Abstract
Background
Acute colorectal obstruction requires immediate surgical treatment. Although one-stage surgery with transanal drainage tubes (TDT) is reportedly safe and feasible, the long-term outcome of this procedure remains unclear.
Aim
To assess the outcome of one-stage surgery using TDT in the acute left colon or rectal obstructions due to colorectal carcinomas.
Methods
Clinicopathological data were recorded from patients with colorectal cancer with acute obstructions between 2006 and 2013.
Results
A total of 43 patients were enrolled including 29 males and 14 females. Among 39 patients, TDT was successful in 33 (84 %) and was incomplete in 6. Thus, 33 patients received one-stage surgery with TDT decompression, and 9 patients, including 6 with incomplete decompression, received one-stage surgery with no decompression. No significant differences in clinicopathological factors were observed between decompression and non-decompression groups. Adjusted analyses revealed that decompression using TDT was significantly associated with OS (hazard ratio 0.24; 95 % confidence interval, 0.08–0.72; p = 0.01). Furthermore, OS in the TDT decompression group was significantly longer than that in the non-decompression group (p = 0.01).
Conclusions
One-stage surgery with decompression using TDT may be effective to avoid stomas and to improve overall survival in patients with obstructing colorectal cancers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients with obstructing colorectal cancers are known to have poorer outcomes than those with no obstructions.1,2 A previous study showed that approximately 20 % patients with colorectal cancer developed colorectal obstructions, which may present as life-threatening emergencies that are often difficult to manage.3 Furthermore, patients with obstructing colorectal cancers are usually elderly and often have underlying diseases that lead to risks during major surgery.1,2
Most surgeons advocate two-stage surgery to avoid major postoperative complications, such as anastomotic leakage and septic multiple organ failure, which increase morbidity and mortality.4,5 Two-stage surgery with stoma, colostomy or ileostomy is a safe and feasible procedure that overcomes critical situations, but increases patient discomfort, cost, and duration of hospitalization. Several previous studies demonstrate one-stage surgeries including intraoperative colonic lavage,6 preoperative small bowel and colonic decompression, and lavage with long nasointestinal tubes.7,8 Decompression using self-expandable metallic stents has recently been shown to relieve malignant colorectal obstructions.3,9–12 However, decompression with transanal drainage tubes (TDT) also helps avoid two-stage surgery.13–16 These two new procedures reportedly facilitate management of obstructing colorectal cancers, although the associated safety, cost, and technical aspects remain unclear.
Although decompression before one-stage surgery is known to be effective, the long-term outcomes of this procedure remain unclear. Sabbagh et al. reported that compared with immediate surgery, insertion of self-expanding metallic stents decreased overall survival (OS) of patients.17 However, the long-term outcomes of one-stage surgery with TDT remain unclear.
In this study, we present the outcomes of one-stage surgery with TDT decompression and make comparisons with non-decompression patients to assess the outcomes of one-stage surgery using TDT decompression for management of acute left colon and rectal obstructions due to colorectal carcinomas.
Materials and Methods
Patients and Data Extraction
Obstructing colorectal cancers were retrospectively identified in 61 patients from our institution between 2006 and 2013. These patients were admitted to our hospital with abdominal pain, distension of the abdomen, vomiting, or melena due to acute colonic obstructions.
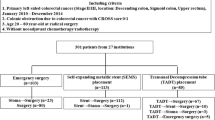
Eight patients with colon perforations at hospital admission and ten patients who received two-stage surgery were excluded from the present analysis. Thus, data were included for a total of 43 patients (Fig. 1). Age, sex, body mass index (BMI), tumor location, tumor differentiation, depth of invasion, presence of lymphovascular invasion, number of dissected and metastatic lymph nodes, presence of synchronous metastasis, postoperative complications, duration of hospitalization, and status at most recent follow-up were retrospectively recorded through a review of medical records.
Emergency and Planned Procedures
Procedure of Transanal Drainage Tube
TDT were Dennis colorectal tubes (22 Fr) having an outer diameter of 7.3 mm and length of 120 cm (Nippon Sherwood, Tokyo, Japan).14,18 Urgent colonoscopy was performed after evaluation of acute colorectal obstructions. Under fluoroscopic and endoscopic guidance, guide wires were introduced through the tumor beyond the point of the obstruction and as proximal as possible to the distended colon. Subsequently, the endoscope was removed and a Dennis colorectal tube was introduced over the guide wire. After confirming that the balloon part of the tube had passed the lesion, the balloon was inflated with 15–20 ml of sterilized water, and the position of the tube was fixed. Finally, the intestinal tract was flushed several times with water.
Immediately following the tube placement, the colon is irrigated discontinuously using 3 to 5 L of warm water. Because the tube may be clogged easily by suctioning shortly after TDT placement, irrigation and suctioning should be performed by hand. Oral intake was restricted during decompression, and the intestinal tract was cleaned twice or thrice daily using 500–1,000 ml of water for a few days before surgery until fecal colonic content was reduced. After colorectal dilatation is relieved, contrast radiography of the proximal colon was performed to exclude the possibility of synchronous carcinomas. One- or two-stage surgical procedures were then selected on the basis of clinical conditions.
Surgical Procedures
Patients with TDT decompression elected to receive either laparoscopic or open surgery. Patients in whom TDT placement failed to reduce pressure in the intestinal tract received emergency one-stage surgery. Colectomy was performed according to optimal oncological principles in both groups regardless of whether the surgery was elective or emergency.
Oncological Management
Adjuvant chemotherapy was suggested for patients with stage II or III disease, and systemic chemotherapy was suggested for stage IV patients. Follow-up comprised a combination of physical examinations and serum tumor marker tests at 3 months, ultrasound or computerized tomography scans at 6 months, and an annual colonoscopy.
Statistical Analysis
All statistical analyses were performed using Stata software Version 11.0 (StatCorp, College Station, TX, USA). Relationships between treatment groups and clinicopathological variables were evaluated using chi-square or Mann–Whitney U tests, and differences were considered significant when p < 0.05. OS was defined as the time between the day of surgery and the date of death or last follow-up. Survival distributions were estimated using the adjusted Kaplan–Meier method and were compared using log-rank tests.
Univariate and multivariate Cox proportional hazards models were used to assess prognostic factors for overall survival and to compute hazard ratios and their 95 % confidence intervals.
Results
Patient Characteristics
Data was collected and analyzed for a total of 43 patients (29 males, 67 %; 14 females, 33 %). The median age at diagnosis was 70 years (interquartile range, 62–77 years). Tumors were located in the colons of 38 patients and in the rectums of 5 patients. Twenty-six patients had stage 2 or 3 disease and 17 had stage 4 disease. The median OS was 18 months (interquartile range, 12–38).
Decompression using TDT was successful in 33 patients (decompression group) and was unsuccessful in 10 patients (non-decompression group). Demographic and oncological characteristics of the patient population are shown in Table 1. There were no significant differences in preoperative data, pathological data, synchronous metastasis rates, or number of hospital admissions between decompression and non-decompression groups.
Postoperative Outcomes
Short-Term Outcomes
TDT decompression was performed in 39 patients (90.7 %); it was successful in 33 (84.6 %) and failed in 6. The tumor was located in the sigmoid colon in all six cases. During endoscopy, guide wire passage through the primary tumor was not feasible in 7.7 % of cases (3 of 39 patients). Perforations (7.7 % of cases) due to the guide wire were diagnosed during TDT insertion in three patients, who were subsequently treated with emergency surgery. Trans-nasal drainage tubes were placed in the intestines of three patients, but were not effective, and emergency surgery was performed without decompression. One patient received an emergency Hartmann’s operation.
The median time from TDT insertion to surgery was 12 (interquartile range, 8–16) days. The median number of resected lymph nodes in the decompression group was 24 (interquartile range, 14–43) and was 17 (interquartile range, 8–26) in the non-decompression group. No differences in chemotherapy (either adjuvant or systemic chemotherapy) access rates were found between the two groups (60.6 vs. 50 %, p = 0.18). The stoma rate was significantly lower, and the primary anastomosis rate was significantly higher in decompression group than in the non-decompression group (stoma, 6.1 vs. 50 %, p = 0.001; primary anastomosis, 96.7 vs. 70 %, p = 0.01); however, there were no differences in anastomosis leakage rates (3.0 vs. 10 %, p = 0.36). No postoperative peritoneal sepsis or surgery-related mortality occurred in either group. Perioperative and oncological data are summarized in Tables 1 and 2.
Long-Term Outcomes
Cancer-specific mortality rates (33.3 vs. 80 %, p = 0.009) were significantly lower in the TDT decompression group. Accordingly, median overall survival was 19 months (interquartile range, 12–44) in the TDT decompression group, and 14 months (interquartile range, 12–23) in the non-decompression group.
One patient with perforation that occurred due to TDT insertion developed liver metastasis within 50 months after surgery and receiving systemic chemotherapy, with the overall survival of 58 months. Two other patients with perforation died after surgery with the overall survival of 14 and 16 months. Peritoneal dissemination was not detected in all three cases.
Median time interval for cancer-specific mortality in total was 18 months (interquartile range, 13–32). Furthermore, median time interval was 24 months (interquartile range, 16–48) in the TDT decompression group and 14 months (interquartile range, 9.5–19.5) in the TDT decompression group. Although there was no significant difference, patients with TDT decompression were more likely to have long time interval (p = 0.052).
Univariate analysis showed that TDT decompression [hazard ratio (HR), 0.24; 95 % confidence interval (CI), 0.09–0.64; p = 0.004], tumor differentiation (HR, 7.41; 95 % CI, 1.41–38.99; p = 0.02), and lymphatic invasion (HR, 2.95; 95 % CI, 1.15–7.62; p = 0.02) were significantly associated with OS (Table 3). Furthermore, multivariate analysis revealed that TDT decompression significantly affected OS (HR, 0.24; 95 % CI, 0.08–0.72; p = 0.01; Table 3).
After adjustment for tumor differentiation and the presence of lymphovascular invasions and synchronous metastasis, OS was significantly longer in the decompression group than in the non-decompression group (log rank test, p = 0.01). Kaplan–Meier curves are shown in Fig. 2.
Discussion
Acute colorectal obstructions are potentially life-threatening, and colorectal carcinomas are known as the most common cause of large bowel obstructions.19 Accordingly, McGregor and O’Dwyer reported that 15–20 % of all colon carcinomas present with acute bowel obstruction.20 Furthermore, almost 90 % of large bowel obstructions are distal to the splenic flexure.1 The management of acute colorectal obstructions, particularly in the left side of the colon and rectum, generally mandates emergency surgical procedures and decompression of the intestinal tract. Because of the poor general conditions, such as electrolyte disturbances, dehydration, and other medical comorbidities, two-stage surgery is frequently selected.1,2,4 However, quality of life decreases with discomfort of the stoma, and previous studies report various feasible and safe treatment procedures for one-stage surgery including intraoperative colonic lavage, decompression with colonic stents, and decompression using TDT for patients with primary anastomosis and no stoma.5,6,8,10,12 However, intraoperative colonic lavage is not a standard treatment and is associated with a high frequency of postoperative complications.6,21
Reportedly, mortality rates for emergency surgery are much higher than those for elective surgery regardless of whether the operation is one- or two-stage.22,23 Because high postoperative morbidity and mortality rates correlate with general status, strong recovery from severe surgical and disease events can significantly reduce mortality.24 Importantly, colonic stents and TDT decompressions are known to effectively improve patient conditions.
This study compared the outcome of one-stage surgery with or without decompression of the intestinal tract using TDT. Numerous studies report the impact of TDT decompression as a “bridge to surgery” that avoids stoma. However, the effects on OS remain poorly understood, and the present study is the first to report significant effects of TDT decompression in obstructing colorectal cancer treatments. Importantly, multivariate analyses showed a significant association between successful TDT decompression and OS. Although clinicopathological factors did not differ between the present study groups, OS was significantly longer in the TDT decompression group than in the non-decompression group. However, the reason why TDT decompression improved OS remains unclear. Okamoto et al. reported the association between gut-associated lymphoid tissue changes and infectious complication morbidity.25 Although the study design and target differ from our study, we hypothesize that the poor general conditions occurred due to the fact that obstructing colorectal cancer may associate with the suppression of antitumor immunity, and this factor may contribute to worsening overall survival in non-decompression group.
In this study, TDT decompression was performed in 39 patients with obstructing colorectal cancer, with a technical success rate of 84.6 % and a perforation rate of only 7.7 %. Similarly, previous studies report successful placement of TDT in 84–98 % of patients.14,16,19 Moreover, all failures of TDT placement occurred in patients with cancers of the sigmoid colon. Accordingly, Fischer et al. reported that decompression failures increase with the height of the tumor in the colon.19 Success of TDT placement may not depend on the stage of cancer progression. Perforation occurred in three of the present cases, and primary anastomosis was performed. However, peritoneal sepsis did not occur in all cases and perforations caused by TDT did not significantly affect short-term outcomes of emergency surgery. Moreover, among all of the present subjects, the median time interval from emergency admission to surgery was 12 days.
Colonic stents are widely used to facilitate bowel decompression and to act as a “bridge to surgery”.26 Compared with emergency surgery, colonic stents have many advantages including decreased rates of morbidity, mortality, permanent stoma, and surgical site infections.27–29 However, randomized controlled trials indicated no decisive clinical advantages of colonic stenting for emergency surgery.30,31 Furthermore, Sabbagh et al. reported inferior OS of patients with obstructing colorectal cancers after insertion of self-expandable metal stents during immediate surgery.17 Thus, although colonic stents may be an effective method for decompression of the intestinal tract and as a “bridge to surgery,” their efficacy remains controversial.
Colonic stents can also facilitate immediate resumption of eating, leading to improved quality of life and shorter hospital stays. However, Fernández-Esparrach et al. reported late complications after placement of colonic stents including migration, stent reobstruction and late perforation.32 These complications may have led to shorter OS of patients in the study by Sabbagh et al.17 On the other hand, TDT decompression improved OS compared with the non-decompression group in this current study. This conflicting result may be due to the risk of migration of colonic stents. There is a possibility of improvement in overall survival using TDT rather than colonic stents; however, further investigation is required to assess this contradiction.
Neo-adjuvant chemotherapy is known to be effective treatment for rectal cancer. Neo-adjuvant chemotherapy with colonic stents or diverting stoma may be another treatment option for obstructing rectal cancer. However, there are many studies that report the association between late complication (including perforation) of colonic stent and chemotherapy.33 Neo-adjuvant chemotherapy with diverting stoma seems to be safe and feasible, but the quality of life decreases with discomfort of the stoma. Further study is needed to clarify the best treatment for rectal cancer.
Although medical expenses may be different in each country, the estimated cost was calculated for inhospital stay, colonic stent, and two-stage surgery with diverting stoma. The estimated cost was approximately US$17,000 (1.7 million yen) by TDT decompression (including 12 days of interval from the emergency admission to surgery), whereas colonic stent (including 3 days of hospital stay after the insertion) was US$20,000 (two million yen) and two-stage surgery (including 3 days of hospital stay after the stoma operation) was US$17,000 (1.7 million yen). The estimated cost of colonic stent was the most expensive procedure in Japan; however, TDT decompression was little differentiated from two-stage surgery.
The conclusions of the present study are limited by small patient numbers, a relatively short follow-up period, and a retrospective design. Moreover, some of the subjects failed to return to the hospital and others are still being treated with systemic chemotherapy. Thus, large prospective studies assessing postoperative recurrence and OS are required to validate the effects of TDT decompression in one-stage surgery for obstructing colorectal cancer. Nonetheless, the present study is the first to investigate the efficacy of one-stage surgery with TDT decompression for patients with obstructing colorectal cancers and may motivate future research and the use of minimally invasive treatments.
Conclusion
Decompression using TDT may be an effective technique for one-stage surgery and may help avoid stoma and preserve quality of life. Moreover, the present data suggest that TDT decompression improves overall survival in obstructing colorectal cancer.
References
Ohman U. Prognosis in patients with obstructing colorectal carcinoma. American journal of surgery 1982;143:742–7.
Deans GT, Krukowski ZH, Irwin ST. Malignant obstruction of the left colon. The British journal of surgery 1994;81:1270–6.
Baron TH, Rey JF, Spinelli P. Expandable metal stent placement for malignant colorectal obstruction. Endoscopy 2002;34:823–30.
Deutsch AA, Zelikovski A, Sternberg A, Reiss R. One-stage subtotal colectomy with anastomosis for obstructing carcinoma of the left colon. Diseases of the colon and rectum 1983;26:227–30.
Binkert CA, Ledermann H, Jost R, Saurenmann P, Decurtins M, Zollikofer CL. Acute colonic obstruction: clinical aspects and cost-effectiveness of preoperative and palliative treatment with self-expanding metallic stents—a preliminary report. Radiology 1998;206:199–204.
Murray JJ, Schoetz DJ, Jr., Coller JA, Roberts PL, Veidenheimer MC. Intraoperative colonic lavage and primary anastomosis in nonelective colon resection. Diseases of the colon and rectum 1991;34:527–31.
Terasaka R, Itoh H, Nakafusa Y, Matsuo K. Effectiveness of a long intestinal tube in a one-stage operation for obstructing carcinoma of the left colon. Diseases of the colon and rectum 1990;33:245–8.
Adachi Y, Okita K, Nozoe T, Iso Y, Yoh R, Matsumata T. Long tube for obstructing left-sided colon cancer. Digestive surgery 1999;16:178–9.
Camunez F, Echenagusia A, Simo G, Turegano F, Vazquez J, Barreiro-Meiro I. Malignant colorectal obstruction treated by means of self-expanding metallic stents: effectiveness before surgery and in palliation. Radiology 2000;216:492–7.
Martinez-Santos C, Lobato RF, Fradejas JM, Pinto I, Ortega-Deballon P, Moreno-Azcoita M. Self-expandable stent before elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rates. Diseases of the colon and rectum 2002;45:401–6.
Suzuki N, Saunders BP, Thomas-Gibson S, Akle C, Marshall M, Halligan S. Colorectal stenting for malignant and benign disease: outcomes in colorectal stenting. Diseases of the colon and rectum 2004;47:1201–7.
Mucci-Hennekinne S, Kervegant AG, Regenet N, Beaulieu A, Barbieux JP, Dehni N, Casa C, Arnaud JP. Management of acute malignant large-bowel obstruction with self-expanding metal stent. Surgical endoscopy 2007;21:1101–3.
Tanaka T, Furukawa A, Murata K, Sakamoto T. Endoscopic transanal decompression with a drainage tube for acute colonic obstruction: clinical aspects of preoperative treatment. Diseases of the colon and rectum 2001;44:418–22.
Horiuchi A, Nakayama Y, Tanaka N, Kajiyama M, Fujii H, Yokoyama T, Hayashi K. Acute colorectal obstruction treated by means of transanal drainage tube: effectiveness before surgery and stenting. The American journal of gastroenterology 2005;100:2765–70.
Yokohata K, Sumiyoshi K, Hirakawa K. Merits and faults of transanal ileus tube for obstructing colorectal cancer. Asian journal of surgery/Asian Surgical Association 2006;29:125–7.
Xu M, Zhong Y, Yao L, Xu J, Zhou P, Wang P, Wang H. Endoscopic decompression using a transanal drainage tube for acute obstruction of the rectum and left colon as a bridge to curative surgery. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 2009;11:405–9.
Sabbagh C, Chatelain D, Trouillet N, Mauvais F, Bendjaballah S, Browet F, Regimbeau JM. Does use of a metallic colon stent as a bridge to surgery modify the pathology data in patients with colonic obstruction? A case-matched study. Surgical endoscopy 2013;27:3622–31.
Horiuchi A, Maeyama H, Ochi Y, Morikawa A, Miyazawa K. Usefulness of Dennis Colorectal Tube in endoscopic decompression of acute, malignant colonic obstruction. Gastrointestinal endoscopy 2001;54:229–32.
Fischer A, Schrag HJ, Goos M, Obermaier R, Hopt UT, Baier PK. Transanal endoscopic tube decompression of acute colonic obstruction: experience with 51 cases. Surgical endoscopy 2008;22:683–8.
McGregor JR, O’Dwyer PJ. The surgical management of obstruction and perforation of the left colon. Surgery, gynecology & obstetrics 1993;177:203–8.
Biondo S, Perea MT, Rague JM, Pares D, Jaurrieta E. One-stage procedure in non-elective surgery for diverticular disease complications. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 2001;3:42–5.
Runkel NS, Schlag P, Schwarz V, Herfarth C. Outcome after emergency surgery for cancer of the large intestine. The British journal of surgery 1991;78:183–8.
Griffith RS. Preoperative evaluation. Medical obstacles to surgery. Cancer 1992;70:1333–41.
Tobaruela E, Camunas J, Enriquez-Navascues JM, Diez M, Ratia T, Martin A, Hernandez P, Lasa I, Martin A, Cambronero JA, Granell J. Medical factors in the morbidity and mortality associated with emergency colorectal cancer surgery. Revista espanola de enfermedades digestivas : organo oficial de la Sociedad Espanola de Patologia Digestiva 1997;89:13–22.
Okamoto K, Fukatsu K, Hashiguchi Y, Ueno H, Shinto E, Moriya T, Saitoh D, Yamamoto J, Hase K. Lack of preoperative enteral nutrition reduces gut-associated lymphoid cell numbers in colon cancer patients: a possible mechanism underlying increased postoperative infectious complications during parenteral nutrition. Annals of surgery 2013;258:1059–64.
Kim JS, Hur H, Min BS, Sohn SK, Cho CH, Kim NK. Oncologic outcomes of self-expanding metallic stent insertion as a bridge to surgery in the management of left-sided colon cancer obstruction: comparison with nonobstructing elective surgery. World journal of surgery 2009;33:1281–6.
Meisner S, Hensler M, Knop FK, West F, Wille-Jorgensen P. Self-expanding metal stents for colonic obstruction: experiences from 104 procedures in a single center. Diseases of the colon and rectum 2004;47:444–50.
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M. Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. The American journal of gastroenterology 2004;99:2051–7.
Huang X, Lv B, Zhang S, Meng L. Preoperative Colonic Stents Versus Emergency Surgery for Acute Left-Sided Malignant Colonic Obstruction: A Meta-analysis. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2014;18:584–91.
Bridoux V, Kianifard B, Moutel G, Herve C, Tuech JJ. Stenting as a bridge to surgery for colorectal cancer. The lancet oncology 2011;12:621; author reply -2.
Kuss O, Legler T, Borgermann J. Treatments effects from randomized trials and propensity score analyses were similar in similar populations in an example from cardiac surgery. Journal of clinical epidemiology 2011;64:1076–84.
Fernandez-Esparrach G, Bordas JM, Giraldez MD, Gines A, Pellise M, Sendino O, Martinez-Palli G, Castells A, Llach J. Severe complications limit long-term clinical success of self-expanding metal stents in patients with obstructive colorectal cancer. The American journal of gastroenterology 2010;105:1087–93.
Abbott S, Eglinton TW, Ma Y, Stevenson C, Robertson GM, Frizelle FA. Predictors of outcome in palliative colonic stent placement for malignant obstruction. The British journal of surgery 2014;101:121–6.
Acknowledgments
The authors thank A. Asami, K. Takeshima, K. Nagasaki, N. Okamoto, H. Shinozaki, T. Mizutani, and K. Miura for their technical support and helpful discussions.
Grant Support
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shigeta, K., Baba, H., Yamafuji, K. et al. Outcomes for Patients with Obstructing Colorectal Cancers Treated with One-Stage Surgery Using Transanal Drainage Tubes. J Gastrointest Surg 18, 1507–1513 (2014). https://doi.org/10.1007/s11605-014-2541-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2541-1