Abstract
Purpose
To evaluate the effect of pharyngeal surgery on swallowing pattern in patients with obstructive sleep apnea syndrome (OSAS), and to compare two surgical techniques: uvulopalatopharyngoplasty (UPPP) and expansion pharyngoplasty (EP), through videofluoroscopy.
Methods
Longitudinal prospective cohort, in a tertiary referral center. 17 adult patients were enrolled this study, divided into two groups: patients who underwent UPPP (n = 10) or EP (n = 7). Swallowing videofluoroscopy (for both liquid and pasty consistences) was assessed at three different periods: before surgery, and at 14 and 28 days following surgery. Comparisons were performed between pre- and post-operative (PO) swallowing conditions in the same patient, and between surgical techniques.
Results
Asymptomatic OSAS patients already presented altered swallowing pattern before surgery. Both surgical procedures led to an increased hyoid movement time and an increased frequency of laryngeal penetration in early PO during liquid ingestion. For pasty consistency, both techniques reduced velum movement time and increased pharyngeal transit time and the rate of stasis in hypopharynx. All these parameters reached or tended to reach the pre-operative indices at day PO 28.
Conclusions
OSAS patients show sub-clinical changes in swallowing pattern before surgery. Both surgical techniques are related to transitory changes in swallowing biomechanics. Complete or partial reversal to pre-operative swallowing parameters occurs 1 month after both surgery techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea syndrome (OSAS) is the most critical respiratory sleep disorder due to its high prevalence [1, 2], as well as to its associated morbidity, mortality, and reduced quality of life [3].
Several different pharyngeal surgeries have been proposed to treat OSAS. The uvulopalatopharyngoplasty (UPPP) is the oldest technique, and also the better studied. Nevertheless, even in most favorable patients, literature data indicate a success rate of about 50% with this procedure [4]. In our center, the success rate of UPPP among OSAS patients with Friedman I or II was 44% [5].
With these results, new pharyngoplasties have been proposed to treat OSAS; most of them focus on avoiding the lateral pharyngeal collapse, frequently observed after UPPP. Among the pharyngoplasties reported in the literature, two techniques proved to have better clinical and polysomnographic outcomes than UPPP: lateral pharyngoplasty [6] and expansion pharyngoplasty (EP) [7].
Some studies pointed that some OSAS patients, even at baseline condition, may present changes in swallowing, such as premature loss of food to hypopharynx, food stasis in the hypopharynx, and laryngeal penetration [8,9,10]. Two of these studies showed that the frequency and the intensity of these changes are not related to OSAS severity [9, 10].
Of notice, some patients complain of dysphagia after pharyngeal surgeries for OSAS. Although this seems to be a significant clinical complaint, very few studies have specifically addressed this topic, particularly in a prospective setting. This study aimed to assess the swallowing changes observed in patients with OSAS before and up to 1 month after pharyngeal surgery, comparing two techniques: UPPP and EP.
Materials and methods
This study recruited patients with OSAS diagnosis and indicated to surgical treatment, followed at Sleep Respiratory Disorders Outpatient Clinic–Clinics Hospital, Medical School of Ribeirão Preto, University of São Paulo. The study has been approved by local IRB, under the number 3561/2010.
To be indicated to surgery, all the patients underwent clinical evaluation (including BMI), ENT exam (including Mallampati and Friedman Scales), and diagnostic nocturnal polysomnography (examined with a digital polygraph-Bio-Logic®, and a SleepScan Vision Analysis software, version 2.03.05), according to American Academy of Sleep Medicine parameters-2007 [11].
For the study specifically, we included only patients aged from 20 to 50 years, and with BMI lesser than 35 kg/m2, as both age and obesity could influence swallowing patterns. Exclusion criteria also comprised patients with Friedman III or IV, with neurological disorders, genetic syndromes, and patients who have already undergone previous surgical treatment for OSAS.
The patients who accepted to participate were then randomly enrolled in one of these two groups: patients undergoing UPPP and patients undergoing EP. All the surgeries were performed by the same ENT team and supervised by the same surgeon (DSK).
This study was approved by local IRB, under the number 3561/2010.
Swallowing videofluoroscopy
Swallowing videofluoroscopy was performed in three distinct periods: before surgery—T1; on the 14th PO day—T2; and on the 28th PO day—T3. All three evaluations were performed by the same speech therapist and by the same technician, in fluoroscopic equipment, model BV Pulsera (Philips Medical System, Holland). The images were captured at the acquisition rate of 29.97 frames per second, in a lateral view. The exams were recorded and analyzed frame per frame with the Vegas Pro 10.0 Program-Sony.
Before videofluoroscopy, in each moment, all patients answered a standardized questionnaire concerning swallowing symptoms, preferred consistency of the meal at the instant, and pain. A visual analog scale (from 0 to 10, considering 0 “no pain” and 10 “the most intolerable pain”) was also employed mainly for pain.
During the exam, the patients ingested two consistencies of the meal: liquid (water 50 mL + barium sulfate Opti-Bar® 15 mL), and pasty (water 50 mL + barium sulfate Opti-Bar® 15 mL + one teaspoon of Thick & Easy, Hormel Health Labs, USA). For both of them, the patient was instructed to swallow three times of 7 mL each, and the volume was measured in a syringe.
The following parameters were examined [12]:
-
premature loss to hypopharynx (PLH) indicated as present or absent;
-
velum movement time (VMT) interval in seconds between the first movement of soft palate into nasopharynx direction, until its return to rest position, Fig. 1;
-
pharyngeal transit time (PTT) interval in seconds from food passing through posterior nasal spine until it enters entirely into the esophagus;
-
hyoid movement time (HMT) interval in seconds between the first movement of hyoid bone into anterosuperior direction until it returns to its rest position, Fig. 2;
-
pharyngeal constriction time (PCT) interval in seconds from the maximal pharyngeal contraction until the pharynx returns to its rest position;
-
food stasis in hypopharynx (FSH) indicated as present (any volume in any pharyngeal area after swallowing) or absent;
-
laryngeal penetration (LP) reported as present (if contrast reached airways, not surpassing the vocal folds) or absent.
All the exams were randomized and then analyzed by two speech therapists. The level of agreement between exams was measured by Kappa coefficient and by intraclass correlation coefficient [13]. In all parameters, the inter-observer agreement was extremely high (minimal value of 0.97) and highly significant.
Statistical analysis
The program PROC POWER, from Software SAS version 9.2, was used to calculate the sample size. After a pilot study, a statistician calculated the number of patients per group, considering the power test at 90% and the level of significance at 5%. The minimum of seven individuals for each group was determined.
The linear model of mixed effects was employed in all analyses, considering age, BMI and gender as influencers, in a paired test to analyze the effect of surgery in the same patient, and non-paired test to compare the surgical techniques. These models assume that residues present a normal distribution [14]. To fulfill this purpose, the values were transformed into logarithmic, and orthogonal contrasts were estimated. The programs PROC MIXED and PROC TEST, both from Software SAS version 9.2, were employed.
Results
17 patients (10 male and 7 female) were included, with ages ranging from 24 to 49 years. UPPP group comprised 10 participants (6 male and 4 female) with mean age 36.3 ± 7.7 years and mean BMI 28.5 ± 3.9. EP group included 7 participants (4 male and 3 female) with mean age 37.0 ± 8.7 years and mean BMI 30.2 ± 3.7. There was no significant difference between groups regarding age (95% CI − 9.7; 8.3, P = 0.87), nor BMI (95% CI − 5.9; 2.6, P = 0.42). Descriptive data at the pre-operative moment can be better visualized in Table 1.
The groups were also similar in pre-operative AHI: patients who underwent UPPP presented a pre-operative AHI of 36.3 ± 7.7, while patients who underwent EP had a pre-operative AHI of 37 ± 8.7. Post-operative AHI was performed in 13 patients (9 from UPPP group and 4 from EP group), decreasing to 10.4 ± 11.6 for the UPPP group, and to 9.7 ± 8.6 for the EP group. Statistical analysis between pre- and post-operative moments was not performed since the number of patients in group EP (n = 4) was too small. BMI did not differ after surgery, for either group.
The patients did not complain about dysphagia or choking before surgery. On the 14th day, the majority of the patients (nine among UPPP patients and five among EP patients) were still eating a soft meal, and four patients in each group were complaining of pain. Mean visual analogic scale (VAS) was 1.2 in UPPP group, and 3.4 in EP group. Choking and coughs were present in 1 patient in UPPP group and 2 patients in group EP. No patients reported nausea or vomiting.
On the 28th day, only one patient (in the EP group) still preferred the soft meal, all the others returned to habitual ingestion. The pain was mentioned by 2 patients in each group, and mean VAS was 0.4 in UPPP group and 0.6 in EP group. Choking and coughs were reported only by one patient, belonging to UPPP group. No patient complained of nausea or vomiting.
Effect of UPPP on swallowing
The mean values of the analyzed parameters are presented in Table 2, and the statistical values are listed in Table 3.
During liquid ingestion, UPPP significantly increased hyoid movement time on 14th PO day (1.18 ± 0.31 at T1 vs. 1.30 ± 0.35 at T2, P < 0.05); this parameter slightly decreased on 28th PO day (to 1.28 ± 0.32), and it was no longer significantly different from T1 at T3.
Premature loss to hypopharynx (PLH), food stasis in hypopharynx (FSH) and laryngeal penetration (LP) were, respectively, present in 6, 1 and 1 patients at T1. All these parameters increased in frequency at T2 (to 8 patients with PLH, 2 with FSH and 6 with LP), and decreased at T3 (to 3 patients with PLH, 1 with FSH and 2 with LP).
For pasty consistency, UPPP progressively decreased pharyngeal constriction time throughout times (0.67 ± 0.21 at T1 vs. 0.59 ± 0.20 at T2 vs. 0.55 ± 0.19 at T3), and significant difference (P < 0.01) was observed between T1 and T3. Also, velum movement time significantly decreased between T1 and T2 (1.04 ± 0.25 at T1 vs. 0.93 ± 0.14 at T2; P < 0.05), followed by a significant increase at T3 (1.05 ± 0.23, P < 0.01).
PLH was stable for pasty consistency (present in 5 patients in all analyzed moments). However, UPPP led to an immediate increase in frequency of FSH (present in 5 patients at T1, and in 7 patients at T2) and of LP (present in 1 patient at T1, and in 2 patients at T2), followed by an improvement at T3 (1 patient with FSH and 0 with LP).
For all analyses, patients with pre-existing swallowing disturbances had the worst outcome after surgery.
Effect of EP on swallowing
The mean values of analyzed parameters are presented in Table 4, and the statistical values are presented in Table 5.
During liquid ingestion, EP significantly increased pharyngeal transit time (0.66 ± 0.14 at T1 vs. 0.79 ± 0.10 at T2 vs. 0.73 ± 0.11 at T3, being P < 0.01 between T1 and T2 and P < 0.05 between T1 and T3). Hyoid movement time also significantly increased after surgery (1.18 ± 0.30 at T1 vs. 1.35 ± 0.31 at T2 vs. 1.35 ± 0.33 at T3, being P < 0.05 between T1 and T2 and P < 0.01 between T1 and T3).
PLH, FSH, and LP were present, during liquid ingestion, in, respectively, 4, 2 and 1 patients at T1. There was an increase in the presence of these 3 parameters at T2 (to, respectively, 5, 4 and 2 patients), followed by an improvement at T3 (to, respectively, 2, 0 and 0 patients).
For pasty consistency, pharyngeal constriction time decreased immediately after surgery (0.65 ± 0.26 at T1 vs. 0.54 ± 0.22 at T2, P < 0.05), followed by a significant increase in this parameter at T3 (0.62 ± 0.21, P < 0.05 between T2 and T3). Velum movement time decreased between T1 and T2 (1.04 ± 0.19 at T1 vs. 1.02 ± 0.21 at T2, non-significant difference), and increased at T3 (1.06 ± 0.20, being P < 0.05 between T2 and T3). Hyoid movement time progressively improved after surgery (1.20 ± 0.28 at T1 vs. 1.22 ± 0.28 at T2 vs. 1.33 ± 0.22 at T3), being significantly different (P < 0.05) between T1 and T3 and between T2 and T3.
PLH was not influenced by EP for pasty consistency (present in four patients in all three moments). However, EP increased the frequency of FSH (present in four patients at T1, and in six patients at T2) and of LP (present in 0 patients at T1, and in one patient at T2) at T2, followed by an improvement at T3 (to four patients for FSH and 0 for LP).
For all analyses, patients with pre-existing swallowing disturbances had the worst outcome after surgery.
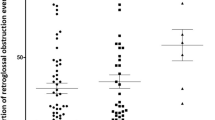
Comparative of surgical techniques
The statistical values comparing both surgeries are presented in Table 6.
There was no statistically significant difference between surgeries regarding any analyzed parameter for liquid ingestion. For pasty consistency, patients who underwent EP presented significantly higher pharyngeal constriction time (P < 0.05) than those submitted to UPPP at T3.
Discussion
The purpose of this study was to address the effect of pharyngeal surgeries on swallowing of adult patients with OSAS, comparing the techniques of UPPP and EP. It is on notice that, even before surgery, these patients already presented altered swallowing pattern. Although this finding has been already described in the literature [8,9,10], it is interesting that the present patients did not spontaneously complain of swallowing symptoms before surgery, maybe because of the concern in other symptoms or morbidities. These findings support that swallowing condition in patients with OSAS should be interrogated by the ENT prior to a pharyngeal surgery, to better identify which patients would be predisposed to swallowing symptoms after surgery. In fact, a recent systematic review showed that swallowing dysfunction is increased in prevalence among patients with OSAS [15].
The displacement and the sustenance of hyoid are essential to protect the airways during swallowing, avoiding laryngeal penetration and aspiration [16], thus, an increased hyoid movement time would be related to a higher probability of food stasis in hypopharynx and of laryngeal penetration. In this study, both surgeries increased the hyoid movement time right after surgery for liquid ingestion. This parameter tended to decrease 1 month after surgery for UPPP but continued to be elevated in EP. Also, hyoid movement time persisted increased in patients submitted to EP for pasty consistency.
At 14th day of surgery, food stasis in hypopharynx was increased in frequency for both consistencies, whereas laryngeal penetration and premature loss to hypopharynx were observed during liquid ingestion. For both groups, these parameters returned to pre-operative values 1 month after surgery. Both laryngeal penetration [8, 10] and food stasis in hypopharynx [8,9,10] have already been reported in OSAS patients, even when they were not submitted to pharyngeal surgery. Some authors report that premature loss is the swallowing change most commonly found in the immediate post-operative period and that this event might occur due to transitory loss of oropharyngeal sensibility after the surgery [17].
Both surgeries also decreased the velum movement time 14 days after surgery, with a recovery of its value on the 28th post-operative day, for pasty consistency. We might infer that this event could be due to edema on the palate. On the 28th day, after the reduction in edema, the tonicity could be recovered to preoperative values. It is worthy of notice that, even with this finding, no patient in our study presented velopharyngeal insufficiency.
Both surgical approaches were related to a decreased pharyngeal constriction time. This finding may be explained by the reduction of the redundant pharyngeal tissue after surgery, with a temporary decrease in contraction of pharyngeal muscles. For those patients who underwent EP, this parameter recovered to pre-operative values, reinforcing that this seems to be a transitory effect of surgery.
The comparison between the two techniques revealed that patients who have undergone EP presented higher pharyngeal constriction time than those submitted to UPPP, on the 28th day after surgery. This event might have occurred due to the anterolateral rotation of palatopharyngeal muscle, as a particular surgical step of this technique, which could increase the pharyngeal area.
Very few studies reported the effect of UPPP on swallowing, and no previous report has investigated these parameters for EP. The present study shows that both techniques are related to changes in swallowing biomechanics, most of them discrete and sub-clinical. Moreover, although the ingestion of pasty food was associated with higher changes in swallowing parameters, laryngeal penetration was especially present during liquid ingestion. Jäghagen et al. [17] and Isberg et al. [18] reported that the most reasonable cause for dysphagia following pharyngeal surgeries would be the loss of oropharyngeal sensibility. Apart from this, we could also assume that post-operative edema, pain, and changes in muscle contraction could also be determinants of this outcome.
It is important to stress that most of the swallowing changes observed in our study were transitory. This is in agreement with the study by Mesti and Cahali [19] in patients submitted to lateral pharyngoplasty. On the contrary, Jäghagen et al. [17] and Isberg et al. [18] reported persistent changes in swallowing pattern, even after 1 year of surgery.
Collectively, our findings point to the importance of considering the identification of swallowing symptoms in patients with OSAS before surgery, to detect patients that could develop dysphagia after surgery. Also, ENT should be aware that the swallowing problems observed after pharyngeal surgery for OSAS are likely to be transitory. This information may also help patients and families to understand possible swallowing problems related to pharyngeal surgeries for OSAS, and how they are expected to evolve over the post-operative period.
Conclusions
OSAS patients already show, before surgery, sub-clinical changes in swallowing pattern. Both UPPP and EP techniques are related to transitory changes in swallowing biomechanics. Recovery to pre-operative levels occurs, in general, 1 month after surgery.
References
Epstein LJ, Kristo D, Strollo PJ Jr et al (2009) Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 5:263–276
Tufik S, Santos-Silva R, Taddei JA, Bittencourt LRA (2010) Obstructive sleep apnea syndrome in the sao paulo epidemiologic sleep study. Sleep Med 11:441–446. https://doi.org/10.1016/j.sleep.2009.10.005
Aurora RN, Casey KR, Kristo D et al (2010) Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep 33:1408–1413
Sher AE, Schechtman B, Piccirillo JR (1996) An American sleep disorders association review the efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 2:156–177
Braga A, Carboni LH, do Lago T, Küpper DS, Eckeli A, Valera FC (2013) Is uvulopalatopharyngoplasty still an option for the treatment of obstructive sleep apnea? Eur Arch Otorhinolaryngol 270:549–554. https://doi.org/10.1007/s00405-012-2042-3
Cahali MB, Formigoni GGS, Gebrim EMMS., Miziara ID (2004) Lateral pharyngoplasty versus uvulopalatopharyngoplasty: a clinical, polysomnographic and computed tomography measurement comparison. Sleep 27:942–950
Pang KP, Woodson BT (2007) Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg 137:110–114. https://doi.org/10.1016/j.otohns.2007.03.014
Jäghagen EL, Berggren D, Isberg A (2000) Swallowing dysfunction related to snoring: a videoradiographic study. Acta Otolaryngol 120(3):438–443. https://doi.org/10.1080/000164800750000702
Schindler A, Mozzanica F, Sonzini G, Piebani D, Urbani E, Pecis M, Montano N (2014) Oropharyngeal dysphagia in patients with obstructive sleep apnea syndrome. Dysphagia 29:44–51. https://doi.org/10.1007/s00455-013-9474-9
Valbuza JS, De Oliveira MM, Zancanella E, Conti CF, Prado LB, Carvalho LB, do Prado GF (2011) Swallowing dysfunction related to obstructive sleep apnea: a nasal fibroscopy pilot study. Sleep Breath 15:209–213. https://doi.org/10.1007/s11325-010-0474-9
Iber C, Ancoli-Israeli S, Chesson A, Quan SF, for The American Academy of Sleep Medicine (2007) The AASM manual for the scoring of sleep and associated events: terminology and technical specifications. 1st edn. AASM, Whestchester
Perry JL, Bae Y, Kuehn DP (2012) Effect of posture on deglutitive biomechanics in healthy individuals. Dysphagia 27:70–80. https://doi.org/10.1007/s00455-011-9340-6
Fleiss J (1975) Measuring agreement between two judges on the presence or absence of a trait. Biometrics 31:651–659
Schall R (1991) Estimation in generalized linear models with random effects. Biometrika 78:719–727
Ghannouchi I, Speyer R, Doma K, Cordier R. Verin E (2016) Swallowing function and chronic respiratory diseases: systematic review. Respir Med 117:54–64. https://doi.org/10.1016/j.rmed.2016.05.024
Kim Y, McCullough GH (2008) Maximum hyoid displacement in normal swallowing. Dysphagia 23:274–279. https://doi.org/10.1007/s00455-007-9135-y
Jäghagen EL, Berggren D, Dahlqvist A, Isberg A (2004) Prediction and risk of dysphagia after uvulopalatopharyngoplasty and uvulopalatoplasty. Acta Otolaryngol 124:1197–1203. https://doi.org/10.1080/00016480410017954
Isberg A, Levring-Jaghagen E, Dahlstrom M, Dahlqvist A (1998) Persistent dysphagia after laser uvulopalatoplasty: a videoradiographic study of pharyngeal function. Acta Otolaryngol 118:870–874
Mesti J, Cahali MB (2012) Evolution of swallowing in lateral pharyngoplasty with stylopharyngeal muscle preservation. Braz J Otorhinolaryngol 78:51–55. https://doi.org/10.5935/1808-8694.20120033
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study has been approved by local IRB (number 3561/2010).
Conflict of interest
All the authors refer that they do not have any conflict related to the article.
Rights and permissions
About this article
Cite this article
Corradi, A.M.B., Valarelli, L.P., Grechi, T.H. et al. Swallowing evaluation after surgery for obstructive sleep apnea syndrome: uvulopalatopharyngoplasty vs. expansion pharyngoplasty. Eur Arch Otorhinolaryngol 275, 1023–1030 (2018). https://doi.org/10.1007/s00405-018-4898-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-4898-3