Abstract
Purpose
The purpose of this study was to compare the therapeutic pressure determined by an automated CPAP device (AutoCPAP) during the titration period, between nasal and oronasal mask and the residual apnea-hypopnea index (AHI) on a subsequent poligraphy performed with the established therapeutic CPAP.
Methods
As a retrospective study, 109 subjects with moderate and severe obstructive sleep apnea-hypopnea (apnea-hypopnea index ≥ 15 events/h) were studied. CPAP titration was performed using an auto-titrating device.
Results
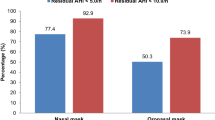
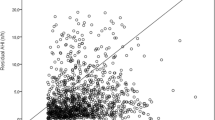
There was significant difference in the mean pressure delivered with autoCPAP between the group of patients using the nasal mask (mean 10.0 cmH2O ± 2.0 SD) and the group which used the oronasal mask (mean 11.2 cmH2O ± 2.1) (p < 0.05). Residual apneas were lower when using a nasal mask: average AHI of 2.6 ± 2.5 compared to 4.5 ± 4.0 using an oronasal mask (p < 0.05). On multivariate analysis, the only independent predictor of the level of therapeutic pressure of CPAP was the type of mask used (r = 0.245, p 0.008).
Conclusions
Therapeutic CPAP level for OSAH is higher when administered via oronasal mask, leaving more residual events. These findings suggest that nasal mask should be the first choice for OSAH treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive Sleep Apnea-Hypopnea (OSAH) is a sleep-related breathing disorder characterized by full or partial occlusion of upper airways during sleep that can lead to repeated oxyhemoglobin desaturations, inspiratory efforts, and sleep fragmentation.
Many studies have shown that untreated OSAH is associated with an increased risk of cardiovascular and cerebrovascular diseases [1–6].
Presently, the main treatment for moderate-to-severe OSAH is continuous positive airway pressure (CPAP), which acts as a pneumatic splint by raising the intraluminal (transmural) pressure above a critical pressure of the upper airway (Pcrit) [7], keeping the upper airway open and preventing obstructive respiratory events [8].
CPAP is delivered to the patient via a hose and a mask. There are many different mask models, generally classified as the ones which only cover nose (nasal mask), nose and mouth (oronasal mask), or entire face [9].
CPAP is virtually always effective in OSAH treatment, but its primary limitation is the low compliance rate [10–12]. Yaggi et al. found that only 58 % of patients with OSAH met minimum criteria for required compliance with CPAP (at least 4 h per night for at least five nights a week) [1].
The reasons for poor compliance are mask discomfort; concomitant pathologic condition such as depression or claustrophobia; side effects due to CPAP therapy such as mucosal dryness, air leaks, nasal congestion, or obstruction; and skin irritation. Mask discomfort plays an important role in poor compliance which is related to the type of mask that the patient (or the physician) chooses on initial CPAP titration session [13]. Although clinicians generally consider that the choice of the interface is crucial for the success of CPAP treatment, so far, only very few studies have specifically looked at the impact of different mask types on CPAP efficacy, and a 2006 Cochrane meta-analysis [14] was not able to establish the optimum form of CPAP delivery interface due to lack of data about use of different masks in OSAH patients.
The aim of this study was to evaluate, in a subgroup of moderate-to-severe OSAH patients, the possible effect of nasal and oronasal masks on the therapeutic pressure determined by an automated CPAP device [15] (AutoCPAP) during the titration period and the residual apnea-hypopnea index (AHI) on a subsequent poligraphy performed with the established therapeutic CPAP.
Materials and methods
This retrospective study was conducted in the Sleep Laboratories of the Respiratory Medicine Department at Spedali Civili Hospital, Brescia, Italy and M. Mellini Hospital, Chiari, Italy.
Subjects suspected for having OSAH were referred to our laboratories from May 2012 to June 2013 and were evaluated with all-night sleep study (Siesta Compumedics Polysomnographs) at baseline. For all patients, the following data were recorded: age, sex, Body Mass Index (BMI), neck and abdominal circumference, Epworth Sleepiness Scale (ESS) [16], Apnea-Hypopnea Index (AHI), and average and minimum oxyhemoglobin saturation (SaO2 %).
Respiratory events were classified according to the AASM criteria [17]: an apnea was defined as a >90 % decrease in peak nasal pressure than baseline, lasting at least 10 s. Hypopnea was defined by a >30 % decrease than baseline nasal pressure, lasting at least 10 s and associated with a ≥4 % oxyhemoglobin saturation drop. Arterial oxygen saturation was continuously measured by a finger tip infrared pulsoximetry and one ECG derivation was also monitored.
On the basis of clinical history and symptoms, patients with an AHI ≥ 15 were considered eligible for CPAP treatment and were enrolled in the study. Exclusion criteria were the presence of comorbidities such as heart failure, COPD, obesity hypoventilation syndrome, history of nasal or paranasal disease, and anatomical problems precluding the use of a nasal or oronasal mask.
All patients included in the study underwent a home titration period of three to four nights using Philips-Respironics System One REMstar AutoCPAP with heated humidification. Before the first titration night, patients wore different masks models, choosing the more comfortable ones.
Patients were divided into two groups according to their choice between nasal (Philips-Respironics ComfortGel and EasyLife, Fisher & Paykel FlexiFit) and oronasal (Philips-Respironics ComfortGel Full and ComfortFull, ResMed Mirage Quattro) masks. The most appropriate mask size was applied in each case to minimize leakage. The patients wore the mask connected with AutoCPAP for 2 h in the afternoon adaptation session.
After the home titration period, 90th percentile (therapeutic) AutoCPAP pressure and average unintentional leak were downloaded from AutoCPAP.
Patients underwent a second polisomnographic study on therapeutic CPAP pressure and residual AHI was calculated.
The study was approved by the local Ethic Committee (Spedali Civili, Brescia, Italy; no number available).
Statistical analysis
Continuous variables were compared using two-tailed, unpaired t tests for variables with normally distributed data and Mann–Whitney test for variables with non-normally distributed data. Fisher’s exact test was used to compare categorical data between different groups of subjects. Relationships among variables were analyzed using linear regression where appropriate. A two-tailed p value of <0.05 was considered statistically significant. The variables for which p was less than 0.05 according to univariate analysis were entered into a multivariate model to identify the independent variables that influence the CPAP pressure. Data are expressed as mean ± SD. Statistical analysis was performed using SPSS 18.0 (SPSS; Chicago, IL) and Graph Pad Prism 5.0 (MacKiev Software, Boston, MA).
Results
One hundred and nine patients were included in this retrospective study. Table 1 shows the demographic and descriptive data of patients taken as a whole group and divided between patients who chose nasal and oronasal masks. Nasal masks were preferred in 67 cases (61.5 % of total), oronasal masks in 42 cases (38.5 % of total).
There were no differences between the two groups in terms of gender distribution, age, BMI, baseline AHI, mean and minimum SaO2% both at baseline, and on CPAP polisomnography. Patients who chose oronasal masks had higher residual AHI at polisomnoghraphy on CPAP despite a significantly higher therapeutic pressure determined during titration session (Fig. 1).
Considering the therapeutic CPAP as dependent variable, univariate analysis revealed a significant relationship with BMI, baseline AHI, and mask type. Age, gender, ESS, and mean or minimum SaO2 were not related to the therapeutic CPAP (see Table 2). The multivariate analysis which included the three significant variables described above showed that the only significant independent correlate of the therapeutic CPAP was the type of mask used (r = 0.245, p 0.008) (see Table 3).
Discussion
Continuous positive airway pressure is the most effective treatment for OSAH [18] but the patient’s compliance with CPAP treatment is surprisingly low [11, 19]. Among different reasons of discontinuation, one of the most relevant is the mask discomfort.
Due to the limited number of studies available comparing various interface types, there are no specific recommendations on the initial choice of interface. The physician, however, should evaluate both the most effective mask and patient comfort.
Oronasal masks are frequently used because of presumptive excessive mouth leak while using nasal masks, but some studies showed that the number of residual respiratory events was significantly higher with oronasal masks than with nasal masks [20, 21].
In two studies comparing oronasal and nasal masks on auto-titrating CPAP, Teo et al. and Bakker et al. found no significant differences on the final pressure of CPAP between the two types of mask [20, 21]. However, these studies were limited by small samples size.
In contrast, we showed in this retrospective study that CPAP delivered through a nasal mask is effective for moderate to severe OSAH requiring significantly lower pressures than oronasal mask. Moreover, residual apneas decrease using a nasal mask.
In previous studies [22–25], higher comfort was reported with nasal mask. Accordingly, also in this work, nasal mask was preferred in 61.5 % of cases.
Wearing oronasal masks is associated with an increase in upper airway resistance [26] due to the posterior displacement of the tongue and this might be the cause for higher residual respiratory events than those observed during CPAP treatment. In line with the increase in upper airway resistance induced by oronasal masks, we and others found that oronasal masks were associated with higher therapeutic pressure than nasal ones. We speculate that a higher CPAP pressure is required to counteract the posterior displacement of the mandibula induced by an oronasal mask with increasing risk of unintentional leaks. This may contribute to further reduce CPAP compliance.
For these reasons, in patients with sleep apnea, it seems to be useful to propose a nasal mask from the beginning to improve adherence to CPAP and treatment efficacy.
Conclusions
In summary, the choice of the interface between the patient and the ventilator appears crucial. Since a higher level of therapeutic CPAP is required, on average, with the oronasal mask, the first attempt should be always made with the patient wearing a nasal mask. This could decrease patients’ discomfort and consequently increase the CPAP compliance.
Abbreviations
- SD:
-
Standard deviation
- OSAH:
-
Obstructive Sleep Apnea-Hypopnea
- AHI:
-
Apnea–Hypopnoea Index
- AutoCPAP:
-
automated CPAP device
- BMI:
-
Body Mass Index
- ESS:
-
Epworth Sleepiness scale
- CPAP:
-
Continuous Positive Airway Pressure
References
Sullivan CE, Issa FG, Berthon-Jones M, Eves L (1981) Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1(8225):862–865
Smith PL, Wise RA, Gold AR, Schwartz AR, Permutt S (1988) Upper airway pressure-flow relationships in obstructive sleep apnea. J Appl Physiol 64(2):789–795
Elliott MW (2004) The interface: crucial for successful noninvasive ventilation. Eur Respir J 23(1):7–8
Zozula R, Rosen R (2001) Compliance with continuous positive airway pressure therapy: assessing and improving treatment outcomes. Curr Opin Pulm Med 7(6):391–398
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353(19):2034–2041
Peker Y, Hedner J, Johansson A, Bende M (1997) Reduced hospitalization with cardiovascular and pulmonary disease in obstructive sleep apnea patients on nasal CPAP treatment. Sleep 20(8):645–653
Peker Y, Hedner J, Norum J, Kraiczi H, Carlson J (2002) Increased incidence of cardiovascular disease in middle-aged men with obstructive sleep apnea: a 7-year follow-up. Am J Respir Crit Care Med 166(2):159–165
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342(19):1378–1384
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S et al (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 283(14):1829–1836
Bottini P, Taranto-Montemurro L, Novali M, Bettinzoli M, Roca E, Andreoli C et al (2012) Effects of CPAP on systemic hypertension in OSAH: a monocentric, observational, cohort study. Respir Med 106(9):1329–1334
Borel JC, Tamisier R, Dias-Domingos S, Sapene M, Martin F, Stach B et al (2013) Type of mask may impact on continuous positive airway pressure adherence in apneic patients. PLoS One 8(5):e64382
Engleman HM, Wild MR (2003) Improving CPAP use by patients with the sleep apnoea/hypopnoea syndrome (SAHS). Sleep Med Rev 7(1):81–99
Haniffa M, Lasserson TJ, Smith I (2004) Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev 4, CD003531
Chai CL, Pathinathan A, Smith B (2006) Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev 4, CD005308
Ikeda Y, Kasai T, Kawana F, Kasagi S, Takaya H, Ishiwata S et al (2012) Comparison between the apnea-hypopnea indices determined by the REMstar Auto M series and those determined by standard in-laboratory polysomnography in patients with obstructive sleep apnea. Intern Med 51(20):2877–2885
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
No authors (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research The Report of an American Academy of Sleep Medicine Task Force. Sleep;22(5):667–89
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D et al (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29(3):375–380
Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM et al (1993) Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis 147(4):887–895
Teo M, Amis T, Lee S, Falland K, Lambert S, Wheatley J (2011) Equivalence of nasal and oronasal masks during initial CPAP titration for obstructive sleep apnea syndrome. Sleep 34:951–955
Bakker JP, Neill AM, Campbell AJ (2012) Nasal versus oronasal continuous positive airway pressure masks for obstructive sleep apnea: a pilot investigation of pressure requirement, residual disease, and leak. Sleep Breath 16(3):709–716
Fernandez R, Cabrera C, Rubinos G, Pando A, Galindo R, Rodriguez F et al (2012) Nasal versus oronasal mask in home mechanical ventilation: the preference of patients as a strategy for choosing the interface. Respir Care 57(9):1413–1417
Navalesi P, Fanfulla F, Frigerio P, Gregoretti C, Nava S (2000) Physiologic evaluation of noninvasive mechanical ventilation delivered with three types of masks in patients with chronic hypercapnic respiratory failure. Crit Care Med 28(6):1785–1790
Willson GN, Piper AJ, Norman M, Chaseling WG, Milross MA, Collins ER et al (2004) Nasal versus full face mask for noninvasive ventilation in chronic respiratory failure. Eur Respir J 23(4):605–609
Ebben MR, Oyegbile T, Pollak CP (2012) The efficacy of three different mask styles on a PAP titration night. Sleep Med 13(6):645–649
Borel JC, Gakwaya S, Masse JF, Melo-Silva CA, Series F (2012) Impact of CPAP interface and mandibular advancement device on upper airway mechanical properties assessed with phrenic nerve stimulation in sleep apnea patients. Respir Physiol Neurobiol 183(2):170–176
Conflict of interest
The authors have no conflict of interest to disclose. No financial support, off label, or investigational use received or performed.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was performed at Cattedra di Malattie dell’Apparato Respiratorio Università di Brescia, Brescia, Divisione di Prima Medicina Interna, Spedali Civili, Brescia and at Centro per i Disturbi Cardio-Respiratori nel Sonno, Fisiopatologia Respiratoria A.O. M. Mellini, Chiari, all in Italy.
Rights and permissions
About this article
Cite this article
Bettinzoli, M., Taranto-Montemurro, L., Messineo, L. et al. Oronasal masks require higher levels of positive airway pressure than nasal masks to treat obstructive sleep apnea. Sleep Breath 18, 845–849 (2014). https://doi.org/10.1007/s11325-014-0954-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-014-0954-4