Abstract
Purpose
Patients with obstructive sleep apnea (OSA) may have subclinical swallowing abnormalities due to progressive mechanical trauma of the pharyngeal tissues caused by snoring. There are few trials on swallowing among OSA patients, and most of them used videoradiography. The aim of this trial was to show swallowing function in OSA patients by nasal fibroscopy.
Method
Eleven patients with OSA diagnosed by polysomnography, with a mean age of 48 ± 14 years, without spontaneous complaints of swallowing, and 14 non-snoring volunteers, with a mean age of 47 ± 12 years, without spontaneous complaints of swallowing, participated in the study. The participants were evaluated using nasal fibroscopy. Each participant was offered diet boluses (5 and 10 ml) such as thin liquids, purée, and solids, and their swallowing function was determined according to the following criteria: (1) premature oral leakage to the pharynx; (2) laryngeal penetration; (3) tracheal aspiration; and (4) pharyngeal stasis.
Results
Sixty-four percent of the OSA patients presented premature oral leakage, 55% presented pharyngeal stasis of the bolus after swallowing, and we did not observe laryngeal penetration or tracheal aspiration. There were no subclinical manifestations in the control group.
Conclusion
OSA patients presented subclinical manifestations of abnormal swallowing, when analyzed using nasal fibroscopy, possibly associated with neuromuscular injury caused by snoring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a sleep-related breathing disorder in which the upper airway is obstructed but the respiratory effort continues. This disorder is characterized by recurrent sleep-induced collapse of the pharyngeal airway, and arousal from sleep is required in order to reestablish airway patency [1].
There is evidence that upper-airway mucosal sensory function in the oropharynx is impaired among patients with OSA [2–4]. The pathophysiological mechanism is believed to be local neurogenic lesions in the oropharynx caused by the low-frequency vibration of habitual snoring during OSA [5, 6]. Although several proposed mechanisms, including mechanical or inflammatory-related neuropathic changes that develop secondary to the soft-tissue trauma caused by vibration, have been demonstrated, the mechanism for mucosal sensory impairment in OSA remains uncertain.
Normal evocation of the swallowing reflex and subsequent propagation of the bolus through the pharynx are dependent on the adequacy of the pharyngeal anatomical configuration, such as its sensitivity and function [7]. There is an association between snoring and subclinical dysfunction of pharyngeal swallowing [7, 8], and the swallowing mechanism may be affected by mechanical and/or chemical stimuli, including apnea [9, 10].
There are few trials on swallowing among OSA patients. Most of them used videoradiography, which is the “gold standard” examination for analyzing swallowing. The aim of this trial was to show swallowing function in OSA patients by nasal fibroscopy.
Materials and methods
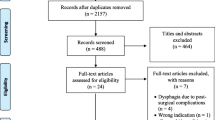
Patients
Eleven consecutive patients referred to the São Paulo Hospital Sleep Laboratory because of snoring and daytime sleepiness were examined clinically and by means of overnight polysomnogram. There were five men and six women, with a mean age of 48 ± 14 years (range 20–65 years) and mean body mass index of 31.55 ± 6.86 kg/m2 (range 21–46 kg/m2). The characteristics of the 11 patients are presented in Table 1.
Volunteers
Fourteen volunteers without snoring and/or sleep apnea confirmed by polysomnography, without spontaneous complaints of swallowing, formed the controls. There were eight men and six women, with a mean age of 47 ± 12 years (range 24–62 years) and mean body mass index of 29.21 ± 3.78 kg/m2 (range 24–35 kg/m2). The characteristics of the 14 controls are presented in Table 2.
None of the participants had previously received any treatment for sleep apnea, nor had they previously been operated in relation to the upper airway. None of the patients suffered from gastroesophageal reflux or dysphagia, and this was confirmed by means of a phonoaudiological clinical evaluation and interview. None of the study patients consumed alcohol or cigarettes, nor did they take hypnotics, sedatives, analgesics, or any medications with known effects relating to ventilation and swallowing, or any histories of neuromuscular disorders.
Sleep assessment
All patients underwent the following tests: overnight polysomnography (PSG), including standard electroencephalographic leads (C4–A1/C3–A2); bilateral electrooculogram; chin and tibialis electromyograms; airflow via nasal pressure cannula and thermistor; thoracoabdominal movements by means of a piezoelectric belt; body position by means of a position sensor; and arterial oxyhemoglobin saturation by means of finger pulse oximetry. All signals were acquired using a digital data-management system (model EQSA-400; Neurotec, Itajuba, MG, Brazil). The assessments were scored manually by a trained, experienced clinical neurophysiologist who was blinded for the purpose of this study. The sleep–wakefulness state was defined in accordance with standard criteria [11]. Obstructive apnea was defined as an episode of cessation of airflow lasting at least 10 s, with persistent respiratory effort. Hypopnea was defined as an episode of reduced airflow or limitation of inspiratory flow on the nasal cannula pressure signal (≥30%), lasting more than 10 s, with associated desaturation of at least 3% or arousal defined in accordance with the American Academy of Sleep Medicine criteria [12].
In this study, OSA was determined by calculating the apnea or hypopnea index (AHI), in which ≥5 episodes/h was classified as mild, ≥15 episodes/h as moderate, and >30 episodes/h as severe [13].
Nasal fibroscopy
The structural and functional swallowing evaluations were made using nasal fibroscopy. All the examinations were recorded on VHS tapes, thus allowing a second look at the images obtained. The nasal fibroscopy equipment used was the Machida 3.2-mm apparatus. The patients were examined in a seated position that was comfortable for swallowing. The nasal fibroscopy equipment was introduced through the patient’s larger nasal orifice, without anesthetics or nasal vasoconstriction. Before the endoscopic examination, all the participants were made aware of the possibility of some discomfort, and they were allowed to stop the examination at any time that they wished. The patients were offered a diet bolus with blue-dyed food, with progressive textures (liquid, soft, and regular) and quantity (5 and 10 ml). The three food types were mineral water, representing thin liquids (L); yoghurt, representing purée (P); and crackers, representing solids (S). Two blinded examiners (one otolaryngologist and one speech therapist) analyzed the anatomical structures and the functional aspects of the swallowing events using the following criteria: (1) premature oral leakage was defined if the bolus entered the pharynx without eliciting the swallowing reflex; (2) laryngeal penetration was defined if the bolus penetrated into the laryngeal vestibule but not below the vocal cords; (3) tracheal aspiration was defined if the bolus penetrated below the vocal cords; and (4) pharyngeal stasis was defined if the bolus remained in the pharynx after the swallowing sequence was over. Any disagreements and discrepancies were resolved in consultation with a third examiner (otolaryngologist).
The study protocol was approved by the ethics committee of Universidade Federal de São Paulo (UNIFESP), São Paulo, Brazil (no. 0303/06). All study participants gave their informed consent.
Results
Swallowing dysfunction was observed among the OSA patients. These events were classified as either premature oral leakage or pharyngeal stasis after swallowing, in relation to the control group. No cases of laryngeal penetration or tracheal aspiration were observed in either group. Repeated premature bolus leakage was observed in seven (64%) of the 11 OSA patients.
Six (55%) of the 11 OSA patients demonstrated pharyngeal stasis in the valleculae after the propagation wave had passed the pharynx and inhibition of respiration had ceased. We did not observe any cases of bolus leakage or pharyngeal stasis in the control group.
The OSA group displayed swallowing dysfunction classified as follows: seven patients (63.6%) with severe sleep apnea (AHI ≥ 25); four patients (36.3%) with moderate sleep apnea (AHI ≥ 15); and none of the patients with mild sleep apnea (AHI ≥ 5). In the control group, without sleep apnea (AHI < 1), we did not observe any subclinical dysfunction.
Discussion
The results from this study reinforce that OSA patients are at higher risk of developing subclinical pharyngeal swallowing dysfunction, compared with controls, regardless of the testing technique used, both when analyzed using nasal fibroscopy and when confirmed using videoradiography [10].
In the present study, 64% of the patients displayed premature bolus leakage. Premature bolus delivery during the oral phase is the most frequent disorder seen in patients with neurological impairments and may result either from poor tongue control or from delayed swallowing reflex [14].
Six of the 11 OSA patients (55%) displayed pharyngeal stasis, thus implying a risk of aspiration. However, no aspiration below the glottic level was observed in this study, which explains why the patients with swallowing dysfunction remained asymptomatic. If the sensitivity of the soft palate and oropharynx is disturbed, there is a risk that a bolus will pass down to a level where sensitivity remains unaffected before the swallowing reflex is triggered [1].
We observed that the duration of the illness (snoring) and not the age of OSA patients had a negative impact on swallowing function. Furthermore, BMI seemed not to interfere in swallowing dysfunction.
However, the risk of pharyngeal swallowing dysfunction did not increase significantly with increasing AHI. We suppose that the high frequency of swallowing dysfunction is probably secondary to the local neurogenic lesions in the soft palate and oropharynx due to vibration trauma caused by snoring [1, 4].
Hypertrophy of the oropharyngeal lumen, collapse or hypotonicity of the tongue and oropharyngeal muscles, and collapse of the lateroposterior pharyngeal walls as revealed by nasal fibroscopy are accepted factors in airway obstruction in OSA patients [15]. It seems that typical OSA patients have redundant pharyngeal tissue and a large tongue, which may affect swallowing [16].
Nasal fibroscopy allows quantitative and qualitative assessment of swallowing, and our findings corroborate with videoradiographic studies [17]. Furthermore, nasal fibroscopy is simple to perform, presents good reproducibility, and is acceptable to patients [18–21].
A case report study [8] mentioned two cases of OSA in whom the swallowing reflex was impaired before the start of nasal continuous positive airway pressure (NCPAP) and was found to have improved 1 year after NCPAP. These cases suggest that impaired swallowing reflex may be reversible through OSA treatment. However, it is also possible that this impaired swallowing reflex may be reversible through methods to increase the upper airway tonus [22].
The limitation of this method is that no evaluation of the laryngopharyngeal lumen can be performed during the swallowing since a white out occurs at the pharyngeal swallowing phase.
Conclusion
OSA patients presented subclinical manifestations of abnormal swallowing, as seen using nasal fibroscopy, which were possibly associated with neuromuscular injury caused by snoring. The duration of the illness and severity of the OSA seemed to be associated with the swallowing dysfunctions in our sample.
References
Guilleminault C, Tilkian A, Dement WC (1976) The sleep apnea syndrome. Annu Rev Med 27:465–485
Nguyen ATD, Jobin V, Payne R, Beauregard J, Naor N, Kimoff J (2005) Laryngeal and velopharyngeal sensory impairment in obstructive sleep apnea. Sleep 28(5):585–593
Friberg D, Ansved T, Borg K, Carlsson-Nordlander B, Larsson H, Svanborg V (1998) Histological indications of a progressive snorers disease in an upper airway muscle. Am J Respir Crit Care Med 157:586–593
Kimoff RJ, Sforza E, Champagne V, Ofiara L, Gendron D (2001) Upper airway sensation in snoring and obstructive sleep apnea. Am J Respir Crit Care Med 164:250–255
Frieberg D, Gazelius B, Lindblad LE, Nordlander B (1998) Habitual snorers and sleep apnoics have abnormal vascular reactions of the soft palatal mucosa on afferent nerve stimulation. Laryngoscope 108:431–436
Larsson H, Carlsson-Nordlander B, Lindblad LE, Norbeck O, Svanborg E (1992) Temperature thresholds in the oropharynx of patients with obstructive sleep apnea syndrome. Am Rev Respir Dis 146:1246–1249
Jäghagen EL, Berggren D, Isberg A (2000) Swallowing dysfunction related to snoring: a videoradiographic study. Acta Otolaryngol 120:438–443
Okada S, Ouchi Y, Teramoto S (2000) Nasal continuous positive airway pressure and weight loss improve swallowing reflex in patients with obstructive sleep apnea syndrome. Respiration 67:464–466
Teramoto S, Sudo E, Matsuse T, Ohga E, Ishii T, Ouchi Y, Fukuchi Y (1999) Impaired swallowing reflex in patients with obstructive sleep apnea syndrome. Chest 116(1):17–21
Jäghagen EL, Franklin KA, Isberg A (2003) Snoring, sleep apnoea and swallowing dysfunction: a videoradiographic study. Dentomaxillofac Radiol 32:311–316
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques and scoring system of sleep stages in human subjects. Brain Information Service/Brain Research Institute, UCLA, Los Angeles
American Academy of Sleep Medicine (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definitions and measurements techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep 22(5):667–689
Bastian RW (1999) Videoendoscopic evaluation of patients with dysphagia: an adjunct to the modified barium swallow. Otolaryngol Head Neck Surg 104:339–350
Veis SL, Logemann JA (1985) Swallowing disorders in persons with cerebrovascular accident. Arch Phys Med Rehabil 66:372–375
Fujita S, Conway W, Zurick F, Roth H (1981) Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 89:923–924
Zohar Y, Grusko I, Sulkes J, Melloul MM (1998) Oropharyngeal scintigraphy: a computerized analysis of swallowing in patients with obstructive sleep apnea. Laryngoscope 108:37–41
Aviv JE (2000) Clinical assessment of pharyngolaryngeal sensitivity. Am J Med 108(Suppl 4a):68S–72S
Kaye GM, Zorowitz RD, Baredes S (1997) Role of flexible laryngoscopy in evaluating aspiration. Ann Otol Rhinol Laryngol 106(8):705–709
Lorenz R, Jorysz G, Tornieporth N, Classen N (1993) The gastroenterologist’s approach to dysphagia. Dysphagia 8(2):79–82
Wu CH, Hsiao TY, Chen JC, Chang YC (1997) Evaluation of swallowing safety with fiberoptic endoscope: comparison with videofluoroscopic technique. Laryngoscope 107(3):396–401
Yanagisawa E, Owens TW, Strothers G, Honda K (1983) Videolaryngoscopy: a comparison of fiberoptic and telescopic documentation. Ann Otol Rhinol Laryngol 92(5pt1):430–436
Valbuza JS, de Oliveira MM, Conti CF, Prado LB, de Carvalho LB, do Prado GF (2010) Methods for increasing upper airway muscle tonus in treating obstructive sleep apnea: systematic review. Sleep Breath 14(4):299–305
Author information
Authors and Affiliations
Corresponding author
Additional information
Juliana Spelta Valbuza and Márcio Moysés de Oliveira contributed equally to this work.
Rights and permissions
About this article
Cite this article
Valbuza, J.S., de Oliveira, M.M., Zancanella, E. et al. Swallowing dysfunction related to obstructive sleep apnea: a nasal fibroscopy pilot study. Sleep Breath 15, 209–213 (2011). https://doi.org/10.1007/s11325-010-0474-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-010-0474-9