Abstract
Purpose
To compare radiation exposure associated with daily practice cardiovascular (CV) examinations performed on two different multidetector computed tomography (MDCT) scanners, a conventional 64-MDCT and a third-generation dual-source (DS) MDCT.
Materials and methods
In this retrospective study, 1458 patients who underwent CV examinations between January 2017 and August 2018 were enrolled. A single-source 64-MDCT (Lightspeed VCT, GE) scan was performed in 705 patients from January to August 2017 (207 coronary examinations and 498 vascular examinations) and 753 patients underwent third-generation 192 × 2-DSCT (Somatom FORCE, Siemens) scan from January to August 2018 (302 coronary examinations and 451 vascular examinations). Volume CT dose index (CTDIvol), dose length product (DLP), effective dose (ED), tube voltage (TV) and exposure time (ET), pitch factor (PF) were registered for each patient. Student’s t test was used to compare mean values between each corresponding group of MDCT and DSCT.
Results
In coronary examinations with DSCT, CTDIvol was 24.4% lower (23.1 mGy vs 30.6 mGy, p < 0.0001) and DLP and ED reductions were 35.6% than with MDCT (465.0 mGy * cm vs 732.3 mGy * cm and 6.5 mSv and 10.3 mSv; vs p < 0.0001). Concerning scan parameters, kVp and ET reductions were 12.7% and 69.4%, respectively (p < 0.0001); PF increase was 73.8% (p < 0.0001). In all vascular studies, DSCT, compared with MDCT, permitted to reduce CTDIvol from 43.5 to 70.6%; DLP and ED reductions were from 50.3 to 73.1%; kVp and ET decreases were from 10.7 to 32.5% and from 26.3 to 68.7%. PF increase was from 16.7 to 58.1% (all differences with p < 0.0001).
Conclusions
In daily practice, CV examinations CTDI, DLP, ED, ET and TV were lower and PF was higher with 192 × 2-DSCT compared to 64-MDCT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
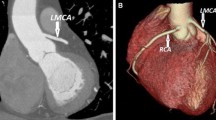
Over the last two decades, computed tomography angiography (CTA) has witnessed significant developments in the diagnosis of cardiovascular (CV) disease, owing to technical improvements in CT imaging, which allows rapid data acquisition with high spatial and temporal resolution [1, 2]. CTA has been widely used in the diagnostic evaluation of many vascular diseases, and serves as first-line modality in the early diagnosis of abdominal aortic aneurysm or aortic dissection and to follow-up patients treated with endovascular stents and stent grafts, with the aim of determining their patency or potential complications [3,4,5,6,7,8,9,10]. On the other side, coronary CTA represents one of the most important technical advancements in CV CT practice, and it is the standard clinical assessment for patients with low-to-intermediate pretest probability for coronary artery disease [11,12,13,14,15,16,17,18,19,20].
However, radiation exposure during diagnostic examinations remains an issue of concern for potential cancer risk radiation-related [21,22,23]. Accordingly, safety considerations of coronary CTA are an ongoing concern to reduce radiation dose exposure, while maintaining diagnostic image quality. Indeed, an effective dose of 5 mSv adds only a small, negligible additional risk to lifetime cancer risk, but the diagnostic information and the clinical consequences resulting from a coronary CTA may outweigh this very small theoretical additional cancer risk [24].
Related to this, the introduction of dual-source CT (DSCT) scanners provided a series of improvements, such as fast gantry rotation speed (from 280 to 250 ms), increased longitudinal detector coverage (from 38 mm for 128-slice DSCT to 58 mm for 192-slice DSCT) and more powerful roentgen tube. This causes reduced gantry rotation time and high-pitch values, which combined with the possibility to reach higher mAs and consequently to reduce kV, should improve image quality and reduce radiation dose, compared with the other CT scanner. Moreover, the DCST scanners equipped of two X-ray sources at 95° to each other [25] provided a new scan protocol, defined TurboFlash (TFP), suitable for patient with regular heart rate lower than 65 beats per minute (bpm) that allows minimal radiation exposure and concurrent reduction in any motion artifacts from moving structures, such as heart, valves or pulsating aortic root [26,27,28,29,30,31]. In addition, faster scan provided by DSCT makes prospective protocol (PP) more widely available (suitable for patient with regular heart rate between 66 and 80 bpm), at low radiation dose [32].
Many clinicians may still be unfamiliar with the magnitude of radiation exposure arising from CTA in daily practice and the tremendous progress that new scanners provide in radiation dose reduction while maintaining or enhancing image quality [33, 34].
Consequently, the purpose of this study was to compare 192 × 2-slice third-generation DSCT and conventional 64-slice single-source MDCT performances in CV examinations, regarding radiation exposure and main scanning parameters that may influence it.
Materials and methods
Patient selection
We retrospectively selected patients from the radiological database of our Hospital who underwent body CV CT examinations from January 2017 to August 2018. Collected sample was divided in two cohorts. The first cohort was composed by patients imaged with a 64-MDCT scanner, between January 2017 to August 2017, divided in coronary examinations and vascular examinations. The second cohort was composed by patients imaged with a 192 × 2-DSCT scanner, from January 2018 to August 2018. Exclusion criteria were: groups of CV type examinations with size smaller than 30 patients in 64-MDCT or in DSCT (superior limbs artery examination, n = 2 with SSCT and n = 15 with DSCT; coronary examinations performed with PP in 64-MDCT n = 7). We chose to collect patients from the same period of two different years to obtain two cohorts as homogenous as possible.
The final population was made up of 1458 patients. The first cohort, composed by 705 patients, is divided in 207 coronary examinations, all examined with retrospective protocol (RP), and 498 vascular examinations. The second cohort, composed by 753 patients, is divided in 302 coronary examinations and 451 vascular examinations. Features of each group are summarized in Table 1.
CT scan protocols
All CT scans were performed with patients in supine position and feet toward the gantry. A 20-gauge cannula was inserted into superficial vein of the right antecubital fossa, connected to a two-way injector: one with contrast medium (CM) (Iopamidol, 370 mg I/ml, Bracco) and the other with saline solution.
64-MDCT (Lightspeed VCT, GE)
Coronary protocol
Retrospective ECG trigger was used. Patients with a heart rate greater than 65 bpm and without contraindications (i.e., severe aortic stenosis, systolic blood pressure < 90 mmHg, bronchial asthma, symptomatic heart failure or advanced atrioventricular block) underwent β-blockade with 25 mg of atenolol by mouth, the evening before the examination. Alternatively, heart rate control with a target of 60 bpm was achieved using 10–60 mg of propranolol injected intravenous before data acquisition.
Bolus tracking technique was used. CM volume was weight-based (1.5 ml/kg) with flow rate of 5 ml/s followed by 50 ml of saline solution at the same flow rate. Scan started, manually, 6 s after that CM arrived in the left ventricle.
Vascular protocol
Bolus tracking technique was used. CM volume was weight-based (2 ml/kg) with flow rate of 3.5 ml/s followed by 50 ml of saline at the same flow rate. Scan started, automatically, 10 s after that a region of interest (ROI) enhancement reached 150 Hounsfield Unit (HU).
Table 2 summarized scan parameters for CV protocols with 64-MDCT.
192 × 2-DSCT (Somatom FORCE, Siemens)
Coronary protocol
ECG-triggered scan was performed with TFP in patients with rhythmic heart rate lesser than 65 bpm, with PP in patients with rhythmic heart rate between 66 and 80 bpm and with RP in patients with heart rate greater than 80 bpm or in case of arrhythmia.
Bolus test technique was used: 4 ml of CM at flow rate of 5 ml/s followed by 35 ml of saline solution at the same flow rate was used to evaluate peak time (PT) in ascending aorta. For scan acquisition was used 45 ml of CM at 5 ml/s followed by 35 ml of saline solution at the same.
Vascular protocol
Bolus tracking technique was used. ECG trigger was employed for thoracic aorta and thoracic–abdominal aorta studies. CM volume was weight-based (1 ml/kg) with flow rate of 5 ml/s followed by 50 ml of saline at the same flow rate. Scan started, automatically, 6 s after that ROI enhancement reached 250 Hounsfield Unit (HU).
Table 3 summarized scan parameters for CV protocols with 192 × 2-DSCT.
Radiation dose
Volume CT dose index (CTDIvol) and dose length product (DLP) were registered for each patient. Effective dose (ED), an useful parameter to optimize RD, was calculated by multiplying DLP value by k factor (k = 0.014 for thoracic examinations and k = 0.015 for abdominal or thoracic–abdominal examinations), according to guidelines from the American Association of Physicists in Medicine [35]. Mean ED values were calculated and compared for each group in MDCT and DSCT.
Scanning parameters
TV, exposure time (ET) and pitch factor (PF) were registered for each patient. Mean values were calculated and compared for each group in MDCT and DSCT.
Statistical analyses
All statistical analyses were performed using MedCalc Software v. 15.8 (Ostend, BEL). The unpaired Student’s t test was used to compare between each groups CTDIvol, DLP, ED, TV, ET and PF. For all comparisons, p value less than 0.05 was considered statistically significant.
Results
Coronary study: radiation dose and scanning parameters
In Table 4 are summarized and compared CTDIvol, DLP, ED, TV, ET and PF between DSCT and MDCT with RP. With DSCT, CTDIvol, DLP, ED, kVp and ET were statistically significant lower than with MDCT. PF was significantly higher.
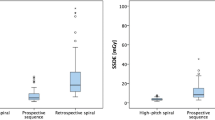
In Table 5 are summarized and compared CTDIvol, DLP, ED, kVp, ET and PF between TFP, PP and RP in DSCT. TFP provided CTDIvol, DLP, ED and ET statistically significant reductions compared to PP and RP; in contrast, PF was significantly higher. PP provided lower CTDIvol, DLP, ED, TV, ET and PF compared to RP. Figure 1 compares ED between MDCT and DSCT in each coronary protocol.
Vascular study: radiation dose and scanning parameters
All values are summarized in Table 6.
In each vascular studies, MDCT, CTDI, DLP, ED, ET and TV were significantly lower compared to DSCT; in contrast, PF was statically significant higher. Figure 2 compares ED between each group in MDCT and DSCT.
Discussion
CTA has been widely used in the diagnostic evaluation of many CV diseases [1,2,3,4,5]. Its increasing use raises justified concerns about radiation exposure and the associated cancer risk [21]. DSCT scanners with two X-ray sources at 95° to each other [25] provided some improvements capable of reducing radiation exposure. Among the others, the introduction of TFP for CTA examinations appears to be very effective [26,27,28,29,30,31].
In the present work, with RP, we obtained in coronary examinations with DSCT, 24.4% CTDIvol decrease and 35.6% DLP and ED reductions than with MDCT (p < 0.0001). By evaluating all considered scanning parameters, our hypothesis are that the radiant dose saving is associated with the TV reduction (12.7%) and ET decrease (69.4%) resulting by PF increase (73.8%). The new generation of iterative reconstruction and the increase in their application level, from adaptive statistical iterative reconstruction (ASiR, GE Healthcare) median level 30 to advanced modeled iterative reconstruction (ADMIRE, Siemens Healthineers) median level 3, could have contributed to TV and ET reductions and radiation dose decrease.
In our work, there are no coronary examinations in 64-MDCT with PP because with this protocol the risk to obtain non-diagnostic images for motion artifacts was very high. Anyway, considering only DSCT results, TFP provided CTDIvol, DLP, ED and ET statistically significant reductions compared to PP and RP, resulting by different PF (2.9 with TFP, 0.8 with PP and 0.9 with RP). In addition, PP provided CTDIvol, DLP, ED, TV, ET reductions compared to RP. In all three protocols, mean TV was between 80 and 90 kV, but it was significantly lower with PP compared to TFP and RP, which instead showed the greater TV (87.8 kV); this can partly justify the higher dose delivered compared with the other protocols. In fact, the most relevant difference between the three protocols is related with ET, significantly lower in RP compared, respectively, with PP (− 60.0%) and RP (− 74.8%), which conceivably has to be considered the largest cause of radiation dose reduction.
Concerning vascular examinations, the greater radiation dose reduction, with DSCT, was found in inferior limb artery study, with 73.1% DLP and ED decrease. In this case, iterative reconstruction application levels in MDCT and DSCT are similar, ASiR (GE Healthcare) median level 50, and ADMIRE (Siemens Healthineers) median level 3 and the impact on acquisition parameters, such as TV and ET, and on radiation dose are less evident than in coronary exams.
In thoracic aorta, abdominal aorta and thoracic–abdominal aorta examinations DLP and ED reductions were 65.8%, 53.1% and 50.3%, respectively. Our hypothesis is that the higher reduction in lower limb artery examination is related with the greater TV decrease compared to the thoracic, abdominal and thoracic–abdominal studies (32.5% vs 12.1, 18.2 and 10.7%, respectively).
However, in all vascular examinations with DSCT compared with 64-MDCT, DLP and ED reduction are probably related to higher PF and lower TV. In particular, the greatest ET reduction occurred in thoracic aorta examinations where at the same time, there was the greater PF increase, compared with the other vascular examinations. On the contrary, due to the need of leaving time to contrast media to arrive at limb extremities, the lowest ET reduction was found in the examinations of lower limb arteries associated with the smaller PF increase, compared to the other vascular exam types. Another remarkable aspect to underline is that in thoracic aorta and thoracic–abdominal aorta, ET and kV were significantly lower with DSCT than with 64-MDCT, because the prospective ECG triggering sometimes used in the latter one was very burdensome in terms of radiation exposure, due to smaller tube coverage and lower PF, which results in higher ET.
To the best of our knowledge, no work has compared radiation dose and scanning parameters between 192-DSTC and 64-SSCT. Only Meyer et al. [36] have compared 192 × 2-DSCT with RP and 128-DSCT, obtaining with the first one DLP and ED values lower than in the present study (324.0 mGy * cm vs 465.0 mGy * cm, 4.5 mSv vs 6.5 mSv, respectively). However, they used 70 kV for all examinations and disabled ECG-controlled tube current modulation, as a standard protocol, instead of our experience in which we prefer to use an automatic modulation of tube voltage (CARE kV, Siemens, Medical Solution) and tube current (CARE dose 4D, Siemens). Moreover, with TFP and PP, our DLP and ED values (129.0 mGy * cm and 242.1 mGy * cm, 1.8 mS and 3.4 mSv, respectively) were lower than these authors. No work has compared radiation dose and scanning parameters between 192-DSTC and 64-SSCT or others scanner in vascular examinations.
Our study has some limitations. First, the study is based on a historical comparison, with no guarantee that the populations are entirely comparable, even if patients were selected from the database of the same Hospital. Second, this was a retrospective study with a relatively small patient cohort in each group; larger prospective studies may be required to confirm our findings. Third, comparisons were made between two consecutive patient groups. Intra-individual comparisons with repeated examinations using different protocols would strengthen our claims, but this is not possible for obvious ethical reasons.
In conclusion, in CV examinations, CTDI, DLP and ED considerably decrease with 192-DSCT in comparison with conventional 64-MDCT, and we can hypothesize that the reduction is mainly associated with higher PF and TV used.
References
Sun Z, Mwipatayi BP, Allen YB, Hartley DE, LawrenceBrown MM (2009) Multislice CT angiography of fenestrated endovascular stent grafting for treating abdominal aortic aneurysms: a pictorial review of the 2D/3D visualizations. Korean J Radiol 10:285–293
Castañer E, Andreu M, Gallardo X, Mata JM, Cabezuelo MA, Pallardó Y (2003) CT in nontraumatic acute thoracic aortic disease: typical and atypical features and complications. Radiographics 23:S93–110
Sebastià C, Pallisa E, Quiroga S, Alvarez-Castells A, Dominguez R, Evangelista A (1999) Aortic dissection: diagnosis and follow-up with helical CT. Radiographics 19:45–60
Schoepf UJ, Goldhaber SZ, Costello P (2004) Spiral computed tomography for acute pulmonary embolism. Circulation 109:2160–2167
Perrier A, Roy PM, Sanchez O, Le Gal G, Meyer G, Gourdier AL, Furber A, Revel MP, Howarth N, Davido A, Bounameaux H (2005) Multidetector-row computed tomography in suspected pulmonary embolism. N Engl J Med 352:1760–1768
Rozenblit AM, Patlas M, Rosenbaum AT, Okhi T, Veith FJ, Laks MP, Ricci ZJ (2003) Detection of endoleaks after endovascular repair of abdominal aortic aneurysm: value of unenhanced and delayed helical CT acquisitions. Radiology 227:426–433
Armerding MD, Rubin GD, Beaulieu CF, Slonim SM, Olcott EW, Samuels SL, Jorgensen MJ, Semba CP, Jeffrey RB Jr, Dake MD (2000) Aortic aneurysmal disease: assessment of stent-graft treatment-CT versus conventional angiography. Radiology 215:138–146
Stavropoulos SW, Clark TW, Carpenter JP, Fairman RM, Litt H, Velazquez OC, Insko E, Farner M, Baum RA (2005) Use of CT angiography to classify endoleaks after endovascular repair of abdominal aortic aneurysms. J Vasc Interv Radiol 16:663–667
Sun Z (2003) Helical CT angiography of abdominal aortic aneurysms treated with suprarenal stent grafting. Cardiovasc Intervent Radiol 26:290–295
Rydberg J, Kopecky KK, Lalka SG, Johnson MS, Dalsing MC, Persohn SA (2001) Stent grafting of abdominal aortic aneurysms: pre-and postoperative evaluation with multislice helical CT. J Comput Assist Tomogr 25:580–586
Sun Z, Jiang W (2006) Diagnostic value of multislice computed tomography angiography in coronary artery disease: a meta-analysis. Eur J Radiol 60:279–286
Sun Z, Lin C, Davidson R, Dong C, Liao Y (2008) Diagnostic value of 64-slice CT angiography in coronary artery disease: a systematic review. Eur J Radiol 67:78–84
Vanhoenacker PK, Heijenbrok-Kal MH, Van Heste R, Decramer I, Van Hoe LR, Wijns W, Hunink MG (2007) Diagnostic performance of multidetector CT angiography for assessment of coronary artery disease: meta-analysis. Radiology 244:419–428
Abdulla J, Abildstrom SZ, Gotzsche O, Christensen E, Kober L, Torp-Pedersen C (2007) 64-multislice detector computed tomography coronary angiography as potential alternative to conventional coronary angiography: a systematic review and meta-analysis. Eur Heart J 28:3042–3050
Stein PD, Yaekoub AY, Matta F, Sostman HD (2008) 64-Slice CT for diagnosis of coronary artery disease: a systematic review. Am J Med 121:715–725
Mowatt G, Cook JA, Hillis GS, Walker S, Fraser C, Jia X, Waugh N (2008) 64-Slice computed tomography angiography in the diagnosis and assessment of coronary artery disease: systematic review and meta-analysis. Heart 94:1386–1393
Sun Z (2012) Cardiac CT imaging in coronary artery disease: current status and future directions. Quant Imaging Med Surg 2:98–105
Sun Z, Choo GH, Ng KH (2012) Coronary CT angiography: current status and continuing challenges. Br J Radiol 85:495–510
Guo SL, Guo YM, Zhai YN, Ma B, Wang P, Yang KH (2011) Diagnostic accuracy of first generation dual-source computed tomography in the assessment of coronary artery disease: a meta-analysis from 24 studies. Int J Cardiovasc Imaging 27:755–771
Pelliccia F, Pasceri V, Evangelista A, Pergolini A, Barillà F, Viceconte N, Tanzilli G, Schiariti M, Greco C, Gaudio C (2013) Diagnostic accuracy of 320-row computed tomography as compared with invasive coronary angiography in unselected, consecutive patients with suspected coronary artery disease. Int J Cardiovasc Imaging 29:443–452
Lee CI, Haims AH, Monico EP, Brink JA, Forman HP (2004) Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology 231:393–398
Einstein AJ, Henzlova MJ, Rajagopalan S (2007) Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 298:317–323
Alkadhi H, Leschka S (2011) Radiation dose of cardiac computed tomography—what has been achieved and what needs to be done. Eur Radiol 21:505–509
Stocker TJ et al (2018) Reduction in radiation exposure in cardiovascular computed tomography imaging: results from the PROspective multicenter registry on radiaTion dose Estimates of cardiac CT angIOgraphy iN daily practice in 2017 (PROTECTION VI). Eur Heart J 39(41):3715–3723
Petersilka M, Bruder H, Krauss B, Stierstorfer K, Flohr TG (2008) Technical principles of dual source CT. Eur J Radiol 68:362–368
Alkadhi H, Stolzmann P, Desbiolles L et al (2010) Low-dose, 128-slice, dual-source CT coronary angiography: accuracy and radiation dose of the high-pitch and the step-and-shoot mode. Heart 96:933–938
Achenbach S, Marwan M, Ropers D et al (2010) Coronary computed tomography angiography with a consistent dose below 1 msv using prospectively electrocardiogramtriggered high-pitch spiral acquisition. Eur Heart J 31:340–346
Leschka S, Stolzmann P, Desbiolles L et al (2009) Diagnostic accuracy of high-pitch dual-source CT for the assessment of coronary stenoses: first experience. Eur Radiol 19:2896–2903
Achenbach S, Goroll T, Seltmann M et al (2011) Detection of coronary artery stenoses by low-dose, prospectively ECG-triggered, high-pitch spiral coronary CT angiography. JACC Cardiovasc Imaging 4:328–337
Lell M, Marwan M, Schepis T et al (2009) Prospectively ECG-triggered high-pitch spiral acquisition for coronary CT angiography using dual source CT: technique and initial experience. Eur Radiol 19:2576–2583
Apfaltrer G et al (2017) Impact on image quality and radiation dose of third-generation dual-source computed tomography of the coronary arteries. Am J Cardiol 119:1156–1161. https://doi.org/10.1016/j.amjcard.2016.12.028
Linsen PMV et al (2016) Computed tomography angiography with a 192-slice dual-source computed tomography system: improvements in image quality and radiation dose. J Clin Imaging Sci 6:44
Morsbach F, Gordic S, Desbiolles L, Husarik D, Frauenfelder T, Schmidt B et al (2014) Performance of turbo high-pitch dual-source CT for coronary CT angiography: first ex vivo and patient experience. Eur Radiol 24:1889–1895
De Zordo T, von Lutterotti K, Dejaco C et al (2012) Comparison of image quality and radiation dose of different pulmonary CTA protocols on a 128-slice CT: high-pitch dual source CT, dual energy CT and conventional spiral CT. Eur Radiol 22:279–286. https://doi.org/10.1007/s00330-011-2251-y
American Association of Physicists in Medicine (2008) The measurement, reporting and management of radiation dose in CT Report of AAPM Task Group 23 of the Diagnostic Imaging Council CT Committee
Meyer M et al (2017) Radiation dose levels of retrospectively ECG-gated coronary CT angiography using 70-kVp tube voltage in patients with high or irregular heart rates. Acad Radiol 24:30–37. https://doi.org/10.1016/j.acra.2016.08.004
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflict of interest associated with this study.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Agliata, G., Schicchi, N., Agostini, A. et al. Radiation exposure related to cardiovascular CT examination: comparison between conventional 64-MDCT and third-generation dual-source MDCT. Radiol med 124, 753–761 (2019). https://doi.org/10.1007/s11547-019-01036-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-019-01036-6