Abstract
Introduction
Rheumatoid arthritis (RA) is linked to increased cardiovascular morbidity and mortality, not completely explained by traditional risk factors. Importantly, the increased risk occurs despite lower levels of total and low-density lipoprotein cholesterol. Whilst systemic inflammation may be a factor, it is possible that changes in individual lipid species contribute to the increased cardiovascular risk.
Objectives
In the present study, we characterized plasma lipidomic profiles in patients with RA in comparison with healthy controls.
Methods
Patients with RA (n = 32) and age- and gender-matched healthy volunteers (n = 84) were recruited. Fasting plasma lipid profiles were measured using electrospray-ionisation tandem mass spectrometry. 24 lipid classes and subclasses were measured.
Results
Patients with RA had normal total, low-density lipoprotein and high-density lipoprotein cholesterol, but higher triglycerides than controls. Five lipid classes (dihydroceramides, alkylphosphatidylethanolamine, alkenylphosphatidylethanolamine, lysophosphatidylinositol, phosphatidylserine) differed between patients with RA and controls. Then we measured 36 lipid species within these 5 classes and found that 11 lipid species were different between patients with RA and controls. Three lipid classes (dihydroceramides, lysophosphatidylinositol, phosphatidylserine) and 10 lipid species remained significantly associated with RA after adjusting for age, sex, body mass index, current smoking, systolic blood pressure and anti-hypertensive treatment in a binary logistic regression model.
Conclusion
This study has identified lipid alterations in RA. These alterations of lipids warrant further investigation as they may be associated with accelerated atherosclerosis and joint inflammation in patient with RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Rheumatoid arthritis (RA) is a common chronic inflammatory disorder that primarily affects joints. It is well known that RA is strongly linked to accelerated atherosclerosis and increased incidence of cardiovascular events and mortality (Avina-Zubieta et al. 2008, 2012; del Rincon et al. 2001; Han et al. 2006). Although RA patients have an increased prevalence of traditional risk factors such as hypertension, smoking and diabetes, the increased cardiovascular risk in RA cannot be completely explained by traditional cardiovascular risk factors (del Rincon et al. 2001). Therefore, the mechanistic or molecular signaling details that promote accelerated atherogenesis in RA remain to be established.
Furthermore, the relationship between cardiovascular disease and lipid levels in patients with RA seems different from that observed in the general population. In healthy individuals without established inflammatory diseases, the risk of developing atherosclerosis increases progressively with increasing levels of low-density lipoprotein cholesterol (LDL-C) and declines with increasing levels of high-density lipoprotein cholesterol (HDL-C) (Perk et al. 2012). However, in active RA patients, reductions in levels of total cholesterol (TC), LDL-C and HDL-C have been seen, these levels being increased by anti-inflammatory treatment (Peters et al. 2010; Chung et al. 2010; Schimmel and Yazici 2009). In the AMORIS study, despite lower levels of TC, the rate of acute myocardial infarction and ischemic stroke was much higher in RA (Semb et al. 2010). This apparent lipid paradox might be explained by an excessive inflammatory burden in RA patients (Myasoedova et al. 2011). However, it is important to explore other cardiovascular risk factors in patients with RA such as changes in other lipids. In addition, since HDL and LDL are aggregates of many lipid species, investigation into individual lipid species is important. The present study was designed to characterize plasma lipid profiles in patients with RA.
2 Materials and methods
The study was approved by the Human Ethics Research Committee of the Alfred Hospital and all subjects provided written informed consent prior to their participation. All clinical investigation was conducted according to the principles expressed in the Declaration of Helsinki.
2.1 Study subjects
Patients with RA (n = 32) were recruited from the RA Clinic at the Alfred Hospital. RA patients fulfilled the diagnostic criteria for the presence of RA proposed by the American Rheumatism Association (Arnett et al. 1988). Age- and gender-matched healthy volunteers (n = 84) were recruited from the risk evaluation clinic of Baker IDI Heart and Diabetes Institute. Patients and controls were older than 35 years. Subjects with known cerebrovascular, coronary or peripheral vascular disease were excluded. Disease activity was assessed by the severity of joint pain, stiffness, and swelling.
2.2 Participant demographics
On the day of the assessment, a detailed medical history and RA history were obtained. Body weight and height were recorded and BMI was calculated, and waist circumference was measured. Blood pressures were measured in the seated position using an automated sphygmomanometer (HEM-907; Omron). Venous blood samples were obtained after overnight fasting. Fasting plasma lipids [TC, triglycerides (TG), LDL-C and HDL-C], and glucose were determined at the Department of Chemical Pathology of the Alfred Hospital. For each participant, a framingham risk score (FRS) for 10-year ‘hard’ coronary heart disease endpoints was calculated (see http://cvdrisk.nhlbi.nih.gov/calculator.asp).
2.3 Sample preparation and lipid extraction
Total lipid extraction from a 10 µL aliquot of plasma was performed by a single-phase chloroform:methanol (2:1) extraction (Meikle et al. 2011; Weir et al. 2013).
2.4 High-performance liquid chromatography–mass spectrometry analysis
Lipid analysis was performed by liquid chromatography, electrospray ionization–tandem mass spectrometry using an Agilent 1200 liquid chromatography system combined with AB SCIEX API 4000 Q/TRAP mass spectrometer with a turbo-ionspray source (350 °C) and Analyst 1.5 data system. The major lipid species of the following lipid classes and subclasses: dihydroceramide (dhCer), ceramide (Cer), monohexosylceramide (MHC), dihexosylceramide (DHC), trihexosylceramide (THC), GM3 ganglioside (GM3), sphingomyelin (SM), phosphatidylglycerol (PG), phosphatidylinositol (PI), phosphatidylethanolamine (PE), phosphatidylcholine (PC), phosphotidylserine (PS), lysophosphatidylethanolamine (LPE), alkylphosphatidylethanolamine [PE(O)], alkenylphosphatidylethanolamine [PE(P)], lysophosphatidylcholine (LPC), alkylphosphatidylcholine [PC(O)], alkenylphosphatidylcholine [PC(P)], lysoalkylphosphatidylcholine (LPO), cholesteryl ester (CE), diacylglycerol (DG), and triaclyglycerol (TG) were analysed using multiple reaction monitoring experiments. From the above 24 lipid classes and subclasses, five were different between RA and the controls. Then, we examined 36 lipid species within these five lipid classes and subclasses. Results were expressed as x nmol/mL of plasma. For clarity we refer the lipid classes by the complete name and use abbreviations for the individual lipid species only.
2.5 Inflammatory cytokines
Plasma levels of tumour necrosis factor (TNF)-α, interleukin (IL)-6, IL-1β, and IL-10 were measured using multiplex kits from Millipore (Massachusetts, USA) according to the manufacturer’s instruction. The appropriate cytokine standards, plasma samples (25 µL), and fluorescent conjugated, antibody-immobilized beads were added to wells of a pre-wet filtered plate and then incubated overnight at 4 °C. The following day, the plate was washed twice with wash buffer and then incubated with secondary detection antibody for 1 h, followed by subsequent incubation with strepavidin-phycoerythrin for 30 min. After the plate was washed twice again with wash buffer, it was run on the Luminex system (Biorad) with the addition of sheath fluid. Concentrations of different analytes in the plasma samples were determined by using respective standard curves generated in the multiplex assays. Neat plasma samples were used for all assays.
Macrophage migration inhibitory factor (MIF) in plasma was measured using commercial ELISA kits (R&D System) according to the manufacturer’s instructions. All samples and standards were measured in duplicate and averages used. High-sensitivity CRP in plasma was measured at the Department of Chemical Pathology of the Alfred Hospital.
2.6 Statistical analysis
Data were expressed as median and interquartile range unless otherwise stated. Prior to any statistical analysis, data were log-transformed. Differences between the control group and RA group were determined using unpaired t test. For ease of interpretation, only untransformed data were presented in the tables. Linear or binary logistic regression analysis on the IQR normalised lipid data [adjusting for age, sex, body mass index (BMI), current smoking status, systolic blood pressure, and antihypertensive treatment] was used to determine the associations of lipid classes, subclasses and individual lipid species with RA, disease duration or severity. The resultant odds ratio for a given lipid measurement represents the number of times an individual with a lipid measurement in the 75th percentile is more likely to have RA than an individual with a lipid measurement in the 25th percentile. For regression analysis, the Benjamini–Hochberg method was employed for correction for multiple comparisons (Benjamini and Hochberg 1995). Correlation analysis between inflammatory markers and lipid classes in the RA group was performed using Spearman’s correlations.
3 Results
3.1 Subject characteristics
Table 1 shows characteristics of study subjects. The groups were matched by age and gender. BMI, waist circumference, systolic and diastolic blood pressure, TG and FRS were significantly higher in patients with RA compared to controls. RA had normal TC, LDL-C, HDL-C, and blood glucose levels. As previously reported (Fan et al. 2014), circulating levels of CRP, IL-1β, IL-6, IL-10, TNF-α, and MIF were elevated in RA patients compared with controls.
The majority of patients with RA (except 2) received treatments including methotrexate (n = 13, 41 %), plaquenil (n = 7, 22 %), leflunomide (n = 7, 22 %), sulfasazine (n = 4, 13 %), biologics (n = 11, 34 %) and steroids (n = 9, 28 %). Biologics include TNF-α and IL-6 antagonists. Mean disease duration of RA patients was 9.2 ± 7.9 years. The majority of RA patients were either asymptomatic or experiencing only mild symptoms at the time of their assessment. Only 28 % of RA patients were experiencing moderate or severe symptoms. Thus, at the time of assessment, the majority of patients were effectively treated with regard to disease signs and symptoms.
3.2 Plasma lipid profiling
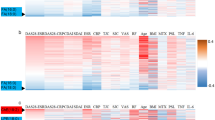
Out of 24 lipid classes and subclasses measured, four (dihydroceramides, alkylphosphatidylethanolamine, alkenylphosphatidylethanolamine, and phosphatidylserine) decreased while one (lysophosphatidylinositol) increased in patients with RA compared to controls (Table 2). Then, we further examined 36 lipid species within these five lipid classes and subclasses (Table 3). Eleven lipid species from the above five lipid classes and subclasses (dhCer 22:0, dhCer 24:0, PE(O-36:4), PE(P-36:4), PE(P-38:5), PE(P-40:5), PE(P-40:4), LPI 18:2, PS 36:1, PS 38:4, and PS 40:6) were different between RA and the controls (Table 3). All of them except LPI 18:2 were decreased in RA. Dihydroceramides and phosphatidylserine were negatively associated while lysophosphatidylinositol was positively associated with RA after adjusting for age, sex, BMI, current smoking, systolic blood pressure and anti-hypertensive treatment in a binary logistic regression model (Table 4). Ten lipid species (dhCer 22:0, dhCer 24:1, dhCer 24:0, PE(P-36:4), PE(P-38:4), PE(P-40:5), PE(P-40:4), PS 36:1, PS 38:4, and PS 40:6) were negatively associated with RA after adjusting for age, sex, BMI, current smoking, systolic blood pressure and anti-hypertensive treatment in a binary logistic regression model (Table 5). The associations for most of these lipid classes and species remained significant after correction by Benjamini–Hochberg method (Tables 4, 5).
3.3 Correlations between lipid classes, inflammatory markers and disease duration and severity
CRP was positively correlated with dihydroceramides (r = 0.382, p = 0.031) and lysophosphatidylinositol (r = 0.363, p = 0.041) and MIF was positively correlated with phosphatidylserine (r = 0.568, p = 0.0007) within the RA group. There were no other significant associations between other inflammatory markers and lipid classes. There were no significant associations between lipids and disease duration or severity.
4 Discussion
This study provides a detailed characterisation of the plasma lipid profiles associated with RA. Patients with RA had normal TC, LDL-C, and HDL, but higher TG. Among 24 lipid classes measured in our study, 5 lipid classes (dihydroceramides, alkylphosphatidylethanolamine, alkenylphosphatidylethanolamine, phosphatidylserine, and lysophosphatidylinositol) were different in patients with RA compared with controls. Then we measured the 36 lipid species within the above 5 lipid classes and found that 11 lipid species were different in RA. Three lipid classes and 10 lipid species from the above 5 lipid classes were associated with RA after adjusting for age, sex, BMI, current smoking, systolic blood pressure and anti-hypertensive treatment in a binary logistic regression model. The associations of lipids with RA are characterized by lower levels of ether lipids, phosphatidylserine, and dihydroceramide, but increased lysophosphatidylinositol. Although relatively moderate changes in lipid profiles are observed in patients with RA in our relatively small study, the findings still provide detailed information on dyslipidemia in RA.
In the present study, we have demonstrated normal levels of TC and LDL-C, and HDL-C but higher levels of TG in RA compared to controls. Previous studies showed reductions in levels of TC, LDL-C, and HDL-C in active RA (Peters et al. 2010; Chung et al. 2010). The majority (72 %) of our RA patients were in remission at the time of the study, which may explain normal TC, LDL-C and HDL-C. Consistently, dislipidemia of RA is generally associated with higher levels of TG, (Heldenberg et al. 1983; Sattar et al. 2003) although lower levels of TG have also been reported (Semb et al. 2010). A meta-analysis of population-based prospective studies has revealed that plasma TG level is a risk factor for cardiovascular disease independent of HDL-C level (Hokanson and Austin 1996). Despite normal or lower levels of LDL in RA, higher levels of small dense LDL particles, which more readily infiltrate the endothelium and thus become more susceptible to oxidative changes have been reported in RA.(Toms et al. 2011) It has also been shown that oxidized LDL levels are raised in RA, (Ajeganova et al. 2012) which are positively associated with intima-media thickness (Ahmed et al. 2010). We observed that ether lipids (alkylphophatidylethanolamine and alkenylphosphatidylethanolamine) were reduced in RA and inversely associated with RA. Ether lipids including the alkylphospholipids (alkylphophatidylcholine and alkylphophatidylethanolamine) and plasmalogens (alkenylphosphatidylcholine and alkenylphosphatidylethanolamine). Plasmalogen are susceptible to oxidation, on account of their high proportion of polyunsaturated fatty acids and the alkenyl linked acyl chains (Skaff et al. 2008). They are proposed to act as endogenous antioxidants and protect other lipids in lipoproteins and membranes from excessive oxidation (Wallner and Schmitz 2011; Engelmann 2004). Thus, reduced ether lipids could result from, and contribute to increased oxidative stress in RA. A previous intervention study on hyperlipidemic subjects showed that the increase in plasma alkenylphosphatidylethanolamine by ingestion of myoinositol, a known nutrient to improve fatty liver disease, was accompanied by a reduction in atherogenic small dense LDL (Maeba et al. 2008). Furthermore, reduced phosphatidylserine might also contribute to atherosclerosis in RA. It is known that adequate efferocytosis is required for resolution of inflammation and suppression of progressive inflammation such as atherosclerosis (Van Vre et al. 2012). Phosphatidylserine, a minor plasma phospholipid, is a major component of platelet membranes and is released as microparticles. Circulating levels of phosphatidylserine have been associated with platelet activation (Morel et al. 2011), which has itself been associated with CVD risk (Ruggeri 2002). However, phosphatidylserine has also been reported to be enriched in highly functional small dense HDL3 and shows positive associations with multiple HDL functions which would be expected to have a beneficial effect on cardiovascular risk (Camont et al. 2013). In addition, lysophosphatidylinositol was increased in RA and positively associated with RA. Lysophosphatidylinositol is an endogenous receptor for GPR55 (Yamashita et al. 2013). It was reported that the exposure of GPR55-expressing cells to lysophosphatidylinositol triggered the phosphorylation of p38 mitogen-activated protein kinase and activating transcription factor 2, suggesting that lysophosphatidylinositol and its receptor GPR55 play essential roles in inflammatory response (Oka et al. 2010). Circulating lysophosphatidylinositol levels were found increased in obese patients (Moreno-Navarrete et al. 2012). In our study, BMI was higher in RA patients than controls, but lysophosphatidylinositol remained significantly associated with RA after adjusting for BMI and other risk factors. Elevated levels of lysophospholipids also suggest an increase in phospholipase activity [especially lipoprotein associated phospholipase A2 (Lp-PLA2)]. This enzyme is highly expressed in atherosclerotic plaque and associated with the pathogenesis of atherosclerosis (Kolodgie et al. 2006; Schmitz and Ruebsaamen 2010). Consistently, Lp-PLA2 was higher in patients with RA than controls (Dulioust et al. 1992) and a very recent study further demonstrated that the level of Lp-PLA2 among patients with RA was associated with subclinical atherosclerosis, prospectively measured by intima-media thickness and flow-mediated dilation (Södergren et al. 2015). Taken together, the altered concentrations of these lipids observed in RA patients might help to explain the increased cardiovascular risk of these patients.
The observed lower levels of ether lipids in RA, which may lead to impaired antioxidant defence, may also contribute to the pathology of joint inflammation in RA. Oxidative stress is an important mediator of inflammation and reactive oxygen species enhance the inflammatory response in the joint by up-regulating expression of inflammatory mediators through the NF-κB signalling pathway (Hitchon and El-Gabalawy 2004). In this study, several species of phosphatidylserine were inversely associated with RA. It was reported that phosphatidylserine inhibited inflammatory gene expression [IL-6, IL-8, and prostaglandin E(2)], which was mediated by inhibition of NF-kb and p38 (Yeom et al. 2013). Thus, a decrease in phosphatidylserine levels might result in enhanced joint inflammation in RA patients. As mentioned above, LPI triggered phosphorylation of p38 mitogen-activated protein kinase and activating transcription factor 2, (Oka et al. 2010) thus LPI could also mediate inflammatory response of joints in RA patients.
Sphingolipids are structural elements of cell membranes and play key roles as signalling molecules in the modulation of inflammation (El Alwani et al. 2006). We found that dihydroceramide and several dihydroceramide species were reduced in RA and inversely associated with RA. Dihydroceramide is a biosynthetic precursor of ceramide but present at relatively low levels in circulation. As such the lower level of dihydroceramide in RA may reflect a higher flux through this pathway to ceramide and the downstream glycosphingolipids, although we do not observe any significant increase in these downstream species. Further investigation with larger study cohorts will be required to clarify the role of dihydroceramide in RA.
Lipid-based therapy could have some potential in treating patients with RA. A previous study showed that administration of plasmalogens had anti-inflammatory effects in LPS-induced neuroinflammation in mice (Ifuku et al. 2012). While a recent study suggested that phosphatidylserine showed a significant inhibitory effect on arthritic and nociceptive symptoms induced by carragee in rats, (Yeom et al. 2013) further studies are required to investigate the potential use of lipids, particularly plasmalogens and phosphatidylserine as either pharmaceutical or dietary supplements for alleviating arthritic symptoms.
This study provides novel information on plasma lipid profiles in RA. However, this needs to be considered within the limitation of the study. Since it was a cross sectional study, it is not clear whether the differences observed in lipids in the RA group are the result of RA or causal in the process. The associations of lipids with inflammatory markers were not strong although this may be a limitation of the study size. Whether other factors such as diet, lifestyle, and medication would affect lipids in RA patients needs further investigation. Most RA patients were in remission at the time of plasma sampling and lipid analysis. Thus, large-scale studies are needed to examine the relationships between lipids profiles and subpopulations of RA patients based on disease duration and disease activity and different types of medications.
5 Conclusion
Patients with RA are associated with reduced ether lipids, phosphatidylserine, and dihydroceramide, but increased lysophosphatidylinositol. These lipids may contribute to cardiovascular risk and joint inflammation in patients with RA.
References
Ahmed, H. M., Youssef, M., & Mosaad, Y. M. (2010). Antibodies against oxidized low-density lipoprotein are associated with subclinical atherosclerosis in recent-onset rheumatoid arthritis. Clinical Rheumatology, 29(11), 1237–1243. doi:10.1007/s10067-010-1436-0.
Ajeganova, S., de Faire, U., Jogestrand, T., Frostegard, J., & Hafstrom, I. (2012). Carotid atherosclerosis, disease measures, oxidized low-density lipoproteins, and atheroprotective natural antibodies for cardiovascular disease in early rheumatoid arthritis—an inception cohort study. Journal of Rheumatology, 39(6), 1146–1154. doi:10.3899/jrheum.111334.
Arnett, F. C., Edworthy, S. M., Bloch, D. A., McShane, D. J., Fries, J. F., Cooper, N. S., et al. (1988). The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis and Rheumatism, 31(3), 315–324.
Avina-Zubieta, J. A., Choi, H. K., Sadatsafavi, M., Etminan, M., Esdaile, J. M., & Lacaille, D. (2008). Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis and Rheumatism, 59(12), 1690–1697. doi:10.1002/art.24092.
Avina-Zubieta, J. A., Thomas, J., Sadatsafavi, M., Lehman, A. J., & Lacaille, D. (2012). Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies. Annals of the Rheumatic Diseases, 71(9), 1524–1529. doi:10.1136/annrheumdis-2011-200726.
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, 57(1), 289–300.
Camont, L., Lhomme, M., Rached, F., Le Goff, W., Negre-Salvayre, A., Salvayre, R., et al. (2013). Small, dense high-density lipoprotein-3 particles are enriched in negatively charged phospholipids: relevance to cellular cholesterol efflux, antioxidative, antithrombotic, anti-inflammatory, and antiapoptotic functionalities. Arteriosclerosis, Thrombosis, and Vascular Biology, 33(12), 2715–2723. doi:10.1161/ATVBAHA.113.301468.
Chung, C. P., Oeser, A., Raggi, P., Sokka, T., Pincus, T., Solus, J. F., et al. (2010). Lipoprotein subclasses determined by nuclear magnetic resonance spectroscopy and coronary atherosclerosis in patients with rheumatoid arthritis. Journal of Rheumatology, 37(8), 1633–1638. doi:10.3899/jrheum.090639.
del Rincon, I. D., Williams, K., Stern, M. P., Freeman, G. L., & Escalante, A. (2001). High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis and Rheumatism, 44(12), 2737–2745.
Dulioust, A., Hilliquin, P., Menkes, C. J., Benveniste, J., & Arnoux, B. (1992). Paf-acether acetylhydrolase activity is increased in patients with rheumatic diseases. Scandinavian Journal of Rheumatology, 21(4), 161–164.
El Alwani, M., Wu, B. X., Obeid, L. M., & Hannun, Y. A. (2006). Bioactive sphingolipids in the modulation of the inflammatory response. Pharmacology and Therapeutics, 112(1), 171–183. doi:10.1016/j.pharmthera.2006.04.004.
Engelmann, B. (2004). Plasmalogens: targets for oxidants and major lipophilic antioxidants. Biochemical Society Transactions, 32(Pt 1), 147–150.
Fan, F., Galvin, A., Fang, L., White, D. A., Moore, X. L., Sparrow, M., et al. (2014). Comparison of inflammation, arterial stiffness and traditional cardiovascular risk factors between rheumatoid arthritis and inflammatory bowel disease. Journal of Inflammation, 11(1), 29. doi:10.1186/s12950-014-0029-0.
Han, C., Robinson, D. W, Jr., Hackett, M. V., Paramore, L. C., Fraeman, K. H., & Bala, M. V. (2006). Cardiovascular disease and risk factors in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. Journal of Rheumatology, 33(11), 2167–2172.
Heldenberg, D., Caspi, D., Levtov, O., Werbin, B., Fishel, B., & Yaron, M. (1983). Serum lipids and lipoprotein concentrations in women with rheumatoid arthritis. Clinical Rheumatology, 2(4), 387–391.
Hitchon, C. A., & El-Gabalawy, H. S. (2004). Oxidation in rheumatoid arthritis. Arthritis Research and Therapy, 6(6), 265–278. doi:10.1186/ar1447.
Hokanson, J. E., & Austin, M. A. (1996). Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. Journal of Cardiovascular Risk, 3(2), 213–219.
Ifuku, M., Katafuchi, T., Mawatari, S., Noda, M., Miake, K., Sugiyama, M., et al. (2012). Anti-inflammatory/anti-amyloidogenic effects of plasmalogens in lipopolysaccharide-induced neuroinflammation in adult mice. J Neuroinflammation, 9, 197. doi:10.1186/1742-2094-9-197.
Kolodgie, F. D., Burke, A. P., Skorija, K. S., Ladich, E., Kutys, R., Makuria, A. T., et al. (2006). Lipoprotein-associated phospholipase A2 protein expression in the natural progression of human coronary atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology, 26(11), 2523–2529. doi:10.1161/01.ATV.0000244681.72738.bc.
Maeba, R., Hara, H., Ishikawa, H., Hayashi, S., Yoshimura, N., Kusano, J., et al. (2008). Myo-inositol treatment increases serum plasmalogens and decreases small dense LDL, particularly in hyperlipidemic subjects with metabolic syndrome. Journal of Nutritional Science and Vitaminology, 54(3), 196–202.
Meikle, P. J., Wong, G., Tsorotes, D., Barlow, C. K., Weir, J. M., Christopher, M. J., et al. (2011). Plasma lipidomic analysis of stable and unstable coronary artery disease. Arteriosclerosis, Thrombosis, and Vascular Biology, 31(11), 2723–2732. doi:10.1161/ATVBAHA.111.234096.
Morel, O., Jesel, L., Freyssinet, J. M., & Toti, F. (2011). Cellular mechanisms underlying the formation of circulating microparticles. Arteriosclerosis, Thrombosis, and Vascular Biology, 31(1), 15–26. doi:10.1161/ATVBAHA.109.200956.
Moreno-Navarrete, J. M., Catalan, V., Whyte, L., Diaz-Arteaga, A., Vazquez-Martinez, R., Rotellar, F., et al. (2012). The L-alpha-lysophosphatidylinositol/GPR55 system and its potential role in human obesity. Diabetes, 61(2), 281–291. doi:10.2337/db11-0649.
Myasoedova, E., Crowson, C. S., Kremers, H. M., Roger, V. L., Fitz-Gibbon, P. D., Therneau, T. M., et al. (2011). Lipid paradox in rheumatoid arthritis: the impact of serum lipid measures and systemic inflammation on the risk of cardiovascular disease. Annals of the Rheumatic Diseases, 70(3), 482–487. doi:10.1136/ard.2010.135871.
Oka, S., Kimura, S., Toshida, T., Ota, R., Yamashita, A., & Sugiura, T. (2010). Lysophosphatidylinositol induces rapid phosphorylation of p38 mitogen-activated protein kinase and activating transcription factor 2 in HEK293 cells expressing GPR55 and IM-9 lymphoblastoid cells. Journal of Biochemistry, 147(5), 671–678. doi:10.1093/jb/mvp208.
Perk, J., De Backer, G., Gohlke, H., Graham, I., Reiner, Z., Verschuren, M., et al. 2012. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). European Heart Journal, 33(13):1635–1701. doi:10.1093/eurheartj/ehs092.
Peters, M. J., Voskuyl, A. E., Sattar, N., Dijkmans, B. A., Smulders, Y. M., & Nurmohamed, M. T. (2010). The interplay between inflammation, lipids and cardiovascular risk in rheumatoid arthritis: why ratios may be better. International Journal of Clinical Practice, 64(10), 1440–1443. doi:10.1111/j.1742-1241.2009.02220.x.
Ruggeri, Z. M. (2002). Platelets in atherothrombosis. Nature Medicine, 8(11), 1227–1234. doi:10.1038/nm1102-1227.
Sattar, N., McCarey, D. W., Capell, H., & McInnes, I. B. (2003). Explaining how “high-grade” systemic inflammation accelerates vascular risk in rheumatoid arthritis. Circulation, 108(24), 2957–2963. doi:10.1161/01.CIR.0000099844.31524.05.
Schimmel, E. K., & Yazici, Y. (2009). Increased lipid levels but unchanged atherogenic index in rheumatoid arthritis patients treated with biologic disease modifying antirheumatic drugs: published experience. Clinical and Experimental Rheumatology, 27(3), 446–451.
Schmitz, G., & Ruebsaamen, K. (2010). Metabolism and atherogenic disease association of lysophosphatidylcholine. Atherosclerosis, 208(1), 10–18. doi:10.1016/j.atherosclerosis.2009.05.029.
Semb, A. G., Kvien, T. K., Aastveit, A. H., Jungner, I., Pedersen, T. R., Walldius, G., et al. (2010). Lipids, myocardial infarction and ischaemic stroke in patients with rheumatoid arthritis in the apolipoprotein-related mortality risk (AMORIS) study. Annals of the Rheumatic Diseases, 69(11), 1996–2001. doi:10.1136/ard.2009.126128.
Skaff, O., Pattison, D. I., & Davies, M. J. (2008). The vinyl ether linkages of plasmalogens are favored targets for myeloperoxidase-derived oxidants: a kinetic study. Biochemistry, 47(31), 8237–8245. doi:10.1021/bi800786q.
Södergren, A., Karp, K., Bengtsson, C., Möller, B., Rantapää-Dahlqvist, S., & Wållberg-Jonsson, S. (2015). Is Lipoprotein-associated phospholipase A2 a link between inflammation and subclinical atherosclerosis in rheumatoid arthritis? Biomed Research International, 2015, 673018. doi:10.1155/2015/673018.
Toms, T. E., Panoulas, V. F., & Kitas, G. D. (2011). Dyslipidaemia in rheumatological autoimmune diseases. Open Cardiovascular Medicine Journal, 5, 64–75. doi:10.2174/1874192401105010064.
Van Vre, E. A., Ait-Oufella, H., Tedgui, A., & Mallat, Z. (2012). Apoptotic cell death and efferocytosis in atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology, 32(4), 887–893. doi:10.1161/ATVBAHA.111.224873.
Wallner, S., & Schmitz, G. (2011). Plasmalogens the neglected regulatory and scavenging lipid species. Chemistry and Physics of Lipids, 164(6), 573–589. doi:10.1016/j.chemphyslip.2011.06.008.
Weir, J. M., Wong, G., Barlow, C. K., Greeve, M. A., Kowalczyk, A., Almasy, L., et al. (2013). Plasma lipid profiling in a large population-based cohort. Journal of Lipid Research, 54(10), 2898–2908. doi:10.1194/jlr.P035808.
Yamashita, A., Oka, S., Tanikawa, T., Hayashi, Y., Nemoto-Sasaki, Y., & Sugiura, T. (2013). The actions and metabolism of lysophosphatidylinositol, an endogenous agonist for GPR55. Prostaglandins and Other Lipid Mediators, 107, 103–116. doi:10.1016/j.prostaglandins.2013.05.004.
Yeom, M., Hahm, D. H., Sur, B. J., Han, J. J., Lee, H. J., Yang, H. I., et al. (2013). Phosphatidylserine inhibits inflammatory responses in interleukin-1beta-stimulated fibroblast-like synoviocytes and alleviates carrageenan-induced arthritis in rat. Nutrition Research, 33(3), 242–250. doi:10.1016/j.nutres.2013.01.006.
Acknowledgments
We are grateful to the clinic support staff in the Rheumatology Clinic of the Alfred Hospital and the Risk Evaluation Service of Baker IDI Heart and Diabetes Institute for help with the clinical aspects of this study. The study was supported by a National Health and Medical Research Council of Australia (NHMRC) program Grant to AMD and the Operational Infrastructure Support (OIS) Program of the Victorian Government, Australia. AMD is a Senior Principal Research Fellow (586656) and PJM is a NHMRC senior research fellow (1042095).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
The study was approved by the Ethics Committee of the Alfred Hospital.
Additional information
Lu Fang and Piyushkumar A Mundra have contributed to the work equally.
Peter Meikle and Anthony Michael Dart are Joint senior Authors.
Rights and permissions
About this article
Cite this article
Fang, L., Mundra, P.A., Fan, F. et al. Plasma lipidomic profiling in patients with rheumatoid arthritis. Metabolomics 12, 136 (2016). https://doi.org/10.1007/s11306-016-1086-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11306-016-1086-6