Abstract
The aim of the study was to realize a mathematical model of insulin–glucose relationship in type I diabetes and test its effectiveness for the design of control algorithms in external artificial pancreas. A new mathematical model, divided into glucose and insulin sub-models, was developed from the so-called “minimal model”. The key feature is the representation of insulin sensitivity so as to permit the personalisation of the parameters. Real-time applications are based on an insulin standardised model. Clinical data were used to estimate model parameters. Root mean square error between simulated and real blood glucose profiles (Grms) was used to evaluate system efficacy. Results from parameter estimation and insulin standardisation showed a good capability of the model to identify individual characteristics. Simulation results with a Grms 1.30 mmol/l in the worst case testified the capacity of the model to accurately represent glucose–insulin relationship in type 1 diabetes allowing self tuning in real time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
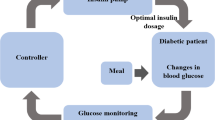
The insulin therapy optimisation for type 1 diabetic patients can significantly improve their quality of life and life expectancy [29]. Therefore, since the early 1970s, an external device capable of tuning insulin infusion to blood glucose changes was the objective of many studies [1, 21]. Research in this field has always been model-based and has moved from the development of the structure of a model of glucose and insulin dynamics stepping towards model parameter estimation and model personalisation to each single patient’s requirements. The models thus represented a platform for the development of insulin control strategies [2] and a tool for their preliminary testing. The Biostator [7] is probably the most important example of bedside extracorporeal artificial pancreas which was developed almost 30 years ago and is still used for research purposes [13, 19, 20]. Its control algorithms were based on intravenous glucose sampling and intravenous insulin infusion. The shift towards the subcutaneous route is still in progress [10, 11, 17, 22, 25, 33, 31], because whilst subcutaneous insulin infusion pumps and rapid acting insulin analogues are a well established reality, stable and reliable subcutaneous glucose sensors that can finely and safely detect blood glucose oscillations and drive insulin feedback are not yet available [6]. In fact, the subcutaneous sensors obtainable from the market [14] have many limitations that are not compatible with the strict requirements of control algorithms. In this context, the study of our mathematical model aimed at realising the basis for a future external wearable artificial pancreas intended as a closed loop system using the subcutaneous route. Model structure and parameter estimation were tailored towards the further development of control algorithms capable of maintaining euglycaemia in type 1 diabetics, adjusting the insulin dose in real time by continuous subcutaneous insulin infusion (CSII). The main objective was the production of a reliable model representing a “virtual patient” that may allow the assessment of different control strategies. But on the other hand, it was clear that the main key to producing an effective insulin infusion control is the capability of the model to represent the single patient (personalisation) following real time changes of the patient’s physiological responses.
Consequently the structure of the model and its estimated parameters must meet the time requirements imposed by this primary real time personalisation task.
The aim of the present study was the realisation of a model complex enough to give a close representation of glucose metabolism pathways but none the less capable of real time parameter estimation in order to achieve fine tuning of safe insulin infusion. The model has been developed on the basis of the so-called minimal model (MM), proposed for healthy subjects by R.N. Bergman and C. Cobelli in the late 1970s [5, 8], which is characterized by a bi-linear description of the insulin-dependent glucose metabolism. The model has been modified to represent type 1 diabetic patients under continuous insulin infusion and external inputs such as meals and glucose boles. Its parameters have been estimated and its accuracy validated by simulations run on data collected during a clinical experiment.
2 Materials and methods
2.1 Mathematical model
The feedback control must face the changes in patient sensitivity to exogenous insulin, which occur both daily (the well-known circadian variation of insulin sensitivity) and in the long term. The controller must meet the requirements of self-tuning, i.e. its parameters must change as a function of the specific patient response. The key for tuning the controller parameters resides in the model of insulin and glucose dynamics and kinetics included in the controller. Moreover, the same insulin–glucose model represents a tool for investigating a feasible structure of the controller itself, and the dependence of its parameters on the main features of insulin dynamics and insulin-dependent glucose metabolism.
In order to be used as the kernel of the self-tuning controller, the model must fulfil the main requirement of on-line identification on the basis of easily and promptly measurable biological quantities. Two biological variables of interest are easily accessible during the patient’s normal life: blood glucose and plasma insulin concentrations. Whilst glucose concentration is easily measured by precise and stable—even if not yet available for implantation—electrochemical sensors, evaluation of insulin concentration at present requires lengthy laboratory analyses that make it useless for feedback control. Therefore, control action must be performed on the basis of glucose values only, whilst the whole insulin dynamics, from its administration site to the sites of glucose metabolism, hepatic release, etc. must be represented by a model that standardises individual behaviour.
Another important issue is the time required for model identification, because it affects promptness and accuracy of the control action. It increases almost exponentially with the number of estimated parameters which, consequently, should be minimized. On the contrary, a negligible time expenditure, is needed for microprocessor units (even implanted) to perform the large number of algebraic and logical operations required by a fairly complex model. Therefore, the model structure should be as refined as possible, to accurately reproduce the biological process in spite of the reduced number of parameters characterizing the patient’s individual response. An adequate set of experimental data is then required to test model accurateness.
The MM describes the glucose metabolism as proportional to the product of glucose and insulin concentrations, thus depending on only one coefficient of “insulin sensitivity” subjected to estimation. MM has been developed and tested on healthy subjects, whose insulin is released by pancreas depending on the actual blood glucose concentration. MM was modified to represent insulin-dependent diabetic patients mainly substituting pancreatic release of endogenous insulin with exogenous insulin administration. Renal clearance, a glucose homeostasis feature peculiar in type 1 diabetes, was included in the glucose balance. The need to simulate food assumption and consequently hepatic balance, led to the introduction of corresponding submodels.
The complete model block diagram (Fig. 1) shows the two main subsystems representing, as in the MM, insulin and glucose dynamics. The insulin block receives the externally administrated insulin, and generates the insulin concentrations acting at the interstitial and hepatic levels. The glucose block receives the glucose contribution from food ingestion, and includes liver uptake and release, insulin-independent metabolism and renal clearance. Moreover, a second interstitial compartment was integrated into the description of glucose metabolism following Regitting et al. [23], where insulin-dependent glucose metabolism is still represented by a bi-linear term, as in the MM. A third algebraic block was then added, representing liver glucose uptake and release and connected to the representation of food assumption.
Model equations are described below. Their variables are listed in Table 1, and parameter meaning and values in Table 2.
2.1.1 Insulin sub-model
The original MM of insulin kinetics includes a plasma compartment (Eq. 1) and a remote one (Eq. 2). We chose to maintain the inherited presence of a “black box” compartment such as the remote one because it gives the opportunity of taking into account some complex phenomena that cause a reduction of the amount of glucose available without increasing the modelling burden. This is the case of the synthesis of proteoglycans which has a diffused biological impact [27, 30, 34] and is responsible for the rate of endothelial glucose uptake. We decided to put this process in the remote “black box” area and to consider the global rate of glucose somehow metabolized while avoiding detailed investigation. The present insulin sub-model is obtained from MM by suppressing therein the input of endogenous insulin, and including the external inputs V iv (μU/h) of exogenous insulin directly administrated in vein and S (μU/h) of insulin coming from subcutaneous administration:
where I (μU/ml) is the plasma insulin concentration and X (μU/ml) the equivalent concentration in the remote compartment: only I is measurable. V iv is the rate of appearance in plasma of insulin administrated by continuous infusion or by boles.
The input S, i.e. the rate of appearance in plasma of insulin coming from subcutaneous administration, is generated by a third equation, which has been added to the previous ones to describe a subcutaneous compartment:
where V sc (μU/h) is the rate of subcutaneous administration (infusion or bolus) and S (μU/h) the release rate to plasma compartment. Therefore, two insulin inputs are available, subcutaneous V sc and intravenous V iv.
Txi (h), Tm (h) and Ti (h) are time constants related to insulin diffusion through the three compartments. The constant Ti of diffusion in the subcutaneous compartment is not identifiable because the variable X (the equivalent insulin concentration in the remote compartment, μU/ml) is not measurable; it has a value (Table 2) obtained from literature and depending on the insulin type [15, 16, 18]. The constants of diffusion in the plasma and remote compartments, Txi and Tm (whose reciprocals are both dominant poles of the insulin sub-model), as well as the gain constant Ki (ml/h), which is related to the plasma distribution volume, are estimated to determine the insulin model. The whole model is shown in Fig. 2.
2.1.2 Glucose sub-model
The original MM includes only one blood glucose compartment. One more interstitial compartment was added here, following Regitting at al. [23], where insulin-dependent glucose metabolism takes place according to the bi-linear rule of MM. Five more terms have been inserted in the blood compartment equation (Eq. 4), to refine the overall description: a constant M i (h) describing the insulin-independent metabolism; two input variables E g (mmol/h) and E b(mmol/h), whose generation will be described in the following sections, accounting for the glucose contributions, respectively, from ingested food and from hepatic release; the external input G iv (mmol/h), from intravenous glucose administration (as in intravenous glucose tolerance tests, IVGTT), and, finally, the glucose subtraction E r (mmol/h) by renal clearance. Therefore, the equations are:
G (mmol/h) and Y (mmol/l) are glucose concentrations, both measurable depending on the glucose sensor type and location. The term G/Tyg − Y/Tgy describes the exchanges between compartments; the values of Vg (distribution volume of blood glucose compartment, 9.91 l), Kyg (rate between the distribution volume 0.952), Tyg (=0.194 h) and Tgy (=0.194 h) are obtained by a best-fit of the experimental responses of Regitting at al. [23]. The insulin sensitivity coefficient Kis (ml/μU/h), in Eq. 5, rules the glucose metabolism according to a bi-linear law which, as already stated, is the main assumption of MM. The non-dimensional coefficient Pcirc allows the description of circadian sensitivity variation, assumed to be sinusoidal:
The values of K is and, if necessary, of the amplitude A c and phase P c of the circadian rhythm are estimated, and characterize the model of the individual subject. It should be borne in mind that the amplitude A c has some meaning only if the set of experimental values covers a reasonable length of time, i.e. it includes the times of minimum and maximum sensitivity; in that case, it is bound to 1 as K is cannot become negative; moreover, no circadian variation should be computed if the model is inserted in a self-tuning controller, where K is is evaluated on-line at a frequency much higher than the circadian rhythm: in that case Pcirc=1. After computing P c, also the time of minimum insulin sensitivity can be determined off-line:
where t ini (h) is the starting time of the experiment.
The renal clearance in hyperglycemic conditions is described by a non-linear feedback loop:
Numerical coefficients have been chosen so as to reproduce the well-known mean course of renal clearance [26]. The whole model is shown in Fig.3.
2.1.3 Food intake
The variable E g (mmol/h), describing glucose input from meals, is obtained by processing a time dependent input representing the rate of food intake. According to Arleth et al. [3, 4], gut absorption is split in three terms, each one corresponding to a class of carbohydrates with different absorption rates: sugar A g (mmol/h), fast absorption starch A s (mmol/h), and slow absorption starch A m (mmol/h), as derived from mixed meals, where the presence of different nutrients slows down the absorption of carbohydrates:
where A g, A s and A m are obtained by filtering the ingestion rate R i by appropriate transfer functions, which were obtained by numerical fitting of the results of Arleth et al. [3]:
where F s is the fraction of starch (and, therefore, 1−F s the fraction of sugar) and F m is the fraction of mixed meal in the total amount of starch. An oral glucose tolerance test (OGTT) is easily represented by a meal of pure sugar, i.e. by putting F s=0.
2.1.4 Hepatic balance
The need to handle food input also requires the representation of liver uptake and release, which play a considerable role in post-prandial glucose homeostasis. A non linear block describes the hepatic balance taking into account glycogenosynthesis, glycogen storage and hepatic release due to glycogenolysis [9, 12, 24] and gluconeogenesis [32], as depending on blood glucose, plasma insulin and gut absorption rate:
where Q r (mmol/h) describes the glucose release:
and Q c (mmol/h) the uptake:
The equation structure, and coefficient values, have been obtained by fitting several average responses reported in [9, 12, 24, 32].
2.2 Clinical data set
Parameters T xi, T m (time constants of insulin diffusion in plasma and remote compartments), K i (constant related to plasma insulin distribution volume, ml/h), K is (sensitivity coefficient in the insulin-dependent glucose metabolism, ml/μU/min) and P c (phase of circadian rhythm) were estimated on the basis of data collected during a 10 h clinical trial on six type 1 diabetic patients (identified according to the WHO criteria) on continuous subcutaneous insulin infusion therapy (CSII) with lispro insulin. All patients had a diabetes history of at least 5 years, were C-peptide negative, and were treated with CSII for at least 6 months before the study. The study was conducted in the outpatient metabolic research unit of the Department of Internal Medicine (DIMI) of Perugia University (Perugia, Italy). Patients arrived at the Hospital at 7:30 a.m. after an overnight fast; during the following 30 min the insulin infusion rate was kept constant. The experiment included two phases, lasting 4 and 6 h, respectively: an infusion suppression phase, used for estimation of T xi (time constant of insulin diffusion in plasma compartment, h), and a recovery phase. The remaining parameters have been estimated on the whole 10 h trial. At 8:00 a.m., starting time of the suppression phase, the CSII was interrupted; at noon it was re-established, a s.c. bolus was administered according to the level of metabolic deterioration and a standard meal (40 g of carbohydrates) was given. The bolus was followed by the reprise of the usual basal insulin infusion. Insulin infusion rate was changed every 30 min during the recovery phase; blood glucose samples were collected every 30 min, plasma insulin every hour. The study ended at 6.00 p.m. after 6 h of recovery.
2.3 Estimation procedure
2.3.1 Insulin sub-model
In order to estimate T xi (time constants of insulin diffusion in remote compartment, h), an explicit model has been deduced from the implicit one of Eqs. 1 and 2. During the suppression phase, the insulin subsystem is not fed by any input, and, therefore, the output of the plasma insulin block evolves in free response bi-exponentially with the time constants T i of the subcutaneous compartment (T i=0.152 h for lispro insulin) and T xi of the plasma compartment. If, as in our case, the infusion rate has been kept constant for at least 15 min before stopping, plasma insulin is given thereafter by:
where I 0 is the initial value, which is also estimated. Estimation was performed by minimizing the RMS error Err between computed and experimental values.
The constant K i, which does not appear in Eq. 16, was then determined by minimizing the RMS error, I rms, between computed and experimental plasma insulin values, on the whole experiment time. Finally, the third time constant T m of insulin sub-model was estimated, together with the main parameter K is of the glucose sub-model, by minimizing the glucose RMS error, G rms.
2.3.2 Glucose sub-model
The insulin sensitivity coefficient of glucose metabolism K is (ml/μU/min), and the circadian variation parameters, A c and M c were computed (together with the remaining time constant T m of the insulin sub-model) on the 10 h glucose response of the model, equipped with the previously computed values of T xi and K i. Estimated and experimental glucose profiles were compared to assess the quality of estimation, the RMS error G rms between real data and simulated blood glucose values was chosen as quality index.
The model was programmed in Matlab 6 language and Simulink 3 graphic toolbox and simulated on personal computers. All values were estimated by a simplex algorithm (Matlab Fminsearch function), which has also been used for the best-fit of literature data on glucose exchanges between compartments, renal clearance, gut absorption and hepatic balance.
3 Results
3.1 Parameter estimation
Three different methods were considered to estimate the unknown model parameters:
-
1.
All parameters were estimated patient by patient, their mean values were then computed (Table 3);
-
2.
A unique value of T xi, (time constant of insulin diffusion in plasma compartment, h), was evaluated for the whole group of patients on the set of the 6×5 insulin values during the suppression phase; then K i (constant related to the plasma insulin distribution volume, ml/h) and all the remaining parameters were estimated for each individual patient;
-
3.
After evaluating T xi and K i as in (2), the remaining individual parameters were computed by using the mean value K i=0.0101 ml/h in place of its individual values (Table 4).
Two ways were tested for evaluating T xi in cases (2) and (3): estimating individual values for each patient, as in case (1), and computing the mean T xi=3.96 h of the 6 estimated values; or directly computing T xi=1.81 h on the whole set of 30 experimental values, after normalizing each individual data series with respect to its mean. The second way was preferred as it produced a lower mean value of the root mean square error I rms between experimental and simulated plasma insulin profiles (4.15±1.17 μU/ml, mean ± SD, vs. 4.72±1.24 μU/ml) while estimating K i, with equal values of the root mean square error G rms between measured and simulated blood glucose profiles.
Method (1), i.e. individual estimation of all parameters, was implemented only for comparison with the remaining ones, as it requires evaluation of insulin concentration case by case and, therefore, is useless for on-line application; moreover, it produces the highest RMS error in the estimation of the glucose parameters (G rms=1.03 mmol/l). Both methods (2) and (3) produced the same glucose error, G rms=0.88 mmol/l, and the third one was preferred as it does not involve case-by-case computation of K i from the insulin values. Tables 3 and 4 also include phase P c of circadian rhythm and time M c of minimum C s off-line computed by Eq. 7.
3.2 Standard insulin model
As seen above, standard values of T xi (time constant of insulin diffusion in plasma compartment, h) and K i (constant related to the plasma insulin distribution volume, ml/h) are required for on-line use of the model, while T m (time constant of insulin diffusion in remote compartment, h) could be estimated, together with K is (sensitivity coefficient ml/μU/min), on the glucose response. Nevertheless, using the mean value T m=2.45 h resulting from Table 4 reduces the burden of on-line computation of two parameters on the basis of the measurement of glucose only, and avoids its loss of accuracy. Therefore, a standard model of insulin kinetics has been characterized by the estimated T xi and the mean values of K i and T m, i.e. T xi=1.81 h, K i=0.0101 ml/h, T m=2.45 h. Such values were used to compute once again the parameters of the glucose sub-model: they are listed in Table 5; the mean insulin sensitivity is K is=0.0481 ml/μU/h. Parameters of circadian variation have also been computed: Table 5 lists, as Tables 3 and 4, phase P c as well as the time of minimum insulin sensitivity. Tables 3, 4 and 5 do not list the estimated values of the amplitude A c as they are meaningless, because the times of minimum and maximum insulin sensitivity are outside the experimental interval (sometimes A c was larger than 1). Figure 4 shows the glucose courses, compared with the simulated responses, of two cases, no.1 with the lowest G rms (0.66 mmol/l) and no.2 with the highest one (1.33 mmol/l).
4 Discussion and conclusions
The present study proposes a mathematical model of insulin and glucose metabolism in type I diabetes which is, first of all, a very easy-to-handle tool, with personalization facilities that allow a quick estimation of its parameters (K is and, if necessary, M c and A c) based only on the blood glucose response of the individual patient. The Simulink structure increases the user-friendliness of the model without affecting the computer performance over time.
Estimation results
The graphs of Fig. 4 show that the model, equipped with the standard insulin parameters, seem capable of producing a satisfactory approximation even in the worst case, where the RMS error G rms between measured and simulated blood glucose profiles is 1.33 mmol/l.
Standard insulin model
Comparison between Tables 3 and 5 show that the use of the standard insulin model does not appreciably affect the accuracy of representation, as measured by glucose RMS error G rms: the use of the standard value of T m, time constant of insulin diffusion in remote insulin compartment, in place of its value estimated case by case, slightly reduces the accuracy (G rms=0.94 vs 0.91 mmol/l). The individual values of the insulin sensitivity are rather different, but their mean values are almost indistinguishable (K is=0.0481±0.0189 vs 0.0441±0.0188 ml/μU/min, mean ± SD). The same is valid even for case (1) (K is=0.0426±0.0214 ml/μU/min). Therefore, the standard insulin model that makes possible the on-line tuning of the model can be assumed as a mean representation of the insulin kinetics, robust enough to be used for different subjects. As a consequence, it can be adopted for developing self-adaptive control algorithms based on on-line model tuning. This inference is also supported by the fact that the mean value of T m is indistinguishable from the corresponding parameter of MM (1.52 h). In other words, the diffusion through compartments of exogenous insulin in diabetics looks quite similar to that of endogenous insulin in healthy subjects.
Circadian rhythm
The values of M c, time of minimum insulin sensitivity, cannot be assumed as being quantitative evaluations of patients’ circadian rhythm, as the experiment time covers only the ascending segment of the sinusoid of Eq. 6; but their mean values, all situated around 6 a.m., are in accordance with the well-known dawn phenomenon [28]. Anyway, they indicate at least a general increase of sensitivity with time, which is more relevant during the first part of the experiment, in accordance with the physiological knowledge.
Virtual patient
The set of Eqs. 1, 2, 3, 4, 5 (with P circ=1) and 8, 9, 10, 11, 12, 13, 14 and 15, once equipped with the standard insulin coefficients of Table 4, and the mean K is value of Table 5, fully characterizes a “virtual patient”, which is a useful tool for first approximation theoretical studies on the structure of a feedback controller. Moreover, variation ranges of the controller parameters can be argued to depend on the range of K is values. The control algorithm could be designed on such a virtual patient resulting from the average values of the estimated parameters for the cluster of patients. This operation will represent a further error filter. Introducing the standard values of insulin model also improves the estimation quality by filtering insulin measurement noise.
Closed loop system
A closed loop external artificial pancreas would basically constitute: (1) a glucose sensor, (2) a micro-controller equipped with a mathematical algorithm able to control insulin infusion as a function of the measured glucose values, and (3) an insulin infusion pump. At present two major obstacles impair the realization of a fully automated artificial pancreas usable in daily life: implanted sensors cannot yet be considered sufficiently reliable for securing the quality of continuous glucose monitoring required to close the loop, and studies on control algorithms are still in progress towards satisfactory results. This mathematical model was conceived with the global aim of making a step towards the realization of a closed loop artificial pancreas. From this general purpose spring two immediate and connected objectives. The model must support studies for the development of control algorithms and must be a tool for their testing, either by simulation or during clinical trials. The capability of the model to be effective in the development of control algorithms is related to its accuracy in representing a diabetic subject. The results in terms of the main accuracy index (G rms) seem to ensure a suitable closeness between real and simulated data but it has to be said that only successive studies on algorithms will finally testify that this range provides the adequate accuracy of diabetes pathophysiology representation and the filtering of measurement artefacts.
Conclusion
At the state of the art of the present study we can conclude that a useful tool has been developed for the purpose of further simulation studies on glucose feedback control algorithms. The model is an adequate representation of diabetic subjects. Technical characteristics of the model ensure that it can be used during a clinical trial on real patients, where the model can work on-line as a virtual interface, representing a particular patient, towards other devices. The model of a virtual patient then gives the possibility of testing control algorithms before applying them to people, improving the expectations and reducing the risk of experimental activities on real patients.
References
Albisser AM, Leibel BS, Ewart TG, Davidovac Z, Botz CK, Zingg W (1974) An artificial endocrine pancreas. Diabetes 23:389–404
Albisser AM, Schiffrin A, Schulz M, Tiran J, Leibel BS (1986) Insulin dosage adjustment using manual methods and computer algorithms: a comparative study. Med Biol Eng Comput 24(6):577–584
Arleth T, Andreassen S, Orsini Federici M, Massi Benedetti M (2000) A model of the endogenous glucose balance incorporating the characteristics of glucose transporters. Comput Methods Programs Biomed 62(3):219–234
Arleth T, Andreassen S, Orsini-Federici M, Timi A, Massi-Benedetti M (2000) A model of glucose absorption from mixed meals. In: IFAC proceedings. Karlsburg/Greifswald, Germany, pp 331–336
Bergman RN, Cobelli C (1981) Physiological evaluation of factors controlling glucose tolerance in men: measurement of insulin sensitivity and beta-cell glucose sensitivity from the response to intravenous glucose. J Clin Invest 68:1456–1467
Brunetti P, Orsini Federici M, Massi Benedetti M (2003) The artificial pancreas. Artif Cells Blood Substit Immobil Biotechnol 31(2):127–138
ClemensAH, Chung PH, Myers RW (1977) Development of biostator, a glucose controlled insulin infusion system (GCIIS). Horm Metab Res Suppl 7:23–33
Cobelli C, Toffolo G (1984) A model of glucose kinetics and their control by insulin, compartmental and non-compartmental approaches. Math Biosci 72:291–235
Defronzo RA, Ferrannini E, Hendler R, Felig P, Wahren J (1983) Regulation of splanchnic and peripheral glucose uptake by insulin and hyperglycemia in man. Diabetes 32:32–35
Fabietti PG, Massi Benedetti M, Bronzo F, Reboldi GP, Sarti E, Brunetti P (1991) Wearable system for acquisition, processing and storage of the signal from amperometric glucose sensors. Int J Artif Org 14(3):175–178
Fabietti PG, Calabrese G, Iorio M, Bistoni S, Brunetti P, Sarti E, Benedetti MM (2001) A mathematical model describing the glycemic response of diabetic patients to meal and i.v. infusion of insulin. Int J Artif Org 24(10):736–742
Ferrannini E, Defronzo RA (1997) Insulin actions in vivo: glucose metabolism. In: International textbook of diabetes mellitus, vol 1. Wiley, New York, pp 505–530
Heinemann L, Ampudia-Blasco FJ (1994) Glucose clamps with the Biostator: a critical reappraisal. Horm Metab Res 26(12):579–583
Heinemann L, Koschinsky T (2002) Continuous glucose monitoring: an overview of today’s technologies and their clinical applications. Int J Clin Pract Suppl 129:75–79
Heinemann L, Chantelau EA, Starke AA (1992) Pharmacokinetics and pharmacodynamics of subcutaneously administered U40 and U100 formulations of regular human insulin. Diab Metab 18:21–24
Hoffman A, Ziv E (1997) Pharmacokinetic considerations of new insulin formulations and routes of administration. Clin Pharmacokinet 33(4):285–301
Hovorka R, Chassin LJ, Wilinska ME, Canonico V, Akwi JA, Orsini Federici M, Massi-Benedetti M, Hutzli I, Zaugg C, Kaufmann H, Both M, Vering T, Schaller HC, Schaupp L, Bodenlenz M, Pieber TR (2004) Closing the loop: the adicol experience. Diab Technol Ther 6(3):307–318
Lindholm A, Jacobsen LV (2001) Clinical pharmacokinetics and pharmacodynamics of insulin aspart. Clin Pharmacokinet 40(9):641–659
Massi Benedetti M, Noy G, Johnston IDA, Worth R, Alberti KGMM (1981) Glucose controlled insulin infusion system (Biostator) application during surgery for a presumed pancreatic microinsulinoma. Diab Metab 7:41–44
Massi Benedetti M, Home PD, Gill GV, Burrin JM, Noy GA, Alberti KGMM (1987) Hormonal and metabolic responses in brittle diabetic patients during feedback intravenous insulin infusion. Diab Res Clin Pract 3:307–317
Pfeiffer EF, Thum C, Clemens AH (1974) The artificial beta cell—a continuous control of blood sugar by external regulation of insulin infusion (glucose controlled insulin infusion system). Horm Metab Res 6:339–342
Pickup J, Mccartney L, Rolinski O, Birch D (1999) In vivo glucose sensing for diabetes management: progress towards non-invasive monitoring. BMJ 319(7220):1289–1295
Regitting W, Trajanoski Z, Leis HJ, Ellmerer M, Wutte A, Sendlhofer G, Schaupp L, Brunner GA, Wach P, Pieber TR (1999) Plasma and interstitial glucose dynamics after intravenous glucose injection. Evaluation of the single-compartment glucose distribution assumption in the minimal models. Diabetes 48:1070–1081
Rizza R (1996) The role of splanchnic glucose appearance in determining carbohydrates tolerance. Diab Med 13:S23–S27
Shichiri M, Kawamori R, Yamasaki Y, Hakui N, Abe H (1982) Wearable artificial endocrine pancreas with needle-type glucose sensor. Lancet 2:1129–1131
Silverman M, Turner RJ (1992) Renal physiology. In handbook of physiology. Oxford University Press, Oxford, pp 2017–2038
Small DH, Mok SS, Williamson TG, Nurcombe V (1996) Role of proteoglycans in neural development, regeneration, and the aging brain. J Neurochem 67:889–899
Stephenson JM, Schernthaner G (1989) Dawn phenomenon and Somogyi effect in IDDM. Diab Care 12(4):245–251
The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986
Van Den Berg BM, Vink H, Spaan JA (2003) The endothelial glycocalyx protects against myocardial edema. Circ Res 92(6):592–594
Wach P, Trajanoski Z, Kotanko P, Skrabal F (1995) Numerical approximation of mathematical model for absorption of subcutaneously injected insulin. Med Biol Eng Comput 33(1):18–23
Wise S, Nielsen M, Rizza R (1997) Effects of hepatic glycogen content on hepatic insulin action in humans: alteration in the relative contribution of glycogenolysis and gluconeogenesis to endogenous glucose production. J Clin Endocrinol Metab 82(6):1828–1833
Yamaguchi M, Kawabata Y, Kambe S, Wardell K, Nystrom FH, Naitoh K, Yoshida H (2004) Non-invasive monitoring of gingival crevicular fluid for estimation of blood glucose level. Med Biol Eng Comput 42(3):322–327
Yanagishita M, Hascall VC (1992) Cell-surface heparan sulfate proteoglycans. J Biol Chem 267:9451–9454
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fabietti, P.G., Canonico, V., Federici, M.O. et al. Control oriented model of insulin and glucose dynamics in type 1 diabetics. Med Bio Eng Comput 44, 69–78 (2006). https://doi.org/10.1007/s11517-005-0012-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-005-0012-2