Abstract
Environmental tobacco smoke (ETS) exposure has been proven to induce digestive diseases such as hepatic steatosis, cirrhosis, and gastrointestinal cancer, yet little is known about the link between ETS exposure and constipation. This study aimed to investigate the impact of ETS exposure on the risk of chronic constipation in adults aged 20 years or older. This is a cross-sectional study based on population. A total number of 7705 participants from the National Health and Nutrition Examination Survey (NHANES) 2005–2010 were included. Cotinine, an alkaloid found in tobacco, serves as a reliable and precise biomarker for measuring exposure to ETS. Hence, the categorization of exposure to ETS was conducted based on serum cotinine levels, resulting in four distinct categories. The association between ETS exposure and the risk of constipation was assessed using multivariable restricted cubic spline and logistic regression with odds ratio (OR) and 95% confidence interval (CI). The weighted prevalence of constipation in this study was estimated to be 7.51% based on stool consistency, or 3.11% based on stool frequency. The fully adjusted models indicated a positive correlation between exposure to ETS and constipation as measured by stool frequency, among adults with poor dietary quality (OR (95% CI): moderate exposure: 2.49 (1.05, 5.94); high exposure: 2.36(1.13, 4.95), P for trend = 0.03), while no significant difference was observed in the subgroup with a higher healthy eating index. Furthermore, the log10-transformed serum cotinine level exhibited a non-linear inverted U-shaped association with constipation in individuals with poor dietary quality (P overall = 0.0207, P non-linear = 0.0427). Conversely, a J-shaped non-linear relationship was observed in the subgroup with a higher healthy eating index (P overall = 0.0028, P non-linear = 0.0036). Our results show that ETS exposure appears to be positively associated with stool frequency-related chronic constipation in adults with poor dietary quality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Environmental tobacco smoke (ETS), which can also be considered passive smoking, includes secondhand smoke (SHS) and thirdhand smoke (THS) (Protano and Vitali 2011, Marques et al. 2021). Currently, more than 7000 chemicals have been identified in tobacco smoke, which include hundreds of toxic compounds and about 70 carcinogens (CDC 2022). Compared with active smoking, ETS contains similar toxins but with potentially higher concentrations (Liu et al. 2021; Pratt et al. 2023) due to the formation of toxic substances under different reducing conditions and at different temperatures (Marques et al. 2021). As the population grows, the number of nonsmokers at risk from ETS continues to increase, and approximately 1.2 million deaths per year are attributed to ETS (WHO 2023).
ETS has been reported to be associated with an increased risk of digestive diseases, such as hepatic steatosis (Tommasi et al. 2020), cirrhosis (Tommasi et al. 2020; Fouda et al. 2021), and gastrointestinal cancers (Li et al. 2020). Chronic constipation is one of the most common gastrointestinal symptoms (Bharucha and Lacy 2020), affecting about 6.6 to 10.1% of adults worldwide (Barberio et al. 2021; Sperber et al. 2021) and imposing a heavy burden on the healthcare resources. The effects of ETS exposure on constipation in children have been studied (Ludvigsson 2006), but the evidence is reliant on self-reported smoke exposure and thus susceptible to bias and subjectivity. Cotinine, a significant nicotine metabolite, is regarded as an objective biomarker that reflects exposure to tobacco smoke (Marques et al. 2021). Nevertheless, estimates of exposure to passive smoking determined by biomarkers are much higher than those determined by self-report (Max et al. 2012).
Evaluation, treatment, and management of chronic constipation have been progressing over time in adults, but remain suboptimal. Limited studies have revealed correlations between ETS exposure biomarkers and chronic constipation in adults. Therefore, this study will evaluate the impact of ETS exposure on chronic constipation based on the National Health and Nutrition Examination Survey (NHANES), which will have important clinical implications for the prevention and management of chronic constipation in adults.
Methods
Study population
NHANES is a cross-sectional survey based on the population and conducted continuously in 2-year cycles (CDC/NCHS 2023). This investigation is unique in using a complex, multi-stage sampling design that focuses on various health and nutrition measures, including biomonitoring of environmental chemicals. The research protocol for NHANES underwent ethical review and approval by the National Center for Health Statistics (approved by Protocol #2005–06). Furthermore, all participants were given informed consent during recruitment process.
NHANES data from three consecutive cycles (2005–2006, 2007–2008, and 2009–2010) were used in this study (Fig. 1). NHANES study participants who had 1) incomplete information on stool consistency or frequency (N = 16,443), 2) chronic diarrhea (N = 1268), 3) missing information on serum cotinine (N = 574), 4) active smokers (N = 3438), and 5) pregnancy (N = 321), self-reported colorectal cancer (N = 60), extreme total energy intakes of < 500 or > 3500 kcal/day for women and < 800 or > 4200 kcal/day for men (Banna et al. 2017) (N = 435), and incomplete information on other variables (N = 790) were excluded from the analysis. Active smoking was defined as: current smoking (smoked more than 100 cigarettes in their lifetime and currently smoke some days or every day) (Hou et al. 2023) or serum cotinine > 10 ng/ml (CDC 2017). Ultimately, the analyses included a total number of 7705 adult participants aged 20 years and older (Fig. 1).
Exposures
Cotinine, one of the major metabolites of nicotine, is a biomarker for the assessment of active or passive smoking exposure (Marques et al. 2021). An isotope dilution high-performance liquid chromatography/atmospheric pressure chemical ionization tandem mass spectrometry (ID HPLC-APCI MS/MS) was used to measure serum cotinine. The limit of detection (LOD) of serum cotinine is 0.015 ng/ml. Samples below the LOD were classified as “no exposure” (Moore et al. 2016), while samples at or above the LOD were divided into “low exposure,” “moderate exposure,” and “high exposure” according to weighted quantiles. In case a variable’s value is established to be lower than the detection limit, it will be allocated a value equal to the LOD divided by the square root of two.
Outcomes
According to the Rome IV criteria (Bharucha and Lacy 2020) and prior NHANES-based studies (Markland et al. 2013; Ballou et al. 2019; Sommers et al. 2019; Wilson 2020; Li et al. 2021), stool consistency and frequency were considered important evidence for the diagnosis of constipation. However, differences in the prevalence of constipation defined by stool consistency or frequency have been reported (Markland et al. 2013). Therefore, we identified chronic constipation based on stool consistency (BHQ060) or stool frequency (BHD050) in the NHANES Intestinal Health Questionnaire in this study.
Participants were presented with a vividly colored card featuring seven types of Bristol Stool Form Scale (BSFS) and were requested to indicate the number that corresponds to their typical or most frequent stool type after viewing the card. Those who designated their usual or most common stool type as BSFS type 1 (separate hard lumps, like nuts) or BSFS type 2 (sausage-like but lumpy) were categorized as suffering from chronic constipation. Chronic diarrhea was composed of type 6 (fluffy pieces with ragged edges, a mushy stool) and type 7 (watery, no solid pieces), and the remaining participants were considered to have normal stool consistency (Li et al. 2021).
The frequency of bowel movements was determined by asking: “How many times per week do you usually have a bowel movement?.” The results were classified as constipation (< 3 stools/week), diarrhea (≥ 21 stools/week), and normal (Ren et al. 2022).
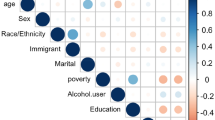
Covariates
Sociodemographic characteristics (gender, age, ethnicity, education level, marital status, ratio of family income to poverty level, and body mass index), self-reported behavioral factors (vigorous physical activity and drinking status), and dietary factors (healthy eating index and total energy intake) were the main covariates measured in our study. Gender was divided into male and female, and age was divided into young (20 to 39 years old), middle-aged (40 to 64 years old), and elderly (65 and older) (Yu et al. 2020). The self-reported race or ethnicity was divided into four categories: Mexican–American, non-Hispanic White, non-Hispanic Black, and other races. Adult education level includes less than high school, high school, and above high school. Marital status was divided into two groups, married/living with a partner and living alone. By dividing family income by poverty guidelines for the survey year, the ratio of family income to poverty (PIR) was calculated. Then, PIR was divided into three levels: < 1.3, 1.3–3.5, and > 3.5 (Johnson et al. 2013). According to body mass index (BMI), the study population was classified as normal/lean (< 25 kg/m2), overweight (25–30 kg/m2), and obesity (≥ 30 kg/m2) (Wang et al. 2021). Vigorous physical activity was defined by doing any vigorous activities that caused heavy sweating or large increases in breathing or heart rate for at least 10 min over the past 30 days (Markland et al. 2013). Defines “at least 12 alcoholic beverages per year” as drinking alcohol (Wang et al. 2021). The healthy eating index-2015 (HEI-2015) is an index to evaluate dietary quality (Liu et al. 2022). The HEI-2015 scores range from 0 to 100, with higher scores indicating a higher quality diet. In order to categorize participants, a threshold of 50 points was established, distinguishing between those with poor diet quality and those in need of improvement or already maintaining a good diet (Al-Ibrahim and Jackson 2019, Bigman and Ryan 2021).
Statistical analysis
All analyses incorporate sampling weights, strata, and primary sampling units to explain NHANES complex sampling designs and provide nationally representative estimates (CDC/NCHS 2023). By using Student’s t test, continuous variables with a normal distribution were reported as mean (standard error) (S.E), but continuous variables with a non-normal distribution were displayed as median (interquartile range) (IQR) (Hou et al. 2023). The chi-square test was used to express categorical variables as number (n) and weighted percentage (%) (Li et al. 2021; Hou et al. 2023). As continuous variables, cotinine levels are log10-transformed to achieve a normal distribution.
The relationship between exposure to ETS and chronic constipation was evaluated using multivariate logistic regression (Ballou et al. 2019; Li et al. 2021; Hou et al. 2023) with odds ratio (OR) and 95% confidence interval (CI). The unadjusted model is Model1. Model2 was adjusted for gender, age, ethnicity, and BMI. Model3 adjusted for marital status, education level, PIR, vigorous physical activity, drinking status, and HEI-2015 scores, total energy intake on the basis of Model2. Logistic regression analysis was used to evaluate the multiplicative interaction between HEI-2015 scores and ETS exposure on the probability of constipation. In addition, we used restricted cubic spline analysis (RCS) to model the non-linear correlation between serum cotinine and constipation (Hou et al. 2023). The R statistical software version 4.2.2 was employed to conduct all statistical analyses, and findings with a P value < 0.05 (bilateral) were regarded as statistically significant.
Results
Clinical characteristics of study participants
A total number of 7705 non-smoking participants from the 2005–2010 NHANES database were included in this analysis. The mean age of participants was 48.84 ± 0.46, 55.03% were female, and 73.76% were non-Hispanic Whites (Table 1). The prevalence of constipation in U.S. adults was estimated at 7.51% (95% CI: 6.58%, 8.45%) and 3.11% (95% CI: 2.51%, 3.71%) as determined by stool consistency and bowel frequency, respectively. Regarding ETS exposure, the study found that 27.74% of participants were reported no exposure, 24.89% were low exposure, 23.32% were moderate exposure, and 24.05% were high exposure (Supplementary Table (1)).
In comparison to individuals without ETS exposure, those with higher ETS exposure were more likely to be male, young, living alone, obesity, consuming alcohol and with lower levels of PIR, HEI-2015 scores, or total energy intake, whereas vigorous physical activity and constipation showed no significant differences (all P > 0.05). In relation to race and education, the proportion of non-Hispanic Whites and those with above high school education level is higher in the crowd of participants, and this proportion decreases as the exposure to ETS increases. However, the situation for non-Hispanic Blacks and with a high school education level or less is the opposite (Table 1).
In addition, Supplementary Table (1) shows the clinical characteristics of the population with constipation defined by stool consistency. Compared to the non-constipated group, individuals with chronic constipation were often female (P < 0.0001), non-Hispanic Blacks (P = 0.002), living alone (P = 0.01), non-drinkers (P < 0.001), and with lower levels of education, PIR, BMI, or total energy intake (all P < 0.001) (Supplementary Table (1)). However, using stool frequency to define constipation caused these results to change. Education level and marital status were no longer significantly associated with constipation (all P > 0.05), while age, HEI-2015 scores, and even serum cotinine levels became significant differences between the constipated and non-constipated groups, as shown in Supplementary Table (2).
Associations between ETS exposure and chronic constipation
Multivariate logistic regression analysis was used to illustrate the independent association between ETS exposure and chronic constipation (Table 2). Contrary to our previous assumptions, we found no significant difference between ETS exposure and chronic constipation after adjusting for covariates. Similarly, the RCS model was determined that there was no statistically significant nonlinear association (P non-linear > 0.05) between Log10-transformed serum cotinine levels and the risk of constipation (both for stool consistency and stool frequency-related constipation) after adjusting for all confounding factors, as shown in Fig. 2.
The dose–response relationship between ETS exposure and risk of chronic constipation. A Stool consistency. B Stool frequency. Adjustments were made in the model for gender, age, race, marriage, education level, PIR, BMI, vigorous physical activity, drinking status, and HEI-2015 scores, total energy intake. The OR of chronic constipation was presented by a solid black line, and the corresponding 95% CI was represented short black dashed lines
Interaction effect between healthy diet and ETS exposure on stool frequency-related constipation
Interestingly, we found that the effect of ETS exposure on stool frequency-related constipation varied according to HEI-2015 scores (P for interaction < 0.05). Subsequently, a stratified analysis of the HEI-2015 scores was conducted to explore the potential differences in the association between ETS exposure and constipation (Table 3). However, a positive association between ETS exposure and constipation was observed only in participants with poor diet quality in the adjusted model. Specifically, among participants with poor diet quality, unadjusted model results showed that moderate and high ETS exposure levels were positively associated with constipation compared to unexposed participants, and that the risk gradually increased with increasing exposure (OR (95% CI): moderate exposure: 2.23 (1.04, 4.81); high exposure: 2.45 (1.26, 4.77), P for trend = 0.02). Similar results were observed in Model2 (OR (95% CI): moderate exposure: 2.62 (1.12, 6.14); high exposure: 2.78 (1.34, 5.79), P for trend = 0.01). In the further adjusted Model3, the positive association between moderate and high ETS exposure and constipation remained statistically significant, although the odds ratio did not increase with increasing exposure (OR (95% CI): moderate exposure: 2.49 (1.05, 5.94); high exposure: 2.36 (1.13, 4.95), P for trend = 0.03) (Table 3).
After adjusting for multiple covariates, a dose–response correlation between ETS exposure and stool frequency-related constipation was observed in both dietary subgroups (Fig. 3). Specifically, in participants with poor diet quality, the dose–response relationship between serum cotinine levels after log10 conversion and constipation was non-linear inverted U-shaped (P overall = 0.0207, P non-linear = 0.0427) (Fig. 3A). In participants with higher HEI-2015 scores, there was a J-type nonlinear relationship between serum cotinine levels after log10 conversion and constipation (P overall = 0.0028, P non-linear = 0.0036) (Fig. 3B).
Dose–response relationship between ETS exposure and stool frequency-related constipation risk in dietary subgroups. A HEI-2015 = poor. B HEI-2015 = needing dietary improvement/good. Adjustments were made in the model for gender, age, race, marriage, education level, PIR, BMI, vigorous physical activity, drinking status, and total energy intake. The OR of chronic constipation was presented by a solid black line, and the corresponding 95% CI was represented short black dashed lines
Discussion
Our results showed that no statistically significant association was found between ETS exposure and adult constipation (using two different definitions). However, we found that the association between ETS exposure levels and constipation (based on stool frequency) was inconsistent across levels of HEI-2015 scores. Specifically, ETS exposure levels were positively associated with stool frequency-related constipation in participants with poor diet quality, while no such association was found in the subgroup with higher HEI-2015 scores. In addition, the serum cotinine level after log10 conversion showed a nonlinear inverted U shape with constipation in the unhealthy diet group, but there was a J-shaped nonlinear relationship with constipation in the subgroup with higher HEI-2015 scores.
Previous studies have shown no link between smoking and bowel frequency, stool consistency, or constipation (Shima et al. 2019; Talley et al. 2021). Studies on passive smoking and constipation have also focused on children (Ludvigsson 2006). Our study provides a new perspective on the effects of ETS on constipation, and ETS’s promoting effects on stool frequency-related constipation may not occur in the population as a whole, but may be relevant in people with unhealthy diets. This is of great interest, as the management of constipation remains a serious challenge, and dietary modification may be an effective way to mitigate the effects of smoke exposure on constipation and to prevent and treat constipation.
A multitude of compounds present in tobacco smoke, such as nicotine, exert either anti-inflammatory or pro-inflammatory influences on inflammatory bowel disease (IBD) via intricate signaling pathways (Zhang et al. 2022). And the level of cotinine is strongly associated with the occurrence of IBD (Widbom et al. 2020). However, bowel problems are common in patients with IBD; therefore, ETS exposure may be secondary to chronic constipation by influencing the occurrence of IBD. In addition, other potential pathways linking ETS exposure to constipation have also been hypothesized.
ETS exposure may cause intestinal symptoms by regulating intestinal flora. The study showed that intestinal microbes in the smoke exposure group showed increased levels of Bacteroidetes (Lee et al. 2018) and Clostridium (Wang et al. 2012) and decreased levels of Bifidobacterium (Northrup et al. 2021), Lactococcus (Wang et al. 2012), rumen coccus (Wang et al. 2012), and Firmicutes and Proteus (Lee et al. 2018), compared with those of never smokers. Second, smoke exposure is strongly associated with damage to the intestinal barrier. Studies have revealed that chronic exposure to smoke can lead to systemic and intestinal ischemia, resulting in angiogenesis and dysfunction of the gastrointestinal tract epithelial barrier (Fricker et al. 2018). Exposure to cigarette smoke condensate induced specific changes in Paneth cells that led to the production of antimicrobial peptides and decreased bactericidal capacity, thereby increasing the susceptibility of mice to bacterial infection resulting in ileal inflammation (Berkowitz et al. 2019). Finally, smoke exposure induces oxidative stress by means of free radicals contained in smoke, resulting in diminished activity of antioxidant enzymes and an imbalance between oxidants and antioxidants; this disruption leads to the disruption of tight junctions within the gastrointestinal tract (Bhattacharyya et al. 2014; Li et al. 2015). However, intestinal microbiome imbalance (Dimidi et al. 2017), intestinal barrier dysfunction (Chang et al. 2017), and inflammation and oxidative stress (McQuade et al. 2016) are closely related to the occurrence of chronic constipation (Fig. 4).
Gut-lung axis. The gut and lungs engage in reciprocal communication via both blood circulation and lymphatic circulation. Exposure to smoke has been observed to induce dysfunction in both the lungs and intestines, while maintaining a healthy diet can positively impact the well-being of the respiratory and intestinal systems. Individuals diagnosed with chronic obstructive pulmonary disease (COPD) and lung cancer frequently experience symptoms of constipation. Various factors such as imbalances in the intestinal flora, inflammatory or oxidative stress, and impairment of the intestinal barrier can contribute to the development of gastrointestinal disorders, including inflammatory bowel disease (IBD), gastrointestinal cancers, and constipation
After adjusting for confounders, ETS exposure had a positive association with fecal frequency-related constipation in participants with poor diet quality, while no such association was found in participants with a healthy diet. This discovery is consistent with previous research, which have demonstrated that smoke exposure exhibited a notable reduction in α diversity within the gut microbiota of mice subjected to a high-fat diet, while no discernible impact on α diversity was observed in mice following a normal diet (Yang et al. 2021). Nevertheless, a high level of α diversity typically signifies a healthy host pattern. Therefore, it is postulated that our findings may be attributed to two distinct explanations. First, the inflammatory and oxidative stress responses caused by ETS can be offset by improving diet. Previous research has shown that higher overall diet quality is protective against chronic constipation (Liu et al. 2022). At the same time, high dietary fiber (Ma et al. 2008), Omega-3 polyunsaturated fatty acids (Jomova et al. 2023), supplementation of antioxidants (vitamin C/vitamin E) (Jomova et al. 2023), and dietary lycopene (Mustra Rakic et al. 2021; Jomova et al. 2023) can prevent the oxidative stress response caused by exposure to SHS by reducing inflammation, reducing the production of reactive oxygen species, and preventing the inhibition of antioxidant enzymes. Furthermore, unhealthy diet can exacerbate the negative effects of ETS on the host, jointly regulating the composition of gut microbiota and promoting the occurrence and development of diseases (Martinez et al. 2021). High-fat diet interacts with cigarette smoke to regulate the enzyme activity of cytochrome P450, which induces pro-inflammatory cytokine storms (Sadler et al. 2018).
Curiously, we only observed an interaction between diet and serum cotinine on stool frequency-related constipation, whereas no such association was found for constipation based on a stool consistency definition. Based on a meta-analysis that examined 21 studies and included 2656 participants, ingesting probiotics that contain Lactobacillus and Bifidobacterium can help increase bowel frequency and reduce the transit time for intestinal contents in adults with constipation (Miller et al. 2017). However, nicotine and cotinine levels were associated with a lower gut microbiome, particularly a lower relative abundance of Bifidobacterium (Northrup et al. 2021). Therefore, diet and ETS exposure is more likely to affect the occurrence of constipation by changing the frequency of stool. In order to attain a more comprehensive understanding of the interconnectedness between exposure to ETS, fecal consistency, and fecal frequency, it is imperative to undertake additional research on this association from both clinical and experimental standpoints in forthcoming studies.
As far as we know, this study is the first to use biomarkers to quantify ETS exposure to assess its association with chronic constipation in adults. Secondly, the study population is from the NHANES database, which is representative of the whole country, which makes the research results more credible. Third, in order to more reasonably estimate the relationship between ETS exposure and chronic constipation, we took into account a wide range of potential confounding factors. However, our study also has several limitations. First, as a result of this study used is a cross-sectional design, causal inference about the relationship between ETS exposure and the risk of chronic constipation cannot be substantiated. Second, according to the Rome IV standard, chronic constipation is defined to include several other symptoms associated with constipation in addition to the consistency and frequency of stools. Therefore, the current study does not accurately represent the true prevalence of constipation. Third, the conclusions from the U.S. may not be applicable to other populations because of differences in genetic background, metabolic factors, dietary patterns, and ETS exposure levels.
Conclusion
In summary, this population-based cross-sectional study found that exposure to ETS is a risk factor for fecal frequency-related constipation in adults with unhealthy diets in the United States. This suggests the potential role of ETS exposure in predicting the risk of chronic constipation, and we suggest that ETS exposure and dietary modification should be considered in medical interventions to prevent chronic constipation. However, to validate the present findings and ascertain the causal link between ETS exposure and the risk of chronic constipation, further prospective studies with larger sample sizes and replicated measures are required.
Abbreviations
- BMI:
-
Body mass index
- BSFS:
-
Bristol Stool Form Scale
- CI:
-
Confidence interval
- ETS:
-
Environmental tobacco smoke
- HEI-2015:
-
Healthy Eating Index-2015
- IBD:
-
Inflammatory bowel disease
- ID HPLC-APCI MS/MS:
-
Isotope dilution high-performance liquid chromatography/atmospheric pressure chemical ionization tandem mass spectrometry
- IQR:
-
Interquartile range
- LOD:
-
Limit of detection
- MEC:
-
Mobile Examination Center
- NET:
-
Neutrophil extracellular trap
- NHANES:
-
National Health and Nutrition Examination Survey
- OR:
-
Odds ratio
- PIR:
-
Ratio of family income to poverty
- RCS:
-
Restricted cubic spline
- S. E:
-
Standard error
- SHS:
-
Secondhand smoke
- THS:
-
Thirdhand smoke
References
Al-Ibrahim AA, Jackson RT (2019) Healthy eating index versus alternate healthy index in relation to diabetes status and health markers in U.S. adults: NHANES 2007–2010. Nutr J 18:26
Ballou S, Katon J, Singh P, Rangan V, Lee HN, McMahon C, Nee J (2019) Chronic diarrhea and constipation are more common in depressed individuals. Clin Gastroenterol Hepatol 17:2696–2703
Banna JC, McCrory MA, Fialkowski MK, Boushey C (2017) Examining plausibility of self-reported energy intake data: considerations for method selection. Front Nutr 4:45
Barberio B, Judge C, Savarino EV, Ford AC (2021) Global prevalence of functional constipation according to the Rome criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 6:638–648
Berkowitz L, Pardo-Roa C, Salazar GA, Salazar-Echegarai F, Miranda JP, Ramírez G, Álvarez-Lobos M (2019) Mucosal exposure to cigarette components induces intestinal inflammation and alters antimicrobial response in mice. Front Immunol 10:2289
Bharucha AE, Lacy BE (2020) Mechanisms, evaluation, and management of chronic constipation. Gastroenterology 158:1232-1249.e3
Bhattacharyya A, Chattopadhyay R, Mitra S, Crowe SE (2014) Oxidative stress: an essential factor in the pathogenesis of gastrointestinal mucosal diseases. Physiol Rev 94:329–354
Bigman G, Ryan AS (2021) Healthy Eating Index-2015 is associated with grip strength among the US adult population. Nutrients 13:3358
CDC (2017): National Biomonitoring Program Cotinine. Accessed 21 May 2023. Available from:https://www.cdc.gov/biomonitoring/Cotinine_BiomonitoringSummary.html
CDC (2022): Smoking & Tobacco Use. Accessed 20 May 2023. Available from:https://www.cdc.gov/tobacco/secondhand-smoke/about.html
CDC/NCHS (2023): National Health and Nutrition Examination Survey. Accessed 21 May 2023. Available from:https://www.cdc.gov/nchs/nhanes/index.htm
Chang J, Leong RW, Wasinger VC, Ip M, Yang M, Phan TG (2017) Impaired intestinal permeability contributes to ongoing bowel symptoms in patients with inflammatory bowel disease and mucosal healing. Gastroenterology 153:723-731.e1
Dimidi E, Christodoulides S, Scott SM, Whelan K (2017) Mechanisms of action of probiotics and the gastrointestinal microbiota on gut motility and constipation. Adv Nutr 8:484–494
Fouda S, Khan A, Chan SMH, Mahzari A, Zhou X, Qin CX, Ye JM (2021) Exposure to cigarette smoke precipitates simple hepatosteatosis to NASH in high-fat diet fed mice by inducing oxidative stress. Clin Sci (lond) 135:2103–2119
Fricker M, Goggins BJ, Mateer S, Jones B, Kim RY, Gellatly SL, Hansbro PM (2018) Chronic cigarette smoke exposure induces systemic hypoxia that drives intestinal dysfunction. JCI Insight 3:e94040
Hou W, Chen S, Zhu C, Gu Y, Zhu L, Zhou Z (2023) Associations between smoke exposure and osteoporosis or osteopenia in a US NHANES population of elderly individuals. Front Endocrinol (lausanne) 14:1074574
Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LR (2013) National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat 2:1–24
Jomova K, Raptova R, Alomar SY, Alwasel SH, Nepovimova E, Kuca K, Valko M (2023) Reactive oxygen species, toxicity, oxidative stress, and antioxidants: chronic diseases and aging. Arch Toxicol 97:2499–2574
Lee SH, Yun Y, Kim SJ, Lee EJ, Chang Y, Ryu S, Lee JH (2018) Association between cigarette smoking status and composition of gut microbiota: population-based cross-sectional study. J Clin Med 7:282
Li H, Wu Q, Xu L, Li X, Duan J, Zhan J, Chen H (2015) Increased oxidative stress and disrupted small intestinal tight junctions in cigarette smoke-exposed rats. Mol Med Rep 11:4639–4644
Li J, Xu HL, Yao BD, Li WX, Fang H, Xu DL, Zhang ZF (2020) Environmental tobacco smoke and cancer risk, a prospective cohort study in a Chinese population. Environ Res 191:110015
Li Y, Tong WD, Qian Y (2021) Effect of physical activity on the association between dietary fiber and constipation: evidence from the National Health and Nutrition Examination Survey 2005–2010. J Neurogastroenterol Motil 27:97–107
Liu J, Benowitz NL, Hatsukami DK, Havel CM, Lazcano-Ponce E, Strasser AA, Jacob P 3rd (2021) 3-Ethenylpyridine measured in urine of active and passive smokers: a promising biomarker and toxicological implications. Chem Res Toxicol 34:1630–1639
Liu Q, Kang Y, Yan J (2022) Association between overall dietary quality and constipation in American adults: a cross-sectional study. BMC Public Health 22:1971
Ludvigsson JF (2006) Epidemiological study of constipation and other gastrointestinal symptoms in 8000 children. Acta Paediatr 95:573–580
Ma Y, Hébert JR, Li W, Bertone-Johnson ER, Olendzki B, Pagoto SL, Liu S (2008) Association between dietary fiber and markers of systemic inflammation in the Women’s Health Initiative Observational Study. Nutrition 24:941–949
Markland AD, Palsson O, Goode PS, Burgio KL, Busby-Whitehead J, Whitehead WE (2013) Association of low dietary intake of fiber and liquids with constipation: evidence from the National Health and Nutrition Examination Survey. Am J Gastroenterol 108:796–803
Marques H, Cruz-Vicente P, Rosado T, Barroso M, Passarinha LA, Gallardo E (2021) Recent developments in the determination of biomarkers of tobacco smoke exposure in biological specimens: a review. Int J Environ Res Public Health 18:1768
Martinez JE, Kahana DD, Ghuman S, Wilson HP, Wilson J, Kim SCJ, Friedman TC (2021) Unhealthy lifestyle and gut dysbiosis: a better understanding of the effects of poor diet and nicotine on the intestinal microbiome. Front Endocrinol (lausanne) 12:667066
Max W, Sung HY, Shi Y (2012) Deaths from secondhand smoke exposure in the United States: economic implications. Am J Public Health 102:2173–2180
McQuade RM, Carbone SE, Stojanovska V, Rahman A, Gwynne RM, Robinson AM, Nurgali K (2016) Role of oxidative stress in oxaliplatin-induced enteric neuropathy and colonic dysmotility in mice. Br J Pharmacol 173:3502–3521
Miller LE, Ouwehand AC, Ibarra A (2017) Effects of probiotic-containing products on stool frequency and intestinal transit in constipated adults: systematic review and meta-analysis of randomized controlled trials. Ann Gastroenterol 30:629–639
Moore BF, Clark ML, Bachand A, Reynolds SJ, Nelson TL, Peel JL (2016) Interactions between diet and exposure to secondhand smoke on the prevalence of childhood obesity: results from NHANES, 2007–2010. Environ Health Perspect 124:1316–1322
Mustra Rakic J, Liu C, Veeramachaneni S, Wu D, Paul L, Ausman LM, Wang XD (2021) Dietary lycopene attenuates cigarette smoke-promoted nonalcoholic steatohepatitis by preventing suppression of antioxidant enzymes in ferrets. J Nutr Biochem 91:108596
Northrup TF, Stotts AL, Suchting R, Matt GE, Quintana PJE, Khan AM, Stewart CJ (2021) Thirdhand smoke associations with the gut microbiomes of infants admitted to a neonatal intensive care unit: an observational study. Environ Res 197:111180
Pratt K, Hilty A, Jacob P, Schick SF (2023) Respiratory exposure to thirdhand cigarette smoke increases concentrations of urinary metabolites of nicotine. Nicotine Tob Res 25:1424–1430
Protano C, Vitali M (2011) The new danger of thirdhand smoke: why passive smoking does not stop at secondhand smoke. Environ Health Perspect 119:A422
Ren W, Zhang C, Wang X, Wang J (2022) Investigating associations between urinary phthalate metabolite concentrations and chronic diarrhea: findings from the National Health and Nutrition Examination Survey, 2005–2010. Environ Sci Pollut Res Int 29:77625–77634
Sadler NC, Webb-Robertson BM, Clauss TR, Pounds JG, Corley R, Wright AT (2018) High-fat diets alter the modulatory effects of xenobiotics on cytochrome P450 activities. Chem Res Toxicol 31:308–318
Shima T, Amamoto R, Kaga C, Kado Y, Sasai T, Watanabe O, Tsuji H (2019) Association of life habits and fermented milk intake with stool frequency, defecatory symptoms and intestinal microbiota in healthy Japanese adults. Benef Microbes 10:841–854
Sommers T, Mitsuhashi S, Singh P, Hirsch W, Katon J, Ballou S, Nee J (2019) Prevalence of chronic constipation and chronic diarrhea in diabetic individuals in the United States. Am J Gastroenterol 114:135–142
Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren M, Tack J, Palsson OS (2021) Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome Foundation Global Study. Gastroenterology 160:99-114.e3
Talley NJ, Powell N, Walker MM, Jones MP, Ronkainen J, Forsberg A, Andreasson A (2021) Role of smoking in functional dyspepsia and irritable bowel syndrome: three random population-based studies. Aliment Pharmacol Ther 54:32–42
Tommasi S, Yoon JI, Besaratinia A (2020) Secondhand smoke induces liver steatosis through deregulation of genes involved in hepatic lipid metabolism. Int J Mol Sci 21:1296
Wang C, Zhang L, Li L (2021) Association between selenium intake with chronic constipation and chronic diarrhea in adults: findings from the National Health and Nutrition Examination Survey. Biol Trace Elem Res 199:3205–3212
Wang H, Zhao JX, Hu N, Ren J, Du M, Zhu MJ (2012) Side-stream smoking reduces intestinal inflammation and increases expression of tight junction proteins. World J Gastroenterol 18:2180–2187
WHO (2023): Tobacco. Accessed 20 May 2023. Available from:https://www.who.int/news-room/fact-sheets/detail/tobacco
Widbom L, Schneede J, Midttun Ø, Ueland PM, Karling P, Hultdin J (2020) Elevated plasma cotinine is associated with an increased risk of developing IBD, especially among users of combusted tobacco. PLoS ONE 15:e0235536
Wilson PB (2020) Associations between physical activity and constipation in adult Americans: results from the National Health and Nutrition Examination Survey. Neurogastroenterol Motil 32:e13789
Yang Y, Yang C, Lei Z, Rong H, Yu S, Wu H, Guo J (2021) Cigarette smoking exposure breaks the homeostasis of cholesterol and bile acid metabolism and induces gut microbiota dysbiosis in mice with different diets. Toxicology 450:152678
Yu B, Zhang X, Wang C, Sun M, Jin L, Liu X (2020) Trends in depression among adults in the United States, NHANES 2005–2016. J Affect Disord 263:609–620
Zhang W, Lin H, Zou M, Yuan Q, Huang Z, Pan X, Zhang W (2022) Nicotine in inflammatory diseases: anti-inflammatory and pro-inflammatory effects. Front Immunol 13:826889
Acknowledgements
We would like to express our heartfelt thanks to all the participants in this study.
Funding
This work is supported by the National Natural Science Foundation of China (the funder: Yongning Zhou, No. 71964021) and the Foundation of The First Hospital of Lanzhou University, China (the funder: Ya Zheng, No. ldyyyn2021-59).
Author information
Authors and Affiliations
Contributions
Project design and conception: R. D., Y. Z., and W. K.; administrative support and supervision: Y. W. and Y. Z.; data download and processing: R. D. and Y. Z.; data analysis and interpretation: R. D. and W. K.; manuscript writing and retouching: R. D.; final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate.
The NHANES study protocol was reviewed and approved by the National Center for Health Statistics ethics review board (approved by Protocol #2005–06) (https://www.cdc.gov/nchs/nhanes/irba98.htm), and informed consent was obtained from all participants at recruitment.
Consent to participate
This is not applicable.
Consent for publication
This is not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available in the NHANES database, https://wwwn.cdc.gov/nchs/nhanes/.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• NHANES data were used to investigate the association between environmental tobacco smoke (ETS) exposure and chronic constipation.
• Serum cotinine levels were used to more objectively assess the extent of ETS exposure.
• ETS exposure is positively associated with a higher risk of chronic constipation in US adults with poor dietary quality.
• The log10-transformed serum cotinine level exhibited a non-linear inverted U-shaped association with constipation in individuals with poor dietary quality. Conversely, a J-shaped non-linear relationship was observed in the subgroup with a higher healthy eating index.
Recommendations.
• Environmental tobacco smoke (ETS) exposure and dietary modification should be considered in medical interventions to prevent chronic constipation.
• Larger sample size studies are needed to verify the association between ETS exposure and the risk of chronic constipation.
• Further prospective studies are needed to determine the causal relationship between serum cotinine levels and chronic constipation.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Duan, R., Zheng, Y., Kong, W. et al. Association of environmental tobacco smoke exposure with chronic constipation: a nationwide survey (NHANES 2005–2010). Environ Sci Pollut Res 30, 115776–115787 (2023). https://doi.org/10.1007/s11356-023-30542-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-30542-4