Abstract
Background
Mucinous appendiceal neoplasms (MAN) with peritoneal dissemination is treated as a standard of care using cytoreductive surgery and hyperthermic perioperative chemotherapy. The extent of the resection of peritoneal surfaces and visceral structures is generally well defined. Exception to this consensus regarding structures to be removed are the right colon and adjacent ileocolic lymph nodes.
Methods
From a prospectively maintained database, all patients with a histologic diagnosis of peritoneal mucinous carcinoma (PMCA) who underwent complete cytoreductive surgery were assessed for the presence versus absence of adenocarcinoma in lymph nodes within the appendiceal mesentery and/or in the lymph nodes of the ileocolic group. The histologic grade of the PMCA was correlated with the incidence of lymph node invasion. Also, in those PMCA patients who had no evidence of lymph node invasion, recurrence within the ileocolic lymph nodes was determined by computed tomography or second look.
Results
In a database of MAN patients, 299 had a histologic diagnosis of PMCA. In well-differentiated (n = 44), moderately differentiated (n = 107), and poorly differentiated (n = 148) PMCA specimens, there were 6.8, 5.6, and 29 % positive lymph nodes, respectively. None of these 151 patients with well- or moderately differentiated PMCA had a computed tomographic scan or clinical evidence by second-look surgery of recurrence within the ileocolic lymph nodes.
Conclusions
There is a low incidence (6.0 %) of positive lymph nodes in patients with low or moderately differentiated PMCA. With high-grade disease, lymph node invasion increased to 29.0 %. Right colectomy is indicated in patients with high-grade PMCA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Appendiceal neoplasms are rare and often show low-grade histologic features. Symptoms and signs related to peritoneal metastases most commonly results in a diagnosis. Historically, epithelial appendiceal neoplasms have routinely been treated by a right colectomy. In 2004, Gonzalez-Moreno and Sugarbaker reported that in mucinous appendiceal neoplasms (MAN) with peritoneal spread, right colon resection with ileocolic lymph node dissection did not confer a survival advantage over appendectomy alone.1 Other groups have made a similar observation.2,3 These reports have modified the surgical management of MAN, whether disseminated or localized, to recommend appendectomy only as the treatment of choice in patients with a low histologic grade of MAN, referred to as disseminated peritoneal adenomucinosis (DPAM).4 However, confusion still exists for the high-grade mucinous neoplasms, referred to as peritoneal mucinous carcinoma (PMCA). Currently, they are usually, but not always, recommended for right colon resection to remove occult positive appendiceal or ileocolic lymph nodes. To date, precise data to guide the selection of a surgical procedure for MAN with PMCA have not been defined.
Materials and Methods
Clinical Features
From a prospective database of 299 MAN patients with a histologic diagnosis of PMCA accumulated over 26 years, a retrospective review of the clinical data and the pathologic material on all patients was performed. From the appendectomy specimens or from a right colectomy specimen, the presence versus absence of lymph node involvement was determined. Sampling of lymph node tissue at 1 mm intervals for histologic study was routine.
Patients with peritoneal lesions characterized by DPAM were not included in this study. PMCA was characterized by invasive peritoneal lesions composed of abundant epithelium with glandular or signet-ring cell morphology with sufficient architectural complexity and cytologic atypia to warrant a diagnosis of mucinous adenocarcinoma. Mucinous adenocarcinomas were further separated into three grades by evaluating epithelial content of the tumors in order to more completely describe the histologic progression.5 Well-differentiated mucinous adenocarcinoma was composed predominantly of single tubular glands. The tumor cells were well polarized, similar to epithelium of an adenoma. Atypia of the tumor cells was remarkable, and an invasive component was identified. Moderately differentiated mucinous adenocarcinoma showed characteristics between well- and poorly differentiated adenocarcinoma. It was composed of solid sheets of malignant cells admixed with glandular formations. The polarity of the tumor cells was minimal or absent. Poorly differentiated adenocarcinoma was composed of highly irregular glandular structures or lacked glandular differentiation. The polarity of the cancer cells had disappeared completely. In some cases, signet-ring cells were seen.
Hybrid appendiceal mucinous tumors as described by the Ronnett criteria included foci of intermediate type and diffuse peritoneal adenomucinosis histology present within the same clinical material.4 The hybrid tumors predominantly demonstrate histologic features of adenomucinosis; however, focal areas (<5 % of the tumor cells) of well-differentiated adenocarcinoma were identified in peritoneal lesions. The hybrid tumors were grouped with the well-differentiated mucinous adenocarcinoma.
Cytoreduction
All patients underwent a complete cytoreductive surgical procedure that was always performed by the same surgical team. Briefly, the goal of surgery was to remove all visible tumor within the peritoneal cavity. Up to five different peritonectomy procedures were used as necessary in various combinations to remove all visible evidence of tumor.6 These procedures included a greater omentectomy with splenectomy, left upper quadrant peritonectomy, right upper quadrant peritonectomy, lesser omentectomy with cholecystectomy, partial or total resection of the stomach, and pelvic peritonectomy with resection of the rectosigmoid colon.
Perioperative Intraperitoneal Chemotherapy
Intraoperatively, the abdomen and pelvis were lavaged with heated chemotherapy using 1.5 L/m2 of 1.5 % dextrose peritoneal dialysis solution with doxorubicin and mitomycin C. This was followed by 5 days of early postoperative intraperitoneal chemotherapy with 5-fluorouracil.6
Identification of Lymph Node Involvement
Lymph node positivity in the mesoappendix or in ileocolic lymph nodes was determined in one of two ways. In 223 patients, a right colon resection (ileocolectomy) was performed and histopathologic assessment of the lymph nodes within the resected specimen occurred. Another 76 patients operated on more recently had a lymph node assessment by complete removal of the tissues posterior to the cecum and involving the appendiceal artery. The mesoappendix was resected and a single lymph node sent for cryostat section. The remainder of the nodes (2–5 in number) were sent for permanent sections. Also, a single ileocolic lymph node closest to the appendix was resected and sent for permanent histopathologic examination. If any resected lymph nodes were grossly or histopathologically positive, the entire ileocolic lymph node chain was resected along with a limited right colon resection. If no invasion was apparent and the margin of resection on the appendix was clear by cryostat section, right colectomy was not performed.
In all PMCA patients who had negative lymph nodes, a failure analysis was performed in an attempt to identify patients whose disease progressed in the right lower quadrant of the abdomen. This was the area thought to be most likely to show lesions by computed tomographic (CT) scan or reoperative surgery if occult ileocolic lymph nodes progressed as a single site for recurrence or as a site for recurrence within other areas of the abdomen and pelvis positive for progression of PMCA.
Results
From the database for MAN with peritoneal metastases, 299 patients who had undergone complete cytoreduction were identified. The histologic type of this group of patients was PMCA. Resection of the right colon and/or the appendiceal lymph nodes was performed in all patients, and gross and histologic assessments of these lymph nodes were available. In the total group of 299 patients, 52 (17 %) were determined to have at least a single positive lymph node (Table 1).
In these 299 PMCA patients, the three grades of appendiceal mucinous adenocarcinoma were determined.5 There were 44 patients (14.7 %) with well-differentiated PMCA peritoneal metastases, 107 (35.8 %) with moderately differentiated PMCA peritoneal metastases, and 148 (49.5 %) with poorly differentiated PMCA peritoneal metastases.
Within these three grades of mucinous adenocarcinoma, the incidence of positive lymph nodes was determined (Table 1). In the 44 well-differentiated PMCA group, there were three with positive lymph nodes (6.8 %). In the 107 moderately differentiated PMCA group, there were six with positive lymph nodes (5.6 %). In the 148 poorly differentiated PMCA group, there were 43 with positive lymph nodes (29 %).
In this group of 299 PMCA patients, 247 were determined to have no histopathologic evidence of regional lymph node metastases. Progressive disease resulted in the death of 107 (43.3 %) of these patients. CT scans and/or intraoperative evaluation of lymph nodes in the right lower quadrant in and along the ileocolic vessels at second look were available in all patients. Only a single patient was identified who had recurrence in the right lower quadrant. In this patient, a right colectomy was performed. There was extensive disease in and around the ileocecal valve region. None of the 10 ileocolic lymph nodes was positive for cancer.
Discussion
Gonzalez-Moreno and Sugarbaker were the first to question the need for right colon resection in patients being treated for peritoneal metastases from a MAN.1 The use of cytoreductive surgery and perioperative chemotherapy in this group of patients has long-term survival as a goal. Leaving occult mucinous neoplasm behind in appendiceal or ileocolic lymph nodes would be expected to have a detrimental effect on survival. Yet by multivariate analysis, these authors did not find a survival advantage for right colon resection with resection of appendiceal and ileocolic lymph nodes versus appendectomy only as a part of the cytoreductive surgery.1 In the 501 patients in the study by Gonzalez-Moreno et al., the survival of 25 with involvement of lymph nodes was compared to 476 without lymph node invasion.7 In the aggressive treatment strategy used in this group of patients, the presence of lymph node metastases did not reduce survival. The lack of significance of lymph node involvement was noted to be unique among gastrointestinal malignancies where positive versus negative regional lymph nodes is a major determinant of survival.
Histologic types of appendiceal neoplasms have been noted to be associated with variable incidence of regional lymph node invasion. Gonzalez-Moreno and Sugarbaker reported lymph node metastases in intestinal type (nonmucinous) appendiceal neoplasms in 66.7 % of patients. In mucinous type of appendiceal neoplasms, lymph nodes were positive in only 4.2 % (p < 0.001). Foster et al. reported a relationship of histologic subtype with lymph node involvement.2 The incidence of node-positive disease in patients treated with right hemicolectomy based on histologic subtype was 2.7 % (1/37) for DPAM, 0 % (0/19) for PMCA-intermediate type, and 25 % (4/16) for PMCA. PMCA-I is an intermediate grade of appendiceal mucinous neoplasm between DPAM and PMCA.
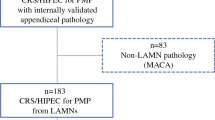
With a long history of grading PMCA emanating from the publication by Yan et al. in 2001, our 299 PMCA appendiceal peritoneal metastases patients have been graded as well differentiated (14.7 %), moderately differentiated (35.8 %), and poorly differentiated (49.5 %).5 This separation of patients by histologic grade allowed a meaningful estimate of lymph node involvement of each group. It was 6.8, 5.6, and 29 %, respectively. This new information regarding the relationship of histologic grade of PMCA to incidence of regional lymph node involvement may be of value in the surgical decision to perform appendectomy only versus right colon resection. The algorithm proposed for the surgical options is shown in Fig. 1. For MAN with DPAM histology and peritoneal metastases, the treatment is cytoreductive surgery with appendectomy and hyperthermic intraperitoneal chemotherapy. The same recommendation is made for PMCA histology if peritoneal metastases histology shows well- or moderately differentiated neoplasms. For PMCA histology with peritoneal metastases showing poorly differentiated appendiceal mucinous neoplasms or intestinal type (nonmucinous) neoplasms, a right colon resection with regional lymph node dissection is needed.
In the absence of a right colon resection, the absence of lymph node metastases was determined by negative appendiceal lymph node sampling. Using this sentinel lymph node approach leaves open the possibility for occult lymph nodes within the ileocolic group to grow at a later time. In order to test that possibility, we surveyed 107 patients whose disease failed to respond to cytoreductive surgery with perioperative chemotherapy, so they either required second-look surgery or were going to die of their disease. If there were ileocolic occult lymph nodes left behind, one would expect a recurrence to be evident within the ileocolic lymph node group at the time of recurrence. In a CT assessment and/or operative assessment, the progression of the disease in ileocolic lymph nodes was sought. None of these patients had clinical suspicion for progression of ileocolic lymph nodes by second look or by CT. By this second assessment, evidence for cancer dissemination to regional lymph nodes when appendiceal lymph nodes were determined to be negative seems highly unlikely.
References
Gonzalez-Moreno S, Sugarbaker PH. Right hemicolectomy does not confer a survival advantage in patients with mucinous carcinoma of the appendix and peritoneal seeding. Br J Surg. 2004;91:304–11.
Foster JM, Gupta PK, Carreau JH, et al. Right hemicolectomy is not routinely indicated in pseudomyxoma peritonei. Am Surg. 2012;78:171–7.
Turaga KK, Pappas S, Clark Gamblin T. Right hemicolectomy for mucinous adenocarcinoma of the appendix: just right or too much? Ann Surg Oncol. 2013;20:1063–7.
Ronnett BM, Shmookler BM, Sugarbaker PH, Kurman RJ. Pseudomyxoma peritonei: new concepts in diagnosis, origin, nomenclature, relationship to mucinous borderline (low malignant potential) tumors of the ovary. In: Fechner RE, Rosen PP, editors. Anatomic pathology. Chicago: ASCP Press; 1997. p. 197–226.
Yan H, Pestieau SR, Shmookler BM, Sugarbaker PH. Histopathologic analysis in 46 patients with pseudomyxoma peritonei syndrome: failure vs. success with a second-look operation. Mod Pathol. 2001;14:164–71.
Sugarbaker PH. An overview of peritonectomy, visceral resections, and perioperative chemotherapy for peritoneal surface malignancy. In: Sugarbaker PH, editor. Cytoreductive surgery and perioperative chemotherapy for peritoneal surface malignancy. Woodbury: Cine-Med Publishing; 2012. p. 1–30.
Gonzalez-Moreno S, Brun E, Sugarbaker PH. Lymph node metastases in epithelial malignancies of the appendix with peritoneal dissemination does not reduce survival in patients treated by cytoreductive surgery and perioperative intraperitoneal chemotherapy. Ann Surg Oncol. 2005;12:72–80.
Disclosure
The author declares no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sugarbaker, P.H. When and When Not to Perform a Right Colon Resection with Mucinous Appendiceal Neoplasms. Ann Surg Oncol 24, 729–732 (2017). https://doi.org/10.1245/s10434-016-5632-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5632-2