Abstract
Background
The prognosis of patients with advanced pancreatic cancer is dismal, and there is a need for novel and effective treatments.
Objectives
Tο determine the maximum tolerated dose (MTD) and dose-limiting toxicities (DLTs) of a novel gemcitabine (G) and temsirolimus (T) combination (phase I) and estimate the 6-month progression-free survival (PFS) in patients treated with the T + G combination (phase II).
Patients and Methods
Eligible patients with histologically confirmed inoperable or metastatic pancreatic carcinoma (MPC) were entered into the trial. G was given bi-weekly and T weekly in a 4-week cycle. The first dose level was set at G 800 mg/m2 and T 10 mg. G was escalated in increments of 200 mg/m2 and T in increments of 5 mg until DLT was reached, and the recommended dose was used for the phase II part.
Results
Thirty patients were enrolled in the phase I component at the pre-planned six dose levels; one bilirubin DLT of grade III occurred at the first dose level. The MTD was established as the approved doses of both drugs. Fifty-five patients were entered into the phase II component. Median relative dose intensities administered in the first cycle were 0.75 for T and 0.99 for G. Grade 3-4 hematological toxicities were recorded in 87.3% of patients. The most common non-hematological adverse events were metabolic disorders (81.8%) followed by gastrointestinal disorders (63.6%). Median PFS was 2.69 months (95% CI 1.74-4.95) and median OS was 4.95 months (95% CI 3.54-6.85), while the 6-month PFS rate was 30.9%.
Conclusions
Combination of G and T is feasible in patients with locally advanced or MPC with manageable side effects, but lacks clinical efficacy.
The study was registered in the Australian New Zealand Clinical Trials Registry (ACTRN12611000643976).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gemcitabine and temsirolimus is a feasible combination in patients with advanced pancreatic cancer. | |
The combination has a relatively increased risk of myelosuppression and infection in these patients. | |
While the combination has modest clinical activity in advanced pancreatic cancer patients, further clinical development should be discouraged in view of new available frontline treatment options. |
1 Introduction
Pancreatic cancer is one of the most lethal human diseases. It is the fourth leading cause of cancer-related death among men and women in the United States. Most patients present with advanced disease and their prognosis is dismal [1]. Even for the small percentage of patients who can undergo surgical resection of the primary tumor, the risk for recurrence remains unacceptably high [2]. Current chemotherapy regimens are not very effective and are associated with significant toxicity [3]. Therefore, it is of outmost importance to develop new effective systemic therapies. In the past decade, significant advances in molecular biology have shed more light on the molecular and genetic mechanisms underlying the processes of pancreatic carcinogenesis, invasion, metastasis, and angiogenesis [4].
For many years, gemcitabine was considered the first-line treatment of choice for advanced pancreatic cancer [5]. Very recently, the combination of gemcitabine and nab-paclitaxel has shown incremental benefit in advanced pancreatic adenocarcinomas, compared to gemcitabine alone [6].
Various studies have demonstrated that the phosphatidylinositol 3-kinase (PI3K)-pathway is activated in pancreatic adenocarcinoma and that it is important for the survival, proliferation, and drug resistance of pancreatic cancer cells [7]. Mammalian target of rapamycin (mTOR), one of the main downstream effectors in the PI3K pathway, is also activated in the majority of pancreatic tumors and cell lines [8]. Temsirolimus (T), a selective mTOR inhibitor, has been shown to potently inhibit the proliferation of various pancreatic cancer cell lines in vitro [9]. In addition, temsirolimus showed significant in vivo antitumor activity in pancreatic cancer xenograft models, both as a single agent and in combination with gemictabine [10].
We, therefore, decided to investigate the feasibility and safety of temsirolimus in combination with gemcitabine, one of the most active chemotherapeutic agents in pancreatic carcinoma, in patients with locally advanced or metastatic pancreatic cancer in a non-randomized phase I-II study. The rationale for the combination of these two active drugs is the possible synergy and the known acceptable toxicity of the single agents.
2 Patients and Methods
2.1 Patient Selection
Chemotherapy-naïve, adult patients with a confirmed histological diagnosis of inoperable locally advanced or metastatic pancreatic carcinoma, were included in the current study. All patients had to have a performance status (PS) of 50-100% on the Karnofsky scale and a life expectancy of greater than 12 weeks. Patients should have had measurable or evaluable disease at screening according to Response Evaluation Criteria in Solid Tumors (RECIST) [11]. Adequate hematological function [white blood cell count (WBC) >4000/μL, platelets (PLT) >100,000/μL, and hemoglobin (Hgb) >9.5 g/dL], liver function [total bilirubin level < 2 mg/dL, ALT and AST <2.5 x upper limits of normal (ULN)], and renal function (serum creatinine ≤1.5 mg/dL or calculated creatinine clearance >60 mL/min) were mandatory for study entry. In the presence of liver metastases, transaminase levels could be up to five times the upper limits of normal. Patients should also have had normal cardiac function (left ventricular ejection fraction within institutional normal range) and no serious cardiac illness or medical conditions in the last 6 months. Patients with ampullary, periampullary, bile duct cancers, or endocrine tumors of the pancreas were also excluded. Other major exclusion criteria were any evidence of clinically active interstitial lung disease, pre-existing motor or sensory grade 2 neurotoxicity according to the WHO criteria, history of previous chemotherapy, and known hypersensitivity to gemcitabine. Concomitant use of CYP3A inducers (phenytoin, carbamazepine, rifampicin, barbiturates, or St John’s Wort) had to be avoided and so should treatment with strong CYP3A inhibitors. All female patients of childbearing potential should have had a negative serum or urine pregnancy test obtained within 2 days prior to the initiation of treatment and pregnant or nursing women were excluded.
The clinical protocol was approved by the HeCOG Protocol Review Committee, the Institutional Review Boards of all participating hospitals (initially two institutions during phase I and 12 more during phase II), the National Organization for Medicines and the National Ethics Committee. The study was registered in the Australian New Zealand Clinical Trials Registry (ACTRN12611000643976). Upon participation in the trial, all patients provided a study specific written informed consent and a separate informed consent for providing biological material for future research studies.
2.2 Study Objectives
The primary objective of the phase I part of the study was to determine the feasibility, the maximum tolerated dose (MTD), and the recommended phase II dose of temsirolimus and gemcitabine in patients with advanced pancreatic cancer. The proposed phase II dose would be one step below the MTD. For the phase II part of the study, the primary endpoint was 6-month progression-free survival (PFS) rate, while secondary endpoints included overall survival (OS), safety, and quality of life (QoL) assessments.
2.3 Dosage and Dose Escalation Schema
This was a multi-center, open-label, non-randomized phase I-II trial. Patients with histologically demonstrable advanced pancreatic cancer who met the selection criteria entered the phase I, dose-finding study. Dose escalation followed the established 3 + 3 dose escalation design schema. Patients received treatment consisting of temsirolimus (T, up to 25 mg weekly in a 30 min intravenous infusion, 30 min after premedication with 4 mg of iv dimethindene) followed by infusion of gemcitabine (G, up to 1000 mg/m2 every 2 weeks in a 30 min intravenous infusion).
This rule-based design proceeded with cohorts of three patients. If none of the three patients in a cohort experienced a dose limiting toxicity DLT, another three patients would be treated at the next higher dose level. However, if one of the first three patients experienced a DLT, three more patients would be treated at the same dose level. The dose escalation continued until at least two patients among a cohort of three to six patients experienced a DLT (i.e., ≥33% of patients with a dose-limiting toxicity at that dose level).
The MTD was defined as the preceding dose at which two out of a maximum of six patients experienced a DLT. If a second DLT was observed within the expanded cohort, then the MTD would have been reached. The dose below the MTD level would be the recommended dose for the patients enrolled in the phase II part of the study. Patients who developed a DLT were to be withdrawn from the trial but would be offered the option of continuing treatment at a lower dose, off-protocol, if deemed clinically appropriate. No pharmakokinetic studies were planned, which was a major limitation of the trial.
2.4 Evaluation of Toxicity
Toxicity was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTAE Version 3.0). Complete blood count, biochemical analyses, and clinical toxicity assessments were performed weekly during all treatment courses. Dose escalation and determination of the DLT and MTD were performed on the basis of toxicity occurring during the first cycle of treatment.
DLT was defined as: grade ≥3 non-hematological toxicity, grade 4 thrombocytopenia (platelets <25.000/μL), or grade 4 neutropenia lasting more than 5 days, and inability to receive next scheduled dose due to toxicity (delay >14 days).
2.5 Evaluation of Response
Patients completing at least two cycles of treatment with at least one follow-up tumor assessment were considered evaluable for response. An initial tumor assessment for all patients was performed within 4 weeks prior to treatment initiation and thereafter every two cycles, while on therapy and every 2 months thereafter, until progression of disease. Response was documented using the RECIST 1.1 response criteria for solid tumors. Furthermore, radiological material pertinent for tumor response from 34 patients was assessed centrally by two experienced radiologists (AKF, GP) at the Department of Radiology, AHEPA University Hospital, Thessaloniki, Greece. For characterization of complete response (CR), total disappearance of all measurable and assessable disease was required; for partial response (PR) a > 30% reduction in the size of all measurable lesions was required, as determined by the sum of the largest diameter of measurable lesions. Confirmation of objective responses was required in all cases, at a minimum time interval of 4 weeks. Duration of response was calculated from the time the objective response was documented until disease progression. Stable disease was measured from the date of treatment initiation until the criteria for progression were met, taking the smallest measurements recorded after the initiation of the treatment as a reference.
2.6 Statistical Analysis
The primary endpoint of the Phase II trial was to estimate the 6-month PFS rate. According to the Flemings’s single-stage design assuming that the expected 6-month PFS rate will be at least 30% and the minimum acceptable rate 15%, a total of 53 patients provided 80% power to test this hypothesis, with a two-sided α of 5%. Given a 3% withdrawal rate, 55 patients needed to be enrolled in the phase II part of the study. Secondary endpoints included OS and toxicity profile. Continuous variables were presented as medians with the corresponding range, and categorical variables as frequencies with the respective percentages. OS was measured from the date of acceptance to the date of patient’s death or last contact, while PFS was also measured from the date of patient’s acceptance into the study to documented first progression, death, or last contact, whichever occurred first. The product limit method and Kaplan-Meier curves were used for estimating and plotting time-to-event distributions, while log-rank tests were used for assessing statistically significant differences. Univariate Cox regression was performed to identify significant factors in terms of PFS and OS. All univariate tests were two-sided, and the significance level was set at 5%.
The statistical analysis was performed using the SAS software (SAS for Windows, version 9.3, SAS Institute Inc., Cary, NC, USA).
3 Results
3.1 Patients and Safety
Between May 2009 and October 2014, a total of 85 patients were enrolled into the study. Baseline demographics and disease characteristics for all patients enrolled in the phase I and phase II parts of the study are shown in Table 1.
Thirty patients were enrolled into the phase I part; however, one patient enrolled at the first dose level did not receive treatment and one additional patient was characterized ineligible due to high total bilirubin level. The second patient was a protocol deviation. Three more patients progressed before completing the first cycle and were not eligible for DLT assessment. All of these five patients were substituted.
A total of 120 cycles (median 3; range 1-19) were administered and bilirubin of grade 3 was the only DLT detected in one patient at the first dose level (Table 2). No DLT was observed in the second dose level. In dose level 3, one patient did not complete the first cycle and was substituted. Once again, no DLT was observed. However, as there had been some dose delays beyond the first cycle and several disease related SAEs, we decided to enroll three more patients to get a clearer picture of the toxicity profile of the study. No DLT was seen. In the next dose level (G 800 mg/m2 and T 25 mg), three patients were enrolled and no DLT was observed. Three more patients were thereafter entered into the fifth dose level (G 1000 mg/m2 and T 20 mg) and again no DLT was seen. Finally the last planned dose level opened (G 1000 mg/m2 and T 25 mg) and three patients were entered; no DLT was documented and the phase I study was terminated.
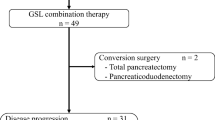
All planned dose levels were completed and an MTD was not achieved. Therefore, dose level 6 of G 1000 mg/m2 and T 25 mg was the recommended dose for the subsequent phase II part of the study. Fifty-five patients were enrolled at eight of the participating centers (Fig. 1). Ten of the 55 patients (18.2%) received more than five cycles of treatment, while only four patients completed seven cycles. The median RDI of T and G in the first cycle was 0.75 and 0.99, respectively. Eighteen patients (32.7%) had the G dose reduced at any point during the study, while the T dose was reduced in only four patients (7.3%) throughout the phase II part of the study.
Most common AEs were similar across the two parts of the study. The most important adverse events and those with incidence greater than 3% of patients for the phase I and phase II part of the study are presented in Supplemental Table 1. All adverse events reported during the phase I and phase II part of the study are depicted in Supplemental Table 2 and Supplemental Table 3, respectively.
In the phase II part, 573 adverse events were reported in 53 of the 55 patients (96.4%). Hematological adverse events were the second most commonly recorded (136 events in 48 patients) and 24.3% of these events were grade 3-4. The most commonly reported non-hematological adverse events were metabolic disorders (218 events in 45 patients) followed by gastrointestinal disorders (70 events in 35 patients). Increased AST, ALT, ALP, blood bilirubin and GTT were observed in 52.7%, 56.4%, 34.5%, 25.5% and 45.5% of the patients, respectively. Twenty-one events of hyperglycemia grade 1-3 were recorded. In addition, diarrhea (13 patients, grade 1-3), nausea (nine patients, eight patients grade 1), vomiting (11 patiens, grade 1-3) and 12 events of mucositis (grade 1-2), were reported. In phase II, 126 events grade 3 and 4 were observed and most of them were metabolic/laboratory events (n = 62, 49.2%), hematological disorders (n = 33, 26.2%), and infections (n = 12, 9.5%).
Thirty-seven serious adverse events were reported throughout the phase II part of the study and five of them had fatal outcome. Three of the fatal events were considered to be related to the study drugs by the investigator and/or sponsor (lung infection, acute massive pulmonary embolism, opportunistic infection/hematoma), but there were also other factors that had contributed to these outcomes, such as diabetes mellitus, hypertension, anemia, and multiple metastases. The most common SAEs were infections (n = 12), thromboembolic events (n = 7), and vomiting (n = 6). Infections mostly involved the respiratory system.
According to the treating physician’s assessment, a definite or (highly) possible/probable causal relationship between the reported adverse event and the study drug(s) was observed for 270 of the 390 adverse events (69.2%) reported throughout the phase I part of the study, while for 111 events there was a doubtful or no causal relationship between the reported adverse event and the study drug(s), and no additional information were available regarding their relationship for 9/ 390 events (2.3%). A total of 28 events were attributed to gemcitabine, 12 events were attributed to temsirolimus, and 230 events to both drugs. Additionally, study disease was the most probable cause for 72 events.
Similarly, a definite or (highly) possible/probable causal relationship between the reported adverse event and the study drug was observed for 267 of the 573 adverse events (46.6%) reported throughout the phase II part of the study. In total, 115 of them (43.1%) were attributed to gemcitabine, 42 were attributed to temsirolimus, and 102 were attributed to both drugs. For eight more events we know that there was a possible relationship between the adverse event and the study drug(s), but we do not have any further information regarding the drug (s) that may have caused the event. In addition, for 276 events (48.2%) there was a doubtful or no causal relationship between the reported adverse event and the study drug(s), while for 189 of them study disease was the most probable cause of the adverse event. It is of note that no information regarding the relationship of the reported adverse event and the study drug(s) was available for 30 of the 573 events (5.2%).
3.2 Efficacy
Fifty-one of the 55 patients (92.7%) discontinued treatment, reasons being disease progression (31 patients; 60.8%), adverse events (12 patients; 23.5%), death (two patients; 3.9%), informed consent withdrawal (five patients; 9.8%), and doctor’s decision (one patient; 2.0%). Among the 55 patients enrolled in the phase II part of the study, twenty-four patients (43.6%) presented with progressive disease, two patients with partial response (3.6%), while stable disease was observed in 30.9% of the study population, as assessed by the investigators at the local hospitals/institutions. Ten patients (18.2%) discontinued treatment prior to tumor evaluation, while for two additional patients (3.6%) tumor assessment was not available at the local institutions, due to early disease progression and death. Central radiological review by RECIST 1.1 criteria was available for 34 patients. Among them, 20 patients (58.8%) had progressive disease, five patients (14.7%) had partial tumor response and nine patients (26.5%) presented with stable disease. A waterfall plot of responses as assessed by central radiology review is presented in Fig. 2. It is of note that 11 of the 55 patients included in the phase II part of the study received second line therapy, while four of them continued to third line treatment and two of them also received fourth line therapy.
At a median follow-up of 69.6 months (95% CI 54.7-84.6), 27 of the Phase I patients were reported dead. One death was caused by toxicity, while the rest were attributed to disease. The median PFS was 3.8 months (95% CI 2.1-4.9). The median OS was 6.1 months (95% CI 4.1-8.9), while 51.7% and 20.7% of the patients survived 6 and 12 months since their acceptance into the study, respectively. Figure 3 presents the Kaplan-Meier plots with respect to PFS and OS for all patients.
In total, 54 deaths (98.2%) were reported among the 55 patients enrolled in the phase II part of the study, while one patient was still alive and on active follow-up at the time of the analysis. Fifty patients (92.6%) died from their disease, while in three patients (5.6%) death was caused by toxicity. It should be mentioned that in one of the three aforementioned patients pancreatic cancer complications also contributed to the fatal outcome. Furthermore, medical history of diabetes mellitus was the most probable reason of death for one additional patient. Median PFS was 2.69 months (95% CI 1.74-4.95), while median OS was 4.95 months (95% CI 3.54-6.85). The 6-month PFS rate was 30.9% and the 12-month OS rate was 23.6%, respectively. Results of the univariate analyses with respect to PFS and OS are presented in Supplemental Table 4 and Supplemental Table 5, respectively.
3.3 Quality of Life Assessment
QoL was assessed using the EUROQOL 5D questionnaire, scheduled for the patients enrolled in the phase II part of the study at screening-baseline, on the day of the administration of cycles 4 and 7, as well as the day of their last treatment cycle. The descriptive system consists of five dimensions including mobility, self-care, usual activities, pain/discomfort and anxiety/depression. The single summary EQ-5D Index was calculated using the European value set. Higher levels of the EQ-5D Index correspond to superior health state levels. In total, 51 patients (92.7%) completed the EQ-5D questionnaire at baseline, while 13 patients completed the questionnaire on their 4th treatment cycle and three patients answered the questionnaire on their 7th cycle of therapy. Thirty patients had the EQ-5D questionnaire completed on the day of their last cycle of treatment. A histogram of the difference of the calculated EQ-5D Index at baseline and at the last treatment cycle was plotted (Supplemental Fig. 1) and the Wilcoxon signed-rank test was used to evaluate baseline and post treatment differences, since they were severely non-normally distributed. Measures of central tendency and dispersion for the calculated EQ-5D Index are presented in Table 3. The mean EQ-5D Index at baseline was 0.67, while at the last treatment cycle, a slight decrease in the mean EQ-5D Index was observed, which was not statistically significant (Wilcoxon signed-rank, p = 0.62).
4 Discussion
For many years, the nucleoside analogue gemcitabine has been the standard therapy for inoperable and metastatic PC, having shown superiority of improved survival and clinical benefit compared to 5-FU [12]. Several combination chemotherapy regimens were associated with increased toxicity but had also failed to demonstrate significant improvement in survival [13, 14]. A recently published meta analysis looking at the outcome of the adittion of a second cytotoxic drug to gemcitabine in this group of patients, showed that gemcitabine combined with either a taxane or an oral fluoropyrimidine improved the disease outcome parameters at the expense of higher toxicities [15].
Furthermore, two recent randomized controlled phase III trials showed that combination chemotherapy with FOLFIRINOX (fluorouracil, leucovorin, irinotecan and oxaliplatin) or gemcitabine plus nab-paclitaxel has led to an improvement in both response rate and survival compared with single agent gemcitabine in patients with good performance status [16, 17]. Neverthless, a noticable proportion of patients with APC are still treated with first-line single agent gencitabine due to poor performance status, liver impairment, and other comorbidities.
Molecular analysis in pancreatic cancer have suggested that the EGFR pathway is playing a significant role in tumorigenesis [18]. The KRAS proto-oncogene is mutated in 90% of pancreatic adenocarcinomas and such mutations in KRAS lead to the continuous activation of downstream intracellular signaling pathways such as RAF/MEK and PI3K/AKT/mTOR. This downstream constitutive activation plays a role in cell growth, proliferation, inhibition of apoptosis, survival, and drug resistance in pancreatic cancer [7] [19]. In addition, the mTOR pathway is involved in the angiogenesis pathway, enhancing endothelial cell growth and proliferation by regulating the production of pro-angiogenic factors [20]. Inhibition of mTOR, therefore, provides a good rationale for exploring in the treatment of APC [21, 22].
To our knowledge this is the first full report with results for an mTOR inhibitor in combination with gemcitabine as front line treatment in advanced pancreatic cancer. However, we acknowledge that the absence of pharmakokinetic data is a major limitation of our study, not allowing for a better interpretation of its results. A similarly designed phase I study by Faris et al. [23] was reported as an abstract only. In this study, the initial dose level of G was at 800 mg/m2 every 2 weeks and T was given as a fixed dose of 10 mg/week. Only nine patients were enrolled at the first dose level and the study was terminated early because of toxicity. Documented toxicities were two episodes of grade 4 neutropenia, and multiple episodes of grade 3 toxicities, including elevated liver function tests, hyperglycemia, hypophosphatemia, diarrhea, and allergic reaction. Coincidentally, nine patients were also enrolled in the first cohort of our study with identical treatment doses of G and T. DLT toxicity was bilirubin grade 3 in one patient and the study moved forward to the next dose level. Unfortunately, the early termination of the study and the fact that the full manuscript has not been published does not allow for further comparisons or reasonable explanations why this schedule was more toxic in this dose level.
Kordes et al. published data on a phase II study of capecitabine and everolimus in patients with APC in the first line setting. Response rate was only 6%, disease control rate was 38% and PFS was 3.6 months. Grade 3 and 4 toxicities reported were hyperglycemia (45%), hand-foot syndrome (16%), diarrhea (6%), and mucositis (3%) [24]. Two other previous studies had explored the role of mTOR inhibitors in gemcitabine-refractory pancreatic cancer. Both treatments, with either everolimus or temsirolimus, failed to demonstrate benefit in the second-line setting [25]. In the phase II part of this study, 34.6% of the patients had stable disease or partial response, while median PFS and OS were 2.69 and 4.95 months, respectively, lower than those observed with gemcitabine monotherapy. Whether the study design, with gemcitabine given every 2 weeks, might have led to such inferior results is an unclear issue.
In contrast to preclinical data, it appears that mTOR inhibitors either as single agents or combinations with chemotherapy drugs do not show promising activity in this disease, while pronounced toxicities have beed documented, leading to significant dose reductions that might have compromised any efficacy. It has also been proposed that there is a negative feedback loop resulting in paradoxical AKT activation secondary to mTOR inhibition [26]. Recent research has shown that clinical development of dual MTORC1/TORC2 inhibitors might confer a better outcome in metastatic PC, but this needs to be confirmed within clinical trials [27].
Gemcitabine given every 2 weeks, combined with weekly temsirolimus, seems to be a reasonably well tolerated regimen with an acceptable toxicity profile. Hematological and liver toxicity was generally higher than commonly seen when both drugs are used as single agents and there is also a higher risk for infection, as expected with mTOR inibitors [28, 29]. Higher incidence of mucositis and hyperglycemia could also have contributed to this risk. One patient developed pneumonia and died from sepsis at the end of the second cycle of treatment in the phase I part of the study. It is unclear whether this infection had developed on the basis of a possible lung toxicity from gemcitabine and thus, no speculation can been made. All other toxicities were modest and resolved quickly.
The events recorded in the phase II part of the study were mostly expected and mild (grade 1-3 events). There were six fatal events and five of them were reported as SAEs. Three of the fatal events were considered to be related to the study drugs by the investigator and/or HeCOG (lung infection, acute massive pulmonary embolism, opportunistic infection/hematoma), but there were also other factors that had contributed to these outcomes. A considerable number of thromboembolic events were recorded and although both study medications could cause such events, pancreatic cancer is a known risk factor for thrombosis, as well as other co-morbidities that the study population suffered from (anemia, hypertension). The incidence of these events in our study was not higher than previously reported in patients with metastatic cancer. A meta analysis by Qi et al., which looked at the impact of mTOR inhibitors on treatment related mortality showed that the use of either temsirolimus or everolimus had increased the risk of fatal adverse events in patients with advanced solid malignancies [30].
In conclusion, outcomes from first-line chemotherapy in advanced pancreatic cancer have clearly been improved over the past 3 years, with the use of more toxic schedules. First-line treatment has moved from single agent gemcitabine to either FOLFIRINOX or a combination of gemcitabine and nab-paclitaxel. Nevertheless, a significant proportion of patients are frail at diagnosis and for such patients, single agent gemcitabine still remains a reasonable option. Combination of gemcitabine and temsirolimus is feasible in patients with inoperable or metastatic pancreatic cancer with manageable side effects However, this is undoubtedly a negative study due to lack of efficacy and early disease progression in the majority of our patients. We feel that this regimen should not be further evaluated, in view also of the shift to the use of gemcitabine and nab-paclitaxel as the new backbone for combination treatments.
References
Bekaii-Saab T, Goldberg R. Therapeutic advances in pancreatic cancer: miles to go before we sleep. J Natl Cancer Inst. 2015;107(2). https://doi.org/10.1093/jnci/dju439.
Enewold L, Harlan LC, Tucker T, McKenzie S. Pancreatic Cancer in the USA: persistence of Undertreatment and poor outcome. J Gastrointest Cancer. 2015;46(1):9–20. https://doi.org/10.1007/s12029-014-9668-x.
Walker EJ, Ko AH. Beyond first-line chemotherapy for advanced pancreatic cancer: an expanding array of therapeutic options? World J Gastroenterol. 2014;20(9):2224–36. https://doi.org/10.3748/wjg.v20.i9.2224.
Hidalgo M. New insights into pancreatic cancer biology. Ann Oncol. 2012;23(Suppl 10):x135–8. https://doi.org/10.1093/annonc/mds313.
Mohammed S, Van Buren G 2nd, Fisher WE. Pancreatic cancer: advances in treatment. World J Gastroenterol. 2014;20(28):9354–60. https://doi.org/10.3748/wjg.v20.i28.9354.
Goldstein D, El-Maraghi RH, Hammel P, Heinemann V, Kunzmann V, Sastre J, et al. Nab-paclitaxel plus gemcitabine for metastatic pancreatic cancer: long-term survival from a phase III trial. J Natl Cancer Inst. 2015;107(2). https://doi.org/10.1093/jnci/dju413.
Ma J, Sawai H, Ochi N, Matsuo Y, Xu D, Yasuda A, et al. PTEN regulates angiogenesis through PI3K/Akt/VEGF signaling pathway in human pancreatic cancer cells. Mol Cell Biochem. 2009;331(1-2):161–71. https://doi.org/10.1007/s11010-009-0154-x.
Kagawa S, Takano S, Yoshitomi H, Kimura F, Satoh M, Shimizu H, et al. Akt/mTOR signaling pathway is crucial for gemcitabine resistance induced by Annexin II in pancreatic cancer cells. J Surg Res. 2012;178(2):758–67. https://doi.org/10.1016/j.jss.2012.05.065.
Azzariti A, Porcelli L, Gatti G, Nicolin A, Paradiso A. Synergic antiproliferative and antiangiogenic effects of EGFR and mTor inhibitors on pancreatic cancer cells. Biochem Pharmacol. 2008;75(5):1035–44. https://doi.org/10.1016/j.bcp.2007.11.018.
Ito D, Fujimoto K, Mori T, Kami K, Koizumi M, Toyoda E, et al. In vivo antitumor effect of the mTOR inhibitor CCI-779 and gemcitabine in xenograft models of human pancreatic cancer. Int J Cancer J Int du Cancer. 2006;118(9):2337–43. https://doi.org/10.1002/ijc.21532.
Tsuchida Y, Therasse P. Response evaluation criteria in solid tumors (RECIST): new guidelines. Med Pediatr Oncol. 2001;37(1):1–3. https://doi.org/10.1002/mpo.1154.
Greenhill C. Pancreatic cancer: gemcitabine confirmed as the first-line therapy for pancreatic cancer. Nat Rev Gastroenterol Hepatol. 2011;8(1):3.
Xie DR, Yang Q, Chen DL, Jiang ZM, Bi ZF, Ma W, et al. Gemcitabine-based cytotoxic doublets chemotherapy for advanced pancreatic cancer: updated subgroup meta-analyses of overall survival. Jpn J Clin Oncol. 2010;40(5):432–41. https://doi.org/10.1093/jjco/hyp198.
Sultana A, Smith CT, Cunningham D, Starling N, Neoptolemos JP, Ghaneh P. Meta-analyses of chemotherapy for locally advanced and metastatic pancreatic cancer. J Clin Oncol. 2007;25(18):2607–15. https://doi.org/10.1200/JCO.2006.09.2551.
Zhang XW, Ma YX, Sun Y, Cao YB, Li Q, Xu CA. Gemcitabine in combination with a second cytotoxic agent in the first-line treatment of locally advanced or metastatic pancreatic Cancer: a systematic review and Meta-analysis. Target Oncol. 2017;12(3):309–21. https://doi.org/10.1007/s11523-017-0486-5.
Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691–703. https://doi.org/10.1056/NEJMoa1304369.
Chen L, Zhang M, Luo S. Outcome of gemcitabine plus molecular targeted agent for treatment of pancreatic cancer: a meta-analysis of prospective phase III studies. Tumour Biol. 2014;35(11):11551–8. https://doi.org/10.1007/s13277-014-2451-6.
Zavoral M, Minarikova P, Zavada F, Salek C, Minarik M. Molecular biology of pancreatic cancer. World J Gastroenterol. 2011;17(24):2897–908. https://doi.org/10.3748/wjg.v17.i24.2897.
Morgensztern D, McLeod HL. PI3K/Akt/mTOR pathway as a target for cancer therapy. Anti-Cancer Drugs. 2005;16(8):797–803.
Karar J, Maity A. PI3K/AKT/mTOR pathway in angiogenesis. Front Mol Neurosci. 2011;4:51. https://doi.org/10.3389/fnmol.2011.00051.
Wolpin BM, Hezel AF, Abrams T, Blaszkowsky LS, Meyerhardt JA, Chan JA, et al. Oral mTOR inhibitor everolimus in patients with gemcitabine-refractory metastatic pancreatic cancer. J Clin Oncol. 2009;27(2):193–8. https://doi.org/10.1200/JCO.2008.18.9514.
Iriana S, Ahmed S, Gong J, Annamalai AA, Tuli R, Hendifar AE. Targeting mTOR in pancreatic ductal adenocarcinoma. Front Oncol. 2016;6:99. https://doi.org/10.3389/fonc.2016.00099.
Faris JE, Blaszkowsky LS, Abrams TA, Enzinger PC, Hezel AF, Wolpin BM, et al. A phase I study of temsirolimus in combination with gemcitabine in previously untreated metastatic pancreatic cancer. J Clin Oncol. 2012;30(4_suppl):296.
Kordes S, Klumpen HJ, Weterman MJ, Schellens JH, Richel DJ, Wilmink JW. Phase II study of capecitabine and the oral mTOR inhibitor everolimus in patients with advanced pancreatic cancer. Cancer Chemother Pharmacol. 2015;75(6):1135–41. https://doi.org/10.1007/s00280-015-2730-y.
Garrido-Laguna I, Tan AC, Uson M, Angenendt M, Ma WW, Villaroel MC, et al. Integrated preclinical and clinical development of mTOR inhibitors in pancreatic cancer. Br J Cancer. 2010;103(5):649–55. https://doi.org/10.1038/sj.bjc.6605819.
Soares HP, Ni Y, Kisfalvi K, Sinnett-Smith J, Rozengurt E. Different patterns of Akt and ERK feedback activation in response to rapamycin, active-site mTOR inhibitors and metformin in pancreatic cancer cells. PLoS One. 2013;8(2):e57289. https://doi.org/10.1371/journal.pone.0057289.
Hassan Z, Schneeweis C, Wirth M, Veltkamp C, Dantes Z, Feuerecker B, et al. MTOR inhibitor-based combination therapies for pancreatic cancer. Br J Cancer. 2018;118(3):366–77. https://doi.org/10.1038/bjc.2017.421.
Liu GF, Li GJ, Zhao H. Efficacy and toxicity of different chemotherapy regimens in the treatment of advanced or metastatic pancreatic Cancer: a network Meta-analysis. J Cell Biochem. 2018;119(1):511–23. https://doi.org/10.1002/jcb.26210.
Xu J, Tian D. Hematologic toxicities associated with mTOR inhibitors temsirolimus and everolimus in cancer patients: a systematic review and meta-analysis. Curr Med Res Opin. 2014;30(1):67–74. https://doi.org/10.1185/03007995.2013.844116.
Qi WX, Huang YJ, Yao Y, Shen Z, Min DL. Incidence and risk of treatment-related mortality with mTOR inhibitors everolimus and temsirolimus in cancer patients: a meta-analysis. PLoS One. 2013;8(6):e65166. https://doi.org/10.1371/journal.pone.0065166.
Acknowledgements
The authors are indebted to all patients and their families for their trust and participation in the HE3/07 trial as well as for the provision of biological material for research purposes. The authors wish to thank Dimitra Katsala for monitoring the study and Maria Moschoni for data coordination.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by Pfizer Inc., by an internal Hellenic Cooperative Oncology Group (HeCOG) translational research grant (HE_R3/07) and by a Hellenic Study Group for Metastatic Liver Disease grant.
Conflict of Interest
Vasilios Karavasilis is a member of the Advisory Boards of Amgen, Pfizer, Novartis, BI, Lilly, Astellas, Genesis-Pharma, and Janssen. Epaminontas Samantas is a member of the Advisory Boards of Merck, MSD, AstaZeneca, Roche, Amgen, and Genesis. George Pentheroudakis is a member of the Advisory Boards of Roche, he has received Honoraria from Roche, he has participated in a Speakers bureau of Roche and he has received grant from Amgen. George Fountzilas ia a member of the Advisory Boards of Pfizer, Sanofi and Roche and he has received Honoraria from AstraZeneca. Georgia-Angeliki Koliou, Anna Kalogera-Fountzila, Ioannis Varthalitis, Helena Linardou, Grigorios Rallis, Maria Skondra, Georgios Papadopoulos, George Papatsibas, Joseph Sgouros, Athina Goudopoulou, Konstantine T. Kalogeras, Christos Dervenis, and Dimitrios Pectasides declare that they have no conflicts of interest that might be relevant to the contents of this manuscript.
Electronic Supplementary Material
ESM 1
(PDF 394 kb)
Rights and permissions
About this article
Cite this article
Karavasilis, V., Samantas, E., Koliou, GA. et al. Gemcitabine Combined with the mTOR Inhibitor Temsirolimus in Patients with Locally Advanced or Metastatic Pancreatic Cancer. A Hellenic Cooperative Oncology Group Phase I/II Study. Targ Oncol 13, 715–724 (2018). https://doi.org/10.1007/s11523-018-0605-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-018-0605-y