Abstract
Background
Dyslipidemia is known to increase significantly the odds of major cardiovascular events in the general population. Its control becomes even more important in the type 2 diabetic (T2DM) population. Bariatric surgeries, especially gastric bypass, are effective in achieving long-term control of dyslipidemia in morbidly obese patients.
Objective
The objective of the study was to evaluate the control of dyslipidemia in patients with T2DM and BMI below 30 that were submitted to the laparoscopic ileal interposition associated to sleeve gastrectomy.
Methods
An observational transversal study was performed in a tertiary care hospital, between June 2005 and August 2007. Mean follow-up was 24.5 months (range 12–38). The procedure was performed in 72 patients: 51 were men and 21 were women. Mean age was 53.1 years (38–66). Mean BMI was 27 kg/m2 (22.1–29.4). Mean duration of T2DM was 10.5 years (3–22). Mean HbA1c was 8.5%. Hypercholesterolemia was diagnosed in 68% of the patients and hypertriglyceridemia in 63.9%.
Results
Mean postoperative BMI was 21.2.kg/m2 (17–26.7). Mean postoperative HbA1c was 6.1%, ranging 4.4% to 8.3%. Overall, 86.1% of the patients achieved an adequate glycemic control (HbA1c < 7) without anti-diabetic medication. HbA1c below 6 was achieved by 50%, 36.1% had HbA1c between 6 and 7, and 13.9% had HbA1c above 7. Total hypercholesterolemia was normalized in 91.8% and hypertriglyceridemia in 89.1% of patients. Low-density lipoprotein below 100 mg/dl was seen in 85.7%.
Conclusions
The laparoscopic ileal interposition associated to sleeve gastrectomy was an effective operation for the regression of dyslipidemia and T2DM in a non-obese population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with type 2 diabetes mellitus (T2DM) have an increased prevalence of lipid abnormalities, which contributes to higher rates of cardiovascular disease (CVD). Most of the complications and hospitalizations in diabetic patients are related to atherosclerosis, which is responsible for about 80% of all diabetic mortality. It is believed that as many as 50% of patients with newly diagnosed T2DM already have cardiovascular disease.1
Persons with low HDL cholesterol levels (less than 40 mg/dl [1.03 mmol/l] in men and less than 50 mg/dl [1.30 mmol/l] in women) are at increased risk of coronary heart disease,2 and death from cardiovascular causes, especially if such persons have diabetes.3 Epidemiologic studies and studies in animals suggest that raising the levels of HDL cholesterol may retard the development of atherosclerosis. In humans, each increase in baseline HDL cholesterol of 1 mg/dl (0.03 mmol/l) is associated with a 6% decrease in the risk of death from coronary disease or myocardial infarction.4
Intervention trials using statins to lower low-density lipoprotein (LDL) cholesterol have consistently shown substantial reductions in major cardiovascular events in the treated groups.5 Furthermore, the magnitude of the reduction in events is a function of the extent of LDL cholesterol lowering, with each decrease of 40 mg/dl (1.0 mmol/l) in LDL cholesterol corresponding to a 24% reduction in major cardiovascular events.6
Hypertriglyceridemia is a common form of dyslipidemia that is frequently associated with premature coronary artery disease.7 Whether hypertriglyceridemia causes coronary artery disease or is a marker for other lipoprotein abnormalities that cause premature coronary artery disease remains controversial.8
Bariatric surgery, especially gastric bypass9 and malabsorptive surgeries,10 are effective in achieving long-term control of obesity, T2DM, and dyslipidemia in morbidly obese patients. For non-morbidly obese patients, with BMI 23.6 to 34.4, the metabolic syndrome (MS) could no longer be characterized in 95% of the patients following the laparoscopic ileal interposition associated to a sleeve gastrectomy. The impact of this operation on the individual components factors of the MS was variable.11
The objective of this study is to evaluate the control of dyslipidemia in patients with T2DM and BMI below 30 that were submitted to the laparoscopic ileal interposition associated to a sleeve gastrectomy (LII-SG).
Materials and Methods
Seventy-two patients with dyslipidemia and T2DM were consecutively submitted to the laparoscopic ileal interposition associated to a sleeve gastrectomy (II-SV) between June 2005 and August 2007. There were 51 (70.8%) men and 21 (29.2%) women. Mean age was 53.1 ± 6.4 years (range 38–66 years). Preoperative BMI ranged from 22.1 to 29.4, with a mean of 27 ± 2.5 kg/m2. Mean duration of T2DM was 10.5 ± 4.7 years, ranged 3–22. Preoperatively, oral hypoglycemic agents were used by 52.8% of the patients (mean number of 2.4) and insulin by 47.2%. The demographics are better illustrated in Table 1.
The diagnosis of T2DM was established according to the American Diabetes Association.12 Inclusion criteria included documentation of hemoglobin A1c (HbA1c) above 7.5% for at least 3 months, stable weight, defined as no significant change, more than 3%, over the 3 months prior to enrollment, and evidence of stable treatment with oral hypoglycemic therapy and or insulin for at least 12 months.
The exclusion criteria included C-peptide levels below 0.5 nmol/l, elderly (>66 years), previous major upper abdominal surgery, pregnancy, malignant or debilitating diseases, severe pulmonary or cardiac diseases, severe renal disease (glomerular filtration rate below 30 ml/min), taking appetite suppressant medication, eating disorder such as bulimia or binge eating, and obesity due to any other endocrine disorder. There were no special criteria for the indication of the two different configurations of the procedures, although we assumed that the diverted version would be more effective in controlling T2DM.
An altered lipid profile was observed in 75% of patients. Hypercholesterolemia was diagnosed in 68% of the patients and hypertriglyceridemia in 63.9%. LDL was abnormal in 68% of the patients and HDL in 34.7%. According to the Third Report of the National Cholesterol Education Program’s Adult Treatment Panel (NECP/ATP III) guidelines, suggested target lipid levels would be LDL cholesterol below 100 mg/dl, triglycerides below 150 mg/dl, and HDL cholesterol above 40 mg/dl.13 Specific preoperative tests included nonesterified fatty acids, test for microalbuminuria, serum creatinine, and estimation of glomerular filtration rate. Other tests included Doppler study of the carotid arteries, retinopathy screening, and detailed cardiac evaluation. Biochemical markers of T2DM were obtained and included fasting plasma glucose, postprandial plasma glucose, glycosylated hemoglobin (HbA1c), fasting plasma insulin, the homeostasis model assessment of insulin resistance (Homa-R), and C-peptide. Plasma glucose concentrations were measured by a glucose oxidase method using a glucose analyzer (Yellow Springs Instrument Model YSI 2300 STAT plus analyzer; YSI, Inc.,Yellow Springs, OH, USA). Plasma insulin and C-peptide concentrations were measured by auto-DELPHIA automatic fluoroimmunoassay (Wallac, Inc., Turku, Finland).
Preoperative preparation for surgery included clear liquids for 48 h prior to the operation in association with regular insulin according to capillary glucose. Preoperative bowel cleansing, perioperative antibiotics, and low molecular weight heparin were administered.
The technique consisted in the interposition of a segment of ileum up to the jejunum or up to the duodenum associated to a sleeve gastrectomy. The sleeve gastrectomy was performed after devascularization of the greater curvature. The gastric resection started 2 to 3 cm above the incisura angularis up to the angle of Hiss. For the ileal interposition, the ligament of Treitz was identified, and the jejunum was divided 20 to 30 cm distally. Then, the cecum was identified, and the distal ileum transected 30 cm proximal to the ileocecal valve. A 150 to 170 cm of ileum was measured proximally and transected. This segment of ileum was interposed in an isoperistaltic way into the proximal jejunum, previously divided. Next, we performed three side-to-side enteroanastomosis. The first one was the ileo-ileostomy, then the jejuno-ileostomy, and finally, the ileo-jejunostomy. All three mesenteric defects were closed with interrupted sutures. To interpose the segment of ileum into the duodenum, the devascularization along the greater curvature of the stomach continued to the duodenum, 3–4 cm beyond the pylorus. The sleeve gastrectomy was performed as mentioned above. The duodenum was transected. An ileal segment of 170 cm was created 30 cm proximal to the ileocecal valve as described above. Next, we performed three anastomosis. The first was an ileo-ileostomy. Then, the segment of ileum was interposed in an isoperistaltic way into the proximal duodenum, previously divided, and the second anastomosis was done between the first portion of the duodenum and the proximal part of the interposed ileum. A point in the jejunum 50 cm from the ligament of Treitz was measured and anastomosed to the distal part of the interposed ileum. The three mesenteric defects were closed (Fig. 1). A detailed description was published elsewhere.14
Postoperatively, all patients were monitored three times daily through capillary plasma glucose and were under insulin therapy according to a sliding scale for 1 month. An appropriate and restricted diet was suggested. Following that, all anti-diabetic medications were to be discontinued until 18 months after the operation. Outcome measures were collected prospectively. The main parameters included evaluation of the total cholesterol, HDL, LDL, triglycerides, NEFFA, fasting and postprandial glucose, HbA1c, diabetes medications usage (agents, doses, and frequency), weight loss (expressed in BMI and percentage of weight loss), resolution or improvement of associated diseases and complications, reoperation rate, and morbidity–mortality of the procedure. Patient and laboratory evaluation were scheduled for every 3 months during the first year after surgery and yearly until 60 months of the operation.
The Hospital’s Institutional Review Board approved the study, and all patients gave written informed consent.
Statistical Analysis
Statistical analysis was done using exact Fisher’s test and Student t test according to the data. A significance level of 0.05 (α = 5%) was adopted, and levels below this were considered significant.
Results
All 72 patients underwent laparoscopic ileal interposition associated to sleeve gastrectomy. Intraoperative complications (8.3%) included resection of an isquemic segment of 5 cm of the transposed ileum (one), hypertensive crisis (one), increased intraoperative bleeding due to intraoperative usage of aspirinR (two), and cardiac arrhythmia (two). Associated procedures included eight (11.1%) cholecystectomies with cholangiography, three (4.2%) hiatal hernia repair, three (4.2%) extensive lysis of adhesions, and seven (9.7%) hepatic biopsies. Mean operative time was 155 min (range 120–220 min) for the II-SG and 175 min for the II-DSG (range 160–260 min). Overall, the mean operative time was 175 min. There was no conversion to open surgery. The median hospital stay was 4.8 days (range 2–51 days).
There was no mortality. Major postoperative complications occurred in 10 patients (13.9%) and included gastrointestinal bleeding that required blood transfusion (one), massive subcutaneous hematoma (two), gastric fistula (one), intraabdominal abscess (one), prolonged ileus (three), acute renal failure (one), and severe cardiac arrhythmia (one). Two patients (2.8%) needed to be reoperated, one with gastric fistula on the 12th postoperative day and one intraabdominal abscess. Prolonged hospitalization was required for six patients (8.3%).
Following discharge from the hospital, during the first postoperative month, postprandial discomfort, early satiety, nausea, anorexia, heartburn, and discomfort in the lower abdomen were the most frequent complains. Two patients (2.8%) were readmitted into the hospital due to persistent vomiting. Both had uneventful resolution with appropriate therapy. There was a progressive improvement of these early symptoms late in the follow-up, with heartburn, anorexia, and food intolerance being the most important symptoms. Persistent diarrhea was observed in two patients (2.8%). There were six (8.3%) late hospitalizations: two due to acute cholecystitis that were submitted to a laparoscopic cholecystectomy, one acute appendicitis submitted to a laparoscopic appendectomy, one pneumonia, and two urinary tract infections.
All 72 patients were followed up a mean of 24.5 months (range 12–38).
The operation adequately treated dyslipidemia. Postoperatively, all patients achieved better parameters than preoperative levels, without medications. Overall, dyslipidemia could no longer be characterized in 90.7% of the patients. Evaluation at different moments, range 1 to 36 months, demonstrated a total cholesterol decrease from a mean of 204.4 ± 57 to 157.4 ± 22.8 mg/dl (p < 0.001). These results were achieved as early as the first evaluation at 1 month following the operation. Up to 36 months, the results were nearly the same (Fig. 2). Hypercholesterolemia was diagnosed in 68% of the patients. Postoperatively, normal levels were observed in 91.8% of these patients. LDL decreased from a mean of 116 ± 54.7 to 84.4 ± 27.4 mg/dl (p = 0.014) and had the same pattern of decrease as the total cholesterol (Fig. 3). Preoperative abnormal levels were seen in 68% of patients, while 85.7% had LDL below 100 mg/dl in the postoperative period. Triglycerides decreased from a mean of 241.5 ± 208.4 mg/dl in the preoperative period to 109.8 ± 46.1 mg/dl postoperatively (p = 0.014) (Fig. 4). Hypertriglyceridemia was diagnosed in 63.9% of the patients before surgery. It was normalized in 89.1% of the patients following the operations, while 4.3% still had triglycerides above 200 mg/dl. HDL increased from a mean of 45.5 ± 5.6 to 47.5 ± 5.2 mg/dl (p = 0.526) (Fig. 5). HDL was altered in 34.7% of the patients and normalized in 68%. Five (6.9%) patients still had low levels of HDL and HbA1c above 6%. Nonesterified free fatty acids decreased from a mean of 0.68 mmol/l (0.4–1.41) to a mean of 0.54 mmol/l, p = 0.542.
Mean HbA1c decreased from 8.5 ± 1.8% to \( 6.1\pm 0.9\% \left( {p < 0.001} \right) \), range 4.4% to 8.2%. Overall, HbA1c < 7% was achieved by 86.1% of the patients without anti-diabetic medication. Normalization, HbA1c < 6%, was reached by 50% of the patients. Glycemic control, HbA1c between 6% and 7%, was achieved by 36.1% of patients and improvement by 13.9% of the patients (Table 2). Nearly 86% of patients permanently discontinued preoperative oral hypoglycemic agents and/or insulin. The other 14% of patients were under oral agents. There was no patient requiring regular insulin therapy. Only 18 patients (25%) had HbA1c above 6.5%. For these patients, the use of metformin or sulfonylurea was implemented. Adjustment of these medications, as monotherapy, on an individual basis, determined a better HbA1c control with all patients achieving levels below 6.5%.
Fasting plasma glucose decreased from 195.8 ± 70.1 to \( {1}0{5}.{1}\pm {23}.{1}\,{\hbox{mg}}/{\hbox{dl}}\left( {p < 0.00{1}} \right) \), and postprandial plasma glucose from 282.1 ± 99.6 to 142.4 ± 48.4 mg/dl (p < 0.001) (Fig. 6). Fasting plasma insulin decreased from 17.6 ± 19.5 to \( {3}.{9}\pm {3}.{7}\,{\hbox{mU}}/{\hbox{ml}}\left( {p < 0.00{1}} \right) \). The homeostasis model assessment of insulin resistance decreased from preoperative levels of 6.4 ± 8.2 to \( {1}.{2}\pm {1}.{1}\left( {p < 0.00{1}} \right) \). C-peptide decreased from 3.2 ± 1.8 to \( {1}.{7}\pm 0.{8}\,{\hbox{ng}}/{\hbox{ml}}\left( {p < 0.00{1}} \right) \).
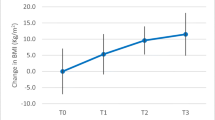
Mean BMI decreased from 27 ± 2.5 kg/m2 in the preoperative to \( {21}.{3}\pm {2}.{3}\,{\hbox{kg}}/{{\hbox{m}}^2}\left( {p < 0.00{1}} \right) \) ranging from 17.8 to 26.2 kg/m2 (Fig. 7). Mean percentage of weight loss was 22 ± 3.6% of the initial weight. (p < 0.001).
Preoperatively, hypertension was present in 55.5% of the patients by means of a casual blood pressure measurement. All patients were using anti-hypertensive medications, mean of 2.1. The blood pressure normalized (≤130/≤85 mmHg), without medication, in 92.5% of the patients (casual blood pressure measurement).
Preoperative nephropathy was diagnosed in 37.5% of the patients. Microalbuminuria was observed in 29.2% of the patients and macroalbuminuria in 8.3%, while 4.2% had glomerular filtration rate between 60 and 89 ml/min. Postoperatively, there was a substantial improvement in the renal function. Mean microalbuminuria decreased from 57.4 ± 138.3 to 27.6 ± 82.2 µg/min (p = 0.026). Microalbuminuria was still present in eight patients (11.1%) and macroalbuminuria in 4.2%. All patients with GFR between 60 and 89 normalized their filtration rate (>90 ml/min).
Coronary heart disease was identified in 20.8% of patients. Postoperatively, a major adverse cardiovascular event (fatal and nonfatal myocardial infarction, coronary insufficiency, heart failure, cardiovascular death, and stroke) was not characterized up to now. Carotid artery evaluation was abnormal in 43.1% of the patients, ranging from intimal–medial thickness to partial stenosis, up to 40% of the arterial lumen. Postoperative routine evaluation at 24 months demonstrated minor improvement.
Discussion
We found in this diverse cohort of type 2 diabetic patients with BMI below 30 that laparoscopic ileal interposition associated to a sleeve gastrectomy was an effective tool for the treatment of dyslipidemia. Overall, dyslipidemia could no longer be characterized in 90.7% of the patients. The impact of this operation on the individual components of dyslipidemia was variable.
Hypertriglyceridemia was normalized in 89.1% of the patients. We hypothesize that diverting the duodenum may alter the GIP resistant state of these T2DM patients. Zhou et al.15 demonstrated that GIP plays a crucial role in switching from fat oxidation to fat accumulation under the diminished insulin action, and inhibition of GIP signaling ameliorated insulin resistance. Central obesity paired with insulin resistance is probably a major factor contributing to hypertriglyceridemia.16 Decrease in insulin resistance and central obesity was observed in almost all of these patients. A first step in evaluating patients with hypertriglyceridemia is to obtain an extensive family history. Hypertriglyceridemia is frequently associated with premature coronary artery disease. A family history of premature coronary artery disease would suggest familial combined hyperlipidemia or familial hypoalphalipoproteinemia.17 This was suspected in 13% of these patients. All but one achieved an adequate control of triglycerides.
In the Framingham Heart Study, HDL cholesterol level was more potent as a risk factor for coronary heart disease than was the level of LDL cholesterol.18 A non-significant rise of HDL was observed following both operations. The Expert Group on HDL recommends considering the addition of a fibrate or niacin for persons whose HDL cholesterol level is less than 40 mg/dl and who have diabetes.19 In the postoperative period, five (6.9%) patients still had low levels of HDL and HbA1c above 6%, so lifestyle modifications, followed by the consideration of pharmacotherapy in these high-risk patients, were suggested.
In individuals without overt cardiovascular disease, the primary goal in treating dyslipidemia is LDL cholesterol below 100 mg/dl. Following these operations, 85.7% of patients with preoperative abnormal levels had LDL below 100 mg/dl, while 34.7% had LDL below 70 mg/dl. A reduction in LDL cholesterol to a goal of <70 mg/dl is an option in very high-risk diabetic patients with overt CVD.20 Hypercholesterolemia resolution was achieved in nearly 92% of patients. In a study in rats, Tsuchiya et al.21 demonstrated that ileal transposition to the upper jejunum affected lipid and bile salt absorption, attenuating cholesterol absorption and transport, possibly by promoting premature absorption of bile salts.
Cardiovascular disease is the major cause of morbidity and mortality for individuals with T2DM and the largest contributor to the direct and indirect costs of diabetes. Dyslipidemia and hypertension are coexisting conditions with T2DM, and benefits are seen when multiple risk factors are addressed globally.22 Postoperatively, we found that 66.7% of patients had normal lipid profile, adequate blood pressure levels, and normal HbA1c, fasting and postprandial glucose. Individually, HbA1c below 7% was achieved by 86.1% of patients and control of hypertension in 92.5%. Lipid management aimed at lowering LDL cholesterol, raising HDL cholesterol, and lowering triglycerides has been shown to reduce macrovascular disease and mortality in patients with T2DM, particularly in those who have had prior cardiovascular events.23 This was the case in 20.8% of the patients of this study. There was an early, as soon as 1 month, adequate, and stable control of postprandial glucose throughout the follow-up. A relation between mortality and plasma glucose at 2 h is observed and is independent of fasting glucose.24 The postprandial plasma glucose and not fasting plasma glucose is associated with cardiovascular disease.25
It has been already demonstrated in previous published studies that this operation made an almost universal improvement in cholesterol and triglycerides levels,26 and also that incretins hormones are impacted by these operations and that GLP-1 exhibited a statistically significant increase in response to meal stimulation. The observed preoperative GLP-1 blunted response was markedly changed, suggesting that levels of meal-stimulated GLP-1 may be restored toward normal with consequent possible improvement control of diabetes, especially postprandial glucose.27 Kumar et al.28 reported their preliminary results confirming the feasibility, safety, and efficacy of this surgical procedure in type 2 diabetic patients. Although we do not want to draw any definitive conclusion, the objective finding of no major cardiac events during this follow-up period may be the result of the global beneficial of the laparoscopic ileal interposition in different cardiovascular risks, including regression of dyslipidemia.
References
National Diabetes Data Group. Diabetes in America 2nd edition. Bethesda: NIH; 1995.
Miller NE, Thelle DS, Forde OH, Mjos OD. (1977) The Tromso heart-study: high-density lipoprotein and coronary heart-disease: a prospective case-control study. Lancet 1:965–8.
Goldbourt U, Yaari S, Medalie JH. (1997) Isolated low HDL cholesterol as a risk factor for coronary heart disease mortality: a 21-year follow-up of 8000 men. Arterioscler Thromb Vasc Biol 17:107–13
Gordon DJ, Knoke J, Probstfield JL, Superko R, Tyroler HA. (1986) High-density lipoprotein cholesterol and coronary heart disease in hypercholesterolemic men: the Lipid Research Clinics Coronary Primary Prevention Trial. Circulation 74:1217–25
Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J; ASCOT investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet 2003; 361:1149–58.
Baigent C, Keech A, Kearney PM (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366: 1267-78. [Erratum, Lancet 2005; 366:1358
Hopkins PN, Heiss G, Ellison RC (2003) Coronary artery disease risk in familial combined hyperlipidemia and familial hypertriglyceridemia: a case-control comparison from the National Heart, Lung, and Blood Institute Family Heart Study.Circulation 108:519–23
Hokanson JE, Austin MA. (1996) Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. J Cardiovasc Risk 3:213–9.
Hickey MS, Pories WJ, MacDonald KG Jr, Cory KA, Dohm GL, Swanson MS,Israel RG, Barakat HA, Considine RV, Caro JF, Houmard JA (1998) A new paradigm for Type 2 Diabetes Mellitus? Could it be a disease of the foregut? Ann Surg. 227:637–644
Greenway SE, Greenway FL, Klein S (2002) Effects of obesity surgery on noninsulin-dependent diabetes mellitus. Arch Surg 137:1109–1117
DePaula, AL, Macedo AL, Rassi N, Vencio S, Machado CA, Mota BR, Silva LQ, Halpern A, Schraibman V (2008) Laparoscopic treatment of metabolic syndrome in patients with type 2 diabetes mellitus. Surg Endosc 22:2670–2678
Executive Summary: Standards of Medical Care in Diabetes (2009) Diabetes Care 32:S6–S12.
Alexander CM, Landsman PB, Teutsch SM, Haffner SM; Third National Health and Nutrition Examination Survey (NHANES III); National Cholesterol Education Program (NCEP) (2003) NCEP-Defined Metabolic Syndrome, Diabetes, and Prevalence of Coronary Heart Disease Among NHANES III Participants Age 50 Years and Older
DePaula AL, Macedo ALV, Rassi N, Machado CA, Schraibman V, Silva LQ, Halpern H (2008) Laparoscopic treatment of type 2 diabetes mellitus for patients with a body mass index less than 35. Surg Endosc 22:706–16.
Zhou H, Yamada Y, Tsukiyama K, Miyawaki K, Hosokawa M, Nagashima K, Toyoda K, Naitoh R, Mizunoya W, Fushiki T, Kadowaki T, Seino Y (2005) Gastric inhibitory polypeptide modulates adiposity and fat oxidation under diminished insulin action. Biochemical and Biophysical Research Communication 335:937–942
Després JP, Lemieux I. (2006) Abdominal obesity and metabolic syndrome. Nature 444:881–7.
Brunzell JD, Schrott HG, Motulsky AG, Bierman EL. (1976) Myocardial infarction in the familial forms of hypertriglyceridemia.Metabolism 25:313–20.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. (1977) High density lipoprotein as a protective factor against coronary heart disease: the Framingham Study. Am J Med 62:707–14
Gotto AM Jr, Brinton EA. (2004) Assessing low levels of high-density lipoprotein cholesterol as a risk factor in coronary heart disease: a working group report and update. J Am Coll Cardiol 43:717–24.
Nissen SE, Tuzcu EM, Schoenhagen P, Brown BG, Ganz P, Vogel RA, Crowe T, Howard G, Cooper CJ, Brodie B, Grines CL, DeMaria AN (2004) Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA 291:1071–1080
Tsuchiya T, Kalogeris TJ, Tso P (1996) Ileal transposition into the upper jejunum affects lipid and bile salt absorption in rats. Am J Physiol 271:G681–G691.
Gaede P, Lund-Andersen H, Parving HH, Pedersen O (2008) Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 358:580–591.
Lindholm LD, Ibsen H, Dahlof B, Devereux RB, Beever G, de Faire U, Fyhrquist F, Julius S, Kjeldsen SE, Kristiansson K, Kederballe-Pedersen O, Niemine MS, Omvik P, Oparil S, Wedel H, Aurup P, Edelman J, Snapin S (2002) Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet 359:1004–1010.
DECODE Study Group. Lancet 1999; 354:617–21
E Barrett-Connor andA Ferrara Isolated postchallenge hyperglycemia and the risk of fatal cardiovascular disease in older women and men. The Rancho Bernardo Study. Diabetes Care 1998; 21:1236–1239
DePaula AL, Macedo ALV, Mota BR, Schraibman V. Laparoscopic ileal interposition associated to a diverted sleeve gastrectomy is an effective operation for the treatment of type 2 diabetes mellitus patients with BMI 21-29. Surg Endosc (2009) 23: 1313–1320.
DePaula AL, Macedo ALV, Schraibman V, Mota BR, Vencio S. Hormonal evaluation following laparoscopic treatment of type 2 diabetes mellitus patients with BMI 20–34. Surg Endosc (2009) 23: 1724–1732.
Kumar KV, Ugale S, Gupta N, Naik V, Kumar P, Bhaskar P, Modi KD. Ileal interposition with sleeve gastrectomy for control of type 2 diabetes. Diabetes Technol Ther. 2009;11:785–9.
Disclosure statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DePaula, A.L., Stival, A.R., DePaula, C.C.L. et al. Impact on Dyslipidemia of the Laparoscopic Ileal Interposition Associated to Sleeve Gastrectomy in Type 2 Diabetic Patients. J Gastrointest Surg 14, 1319–1325 (2010). https://doi.org/10.1007/s11605-010-1252-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-010-1252-5