Abstract
Introduction
Appendiceal tumors represent a subset of colonic neoplasms that frequently defy early diagnosis only to present at advanced stage with peritoneal metastasis. Data on early detection by colonoscopy is limited to case reports or series. The aim of this study is to determine the diagnostic yield of colonoscopy in detecting appendiceal lesions in patients with appendiceal adenocarcinoma and pseudomyxoma peritonei.
Methods
We reviewed clinicopathologic data on 121 consecutive patients with histologically confirmed appendiceal adenocarcinoma with pseudomyxoma peritonei presenting to our institution for intraperitoneal hyperthermic chemotherapy (IPHC) and cytoreductive surgery between February, 1993 and August, 2007, focusing on the colonoscopy findings.
Results
Preoperative colonoscopic data were available on 64 patients (average age = 51; 52 for IPHC patients). Abnormal findings included seven patients with appendiceal lesions (11%), 12 patients with cecal abnormalities (19%), and 28 patients with polyps (44%). Twenty-three patients (36%) had a normal colonoscopy. Malignancy was documented in two of the 64 (3.1%) patients on preoperative colonoscopy biopsies.
Conclusions
Appendiceal abnormalities are infrequently seen on colonoscopy and rarely yield a diagnostic biopsy in patients with appendiceal carcinoma. We found that nearly 42% of patients with carcinoma of the appendix have synchronous colonic polyps, a much higher prevalence than would be expected, supporting a role for a perioperative colonoscopy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Appendiceal adenocarcinoma is a rare lesion, which is, unfortunately, seldom diagnosed early. Presenting symptoms can include right lower quadrant pain, appendicitis, early satiety, and changes in bowel habits or abdominal distention. It is not unusual for these lesions to be detected incidentally at surgery or by cross-sectional imaging. In the USA, there are 561,000 appendectomies performed annually with approximately 250,000 cases of appendicitis per year.1 Mucinous distention of the appendix, or mucocele, is present in 0.2–0.3% of appendectomy specimens and may be a premalignant lesion if associated with adenomatous changes. The incidence of appendiceal adenocarcinoma ranges from 0.11–0.80% in appendectomy specimens.2–5 According to the surveillance, epidemiology and end-results program, the incidence of appendiceal malignancies in the USA is 0.12 cases per 1,000,000 people per year, with adenocarcinoma accounting for the largest subset at 37% of total cases.6 Histologic type predicts extent of disease,7 with signet-ring cell carcinoma of the appendix having metastases at time of diagnosis in 93% of cases, mucinous adenocarcinoma having metastases at time of diagnosis in 71% of cases, and colonic type adenocarcinoma having metastases at time of diagnosis in 83% of cases.6
Pseudomyxoma peritonei is a distinct clinical entity characterized by gelatinous ascites originating from a mucinous appendiceal adenoma or adenocarcinoma. Ronnett et al. found that at least 87% of cases of pseudomyxoma peritonei or mucinous adenocarcinoma with peritoneal involvement were of appendiceal origin.8 Additionally, Misdraji et al. found that 64% of cases of appendiceal mucinous neoplasms showed evidence of appendiceal rupture and peritoneal spread.9 We have found that pseudomyxoma is rarely caused by nonappendiceal tumors.
Endoscopic detection of appendiceal adenoma and adenocarcinoma has been reported as case reports and limited case series in the medical literature.10–20 Ponsky first described the detection of appendiceal mucocele by colonoscopy in 1976 as a yellowish, submucosal, lipoma-like mass.21 In the largest series to date, Zanati et al. described seven patients with mucinous cystadenoma of the appendix detected on colonoscopy over a 14-year period at a single institution.16 Lee et al. first described their abnormal colonoscopy findings in a patient with pseudomyxoma peritonei.22 We are unaware of a large series that adequately describes the preoperative colonoscopic findings in patients presenting with appendiceal adenocarcinoma with pseudomyxoma peritonei. Thus, the aim of this study was to determine the diagnostic yield of colonoscopy in detecting previously diagnosed appendiceal adenocarcinoma with pseudomyxoma peritonei and to characterize the mucosal abnormalities associated with appendiceal adenocarcinoma with pseudomyxoma peritonei.
Methods and Materials
We retrospectively reviewed our experience in 191 patients, from 1993 to 2006, with pseudomyxoma peritonei related to primary appendiceal tumors, who were treated with cytoreductive surgery (CS) and intraperitoneal hyperthermic chemotherapy (IPHC); complete records were available in 121 patients and made up our cohort. Sixty-four patients had a complete colonoscopy either prior to surgery. The initial history and physical, colonoscopy reports, surgical pathology reports, and clinic notes were reviewed for record of colonoscopy performed prior to CS. Reference to prior colonoscopy as normal was deemed to have no appendiceal lesion and no colonic polyps. A total of 64 patients were selected for final review. Colonoscopy report findings of appendiceal lesions, cecal lesions, colonic polyps, and any other mucosal or submucosal defect were compiled. This study was approved by our institutional review board.
Results
Colonoscopy Findings
There were a total of 68 colonoscopies performed on 64 patients prior to IPHC/CS. The indications are summarized in Table 1. The leading indications for performing colonoscopy were new diagnosis of appendiceal adenocarcinoma with pseudomyxoma peritonei (26.6%), cancer of unknown primary source (15.6%), abdominal pain (14.1%), and abdominal mass (10.9%). There were two patients with colonoscopy performed for screening purposes only (3.1%). Indication for colonoscopy was not available in three of the 64 (4.7%) patients.
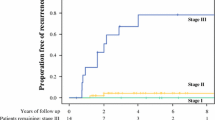
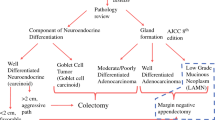
Patients were defined as having normal colonoscopies if a normal endoscopy report was available and/or if the initial history and physical within our medical record reported on a normal colonoscopy. Colonoscopy reports were available on 54 of the 64 patients (84%) and the initial history and physical was used to report “normal” findings in the remaining ten patients (16%). The average age at time of endoscopy was 51 (range 26–74 years), the average age at time of diagnosis was 50 (range 26–74 years), and the average age at time of IPHC C/S treatment was 52 (range 26–74 years). There were 36 males and 28 females. Colonoscopy was performed for an average of 182 days (range 1–1447 days, median 79 days) prior to CS/IPHC. Table 2 summarizes colonoscopic findings. In 23 patients, the colonoscopy was entirely normal (36%). Appendiceal lesions were detected in seven patients (11%). Abnormal findings of the cecum, usually a mass effect, were present in 12 patients (19%). Lesions of the appendix and/or cecum were present in 16 patients (25%). Overall, a malignant diagnosis was made on two of the 64 (3.1%) patients on the preoperative colonoscopic biopsies. Table 3 summarizes the clinicopathological findings of patients with abnormalities at the cecum or appendix. Disseminated adenomucinosis of the appendix is classified as a low grade malignant lesion.7 Colonic polyps were present in 27 patients (42%); only nonhyperplastic polyps were considered significant both within and outside of the cecum. An extrinsic mass in the midascending colon ulcerating through the bowel wall into the lumen was detected concomitantly in one patient (2%). One patient had extensive pancolonic polyps suggestive of familial polyposis (2%).
Surgical Treatments Prior to Colonoscopy
Because many patients presenting for IPHC have prior surgical therapy, we investigated the effect of prior surgery on likelihood of abnormalities being detected with colonoscopy. Prior surgery is defined on a scale of 0–3. Prior surgical score (PSS) of 0 is defined as biopsy only or laparoscopy plus biopsy. PSS of 1 is defined as previous exploratory laparotomy. PSS of 2 is defined as exploratory laparotomy with some resection, usually greater omentectomy or greater omentectomy plus right colectomy. PSS of 3 is defined as extensive surgery with an attempt at complete cytoreduction. PSS was unknown in six patients. There were 16 patients (25%) with PSS of 0, 23 (40%) patients had PSS of 1, 16 (25%) patients had PSS of 2, and three patients had PSS of 3 (5%). The three patients with extensive cytoreduction had normal colonoscopies. Thirty-three of the 64 patients (52%) with colonoscopy prior to IPHC had prior appendectomy.
Forty-four percent of the subset of 16 patients with abnormal findings of the appendiceal orifice and/or cecum had appendectomy prior to colonoscopy. Five of these 16 had PSS of zero, six patients had PSS of 1, and four patients had PSS of 2. PSS was unknown on a single patient.
Discussion
We describe the colonoscopic findings of patients presenting to our institution for treatment of appendiceal adenocarcinoma with pseudomyxoma peritonei with intraperitoneal hyperthermic chemotherapy and cytoreductive surgery. This constitutes the single, largest cohort of patients with appendiceal carcinoma in which preoperative colonoscopic data exist. Our series is limited by the inherent limitations and weaknesses seen in retrospective database studies. Specifically, the time between colonoscopy and surgery (either CS or conventional) varied between a few days and 4 years. Further, the clinical impressions of the endoscopists beyond that included in their report were not queried. In addition, our analysis is limited by a highly selected subset of patients with appendiceal carcinoma associated with pseudomyxoma and not just appendiceal adenocarcinomas and as such is not generalizable. However, it is clear that colonoscopy rarely identifies cancer of the appendix, even when it is in an advanced stage.
Standard colonoscopy continues to be the gold-standard study to evaluate colonic mucosa for abnormalities; however, the predilection of appendiceal adenocarcinoma to spread to the peritoneum limits detection of endoluminal disease with colonoscopy. The general consensus of centers caring for patients with appendiceal adenocarcinoma with pseudomyxoma peritonei is that a colonoscopy is inconsequential in these individuals as they typically have stage IV disease. We found that a colonoscopy alone is poor at definitively diagnosing advanced appendiceal adenocarcinoma with peritoneal spread with only 10% of cases showing an appendiceal abnormality and virtually no masses noted intraluminally. Thus, a normal colonoscopy does not predict the absence of an appendiceal adenocarcinoma.
However, we found a high incidence of synchronous colonic polyps, with no synchronous colon cancer. Wolff and Ahmed reported metachronous colonic neoplasm present in 21.4% in patients with benign lesions of the appendix and a single case (4.8%) of metachronous colonic neoplasm in patients with adenocarcinoma of the appendix.23,24 Colonoscopy is useful in detecting synchronous colonic polyps that may have a higher risk for malignant transformation in this patient population as synchronous colonic neoplasms have been reported in the literature. Nonetheless, the increased incidence of colonic polyps in our cohort (44%) compared to those noted in the age-matched screening population in which adenomas should be detected in ≥25% of men and ≥15% women suggests that these patients are most likely at a higher risk for developing colonic neoplasia.25 Thus, the value of the colonoscopy is not so much in identifying an appendiceal carcinoma, but, moreover, in detecting colonic neoplasia. Although finding polyps in patients with stage IV disease typically has no effect on long-term survival, most patients with peritoneal dissemination from low-grade appendiceal tumors treated with cytoreductive surgery and IPHC have median survival beyond 5 years. Therefore, colonoscopy and polypectomy may be of value in selected patients being evaluated for surgery.
Conclusion
We examined the yield of colonoscopy in detecting appendiceal adenocarcinoma in a cohort of patients with advanced disease and pseudomyxoma peritonei. There was a low detection rate of 11% for appendiceal abnormalities and 19% for cecal abnormalities. Despite a priori knowledge of the patient’s appendiceal carcinoma diagnosis, the endoscopist was able to document malignancy in only 3% of patients on preoperative colonic biopsies. This data represents the largest series of colonoscopic examinations in the literature. We confirm that the likelihood of finding early lesions of the appendix is rare using endoscopic evaluation. Indeed, a negative colonoscopy was commonly present in our cohort with advanced disease, indicating that a negative colonoscopy does not rule out appendiceal primary tumor. There was a higher than expected rate of synchronous colon polyps in our cohort. Colonoscopy should be performed in selected patients diagnosed with appendiceal adenocarcinoma with pseudomyxoma peritonei to evaluate for synchronous premalignant lesions. Endoscopists should be aware that colonoscopy is unlikely to detect advanced appendiceal adenocarcinoma. However, findings of a smooth, submucosal lesion in the cecum near the appendiceal orifice or free-flowing mucin from the appendiceal orifice should raise concern for appendiceal adenocarcinoma.
References
Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990;132:910–925.
Collins DC. 71,000 human appendix specimens. A final report, summarizing forty years’ study. Am J Proctol 1963;14:265–281.
Marudanayagam R, Williams GT, Rees BI. Review of the pathological results of 2660 appendicectomy specimens. J Gastroenterol 2006;41:745–749. doi:10.1007/s00535-006-1855-5.
Blair NP, Bugis SP, Turner LJ, MacLeod MM. Review of the pathologic diagnoses of 2,216 appendectomy specimens. Am J Surg 1993;165:618–620. doi:10.1016/S0002-9610(05)80446-5.
Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum 1998;41:75–80. doi:10.1007/BF02236899.
McCusker ME, Coté TR, Clegg LX, Sobin LH. Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973–1998. Cancer 2002;94:3307–3312. doi:10.1002/cncr.10589.
Bradley RF, Stewart JH, Russell GB, Levine EA, Geisinger KR. Pseudomyxoma peritonei of appendiceal origin: a clinicopathologic analysis of 101 patients uniformly treated at a single institution, with literature review. Am J Surg Pathol 2006;30:551–559. doi:10.1097/01.pas.0000202039.74837.7d.
Ronnett BM, Zahn CM, Kurman RJ, Kass ME, Sugarbaker PH, Shmookler BM. Disseminated peritoneal adenomucinosis and peritoneal mucinous carcinomatosis. A clinicopathologic analysis of 109 cases with emphasis on distinguishing pathologic features, site of origin, prognosis, and relationship to “pseudomyxoma peritonei”. Am J Surg Pathol 1995;19:1390–1408. doi:10.1097/00000478-199512000-00006.
Misdraji J, Yantiss RK, Graeme-Cook FM, Balis UJ, Young RH. Appendiceal mucinous neoplasms: a clinicopathologic analysis of 107 cases. Am J Surg Pathol 2003;27:1089–1103. doi:10.1097/00000478-200308000-00006.
Hamilton DL, Stormont JM. The volcano sign of appendiceal mucocele. Gastrointest Endosc 1989;35:453–456.
Nakagawa T. Colonoscopic diagnosis of mucocele of the appendix. Gastrointest Endosc 1993;39:733–734.
Raijman I, Leong S, Hassaram S, Marcon NE. Appendiceal mucocele: endoscopic appearance. Endoscopy 1994;26:326–328. doi:10.1055/s-2007-1008979.
Mizuma N, Kabemura T, Akahoshi K, Yasuda D, Okabe H, Chijiiwa Y, Nawata H, Matsui N. Endosonographic features of mucocele of the appendix: report of a case. Gastrointest Endosc 1997;46:549–552. doi:10.1016/S0016-5107(97)70013-0.
Minagawa M, Ishikawa H, Date K, Kosugi S, Hatakeyama K, Endo K, Kimura K, Fukuda F. Mucus outflow from the appendiceal orifice due to an appendiceal mucocele. Gastrointest Endosc 2001;53:493. doi:10.1067/mge.2001.113584.
Shami VM, Yerian LM, Waxman I. Adenoma and early stage adenocarcinoma of the appendix: diagnosis by colonoscopy. Gastrointest Endosc 2004;59:731–733. doi:10.1016/S0016-5107(04)00008-2.
Zanati SA, Martin JA, Baker JP, Streutker CJ, Marcon NE. Colonoscopic diagnosis of mucocele of the appendix. Gastrointest Endosc 2005;62:452–456. doi:10.1016/j.gie.2005.04.018.
Qualia CM, Drugas GT, Jones LT, Rossi TM. Colonoscopic diagnosis of an appendiceal mucocele. J Pediatr Gastroenterol Nutr 2007;45:145–146. doi:10.1097/MPG.0b013e3180686da7.
Isaacs KL, Warshauer DM. Mucocele of the appendix: computed tomographic, endoscopic, and pathologic correlation. Am J Gastroenterol 1992;87:787–789.
Hu CC, Chang JJ, Chen TC, Yen CL, Chien RN. Colonoscopic feature of primary adenocarcinoma of the appendix. Intern Med 2008;47:255–257. doi:10.2169/internalmedicine.47.0192.
Itaba S, Akahoshi K, Araki Y, Nakamura K, Chijiiwa Y, Ohata Y, Shimura H, Nawata H. Preoperative colonoscopic diagnosis of minute appendicular adenoma: report of a case. Endoscopy 1998;30:S64. doi:10.1055/s-2007-1001331.
Ponsky JL. Endoscopic view of mucocele of appendix. Gastrointest Endosc 1976;23:42–43.
Lee Y, Wu H, Hung M, Lin S, Hwang Y, Huang M. Ruptured appendiceal cystadenoma presenting as right inguinal hernia in a patient with left colon cancer: a case report and review of literature. BMC Gastroenterol 2006;6:32. doi:10.1186/1471-230X-6-32.
Wolff M, Ahmed N. Epithelial neoplasms of the vermiform appendix (exclusive of carcinoid). I. Adenocarcinoma of the appendix. Cancer 1976;37:2493–2510. doi:10.1002/1097-0142(197605)37:5<2493::AID-CNCR2820370543>3.0.CO;2-D.
Wolff M, Ahmed N. Epithelial neoplasms of the vermiform appendix (exclusive of carcinoid). II. Cystadenomas, papillary adenomas, and adenomatous polyps of the appendix. Cancer 1976;37:2511–2522. doi:10.1002/1097-0142(197605)37:5<2511::AID-CNCR2820370544>3.0.CO;2-L.
Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE, Hoffman B, Jacobson BC, Mergener K, Petersen BT, Safdi MA, Faigel DO, Pike IM. ASGE/ACG taskforce on quality in endoscopy. Quality indicators for colonoscopy. Am J Gastroenterol 2006;101:873–885.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was previously presented in poster form at the Surgical Society of the Alimentary Tract Washington, DC 2007.
Rights and permissions
About this article
Cite this article
Trivedi, A.N., Levine, E.A. & Mishra, G. Adenocarcinoma of the Appendix Is Rarely Detected by Colonoscopy. J Gastrointest Surg 13, 668–675 (2009). https://doi.org/10.1007/s11605-008-0774-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0774-6