Abstract
Background
Colorectal stents are being used for palliation and as a “bridge to surgery” in obstructing colorectal carcinoma. The purpose of this study was to review our experience with self-expanding metal stents (SEMS) as the initial interventional approach in the management of acute malignant large bowel obstruction.
Methods
Between February 2002 and May 2006, 67 patients underwent the insertion of a SEMS for an obstructing malignant lesion of the left-sided colon or rectum.
Results
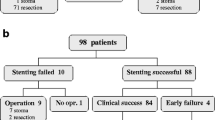
In 55 patients, the stents were placed for palliation, whereas in 12 they were placed as a bridge to surgery. Stent placement was technically successful in 92.5% (n = 62), with a clinical success rate of 88% (n = 59). Two perforations that occurred during stent placement we retreated by an emergency Hartmann operation. In intention-to-treat by stent, the peri-interventional mortality was 6% (4/67). Stent migration was reported in 3 cases (5%), and stent obstruction occurred in 8 cases (13.5%). Of the nine patients with stents successfully placed as a bridge to surgery, all underwent elective single-stage operations with no death or anastomotic complication.
Conclusions
Stent insertion provided an effective outcome in patients with malignant colonic obstruction as a palliative and preoperative therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Self-expanding metallic stents (SEMS) have been used to relieve obstruction in many different settings, including cardiac, peripheral vascular, biliary, hepatic, and esophageal [3, 12, 23, 25]. Stent application to colonic lesions was first described by DOHMOTO [7] in 1991. in 1994, TEJERO et al. [30] published a preliminary report of two patients with colonic obstruction who had metallic stents placed before surgery. Since then, a number of publications have appeared that suggest that colonic stent placement is a relatively simple and safe alternative to standard surgical management of acute malignant obstruction of the left colon, thereby obviating the need for emergency surgery or colostomy [4, 29, 32].
The aim of this study was to review our experience with self-expanding stents as the initial interventional approach in the management of acute malignant large-bowel obstruction.
Patients and methods
From February 2002 to May 2006, 67 patients (42 men, 25 women) with a mean age of 73.5 years (range, 47–97 years) underwent the insertion of a SEMS for an obstructing neoplastic lesion in the left-sided colon or rectum. In 55 patients, the procedure was considered as a definitive palliative measure for obstructing primary colorectal cancer. The following indications for SEMS implantation were observed:
-
Metastasized colorectal carcinoma and general inoperability in 33 patients.
-
Local unresecability of the colorectal carcinoma in 6 multimorbid patients.
-
High operative risk (ASA 4) in 5 patients.
-
Recurrent tumor growth of the colorectum extraluminally with consecutive colonic obstruction in one patient.
Twelve patients (18%) had stent placement as a bridge to surgery, with plans to undergo an elective procedure within 2 weeks of stent placement. All patients had clinical features of colorectal obstruction with symptoms of constipation and abdominal distension. The abdominal x-ray films showed dilated colon proximal to the obstruction site. The obstruction was confirmed by water-soluble enema examinations (n = 21), computed tomographic (CT)-scan (n = 45), and endoscopy (n = 67), and SEMS placement was performed under endoscopic and fluoroscopic control within 12 h of diagnosis. Patients with features of peritonitis were excluded.
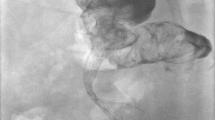
The endoprosthesis used was Hanarostent (MI Tech). The patients were placed in a left lateral position on the fluoroscopic table. Conscious sedation was used in all patients. Blood pressure, pulse oximetry, and heart rate were continuously monitored. A flexible video-colonoscope was advanced until the tumor was identified. A water-soluble contrast agent was injected via the working channel of the colonoscope using fluoroscopy to delineate the length of the obstruction. A flexible guidewire was then introduced via the working channel of the colonoscope and passed across the tumor under fluoroscopic guidance. The stent and its delivery system (Hanarostent, MI Tech) were then introduced over the guidewire, and the stent was deployed to the desired position under fluoroscopic guidance. The stent was deployed so that it was centered on the area of the stenosis. The length of the stent was chosen such that the proximal and the distal ends of the stent rested a few centimetres proximal and distal to the lesion. A water-soluble enema examination was performed immediately after the procedure or the following day to check for patency and leakage. Success of the procedure was defined as the relief of obstruction within 24 h after placement of the stent. Complications were defined as early and late (i.e., occurring < 30 days or > 30 days after the procedure, respectively).
Results
In 67 patients with acute malignant large-bowel obstruction, the site of obstruction was rectosigmoid junction (n = 28), sigmoid colon (n = 24), descending colon (n = 12), and splenic flexure (n = 2). In one patient with recurrent sigmoid colon cancer following surgery, a stent was placed at the anastomotic site. The length of the obstructions ranged from 2 to 11 cm (mean, 6 cm). In three patients with a stricture of the sigmoid colon, stent placement was not possible, because the stricture could not be negotiated with a guidewire. These patients were taken to the operating room for a left colectomy (n = 2) and a colostomy (n = 1). Complications occurred in four patients who underwent SEMS placement: two perforations during stent placement diagnosed immediately and treated by an emergency Hartmann operation, one no stent expansion, and one immediate stent migration above the tumoral stenosis. The latter two cases were treated by immediate stent reinsertion. Stent placement was technically successful in 62 patients (92.5%), with a clinical success rate of 88% (n = 59); in three patients, the stent that was placed did not decompress the obstruction completely, requiring stent reinsertion in two cases (respectively on the 5th and 7th day) and a colostomy in one case (on the 5th day). In intention-to-treat by stent, the peri-interventional mortality was 6% (4/67) (Table 1). Three patients died after emergency surgery (colostomy: n = 1, left colectomy n = 1, Hartmann procedure n = 1) due to failure or complication of stent insertion (impossible stent placement due to a stricture: n = 2; perforation during stent placement: n = 1); one patient with permeable stent died on day 12 from acute renal failure. Early and late complications related to the placement of colonic stents are summarized Table 2. Late stent occlusion occurred between 5 and 12 months (mean: 6.3 months) after insertion in 7 patients, all of whom were treated by stent reinsertion in 5 cases or surgery in 2 cases (left colectomy n = 1, colostomy n = 1).
The median time required for stent placement was 25 min (range, 12–90 min). With all 57 in whom stent placement was successful, clinical signs and findings of obstruction were resolved within 24 h after SEMS placement. The median hospital stay with stents successfully placed in palliative conditions without a secondary operative procedure was 6 days (range, 4–8 days).
Of the nine patients with stents successfully placed as a bridge to surgery, all underwent elective single-stage operations with no deaths or anastomotic complications. The median length of time between stent placement and subsequent surgery was 10.5 days (range, 3–21 days).
Discussion
Between 7% and 30% of patients with colorectal carcinoma present with acute intestinal obstructions, of which almost 90% are located at or distal to the splenic flexure [5, 22]. The management of these obstructions generally mandates emergency surgical procedure and, at the minimum, decompression. The operative mortality, however for acute malignant large bowel obstruction has been reported to be 23%–45% [2, 15]. If the ileocecal valve is competent, with absence of small bowel dilatation, the patient is considered to be at increased risk for development of a perforation. Furthermore, electrolyte imbalance, bowel ischemia, and sepsis caused by bacterial translocation are particular concerns in this situation [10]. Additionally, these patients are often malnourished, older, dehydrated, and may have widely disseminated disease at the time of presentation [4, 10, 32]. In such patients, in addition to the risk factors already mentioned, the lack of bowel preparation and the severe dilatation of proximal bowel segments often lead the surgeon to perform multiple procedures, with operative mortality rates as high as 60% [2, 10, 15, 17].
To avoid the consequence of multiple or two-stage procedures, some authors [21] have used intraoperative colonic lavage, with some success, but this operative procedure is tedious and complex, requires a longer operative time, and is associated with increased morbidity [9]. A total or subtotal colectomy has been proposed by some authors [1], but in the case of rectal obstruction, this operation may be associated with unacceptable, intractable diarrhea. For a more proximal obstruction, subtotal colectomy with ileocolonic anastomosis is generally a good choice with a low morbidity and mortality rate [31]. Emergency colostomy or ileostomy, with or without resection, is still the standard for treatment of high-risk patients with complete malignant large bowel obstruction [13]. This surgical procedure, however, also is associated with a high mortality rate [2, 5, 10]. Furthermore, the stoma itself may be a major source of morbidity, and 30% of patients with colostomies will never have restoration of digestive continuity [5].
Endoluminal decompression can be obtained by means of laser, cryosurgical destruction, or argon-plasma coagulation [8, 11, 28]. These treatments have been shown to be effective for palliation through destruction of the tumor and creation of a temporary open lumen. However, patients usually must return for repeated treatment (every 5 or 9 weeks) to avoid recurrent obstruction [26].
In the late 1990s the placement of SEMS became the dominant endoscopic procedure for relieving colonic obstruction. A number of reports have recommended the placement of a metallic stent for malignant large bowel obstruction, either for palliation or for decompression before elective surgery. In the systematic review performed by Khot and co-workers [14], the results of stenting of 598 patients were reported. Technical success was achieved in 551 (92%) and clinical success in 525 (88%). Palliation was achieved in 302 (90%) of 336 cases, while 223 (85%) of 262 insertions succeeded as a bridge to surgery (95% had one-stage surgical procedure). There were three deaths (1%), and stent perforation occurred in 4%, migration in 10%, and reobstruction in 10%. Their reported mortality and morbidity does not include the results from the subsequent surgery performed in 262 patients in whom the stent was placed as a bridge to surgery. In 2002, Dauphinée et al. [4] in a summary of literature reviews of stent in the management of malignant colonic obstruction including 187 patients reported similar results. Most series confirmed that stent insertion provided an effective outcome in patients with malignant colonic obstruction as a palliative and preoperative therapy [6, 16, 18–20, 24, 27, 33].
In summary, these results suggest that colorectal stents offer good palliation and are safe and effective as a bridge to surgery. Stent usage can avoid the need for a stoma, and it is associated with low rates of mortality and morbidity.
References
Aranud JP, Bergamaschi R (1994) Emergency subtotal/total colectomy with anastomosis for acutely obstructed carcinoma of the left colon. Dis Colon Rectum 37: 685–688
Buechter KJ, Boustany C, Caillouette R (1988) Surgical management of the acutely obstructed colon. Am J Surg 156: 163–168
Cwikiel W, Stridbeck H, Tranberg KG, von Holstein CS, Hambraeus G, Lillo-Gil R, Willen R (1993) Malignant esophageal strictures: treatment with a self-expanding nitinol stent. Radiology 187:661–665
Dauphinée CE, Tan P, Beart RW, Vukasin P, Cohen H, Corman ML (2002) Placement of self-expanding metal stents for acute malignant large-bowel obstruction: a collective review. Ann Surg Oncol 9: 574–579
Deans GT, Krukowski ZH, Irvin ST (1994) Malignant obstructions of the left colon. Br J Surg 81:1270–1276
de Gregorio MA, Mainar A, Tejero E, Alfonso E, Gimeno MJ, Herrera M (2002) Use of introducer sheath for colonic stent placement. Eur Radiol 12: 2250–2252
Dohmoto M (1991) New method—endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endosc Dig 3:1507–1512
Eckhauser ML, Mansour EG (1992) Endoscopic laser therapy for obstructing and for bleeding colorectal carcinoma. Am J Surg 58:358–363
Egozi L, Sorrento JJ, Golub R, Schultz EH (1993) Complication of the intracolonic by pass. Dis Colon Rectum 36:191–193
Gandrup P, Lund L, Balslev I (1992) Management of acute malignant large bowel obstruction. Eur J Surg 158:427–430
Gund KE, Storek D, Farin G (1994) Endoscopic argon plasma coagulation (APC) first clinical experiences in flexible endoscopy. Endosc Surg Allied Technol 2:42–6
Irving JD, Adam A, Dick R, Dondelinger RF, Lunderquist A, Roche A (1989) Gianturco expandable metallic biliary stents: results of a European clinical trial. Radiology 172:231–326
Keighley MRB, Williams NS (1999) Surgery of the Anus, Rectum and Colon. 2nd edn. London, W.B. Sanders Company 2185–2188
Khot UP, Wenk Lang A, Murali K, Parker M (2002) Systemic review of the efficacy and safety of colorectal stents. Br J Surg 89:1096–1102
Lee YM, Law WL, Chu KW, Poon RT (2001) Emergency surgery for obstructing colorectal cancers: a comparison between right-sided and left-sided lesions. J Am Coll Surg 192:719–725
Maetani I, Tada T, Ukita T, Inoue H, Yoshida M, Saida Y, Sakai Y (2004): Self-expandable metallic stent placement as palliative treatment of obstructed colorectal carcinoma. J Gastroenterol 39:334–338
Mainar A, Tejero E, Maynar M, Ferral H, Castaneda-Zuniga W (1996) Colorectal obstruction: treatment with metallic stents. Radiology 198:761–764
Martinez-Santos C, Lobato RF, Fradejas JM, Pinto I, Ortega-Deballon P, Moreno-Azcoita M (2002) Self-expandable stent before elective surgery versus emergency surgery for the treatment of malignant colorectal obstruction: comparison of primary anastomosis and morbidity rates. Dis Colon Rectum 45:401–406
Meisner S, Hensler M, Krag-Knop F, West F, Wille-Jorgensen P (2004) Self-expanding metal stents for colonic obstruction: experiences from 104 procedures in a single center. Dis Colon Rectum 47:444–450
Morino M, Berello A, Garbarini A, Rozzio G, Repici A (2002) Malignant colonic obstruction managed by endoscopic stent decompression followed by laparoscopic resection. Surg Endosc 16:1483–1487
Murray JJ, Schoetz DJ, Coller JA, Roberts PL, Veidenheimer MC (1991) Intraoperative colonic lavage and primary anastomosis in nonelective colon resection. Dis Colon Rectum 34:527–531
Ohman U (1982) Prognosis in patients with obstructing colorectal carcinoma. Am J Surg 143:742–747
Parodi JC, Palmaz JC, Barone HD (1991) Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg 5:491–499
Ptok H, Meyer F, Marusch F, Steinert R, Gastinger L, Lippert H, Meyer L (2006) Palliative stent implantation in the treatment of malignant colorectal obstruction. Surg Endosc 20:909–914
Roubin GS, Cannon AD, Agrawal SK, Macander PJ, Dean LS, Baxley WA, Breland J (1992) Intracoronary stenting for acute and threatened closure complicating percutaneous transluminal coronary angioplasty. Circulation 85:916–927
Sardi A, Ojeda H, Barco E (1999) Cryosurgery: adjuvant treatment at the time of resection of a pelvic recurrence in rectal cancer. Am Surg 65:1088–1091
Suzuki N, Saunders BP, Thomas-Gibson S, Akle C, Marshall M, Halligan S (2004) Colorectal stenting for malignant and benign disease: outcomes in colorectal stenting. Dis Colon Rectum 47:1201–1207
Tan CC, Iftikhar SY, Allan A, Freeman JG (1995) Local effects of colorectal cancer are well palliated by endoscopic laser therapy. Eur J Surg Oncol 21:648–652
Tejero E, Fernandez L, Tobio R, Mainar A (1997) Initial results of a new procedure for treatment of malignant obstruction of the left colon. Dis Colon Rectum 40:432–436
Tejero E, Mainar A, Fernandez L, Tobio R, Degregorio MA (1994) New procedure for the treatment of colorectal neoplastic obstructions. Dis Colon Rectum 37:1158–1159
The Scotia Study Group (1995) Single-stage treatment for malignant left-sided colonic obstruction: a prospective randomized clinical trial comparing subtotal colectomy with segmental resection following intraoperative irrigation. Br J Surg 82:1622–1627
Wholey MH, Levine EA, Ferral H, Castaneda-Zuniga W (1998) Initial clinical experience with colonic stent placement. Am J Surg 175:194–197
Xinopoulos D, Dimitroulopoulos D, Theodosopoulos T, Tsamakidis K, Bitsakou G, Plataniotis G, Gontikakis M, Kontis M, Paraskevas I, Vassilobpoulos P, Paraskevas G (2004) Stenting or stoma creation for patients with inoperable malignant colonic obstruction? Surg Endosc 18:421–426
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mucci-Hennekinne, S., Kervegant, A.G., Regenet, N. et al. Management of acute malignant large-bowel obstruction with self-expanding metal stent. Surg Endosc 21, 1101–1103 (2007). https://doi.org/10.1007/s00464-007-9258-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9258-0