homologous blood transfusion in this group of patients.
The incidence and type of intraoperative complications in the current study were similar between group 1 (6.9%) and group 2 (4.8%) and did not cause additional postoperative morbidity. None of the patients who had splenic or small bowel resections experienced more complications than the overall group. Similar intraoperative results were reported by Scheidbach et al. [16], who compared laparoscopic surgeries in patients older or younger than 75 years and noted respective intraoperative complication rates of 6.1% and 5.4%. Scheidbach et al. [16] also reported higher rates of morbidity (32.7% vs 17%) and mortality (4.1% vs 0.7%) among elderly patients, predominantly due to cardiorespiratory and other medical complications.
In the current study, as expected, the incidence of cardiovascular, respiratory, and urinary morbidity in a group of octogenarian patients was high. Nevertheless, the patients who underwent laparoscopic surgery had less exacerbation of preexisting medical comorbidity than the patients who had laparotomy. The advantages were accentuated in patients in whom laparoscopic procedures were successfully completed.
Postoperative recovery was faster with the minimally invasive approach, which was represented by a shorter hospital stay, as reported in earlier studies. Intra- and postoperative outcomes among different institutions that compared open and laparoscopic colorectal resections in elderly patients are described in Table 5. The current study showed a shorter hospital stay for laparoscopy, although the time until bowel movements was similar and the time to resumption of a regular diet was shorter only after complete laparoscopy.
Surgical morbidity was similar for laparotomy and laparoscopy, as shown by other studies [5, 7, 8, 11, 12]. The incidence of anastomotic leak in the elderly population varied from 0% to 6.5% [6–8, 11–13]. The overall leak rate for our patients was 1.5%, which is consistent with the literature. The leak rate for laparoscopy was relatively higher (2.4% vs 0.8%), possibly due to the higher incidence of anastomosis construction among these patients. Reoperation also was consistent with other data reflecting rates of 1% to 6.3% after laparoscopic surgery and 0.8% to 9% after laparotomy [5–8, 11, 12]. The current series had reoperation rates of 2.6% after laparotomy and 3.6% after laparoscopy, with no significant difference between the two groups.
Hospital readmission was not well described in the studies reviewed. However, elderly patients have a tendency to return to the hospital due to less reserve and medically associated conditions. Senagore et al. [11] noted low readmission rates for older patients undergoing laparoscopy (6%) and laparotomy (6.5%). However, these authors reported significantly higher readmission rates for young patients who underwent laparoscopic colorectal resections rather than laparotomy. Our readmission rates were approximately 13% for both groups due to medically related problems in nearly all the patients.
Conversion rates are always debatable and vary widely depending on definition. The reported conversion rates for elderly patients range from 1% to 25% [5–8, 11, 12, 15, 18]. The current series had a rate of 25.3% for conversions, most of which were preemptive and not reactive [19].
Several prior studies have compared the laparoscopic approach between elderly and young patients, showing relatively worse results for the elderly. The findings were attributed to the higher preoperative morbidity in the elderly patients [16, 17]. The largest study investigating laparoscopic colorectal resections for cancer in octogenarians was reported by Cheung et al. [15]. The authors had outstanding outcomes including an average operative time of 110 min, an EBL of 50 ml during surgery, and one conversion. The postoperative morbidity was 17%, and the mortality was 3%, although the study lacked a control group.
The results of the current study endorse the reliability and feasibility of laparoscopic colorectal resections, which should encourage surgeons to increase their offering of laparoscopy to elderly patients, especially octogenarians. Laparoscopy should be the preferred approach for octogenarians.
Conclusions
Laparoscopic colorectal resection is effective and safe for octogenarians. Compared with laparotomy, laparoscopy did not require a longer time to perform. Consequently, it was associated with less blood loss, less intraoperative transfusion, a shorter hospital stay, and a lower morbidity rate than laparotomy. These results were even more pronounced when the completely successful laparoscopic cases were evaluated separately.
References
Annual report 2003. Department of Health, Hong Kong, SAR. Retrieved 30 January 2009 at http://www.census.gov/population/www/projections/usinterimproj/
Sylla P, Kirman I, Whelan RL (2005) Immunological advantages of advanced laparoscopy. Surg Clin North Am 85:1–18
Abraham NS, Young JM, Solomon MJ (2004) Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg 91:1111–1124
Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, Lai PB, Lau WY (2004) Laparoscopic resection of rectosigmoid carcinoma: prospective randomized trial. Lancet 363:1187–1192
Stocchi L, Nelson H, Young-Fadok TM, Larson DR, Ilstrup DM (2000) Safety and advantages of laparoscopic vs open colectomy in the elderly: matched-control study. Dis Colon Rectum 43:326–332
Law WL, Chu KW, Tung PH (2002) Laparoscopic colorectal resection: a safe option for elderly patients. J Am Coll Surg 195:768–773
Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C (2005) Laparoscopic vs open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum 48:2070–2075
Sklow B, Read T, Birnbaum E, Fry R, Fleshman J (2003) Age and type of procedure influence the choice of patients for laparoscopic colectomy. Surg Endosc 17:923–929
Stewart BT, Stitz RW, Lumley JW (1999) Laparoscopically assisted colorectal surgery in the elderly. Br J Surg 86:938–941
Feng B, Zheng MH, Mao ZH, Li JW, Lu AG, Wang ML, Hu WG, Dong F, Hu YY, Zang L, Li HW (2006) Clinical advantages of laparoscopic colorectal cancer surgery in the elderly. Aging Clin Exp Res 18:191–195
Senagore AJ, Madbouly KM, Fazio VW, Duepree HJ, Brady KM, Delaney CP (2003) Advantages of laparoscopic colectomy in older patients. Arch Surg 138:252–256
Frasson M, Braga M, Vignalli A, Zuliani W, Di Carlo V (2008) Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 51:296–300
Fielding LP, Philips RK, Hittinger R (1989) Factors influencing mortality after curative resection for large bowel cancer in elderly patients. Lancet 1:595–597
Payne JE, Chapuis PH, Pheils MT (1986) Surgery for large bowel cancer in people aged 75 years and older. Dis Colon Rectum 29:733–737
Cheung HYS, Cung CC, Fung JTK, Wong JCH, Yau KKK, Li MKW (2007) Laparoscopic resection for colorectal cancer in octogenarians: results in a decade. Dis Colon Rectum 50:1905–1910
Scheidbach H, Schneider C, Hugel O, Yildirim C, Lippert H, Köckerling F (2005) Laparoscopic surgery in old patients: do indications and outcomes differ? Langenbecks Arch Surg 390:328–332
Person B, Cera SM, Sands DR, Weiss EG, Vernava AM, Nogueras JJ, Wexner SD (2007) Do elderly patients benefit from laparoscopic colorectal surgery? Surg Endosc 22:401–405
De Santis L, Frigo F (2006) Laparoscopic colorectal surgery in the elderly. Acta Bio-Medica de I Ateneo Parmense 76:24–26
Shawki S, Bashankaev B, Denoya P, Seo C, Weiss EG, Wexner SD (2009) What is the definition of “conversion” in laparoscopic colorectal surgery? Surg Endosc 23:2321–2326
Disclosures
Steven D. Wexner is a consultant in the field of laparoscopy for Covidien and for Karl Storz Endoscopy. He is also entitled to recieve inventors income from Karl Storz Endoscopy. Rodrigo A. Pinto, Dan Ruiz, Yair Edden, Eric G. Weiss, and Juan J. Nogueras have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinto, R.A., Ruiz, D., Edden, Y. et al. How reliable is laparoscopic colorectal surgery compared with laparotomy for octogenarians?. Surg Endosc 25, 2692–2698 (2011). https://doi.org/10.1007/s00464-011-1631-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1631-3