Abstract
Noninvasive coronary angiography with multislice computed tomography (CT) scanners is feasible with high sensitivity and negative predictive value. The radiation exposure associated with this technique, however, is high and concerns in the widespread use of CT have arisen. We evaluated the diagnostic accuracy of coronary angiography using 320-row CT, which avoids exposure-intensive overscanning and overranging. We prospectively studied 118 unselected consecutive patients with suspected coronary artery disease (CAD) referred for invasive coronary angiography (ICA). All patients had 320-row CT within 1 week of ICA, which, together with quantitative analysis, served as the reference standard. Of the 65 out of 118 patients who were diagnosed as having CAD by ICA, 64 (98 %) were correctly identified at 320-row CT. Noteworthy, 320-row CT correctly detected CAD in 3 patients with atrial fibrillation and ruled out the disease in the other 8 patients. From 151 significant coronary stenoses detected on ICA, 137 (91 %) were correctly identified with 320-row CT. In the per-patient analysis, sensitivity and specificity of 320-row CT were 98 and 91 %, respectively. In the per-vessel analysis, sensitivity and specificity of 320-row CT were 93 and 95 %, respectively. In the per segment analysis, sensitivity and specificity of 320-row CT were 91 and 99 %, respectively. Diameter stenosis determined with the use of CT showed good correlation with ICA (P < 0.001, R = 0.81) without significant underestimation or overestimation (−3.1 ± 24.4 %; P = 0.08). Comparison of CT with ICA revealed a significantly smaller effective radiation dose (3.1 ± 2.3 vs. 6.5 ± 4.2 mSv; P < 0.05) and amount of contrast agent required (99 ± 51 vs. 65 ± 42 ml, P < 0.05) for 320 row CT. The present study in an unselected population including patients with atrial fibrillation demonstrates that 320-row CT may significantly reduce the radiation dose and amount of contrast agent required compared with ICA while maintaining a very high diagnostic accuracy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Computed tomography (CT) has become a highly accurate noninvasive approach for delineation of the presence and severity of coronary artery disease (CAD) based on the results of multiple studies performed with the 64-row CT [1–3]. With its high negative predictive value cardiac, CT is optimally suited for the non-invasive exclusion of CAD at relatively low cost and risk [4]. While the number of CT examinations in cardiac imaging continues to increase, concerns in the widespread use of CT have arisen, given either the current technical limitations of the technique or the fact that CT is a high-radiation imaging modality [5].
Expansion of CT systems from 64-row to the latest models of 320-row systems has allowed whole heart coverage in one gantry rotation, with a slice thickness of 0.5 mm, yielding a maximum of 16 cm of cranio-caudal coverage in a single heart-beat [6, 7]. Similarly to the newest scanners that using prospective ECG-triggered high-pitch helical scanning allow low radiation dose [8, 9], 320-row CT provides excellent image quality [10], with an ability to study also patients with arrhythmias including atrial fibrillation [11].
We have therefore conducted a prospective study to analyze the effective dose and diagnostic performance of 320-row CT compared with invasive coronary angiography (ICA) in patients with suspected CAD.
Methods
Study population
This study was planned prospectively as a single Institution assessment of 320-row CT for the detection of coronary artery stenosis with ≥50 % diameter obstruction, with quantitative analysis of ICA used as the reference standard. Patients were eligible for the study if they were at least 40 years of age, because younger patients have increased susceptibility to ionizing radiation [12]. Between January 1, 2011 and June 30, 2011, 551 consecutive patients underwent ICA for suspected CAD at our Institution. Patients were included in this study regardless of weight and cardiac rhythm, whereas 25 were excluded because they were younger than 40 years, 181 because of diagnosis of acute coronary syndrome, 169 because of a previous diagnosis of CAD, 20 because of history of allergic reaction, 28 for chronic renal failure (i.e., estimated glomerular filtration rate <60 ml/min/1.73 m2), and 10 for lack of consent. Thus, the final study-group consisted of 118 consecutive patients (78 men and 40 women, mean age: 61 ± 10 years, range: 40–80 years).
Study protocol
Patients underwent 320-row CT within 1 week of ICA. If no contraindications were present, each patient received sublingual isosorbide dinitrate (5 mg) before scanning. In case of heart rate >65 beats/min, patients were given 50 mg of metoprolol orally 1 h before CT examination and, additionally, intravenous metoprolol (up to 3 doses of 5 mg) if the heart rate was still >65 beats/min. The study conforms to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Institutional Board Review Committee of our Institution (ID Number: 671/2009/D). All participants gave their written informed consent for the entire study, including radiation exposure. The STARD guidelines for reporting studies of diagnostic accuracy were followed [13].
Coronary assessment with 320-row CT
Imaging was performed with a snapshot (no table movement, pitch of 0) whole-heart scan on a 320-row CT with 0.5-mm detector elements, 350 ms of gantry rotation time, and up to 16 cm of coverage in Z direction (Aquilion ONE, Toshiba Medical Systems, Otawara, Japan). The median Z direction scan range covered was 12 cm (range, 12–14 cm). Scanner settings of 350–450 mA (350 mA for <60 kg, 400 mA for 60–80 kg, and 450 mA for >80 kg) and 120 kV were used. In all patients, the aim was to achieve a target heart rate ≤65 bpm during scanning because this is the threshold below which there is a sufficiently long rest period of the coronary arteries to allow scanning during a single heartbeat. In the 8 patients with heart rate >65 bpm at time of CT scanning, 2 or 3 heartbeats were used for image acquisition to allow multicycle reconstruction to be applied for improved temporal resolution. Immediately before the contrast agent was injected, a breathhold trial was performed by simulating scanning with a single 5-second breathhold command to adjust scanner settings to individual patients as described recently [14]. The iodinated contrast media used were iomeprol 400 (Iomeron, 400 mg I/ml; Bracco, Milan, Italy) and iopamidol 370 (Iopamiro, 370 mg I/ml; Bracco, Milan, Italy). The average breathhold time was 3.6 ± 0.6 s (including a 3-second delay before scanning, so that the heart rate can normalize after submaximal inspiration) [15]. The bolus tracking method was used to achieve adequate contrast enhancement in the coronary arteries, initiating CT scanning after a threshold of 180 Hounsfield units in the descending aorta had been reached [16]. Prospective CT angiography was performed from 70 to 100 % and 35 to 100 % of the RR interval in patients with heart rates of ≤65 and >65 bpm, respectively. Dose-length product measurements were displayed after each scan on the scanner’s console. Data were reconstructed with 0.25-mm slice increments, providing up to 640 axial slices with 0.5-mm thickness.
Image analysis was carried out in all 16 coronary artery segments (according to the classification of the American Heart Association) [17], plus the intermediate branch if present (i.e., segment 17) and constituted the basis for detection of at least 50 % diameter stenosis independent of reference vessel size. Assessment of stenoses was performed by two readers unaware of the ICA result with the workstation’s (Vitrea2 FX, Vital Images, Plymouth, Minnesota) coronary artery CT protocol using a vessel detection tool available with the workstation, which allowed the automatic creation of curved multiplanar reformations along the coronary arteries, maximum-intensity projections, and so-called CATH views [18]. Boundaries of the vessel wall were manually corrected if the automatically extracted boundaries needed adjustment. The degree of stenosis was measured by correlating the difference between the reference vessel diameter (average of 2 measurements directly proximal and distal to the stenosis) and the stenotic vessel diameter to the reference vessel diameter. All coronary artery segments with at least 20 % diameter reduction were classified quantitatively on images orthogonal to the vessel (cross-sectional images).
Quantitative coronary angiography
Quantitative ICA was regarded as the gold-standard method. Left and right coronary angiography was performed in multiple views by using the transfemoral Judkins approach within 1 week of CT. Quantitative ICA allowed identification of arteries with significant flow-limiting lesion as defined by a >50 % diameter stenosis. The operators who performed the evaluation were unaware of the study protocol and patients characteristics. Digital angiograms were analyzed off-line with the use of an automated edge-detection system (Cardiovascular Medical System, MEDIS Imaging Systems, Leiden, The Netherlands) [19]. A dose of 200 micrograms of intracoronary nitroglycerin was given before coronary angiography. All measurements were performed on cineangiograms recorded after nitroglycerin administration [20]. All visible lesions, including wall irregularities, were analyzed on the angiograms. Multiple lesions within one coronary artery segment were considered distinct whenever separated by a visually smooth arterial wall. The measurement of percent diameter stenosis was performed in the projection showing the highest degree of narrowing. The contrast-filled nontapered catheter tip was used for calibration, and the reference diameter was measured by interpolation. At baseline, all segments >2 mm in diameter with a >20 % but <100 % diameter stenosis were measured [19]. Percent diameter stenosis was calculated as (reference diameter-minimal luminal diameter)/(reference diameter) × 100).
Effective dose radiation estimation
Radiation dose for 320-row CT was determined on the basis of the dose-length product (DLP), as documented in the CT scan protocol separately for the test bolus acquisition and the coronary CT acquisition. Effective doses were estimated as a product of DLP × a conversion coefficient for the chest in adults (k = 0.014 mSv/mGy × cm) averaged between male and female models [21]. Similarly, radiation dose for ICA was estimated as a product of the dose-area product (DAP) of the diagnostic coronary scenes × a conversion factor for the chest (k = 0.22 mSv/mGy × cm2) based on the National Radiological Protection Board tables [22].
Statistical analysis
Data are presented as mean ± standard deviation for continuous variables or frequency percentages (with 95 % CI) for categorical variables. In all study patients, pretest likelihood of CAD was calculated according to an updated Diamond–Forrester [23]. Kolmogorov–Smirnov testing was applied to assess normality of distribution for continuous variables. Chi-square test, or Fisher’s exact tests, when appropriate, were used to compare differences between categorical variables. Continuous variables were compared by t test or Mann–Whitney U test. Diagnostic accuracy of 320-row CT to detect significant coronary stenoses was compared to ICA as the reference standard and presented as sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio and negative likelihood ratio (all with 95 % CI). Likelihood ratios were weighted for prevalence, when prevalence was different from 50 %, according to the formula: prevalence × sensitivity/(1-prevalence) × (1-specificity). We compared percent diameter stenoses determined by CT and quantitative ICA as described above using linear regression analysis (to determine correlation coefficients) [24], and Bland–Altman analysis (to determine limits of agreement) [25]. We also compared interobserver variability of CT and quantitative ICA for determining percent diameter stenosis using images from both tests analyzed by a second independent reader (separate second reader for each test). Agreement between the two readers was assessed by Cohen’s K statistics. Differences were considered statistically significant if the P value (twotailed) was <0.05. Analyses were performed with the SPSS 12.0 statistical package (SPSS Inc, Chicago, Illinois).
Results
Technical aspects
Time interval between 320-row CT and ICA was 2 ± 2 days (range: 1–7 days) and there were no clinical events between the two exams in any patient. For 320-row CT, DLP was 221 ± 164 mGy cm. For ICA, DAP was 29.5 ± 19.1 mGy cm2. Effective radiation dose was lower for 320-row CT angiography than for ICA (3.1 ± 2.3 vs. 6.5 ± 4.2 mSv; P < 0.05). Similarly, more contrast agent amount was required for ICA than for 320-row CT (99 ± 51 vs. 65 ± 42 ml, P < 0.05). Effective radiation dose with 320-row CT was 2.1 ± 1.1 mSv in the 110 patients who had standard acquisition and 4.2 ± 2.9 mSv in the 8 patients who had multicycle reconstruction. No segments were uninterpretable with the examinations, and no coronary artery anomalies were seen on both tests.
Clinical and angiographic features
Demographic and clinical characteristics of the study patients are depicted in Table 1. ICA identified 151 significant stenoses affecting 65 patients. According to ICA, patients were classified as having no CAD (N = 53), single-vessel disease (N = 24), two-vessel disease (N = 30), and three-vessel disease (N = 11). Of the 11 patients with atrial fibrillation at time of 320-row CT, 3 were found to have CAD. An intermediate branch was present in 21 patients, and therefore a total of 379 coronary arteries and a total of 1,909 coronary segments were available for analysis.
Relation between quantitative analysis of coronary arteries
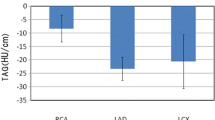
Analysis of all coronary artery segments with at least 20 % diameter reduction on ICA showed good correlation with percent diameter stenosis determined with the use of 320-row CT (R = 0.81, P < 0.001; Fig. 1) without significant underestimation or overestimation (−3.1 ± 24.4 %; P = 0.08) and 95 % limits of agreement between −25.1 and +22.3 % (Fig. 2). Figures 3 and 4 show a representative cases of coronary stenosis that were detected by both CT and ICA.
Representative case of accurate detection of significant coronary stenosis with both 320-row CT and ICA (a). The curved multiplanar reconstruction at 320-row CT reveals an ostial sub-total occlusion of the left anterior descending coronary artery (middle panel, arrow). The corresponding ICA confirms the presence of the sub-occlusive ostial stenosis in the left anterior descending coronary artery (left panel, arrow). The circumflex coronary artery (b) did not have evidence of any significant stenosis at both 320-row CT (right panel) and ICA (left panel). The right coronary artery (c) had a 80 % significant stenosis in the middle segment either at 320-row CT (right panel) or at ICA (left panel)
Representative case of accurate detection of significant coronary stenosis with both 320-row CT and ICA. A narrow significant stenosis in the proximal left anterior descending coronary artery (a) was seen at 320-row CT (right panel) and then confirmed at ICA (left panel). Conversely, the left circumflex artery and right coronary artery (b) did not show any significant stenosis at both 320-row CT and ICA
Patient, vessel and segment-based analysis
Of the 65 out of 118 patients who were diagnosed as having CAD by ICA, 64 (98 %) were correctly identified at 320-row CT, as well. Noteworthy, 320-row CT was able to detect CAD in 3 patients with atrial fibrillation and to rule out the disease in the other 8 patients with this condition. From a total of 151 significant coronary stenoses detected on ICA, 137 (91 %) were correctly identified with 320-row CT. Reasons for discrepancy between ICA and 320-row CT included the presence of a poor signal-to-noise ratio (N = 6), motion artifact (N = 5), and calcifications (N = 3). On the opposite, 7 stenoses at 320-row CT were false-positive findings at ICA, due to the presence of significant calcifications (N = 4) and poor signal-to-noise ratio (N = 3).
Table 2 provides direct comparisons of 320-row CT with ICA with regard to the analysis of patients, coronary arteries, and coronary segments considering a cut-off value of 50 % for significant stenosis (both for 320-row CT and ICA). In the per-patient analysis, the sensitivity and specificity of 320-row CT were 98 and 91 %, respectively. In the per-vessel analysis, the sensitivity and specificity of 320-row CT were 93 and 95 %, respectively. In the per-segment analysis, the sensitivity and specificity of 320-row CT were 91 and 99 %, respectively (Table 3).
Considering a cut-off value of 70 % for significant stenosis (both for 320-row CT and ICA) the per-patient sensitivity and specificity were 98 and 92 %, respectively, the per-vessel sensitivity and specificity were 92 and 96 %, respectively, and the per segment sensitivity and specificity were 88 and 100 %, respectively (Table 4).
Interobserver agreement
Agreement between the two readers was achieved for 366 of the 375 coronary arteries for ICA (98 %) and 360 of the 375 coronary arteries for 320-row CT (96 %, P = 0.30). Cohen’s κ in the per-patient analysis was 0.95 for quantitative ICA and 0.91 for 320-row CT. Cohen’s κ in the per-vessel analysis was 0.95 for quantitative ICA and 0.91 for 320-row CT. Cohen’s κ in the per-segment analysis was 0.94 for quantitative ICA and 0.89 for 320-row CT.
Discussion
Our study shows that 320-row CT compares favorably with ICA in the real world clinical practice, as it yields a similar diagnostic accuracy for CAD and provides a significant reduction in the effective radiation dose. In fact, with an average radiation dose of 3 mSv, 320-row CT reduced radiation exposure compared with the old coronary CTs’ with the use of conventional helical acquisition approaches (average of 12–15 mSv were reported in previous studies) [12].
Diagnosis of CAD
The introduction of 320-row CT has eliminated misalignment artifact seen in helical scanning techniques, thus further improving image quality and diagnostic performance [6–11]. In the present study we found excellent results with this technique: 320-row CT correctly identified patients with significant coronary stenoses with a 93 % positive predictive value and a 98 % negative predictive value and achieved a very good correlation with quantitative ICA also in quantifying the percent diameter stenosis, with a 95 % limits of agreement for evaluating coronary stenosis less than ±24 %.
Although previous studies have reported a good diagnostic value of 320-row CT, the role of the new technique in consecutive, unselected, elective patients with suspected CAD needs confirmation. In a study enrolling 64 patients, de Graaf et al. [26] reported a high diagnostic value in identifying patients with significant CAD with a 92 % positive predictive value and a 100 % negative predictive value. Also, Dewey et al. [27] studied 30 patients to evaluate information provided by 320-row CT with those obtained at conventional ICA, and found a positive predictive value of 92 % and a negative predictive value of 100 % in the per-patient analysis. Similarly, Nasis et al. [28] reported high diagnostic accuracy for 320-row CT in 63 patients, with positive predictive value of 88 % and negative predictive value of 93 % in the per-patient analysis as compared to ICA. Recently, two papers have described findings at 320-row CT in relative large groups of patients. van Velzen et al. [29] reported sensitivity of 100 % and specificity of 87 % for 320-row CT in 106 patients admitted to the Emergency Department with acute chest pain. However, 320-row CT was not compared with ICA in all cases, as patients with normal findings at CT did not undergo ICA but were discharged home. Also, Zhang et al. [30] have recently reported their experience on 107 patients who underwent 320-row CT only in order to compare the 100-kV and 120-kV protocols, but with no comparison with ICA. Overall, our data confirm and expand all these previous experiences, showing that 320-row CT may achieve excellent diagnostic accuracy.
The risk of radiation exposure
Despite the promising results in detecting CAD, CT has the disadvantage of requiring a high radiation dose. Conventional ICA requires a radiation dose from 3 to 9 mSv, while earlier studies underlined that coronary CT delivers a radiation dose as high as 20 mSv [11–13]. The radiation risks arising from coronary CT have raised concerns in the medical field [26]. Therefore, the benefit of using CT in the diagnostic workup and patient management must be weighed against the potential risks related to radiation exposure.
Despite the promising results in detecting CAD, CT is generally thought to have the disadvantage of requiring a high radiation dose. Earlier studies reported that coronary CT delivered a radiation dose as high as 20 mSv [14, 15], while conventional ICA requires a radiation dose from 3 to 9 mSv. For this reason, the radiation exposure associated with coronary CT has raised some concerns in the medical field and therefore the benefit of using CT in the diagnostic workup and patient management is usually weighed against the potential risks related to radiation exposure [31].
With the use of recent advances in technology, however, coronary CT is now able to achieve a significant and relevant dose reduction compared with the reference standard ICA. Radiation exposure with 320-row CT is particularly low in patients with heart rates <65 bpm, whereas the effective dose may be significantly higher in those with higher heart rates, where it may be necessary to acquire data over multiple cardiac cycles. It is also important to note that coronary 320-row CT allows the use of significantly less contrast agent than ICA.
Diagnosis of CAD in atrial fibrillation
As soon as introduced in clinical practice, coronary 320-row CT has shown to be able to properly work in patients with atrial fibrillation [11]. Pasricha et al. [32] compared image quality of 320-row CT in patients with atrial fibrillation with that acquired from the group with sinus rhythm. In this study, 96 % of the coronary segments were assessable with sufficient quality for diagnosis in patients with atrial fibrillation, and this showed the potential application of 320-row CT in this patient group. Similarly, Nasis et al. [28] reported that atrial fibrillation had no apparent influence on diagnostic accuracy. Although the number of patients with atrial fibrillation included in the present study is relatively low (N = 11), we did not find any difference in diagnostic accuracy in this group of patients: indeed, presence or absence of significant CAD was correctly identified in 3 patients and excluded in the remaining 8 patients with atrial fibrillation.
Pre-test probability of CAD
We found a relatively low prevalence of CAD in our unselected population of consecutive patients, and as many as 45 % of patients did not show coronary stenosis ≥50 %. Indeed, this finding is at variance with the results of previous investigations [26–28]. This may be due to specific features of the population studies, in particular, the exclusion by protocol of patients with known previous CAD. Since the most obvious indication for coronary CT is to rule out CAD in patients with a low to intermediate pretest likelihood of disease and given that the prevalence of disease influences the negative and positive predictive values of any diagnostic test, the present study may be more similar to the routine clinical use of CT scan. In our investigation, pretest likelihood was 46 % and prevalence was 38 %, making the results valid for patients with intermediate probability of disease, who are told to be those who benefit most from coronary CT [27].
Study limitations
Although a significant reduction of radiation dose is undisputable with 320-row CT, one should admit that other new modalities, such as dual-source CT [8], and high-pitch spiral CT [9], are reasonable alternatives to reduce radiation exposure. Accordingly, further studies aimed at comparing diagnostic accuracy and radiation exposure of the newer CT systems are needed to allow one to generalize the results of the present study. Indeed, use of radiation still limits the application of CT scan for serial measurements. In addition, patients who undergo noninvasive CT and are found to have a clinically significant stenosis require subsequent ICA with additional radiation exposure, highlighting the importance of properly selecting patients with low to intermediate likelihood of disease for CT [33]. One should admit that CT and ICA are both subjective tests, with considerable variation seen between different readers. Since the aim of the study was to compare CT and ICA in a real world situation (where CT would be performed before or instead of ICA), quantitative assessment of coronary stenoses at 320-row CT was performed by readers unaware of findings at ICA, and therefore minimum coronary diameters at 320-row CT could not always be measured in the same orientation accessible by ICA. Our analysis of quantification of coronary artery stenosis, however, shows similar accuracy of 320-row CT and ICA in terms of interobserver variability.
Conclusions
In conclusion, the present study demonstrates that 320-row CT may significantly reduce the radiation dose and amount of contrast agent required compared with ICA while maintaining a very high diagnostic accuracy. Thus, 320-row CT constitutes an alternative to other techniques, such as high-pitch helical scanning coupled with reduced tube voltage and prospective ECG gating, that are now available to decrease dramatically radiation exposure during coronary CT. Finally, 320-row CT has the potential to broaden the use of noninvasive angiography to subgroups, such as patients with atrial fibrillation, in whom definition of coronary anatomy has long been limited with older scanners.
References
Miller JM, Rochitte CE, Dewey M et al (2008) Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 359:2324–2336
Meijboom WB, Meijs MF, Schuijf JD et al (2008) Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol 52:2135–2144
Budoff MJ, Dowe D, Jollis JG et al (2008) Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 52:1724–1732
Chow BJ, Freeman MR, Bowen JM et al (2011) Ontario multidetector computed tomographic coronary angiography study: field evaluation of diagnostic accuracy. Arch Intern Med 171:1021–1029
Coles DR, Smail MA, Negus IS et al (2006) Comparison of radiation doses from multislice computed tomography coronary angiography and conventional diagnostic angiography. J Am Coll Cardiol 47:1840–1845
Rybicki FJ, Otero HJ, Steigner ML et al (2008) Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging 24:535–546
Hein PA, Romano VC, Lembcke A, May J, Rogalla P (2009) Initial experience with a chest pain protocol using 320-slice volume MDCT. Eur Radiol 19:1148–1155
Neefjes LA, Dharampal AS, Rossi A et al (2011) Image quality and radiation exposure using different low-dose scan protocols in dual-source CT coronary angiography: randomized study. Radiology 261:779–786
Achenbach S, Goroll T, Seltmann M et al (2011) Detection of coronary artery stenoses by low-dose, prospectively ECG-triggered, high-pitch spiral coronary CT angiography. JACC Cardiovasc Imaging 4:328–337
Hausleiter J, Meyer T, Hermann F et al (2009) Estimated radiation dose associated with cardiac CT angiography. JAMA 301:500–507
Gaudio C, Evangelista A, Pasceri V et al (2011) Visualization of coronary arteries and coronary stents by low dose 320-slice multi-detector computed tomography in a patient with atrial fibrillation. Int J Cardiol 151:e6–e7
Einstein AJ, Henzlova MJ, Rajagopalan S (2007) Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 298:317–323
Bossuyt PM, Reitsma JB, Bruns DE et al (2003) Standards for reporting of diagnostic accuracy. The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Ann Intern Med 138:40–44
Engelken FJ, Lembcke A, Hamm B, Dewey M (2009) Determining optimal acquisition parameters for computed tomography coronary angiography: evaluation of a software-assisted, breathhold exam simulation. Acad Radiol 16:239–243
Dewey M (2008) Examination and reconstruction. In: Dewey M (ed) Coronary CT angiography. Springer, Heidelberg
Weigold WG, Abbara S, Achenbach S et al (2011) Standardized medical terminology for cardiac computed tomography: a report of the society of cardiovascular computed tomography. J Cardiovasc Comput Tomogr 5:136–144
Austen WG, Edwards JE, Frye RL et al (1975) A reporting system on patients evaluated for coronary artery disease: report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 51:5–40
Dewey M, Schnapauff D, Laule M et al (2004) Multislice CT coronary angiography: evaluation of an automatic vessel detection tool. Rofo 176:478–483
Waters D, Lespérance J, Craven TE, Hudon G, Gillam LD (1993) Advantages and limitations of serial coronary arteriography for the assessment of progression and regression of coronary atherosclerosis: implications for clinical trials. Circulation 87(Suppl II):38–47
Reiber JH, Serruys PW, Kooijman CJ et al (1985) Assessment of short-, medium-, and long-term variations in arterial dimensions from computer-assisted quantitation of coronary cineangiograms. Circulation 71:280–288
Lell M, Hinkmann F, Anders K et al (2009) High-pitch electrocardiogram-triggered computed tomography of the chest: initial results. Invest Radiol 44:728–733
Lobotessi H, Karoussou A, Neofotistou V, Louisi A, Tsapaki V (2001) Effective dose to a patient undergoing coronary angiography. Radiat Prot Dosim 94:173–176
Genders TS, Steyerberg EW, Alkadhi H et al (2011) A clinical prediction rule for the diagnosis of coronary artery disease: validation, updating, and extension. Eur Heart J 32:1316–1330
Rawles J, Bignall JC (1986) Regression analysis. Lancet 327:614–615
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet i:307–310
de Graaf FR, Schuijf JD, van Velzen JE et al (2010) Diagnostic accuracy of 320-row multidetector computed tomography coronary angiography in the noninvasive evaluation of significant coronary artery disease. Eur Heart J 31:1908–1915
Dewey M, Zimmermann E, Deissenrieder F et al (2009) Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 120:867–875
Nasis A, Leung MC, Antonis PR et al (2010) Diagnostic accuracy of noninvasive coronary angiography with 320-detector row computed tomography. Am J Cardiol 106:1429–1435
van Velzen JE, de Graaf FR, Kroft LJ et al (2011) Performance and efficacy of 320-row computed tomography coronary angiography in patients presenting with acute chest pain: results from a clinical registry. Int J Cardiovasc Imaging 26:1–12
Zhang C, Zhang Z, Yan Z, Xu L, Yu W, Wang R (2011) 320-row CT coronary angiography: effect of 100-kV tube voltages on image quality, contrast volume, and radiation dose. Int J Cardiovasc Imaging 27:1059–1068
Vanhecke TE, Madder RD, Weber JE, Bielak LF, Peyser PA, Chinnaiyan KM (2011) Development and validation of a predictive screening tool for uninterpretable coronary CT angiography results. Circ Cardiovasc Imaging 4:490–497
Pasricha SS, Nandurkar D, Seneviratne SK et al (2009) Image quality of coronary 320-MDCT in patients with atrial fibrillation: initial experience. Am J Roentgenol 193:1514–1521
Meijboom WB, Mollet NR, Van Mieghem CA et al (2007) 64-slice computed tomography coronary angiography in patients with high, intermediate, or low pretest probability of significant coronary artery disease. J Am Coll Cardiol 50:1469–1475
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article has been retracted at the request of the Editor-in-Chief as it contains large portions of text that have been duplicated from "Noninvasive Coronary Angiography by 320-Row Computed Tomography with Lower Radiation Exposure and Maintained Diagnostic Accuracy. Comparison of Results with Cardiac Catheterization in a Head-to-Head Pilot Investigation" by M. Dewey, E. Zimmermann, F. Deissenrieder, M. Laule, H.-P. Dübel, P. Schlattmann, F. Knebel, W. Rutsch and B. Hamm published online in Circulation: Cardiovascular Imaging on August 24, 2009, DOI 10.1161/CIRCULATIONAHA.109.859280.
An erratum to this article is available at http://dx.doi.org/10.1007/s10554-014-0400-5.
About this article
Cite this article
Pelliccia, F., Pasceri, V., Evangelista, A. et al. RETRACTED ARTICLE: Diagnostic accuracy of 320-row computed tomography as compared with invasive coronary angiography in unselected, consecutive patients with suspected coronary artery disease. Int J Cardiovasc Imaging 29, 443–452 (2013). https://doi.org/10.1007/s10554-012-0095-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-012-0095-4