Abstract
Purpose
This single-blinded, randomized, controlled pilot study aimed to investigate whether there is a difference between nasal and oronasal masks in therapeutic continuous positive airway pressure (CPAP) requirement, residual disease, or leak when treating obstructive sleep apnea (OSA) and if differences were related to measures of upper airway size.
Methods
Patients with severe OSA currently using CPAP at ≥4 h/night with a nasal mask were examined (including Mallampati scale, incisal relationship, and mandibular protrusion) and then randomized to receive auto-positive airway pressure (PAP) or fixed CPAP at a manually titrated pressure for 1 week each at home, with immediate crossover. Within each week, a nasal mask and two oronasal masks were to be used for two or three nights each in random order. Data were downloaded from the device.
Results
Twelve patients completed the trial (mean ± SD AHI 59.8 ± 28.6 events/h; CPAP 11.1 ± 3.2 cmH2O; BMI 37.7 ± 5.0 kg/m2). During auto-PAP, the median 95th percentile pressure delivered with all masks was within 0.5 cmH2O (p > 0.05). During CPAP, median residual AHI was 0.61 (IQR = 1.18) for the nasal mask, 1.70 (IQR = 4.04) for oronasal mask 1, and 2.48 (IQR = 3.74) for oronasal mask 2 (p = 0.03). The 95th percentile leak was lowest with the nasal mask during both CPAP and auto-PAP (both p < 0.01). Differences in pressure or residual disease were not related to measures of upper airway shape or body habitus.
Conclusions
In obese OSA patients changing from a nasal to oronasal mask increased leak and residual AHI but did not affect the therapeutic pressure requirement. The findings of the current study highlight mask leak as the major difficulty in the use of oronasal masks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
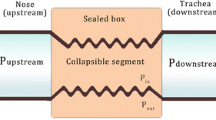
Obstructive sleep apnea (OSA) is a condition characterized by frequent partial or complete blockage of the upper airway during sleep and is associated with daytime hypersomnolence [1, 2], neurocognitive impairment [3], and an increased risk of cardiovascular morbidity and mortality in the long term [4–6]. The first-line therapy for moderate-to-severe OSA is continuous positive airway pressure (CPAP), which prevents airway collapse by delivering positive pressure to the upper airway at a prescribed therapeutic level, through either a nasal, oral, or oronasal mask interface [7].
Anecdotally, we have observed marked differences in therapeutic pressure when CPAP is manually titrated using a nasal mask compared with a standard oronasal mask that seals beneath the lower lip. We suspect that the pressure placed on the lower jaw by this type of mask may result in the posterior positioning of the mandible, leading to a reduced upper airway diameter and increased collapsibility. It is known that mandibular retrognathia contributes to OSA [8], and a small oropharynx diameter is associated with OSA [9, 10]; hence, a higher pressure is required to maintain airway patency [11]. This issue may potentially be avoided by using an oronasal mask that seals beneath the chin.
The comparison of various CPAP delivery interfaces was the subject of a 2009 Cochrane systematic review and meta-analysis [12]. Only one randomized controlled trial was available for inclusion, comparing nasal and oronasal masks. It reported that nasal masks led to significantly higher adherence and less daytime sleepiness than oronasal masks [13]. Prosise et al. reported in 1994 that there is no significant difference in residual apnea–hypopnoea index (AHI) between nasal and oronasal masks [14], but this study did not investigate pressure requirement. We are aware of only two studies that have reported therapeutic pressure as determined using nasal and oronasal masks. In 2003, Beecroft et al. found in a non-randomized study that a standard oronasal mask required on average 2.0 cmH2O higher pressure than a nasal mask, which did not reach statistical significance [15]. More recently, Teo et al. reported the 95th percentile pressure as determined during a single-night titration with an APAP device to be 0.3 cmH2O lower with a standard oronasal mask (non significant) and with a significantly increased leak compared with a nasal mask [16]. However, none of the aforementioned studies utilized an under-chin oronasal mask design.
Current clinical guidelines state that a variety of mask types should be available for each patient and do not specify a clinically significant level of leak at which a change of mask should occur [17]. In many laboratories, it is standard practice that patients with a patent nasal airway begin CPAP using a nasal mask, with a swap to an oronasal mask if excessive mouth leak is evident or if the nasal mask is not tolerated. Hence, therapeutic pressure for many patients is determined during titration with a nasal mask, which may be insufficient for long-term oronasal mask use. The presence of even a low level of obstructed breathing is associated with daytime sleepiness [2] and continued risk of hypertension [18]. We therefore aimed to investigate in a single-blinded, randomized, controlled pilot study whether there is a difference in therapeutic pressure requirement, residual AHI, or leak levels between nasal, standard oronasal, and under-chin oronasal masks. A secondary aim was to investigate whether measurements of upper airway shape or body habitus were correlated with a difference in therapeutic pressure between masks.
Methods
Ethical approval was granted by the Central Region Ethics Committee (CEN/10/07/028), and all patients gave written informed consent. The trial was registered with the Australia and New Zealand Clinical Trials Registry (12610000583044).
Recruitment
Patients meeting the following inclusion criteria were randomly selected from a database of patients already established on CPAP: ≥25 years of age, full-night diagnostic polysomnography (PSG) indicating an AHI ≥30 events/h, full-night manual CPAP titration within the previous 3 years undertaken using a nasal mask, availability of a pre-diagnostic Epworth Sleepiness Scale score [19], CPAP usage averaging ≥4 h/night since the beginning of treatment, currently using a nasal cushion mask (as opposed to nasal pillows) without chinstrap, and subjective report of predominantly supine sleep. Patients with a significant cardiac, respiratory, or sleep co-morbidity interpreted by a sleep/respiratory physician (including central sleep apnea), those regularly taking sedative, psychotropic or stimulant drugs including excessive alcohol or caffeine, and those with a full upper and/or lower denture were excluded. Diagnostic and titration studies were performed and scored by experienced polysomnographic technologists according to standard criteria [20–22].
Measurement of upper airway shape and body habitus
The following measurements were obtained at baseline: body mass index (BMI), neck, waist and hip circumferences, oral cavity crowding as per the Mallampati scale (grades I–IV) [23], incisal relationship assessed visually (class I normal, class II overbite, class III underbite), and degree of mandibular protrusion measured using a Somnodent George Gauge (SomnoMed, NSW, Australia), calculated as the absolute value when the mandible was in the retrognathic position (millimeters from zero) plus the absolute value when the mandible was in the prognathic position (millimeters from zero).
Randomized trial
All patients were fitted with (a) a standard oronasal mask (Quattro; ResMed, Sydney Australia), (b) under-chin oronasal mask (Forma; Fisher & Paykel Healthcare, Auckland, New Zealand), and (c) their own nasal cushion mask (of either manufacturer). The masks were adjusted until leak was <20 l/min with CPAP delivered at 8 cmH2O while the patients were awake and in supine position for at least 10 min; if this was not possible, then the patients were excluded at this point. The patients were issued with a ResMed S9 device and were randomized using a (1,2) urn randomization procedure [24] to receive either auto-adjusting PAP (APAP) or standard CPAP for seven nights at home using their manually titrated pressure, with immediate crossover to the alternate arm. APAP was set to vary between 4 and 20 cmH2O. During each seven-night period, the patients were instructed to use their own nasal cushion mask for three nights and each of the oronasal masks for two nights, also randomized using the aforementioned procedure.
All masks have a certain degree of intentional leak through the exhalation ports to prevent re-breathing, which will vary depending on the mask design and the pressure delivered. Most modern CPAP/APAP devices enable the user to enter the mask type being used so that accurate intentional leak can be subtracted from total leak, giving unintentional leak data (comprising mouth leak and/or leak around the seal). However, this option is available only when using a mask made by the same manufacturer as the device. Given that masks designed by different manufacturers were used in this study, the generic “full face mask” and “nasal mask” settings were used on the appropriate nights.
Details on the median, maximum and 95th percentile pressure, median, maximum and 95th percentile unintentional leak, residual AHI, and adherence for each night were downloaded from the device at the conclusion of the trial. Patients filled in a diary, detailing the position they slept in each night and the amount of caffeine, alcohol, and prescription medications consumed throughout the 2-week protocol. Although the data analyst remained blinded, it was not possible to blind patients as to their mask usage.
Statistical analysis
All analyses were performed using SPSS (Version 18.0; NY, USA). Comparisons between mask types were made using repeated-measures ANOVA (parametric) or Friedman’s ANOVA (non-parametric). Post-hoc analyses between the three mask types were conducted only when initial tests were statistically significant at p ≤ 0.05, using dependent t-tests (parametric) or Wilcoxon tests (non-parametric). A Bonferroni correction was used, such that post-hoc analyses were considered as statistically significant when p ≤ 0.0167 (0.05/3). More details regarding the study procedure and analyses are available from the corresponding author.
Results
Study sample
Figure 1 shows a flowchart of the study protocol. Fourteen patients gave their consent and underwent an initial mask fit while awake in the supine position. At this point, one patient was excluded due to unacceptable leak using the Forma (>20 l/min). Ten of the remaining 13 patients used ResMed nasal cushion masks throughout the study (Micro or Activa), while three used Fisher & Paykel nasal cushion masks (HC405, HC406, or HC407). Patients reported sleeping in the same position across each arm and did not markedly change their regular caffeine, alcohol, or medication intake.
One further patient dropped out during the first arm (CPAP) due to an unwillingness to use either of the oronasal masks; a total of 12 patients therefore completed the 2-week protocol. The only missing data were due to skipped nights of treatment, comprising six nights out of a total of 168 (12 patients, 14 night protocol; 3.6% missing data). However, because the two or three night’s usage for each mask was averaged, a complete data set was available for all 12 patients.
Descriptive data are shown in Table 1. Patients were obese with increased neck circumference; most had a low soft palate (75% with Mallampati Grade II or more) and a normal incisal relationship (one patient class III underbite, all others class I). Average adherence was high at >6 h per night, with no significant differences between mask types (p > 0.05).
Differences in pressure delivered between masks
There was no significant difference in the 95th percentile pressure delivered with APAP between the nasal mask (median 11.07, IQR = 3.30 cmH2O), under-chin oronasal mask (median 11.10, IQR = 2.60 cmH2O), or standard oronasal mask (median 11.15, IQR = 2.22 cmH2O; λ 2(2) = 0.83, p = 0.66 (see Fig. 2)). The average 95th percentile pressure delivered with both of the oronasal masks was within 2.5 cmH2O of the nasal mask for nine of the 12 patients. The remaining three patients with a >2.5-cmH2O pressure difference (represented in Fig. 2 as dashed lines) were not distinguishable in terms of BMI, neck circumference, waist–hip ratio, mandibular protrusion, Mallampati score, or incisal relationship.
Mean 95th percentile pressure with APAP using the nasal, under-chin oronasal (Forma), and standard oronasal (Quattro) masks for each individual patient (p = 0.66, overall). Patients used each mask for two to three nights, and these data were averaged. The three dashed lines indicate patients with a difference of ±2.5 cmH2O between any two mask types
Differences in residual AHI between masks
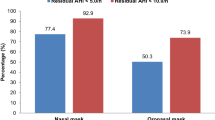
There was a significant difference in residual AHI during the CPAP arm between the nasal, under-chin oronasal, and standard oronasal masks (median 0.61, IQR = 1.18; median 1.70, IQR = 4.04; and median 2.48, IQR 3.74 events/h, respectively; λ 2(2) = 7.17, p = 0.03; see Fig. 3); however, all were within the optimal treatment range of <5 events/h. Only one patient had a mean difference in residual AHI ≥5 events/h between the nasal mask and under-chin oronasal mask (26.3 events/h higher with the under-chin oronasal mask; visible in Fig. 3); these data are likely confounded by the very high leak recorded on these two nights (median 61.2 l/min; 95th percentile 106.8 l/min). When this data point was removed for statistical analysis, the difference in residual AHI between masks remained significant (λ 2(2) = 2.64, p = 0.04).
Mean residual AHI with CPAP using the nasal, under-chin oronasal (Forma), and standard oronasal (Quattro) masksm (p = 0.03, overall). Patients used each mask for two to three nights, and these data were averaged. The dashed line represents the optimal treatment range of AHI <5 events/h. Asterisk, statistical significance using Bonferroni correction of p ≤ 0.0167; n/s non-significant
Mask leak
Maximum leak during mask fitting (awake in the supine position using 8-cmH2O pressure) was 8.8 ± 3.2, 13.6 ± 3.9, and 9.6 ± 3.7 l/min with the nasal, under-chin oronasal, and standard oronasal masks, respectively (significant difference across masks, λ 2(2) = 14.48, p = 0.001).
The 95th percentile leak was significantly different across masks during both the APAP (F(2, 22) = 7.61, p = 0.003) and CPAP arms (F(2, 22) = 7.99, p = 0.002). Post-hoc analyses of the APAP data indicated that the 95th percentile leak with the nasal mask was significantly lower than both the under-chin oronasal mask (t(11) = −3.72, p = 0.002) and standard oronasal mask (t(11) = −3.41, p = 0.003). Post-hoc analyses of the CPAP data indicated that the 95th percentile leak with the nasal mask was significantly lower than the under-chin oronasal mask (t(11) = −3.39, p = 0.001) but not the standard oronasal mask (t(11) = −2.41, p = 0.02). There were no significant differences between the two oronasal masks during either APAP or CPAP use (both p > 0.0167) (Table 2). During the APAP arm, only one patient had a 95th percentile leak above 20 l/min with the nasal mask (36.40 l/min), while 50% had unacceptably high leak with the under-chin oronasal mask (highest 95th percentile leak 96.6 l/min) and 41.7% had unacceptably high leak with the standard oronasal mask (highest 95th percentile leak 102.0 l/min).
Correlations with upper airway shape and body habitus
The differences in 95th percentile pressure during APAP between the nasal and under-chin oronasal masks and between the nasal and standard oronasal masks were investigated for correlation with BMI, neck circumference, waist–hip ratio, and mandibular protrusion. There were no significant relationships, and the effect sizes (r p) were all <0.20. ANOVA indicated no significant differences of these variables across Mallampati categories.
Discussion
In obese patients with severe OSA, this single-blinded pilot randomized controlled trial found no significant difference in the mean, 95th percentile, or maximum pressure recorded during APAP use between nasal, standard oronasal (Quattro), or under-chin oronasal (Forma) mask designs. Three of the twelve patients had 95th percentile pressure differences of >2.5 cmH2O between mask types which could be problematic in a clinical setting; however, the trend was not always towards higher pressure requirement for oronasal masks, and these patients were not distinguishable from the whole group when analyzing body habitus and upper airway shape.
Our results concerning pressure requirement are therefore in agreement with Beecroft et al. [15], who used manual titrations rather than APAP data to determine therapeutic CPAP with nasal and standard oronasal masks. The pressure difference between these masks was larger in the study of Beecroft et al. (2.0 cmH2O compared with no mean difference in the current study), possibly due to the recruitment of patients with a larger spread of disease severity and therefore CPAP requirement. Similarly, our results are in agreement with Teo et al. who used the same standard oronasal mask (ResMed Quattro) and also reported a non-significant pressure difference but significantly increased leak compared with a nasal mask [16]. We have extended the findings of these two trials by including the assessment of the under-chin oronasal mask design, as well as a variety of measurements of upper airway shape and body habitus.
In contrast with Prosise et al. [14], we found a significant difference between the nasal mask and standard oronasal mask in terms of the residual AHI recorded during CPAP use; however, the median difference of 1.09 events/h was small and unlikely to be clinically significant. The mean residual AHI was above the optimal treatment cutoff (5 events/h) for only two patients, most likely due to high leak. As part of the inclusion criteria, maximum leak during the awake trial with CPAP was required to be <20 l/min on each mask when fitted by the researcher. Despite this, the 95th percentile leak was ≥30 l/min for both full-face masks during the APAP and CPAP arms when the masks were fitted by the patients at home.
Current clinical guidelines state that, “there is insufficient evidence for what constitutes a significant leak… however, in general, an unacceptable leak for PAP is one that is substantially higher than the leak recorded at a given pressure from a well-fitted, applied and secured interface” [17] (page 166). By this criterion then, the 95th percentile leak levels with both oronasal masks were unacceptable when compared to the nasal mask (differences in leak of >30 l/min). It was reported in 2005 that an early-model APAP device underestimated pressure requirement when leak reached 30 l/min [25], and it is known that high leak is associated with poor PAP adherence [26, 27]. We therefore believe that the high leak levels reported here are clinically, as well as statistically, significant.
No measure of upper airway shape or body habitus measured were significantly associated with the difference in 95th percentile pressure between the nasal and under-chin oronasal mask or the difference in 95th percentile pressure between the nasal and standard oronasal mask. Although the effect sizes were all small/medium (r p < 0.20), a subsequent larger study may detect such associations. Alternatively, there may be other important anatomical contributions that we have not investigated here.
The randomized crossover nature of the study design meant that we recruited patients with patent nasal airways so that accurate data could be obtained during use of the nasal mask. This limits the generalizability of our study. However, patients undergoing a parallel-arm study design would not be randomized, as mouth breathers would not be able to be allocated to the nasal mask group, potentially introducing uncontrolled bias and variability. Our aims were mainly concerned with swapping a patient from a nasal to an oronasal mask following titration; a mouth-breathing patient would most likely be titrated on an oronasal mask, thereby avoiding this issue.
Due to financial constraints, we chose to analyze the metrics recorded by the S9 device, allowing data collection to occur in the patients’ homes. Very few studies have systematically examined the accuracy of machine-interpreted indexes such as the AHI, and none that we are aware of has evaluated the S9 device. For the primary comparison of the 95th percentile pressure delivered during S9 APAP with each mask, however, we believe that the use of the APAP device was appropriate given that many laboratories now use these data to assign an ongoing therapeutic CPAP pressure in the clinical setting. More accurate results would have been obtained by averaging data collected over a week or more for each mask type, given that a laboratory using an APAP protocol to determine therapeutic pressure would be unlikely to make this decision based on only two to three nights of data. The lack of in-laboratory PSGs undertaken with each mask also meant that we were unable to objectively control for sleep position, which can affect the therapeutic pressure requirement [28]; instead we relied on subjective report. Using the generic compensation for intentional leak is a regrettable yet unavoidable limitation of our study, given the focus on comparing masks of different manufacturers with the same device. Another major limitation of this study was the small sample size, as we intended to use these data to perform post-hoc power analyses to determine an appropriate sample size for a subsequent study. However, as hypothesized, we found significant differences between masks concerning the residual AHI with CPAP and several leak measures, so the sample size appears adequate for these analyses. We did not perform a power analysis to determine a sample size to detect the difference in 95th percentile pressure with APAP as all three masks were within 0.5 cmH2O with reasonably low variance. Finally, more insight would have been gained if we had included a third arm, during which patients used CPAP at the pressure indicated during their APAP arm while using the nasal mask in order to determine whether using this pressure led to a significantly higher residual AHI with either of the oronasal mask designs.
Despite anecdotal questioning as to whether nasal and oronasal masks lead to different pressure requirements, levels of residual disease, or system leak, this is the first study that we are aware of that has assessed two distinct designs of oronasal masks compared with a nasal mask. The rigorous design of the study, the collection of multiple measures of leak, and the use of objective measures of upper airway shape and body habitus are further strengths of the current study.
The findings of the current study highlight leak as the major difficulty in the use of oronasal masks, despite detecting no significant difference in APAP 95th percentile pressure between nasal and oronasal masks, and recording levels of residual disease during CPAP within the acceptable treatment range for all masks. The fact that the researcher was able to obtain an acceptable mask fit during an awake in-laboratory trial which was not able to be replicated by the patients when at home emphasizes the need for a close follow-up of patients following changes of mask design.
References
Mulgrew AT, Ryan CF, Fleetham JA, Cheema R, Fox N, Koehoorn M, Fitzgerald JM, Marra C, Ayas NT (2007) The impact of obstructive sleep apnea and daytime sleepiness on work limitation. Sleep Med 9(1):42–53
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235
Nowak M, Kornhuber J, Meyrer R (2006) Daytime impairment and neurodegeneration in OSAS. Sleep 29(12):1521–1530
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T (2008) Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol 52(8):686–717
Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O’Connor GT, Rapoport DM, Redline S, Resnick HE, Robbins JA, Shahar E, Unruh ML, Samet JM (2009) Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 6(8):e1000132
Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR (2008) Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 31(8):1079–1085
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, Boehlecke B, Brown TM, Coleman J Jr, Friedman L, Kapen S, Kapur VK, Kramer M, Lee-Chiong T, Owens J, Pancer JP, Swick TJ, Wise MS (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29(3):375–380
Svensson M, Holmstrom M, Broman JE, Lindberg E (2006) Can anatomical and functional features in the upper airways predict sleep apnea? A population-based study in females. Acta Otolaryngol 126(6):613–620
Vos W, De Backer J, Devolder A, Vanderveken O, Verhulst S, Salgado R, Germonpre P, Partoens B, Wuyts F, Parizel P, De Backer W (2007) Correlation between severity of sleep apnea and upper airway morphology based on advanced anatomical and functional imaging. J Biomech 40(10):2207–2213
Isono S, Remmers JE, Tanaka A, Sho Y, Sato J, Nishino T (1997) Anatomy of pharynx in patients with obstructive sleep apnea and in normal subjects. J Appl Physiol 82(4):1319–1326
Akashiba T, Kosaka N, Yamamoto H, Ito D, Saito O, Horie T (2001) Optimal continuous positive airway pressure in patients with obstructive sleep apnoea: role of craniofacial structure. Respir Med 95(5):393–397
Chai CL, Pathinathan A, Smith B (2006) Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev (4):CD005308
Mortimore IL, Whittle AT, Douglas NJ (1998) Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax 53(4):290–292
Prosise GL, Berry RB (1994) Oral–nasal continuous positive airway pressure as a treatment for obstructive sleep apnea. Chest 106(1):180–186
Beecroft J, Zanon S, Lukic D, Hanly P (2003) Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest 124(6):2200–2208
Teo M, Amis T, Lee S, Falland K, Lambert S, Wheatley J (2011) Equivalence of nasal and oronasal masks during initial CPAP titration for obstructive sleep apnea syndrome. Sleep 34(7):951–955
Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, Parthasarathy S, Quan SF, Rowley JA (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 4(2):157–171
Dimsdale JE, Loredo JS, Profant J (2000) Effect of continuous positive airway pressure on blood pressure: a placebo trial. Hypertension 35(1 Pt 1):144–147
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques, and scoring systems for sleep stages of human subjects. UCLA Brain Information Service/Brain Research Institute, Los Angeles
American Sleep Disorders Association (1992) EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force. Sleep 15(2):173–184
American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep 22(5):667–689
Nuckton TJ, Glidden DV, Browner WS, Claman DM (2006) Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep 29(7):903–908
Schulz KF, Grimes DA (2002) Generation of allocation sequences in randomised trials: chance, not choice. Lancet 359(9305):515–519
Coller D, Stanley D, Parthasarathy S (2005) Effect of air leak on the performance of auto-PAP devices: a bench study. Sleep Breath 9(4):167–175
Valentin A, Subramanian S, Quan SF, Berry RB, Parthasarathy S (2011) Air leak is associated with poor adherence to autoPAP therapy. Sleep 34(6):801–806
Baltzan MA, Dabrusin R, Garcia-Asensi A, Sully JL, Parenteau M, Tansimat G, Kassissia I, Wolkove N (2011) Leak profile inspection during nasal continuous positive airway pressure. Respir Care 56(5):591–595
Oksenberg A, Silverberg DS, Arons E, Radwan H (1999) The sleep supine position has a major effect on optimal nasal continuous positive airway pressure: relationship with rapid eye movements and non-rapid eye movements sleep, body mass index, respiratory disturbance index, and age. Chest 116(4):1000–1006
Acknowledgements
We wish to thank all participants who consented to the study and we are grateful to Dr. Hugh Trengrove for his insight into the measures of upper airway shape.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bakker, J.P., Neill, A.M. & Campbell, A.J. Nasal versus oronasal continuous positive airway pressure masks for obstructive sleep apnea: a pilot investigation of pressure requirement, residual disease, and leak. Sleep Breath 16, 709–716 (2012). https://doi.org/10.1007/s11325-011-0564-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-011-0564-3