Abstract
Lipid mediators have been suggested to play important roles in the pathogenesis of rheumatoid arthritis (RA). Lipidomics has recently allowed for the comprehensive analysis of lipids and has revealed the potential of lipids as biomarkers for the early diagnosis of RA and prediction of therapeutic responses. However, the relationship between disease activity and the lipid profile in RA remains unclear. In the present study, we performed a plasma lipidomic analysis of 278 patients with RA during treatment and examined relationships with disease activity using the Disease Activity Score in 28 joints (DAS28)-erythrocyte sedimentation rate (ESR). In all patients, five lipids positively correlated and seven lipids negatively correlated with DAS28-ESR. Stearic acid [FA(18:0)] (r = -0.45) and palmitic acid [FA(16:0)] (r = -0.38) showed strong negative correlations. After adjustments for age, body mass index (BMI), and medications, stearic acid, palmitic acid, bilirubin, and lysophosphatidylcholines negatively correlated with disease activity. Stearic acid inhibited osteoclast differentiation from peripheral blood monocytes in in vitro experiments, suggesting its contribution to RA disease activity by affecting bone metabolism. These results indicate that the lipid profile correlates with the disease activity of RA and also that some lipids may be involved in the pathogenesis of RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
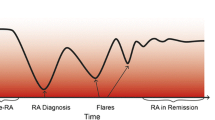
Rheumatoid arthritis (RA) is a disease that causes chronic inflammatory changes in the synovial tissues of the joints, leading to joint destruction and deformity. Its pathogenesis involves the infiltration of leukocytes into synovial tissue and an increase in the production of inflammatory cytokines, such as interleukin (IL)-6 and tumor necrosis factor (TNF), resulting in chronic synovial inflammation [1]. Osteoclasts also play a central role in bone destruction in RA. Osteoclasts are derived from the monocyte-macrophage lineage and function in bone resorption. The monocytes of RA patients have been shown to have an increased potential to differentiate osteoclasts [2] and also have a high bone resorption capacity [3]. Furthermore, enhanced in vitro osteoclast differentiation from peripheral monocytes correlated with severe joint destruction in RA [4].
Endogenous bioactive substances involved in inflammation include lipids. Eicosanoids synthesized from arachidonic acid are typical examples, while specialized pro-resolving mediators, lysophospholipids, and endocannabinoids are also bioactive lipids [5]. Enzymes involved in eicosanoid production, such as cytosolic phospholipase A2 and cyclooxygenase-2, are overexpressed in RA patients [5], and, thus, lipid mediators are also considered to play a role in the pathogenesis of RA.
Recent studies on lipidomics, which is the comprehensive analysis of lipids, revealed the characteristics of the lipid profile in RA. Differences have been reported in lipid profiles between chronic inflammatory diseases, such as RA, psoriatic arthritis, and Lyme disease [6, 7]. Another study has shown that lipid profiles discriminated responsiveness to TNF inhibitors [8]. These studies suggest that lipids profiles may be useful for the diagnosis of RA and predicting response to therapies. Although relationships have been detected between disease activity and lipid metabolites [8,9,10], the lipids identified differed among studies and contradictory findings were also obtained. Therefore, further studies are needed to clarify the relationship between lipids and the pathogenesis of RA.
In the present study, a lipidomic analysis of plasma obtained from large number of RA patients was performed to further clarify the involvement of lipids in the pathogenesis of RA. We analyzed correlation of lipid profile and disease activity, gender, and therapeutic drugs. In addition, in vitro experiments were used to examine the role of lipid, which was associated with disease activity, in the RA pathogenesis.
METHODS
Patients
Patients with RA attending Toho University Omori Medical Center were enrolled in the present study between October 2016 and January 2017. All patients were diagnosed with RA using the 2010 American College of Rheumatology/European League Against Rheumatism classification criteria [11]. Patients who met the classification criteria were enrolled, and there were no exclusion criteria. Clinical characteristics, including age, sex, body mass index (BMI), laboratory assessments, clinical disease activity assessments, and medications, were recorded.
This study was performed in line with the principles of the Declaration of Helsinki. The study protocol for lipidomics was approved by the Ethics Committees of the Faculty of Medicine, Toho University (approval numbers: A22060_A19020_A17059_A16030) and National Institute of Health Sciences (approval numbers: 271, 271–2, 271–3). All study participants provided written informed consent for this study.
Collection of Human Plasma
Venous blood was collected into 3-mL vacutainer plasma separator tubes containing K2-ethylenediamineteraacetic acid for plasma separation (Becton Dickinson, Franklin Lakes, NJ). Samples were centrifuged and plasma was separated within 2 h of the collection of blood samples. Plasma samples were immediately frozen and stored at -80℃. After shipment with dry ice from the hospital, all frozen samples were thawed once on ice and divided into small aliquots before storage at -80℃ until lipid extraction.
Extraction and Measurement of Lipid Metabolites
Lipid extraction was performed using the Microlab NIMBUS workstation (Hamilton, Binaduz, GR, Switzerland). Plasma samples were mixed with nine volumes of methanol/isopropanol (1/1) containing an internal standard (phosphatidylcholine (PC) [12:0/12:0]), which is not detectable endogenously, at 2 μM. Mixed samples were filtered through a FastRemover Protein Removal Plate (GL Science, Tokyo, Japan) using an MPE2 automated liquid handling unit (Hamilton). The resulting lipid-containing filtrate was directly subjected to lipidomics. To obtain lipidomic data, we used reversed-phase liquid chromatography (Ultimate 3000, Thermo Fisher Scientific, Waltham, MA, USA) and MS (Orbitrap Fusion, Thermo Fisher Scientific), as previously described [12, 13]. Compound Discoverer 2.1 (Thermo Fisher Scientific) was used with raw data for peak extraction, annotation, identification, and lipid quantification, as previously reported with a prior version of the software [12, 13]. Quantified raw data were normalized to the internal standard.
Osteoclast Differentiation from Peripheral Blood Monocytes
Peripheral blood mononuclear cells (PBMC) were separated by Lymphocyte Separation Solution (Nacalai Tesque, Kyoto, Japan) from healthy donors. Monocytes were purified by negative selection using MACS microbeads (Pan Monocyte Isolation Kit, human; Miltenyi Biotec, Auburn, CA, USA) according to the manufacturer’s instructions. The study protocol was approved by the Ethics Committees of the Faculty of Medicine, Toho University (approval numbers: A21014_A18084_27060). Written informed consent was obtained before participation in the study.
To induce the differentiation of osteoclasts from peripheral blood monocytes, purified monocytes were cultured in 96-well plates at 1.0 × 105 cells per well in α-MEM (Thermo Fisher Scientific), supplemented with heat-inactivated 10% fetal bovine serum and 20 ng/mL of macrophage colony-stimulating factor (M-CSF) (PeproTech, Rocky Hill, NJ, USA). On the second day of the culture, 40 ng/ml of receptor activator of nuclear factor-κB (NF-κB) ligand (RANKL) (R&D Systems, Minneapolis, MN, USA) with or without stearic acid, dissolved in dimethyl sulfoxide and bovine serum albumin (12.5 or 50 μM), was added to the medium. Every 3 days, the medium was replaced with fresh medium containing the same concentrations of M-CSF, RANKL, and stearic acid. After an incubation for 8 days, cells were stained with a tartrate-resistant acid phosphatase (TRAP) staining kit (Wako Pure Chemical, Osaka Japan). The total number of TRAP-positive multinucleated cells (MNC) containing three or more nuclei per well was counted as osteoclasts under light microscopy.
Real-time Reverse Transcriptase-polymerase Chain Reaction (RT-PCR)
RT-PCR was performed to evaluate the expression of mRNA of nuclear factor of activated T cell 1 (NFATC1). Total RNA was extracted with TRIzol™ Reagent (Thermo Fisher Scientific), and first-strand cDNA was synthesized using a PrimeScript™ RT reagent KIT with genome DNA Eraser (Takara-Bio, Shiga, Japan), according to the manufacturer’s instructions. The cDNA was amplified with TB Green® Premix Ex Taq™ II (Takara-Bio) using QuantStudio 3 (Applied Biosystems, Foster City, CA, USA). The expression of mRNA was normalized to those of β-actin mRNA (ACTB). The sequence of primers was as follows:NFATC1, forward: GCA TCA GAG GGA AGA CCG TGT C; reverse: GAA GTT GAA TGT CGG AGT TTC TGA G; and ACTB, forward: GAC GAC ATG GAG AAA ATC TG; reverse: ATG ATC TGG GTC ATC TTC TC. The reactions were incubated at 94 °C for 10 min, and then 94 °C (15 s), 60 °C (1 min) for 40cycles.
Cytotoxicity Test
Cell viability was measured using lactate dehydrogenase (LDH) assay. The LDH toxicity assay kit (Nacalai Tesque) was used according to the manufacturer’s specification. Monocytes were cultured with M-CSF, RANKL, and different concentrations of stearic acid (0, 6.25, 12.5, 25 or 50 μM). Released LDH in culture supernatants after 3 days was measured.
Culture of Fibroblast-like Synoviocytes (FLSs)
FLSs derived from RA patients were purchased from JCRB Cell Bank (Osaka, Japan). FLSs were resuspended in DMEM (high glucose, Nakalai Tesque) supplemented with 10% fetal calf serum, 100 units/ml penicillin and 100 units/ml streptomycin (Nakalai Tesque), and plated in 48-well plates. After 24-h culture with TNF (10 ng/ml) alone or in combination with stearic acid (0, 6.25, 12.5, 25 or 50 μM), supernatant was collected, and concentration of IL-6 was measured by enzyme-linked immunosorbent assay (R&D Systems) according to the manufacturer’s directions. This experiment was approved by the Ethics Committees of the Faculty of Medicine, Toho University (approval numbers: A21014_A18084_27060).
Statistical Analysis
Correlation coefficients between lipid molecules and clinical data were analyzed by Spearman’s rank correlation test using R statistical environment software (https://r-project.org/). Principal component analysis (PCA) and orthogonal partial least squares discriminant analysis (OPLS-DA) were performed by Metaboanalyst 6.0 (https://www.metaboanalyst.ca/). Data normalization was performed using log transformation and auto scaling. In OPLS-DA, the robustness of created model was evaluated by R2 value and Q2 value. The R2 was monitoring the model fit, and the Q2 represented predictive ability. The R2 (close to 1) and Q2 (> 0.4) were considered adequate models. Spearman’s rank correlation test between stearic acid and individual clinical parameters and Mann–Whitney test for comparisons of stearic acid between users and non-users of biologics were performed using Prism ver. 8.0 software (GraphPad Software, San Diego, CA). For multiple group comparison, a one-way analysis of variance with the Bonferroni post hoc test was performed using Prism ver. 8.0 software. In all analyses, p < 0.05 was considered to be significant.
RESULT
Study Participants
A total of 229 females and 49 males with RA were enrolled. The clinical data of participants are shown in Table 1. According to the Disease Activity Score in 28 joints (DAS28)-erythrocyte sedimentation rate (ESR) criteria [14], 135 females (59.0%) and 35 males (71.4%) were in remission, while 94 females (31.0%) and 14 males (28.6%) had low or moderate disease activity. There were no patients with high disease activity. Methotrexate was used for approximately 75% of patients of both sexes. Glucocorticoids (GC) were being administered to 32 females (14.0%) and 12 males (24.5%), and biologics to 83 females (36.4%) and 22 males (44.9%).
Relationships Between Plasma Lipids and the Disease Activity Index of RA
Lipid metabolites were measured in the plasma of RA patients. A total of 329 lipid molecules were detected. Correlation coefficients between lipids and each clinical parameter, including DAS28-ESR, are shown as heatmaps (Fig. 1). Heatmaps show lipids sorted in descending order of correlation coefficients with DAS28-ESR. Positive correlations are indicated by red and negative correlations by blue. In the heatmap of all patients (Fig. 1a), disease activity scores, such as DAS28-C-reactive protein (CRP), the clinical disease activity index (CDAI), simplified disease activity index (SDAI), each component of disease activity scores [tender joint count (TJC) and global visual analog scale (VAS)], age, and the dosage of prednisolone (PSL) showed similar patterns of correlations to lipids and DAS28-ESR. Furthermore, ESR, CRP, swollen joint count (SJC), and rheumatoid factor (RF), but not BMI, the dosage of methotrexate, or the use of biologics, TNF inhibitors and IL-6 inhibitor, showed similar patterns of correlations to lipids. The heatmap for female patients showed similar correlation patterns to all patients (Fig. 1b). On the other hand, in the heatmap for male patients, the patterns of correlations of lipids with SJC, age and the dosage of PSL was different from that of disease activity scores (Fig. 1c).
Heatmaps of correlation coefficients between plasma lipids and the disease activity index, clinical parameters, and medication. Lipids were sorted in descending order of correlation coefficients with DAS28-ESR. a Heatmap of all rheumatoid arthritis patients. b Only female patients are included. c Only male patients are included. Correlation coefficients were analyzed by Spearman’s rank correlation test. Red cells show a positive correlation and blue cells a negative correlation. Lipids that strongly correlate with DAS28-ESR are noted on the left side of each heatmap (10 lipid metabolites with the absolute values of correlation coefficients > 0.3). Abbreviations: BMI: body mass index, CDAI: clinical disease activity index, ChE: cholesterolester, CRP: C-reactive protein, DAS28: disease activity score in 28 joints, ESR: erythrocyte sedimentation rate, FA(16:0): palmitic acid, FA(18:0): stearic acid, IL-6: interleukin-6 inhibitor, LPC: lysophosphatidylcholine, LPE: lysophosphatidylethanolamine, MTX: dose of methotrexate, PC: phosphatidylcholine, PSL: dose of prednisolone, RF: rheumatoid factor, SDAI: simplified disease activity index, SJC: swollen joint count, TJC: tender joint count, TNF: tumor necrosis factor inhibitors, VAS: global visual analog scale.
Lipids that correlated with DAS28-ESR (absolute correlation coefficient > 0.2) are shown in Table 2. In all patients, five lipids, including, sphingomyelin [SM(d41:3), SM(d40:3), SM(d42:4), SM(d41:2)1 and SM(d42:3)], positively correlated with DAS28-ESR, while seven lipids, including stearic acid [FA(18:0)], palmitic acid [FA(16:0)], bilirubin, lysophosphatidylcholine [LPC(16:0), LPC(18:2), and LPC(18:1)] and acylcarnitine [Car(18:2)] negatively correlated with DAS28-ESR. Stearic acid [FA(18:0)] (r = -0.45) and palmitic acid [FA(16:0)] (r = -0.38) showed strong negative correlations with DAS28-ESR. In female patients, 11 lipids showed positive correlations, while five lipids showed negative correlations with DAS28-ESR (absolute values of the correlation coefficients > 0.2) (Supplementary Table 1). Stearic acid [FA(18:0)] (r = -0.41) and palmitic acid [FA(16:0)] (r = -0.32) showed strong negative correlations, while Ceramide [Cer(d42:2)] (r = 0.27) also showed a strong positive correlation with DAS28-ESR. In males, six lipids positively correlated with DAS28-ESR, while 85 lipids negatively correlated with DAS28-ESR (Supplementary Table 2). The correlation coefficients of lysophosphatidylcholine [LPC(16:0)] (r = -0.52) showed the lowest value, followed by phosphatidylcholine [PC(40:5)2] (r = -0.48), palmitic acid [FA(16:0)] (r = -0.47), lysophosphatidylcholine [LPC(18:0)2] (r = -0.46), and stearic acid [FA(18:0)] (r = -0.45). In comparisons between females and males, stearic acid, palmitic acid, phosphatidylcholines, lysophosphatidylcholines, and sphingomyelins correlated similarly with DAS28-ESR in both sexes. On the other hand, ceramides, monosialodihexosylganglioside, phosphatidylinositols and lysophosphatidylethanolamines showed positive correlations in females, but negative correlations in males. Cholesterolester showed positively correlated only in males, while triacylglycerols, phosphatidylethanolamines, diacylglycerols, acylcarnitines, and fatty acid [FA(22:6)] showed negative correlation only in males.
Since age, BMI, and medications may have been confounding factors in lipid and DAS28-ESR correlation analyses, we analyzed partial correlation coefficients adjusted for these factors. The results obtained showed that stearic acid [FA(18:0)] (r = -0.41) and palmitic acid [FA(16:0)] (r = -0.35) still negatively correlated with DAS28-ESR (Table 3).
The PCA and OPLS-DA including all RA patients were then performed. PCA scores plot, OPLS-DA scores plot and lipids with higher variable importance in projection (VIP) scores in OPLS-DA model with lipid concentrations for each group are shown in Fig. 2. In a PCA scores plot, the group with moderate disease activity on the DAS28-ESR (≥ 3.2) overlapped with the group with low disease activity and remission (< 3.2). The OPLS-DA was also performed, but the Q2 value was very low (Q2 = 0.0394) (Fig. 2a). The VIP scores were high for stearic acid, palmitic acid and lysophosphatidylcholines; these lipids were high concentrations in low disease activity (< 3.2), coinciding to the above results of correlation analysis (Fig. 2a). The OPLS-DA scores plot by gender discriminated males from females, with Q2 value was 0.479 and R2 value was 0.743 (Fig. 2b). The VIP scores were high for sphingomyelins and phosphatidylcholines, and these lipids were high concentrations in females (Fig. 2b). No clear clustering was generated to distinguish the use of therapeutic agents such as GC, methotrexate, and biologics (Figs. 2c, d and e), although several lipids showed high VIP score. The results of analyzing the differences in lipids between GC users and non-users by gender were shown in Fig. 3. In both males and females, separated clusters were not observed in the 2D score plots of PCA and OPLS-DA. The VIP score for triacylglycerols was high in males and females, and concentration was higher in GC users of both sexes. The VIP score for phosphatidylcholine was also high in both males and females, while concentrations were low in male GC users, and high in female GC users.
PCA and OPLS-DA of the lipid profile in plasma of RA patients. Plots of PCA scores (left panels), plots of OPLS-DA scores (middle panels) and VIP scores in OPLS-DA model with lipid concentrations for each group (right panels) for comparisons between moderate disease activity group (DAS28 ≥ 3.2) and lower than low disease activity group (DAS28 < 3.2) a females and males b glucocorticoid users and non-users c methotrexate users and non-users d and biologics users and non-users e. Top 10 lipids were shown in the OPLS-DA VIP score. Abbreviations: Bio: biologics, Car: acylcarnitine, Cer: ceramide, ChE: cholesterolester, CRP: C-reactive protein, DAS28: disease activity score in 28 joints, DG: diacylglycerol, ESR: erythrocyte sedimentation rate, FA(16:0): palmitic acid, FA(18:0): stearic acid, GC: glucocorticoid, GM3: monosialodihexosylganglioside, LPC: lysophosphatidylcholine, MTX: methotrexate, OPLS-DA: orthogonal partial least squares discriminant analysis, PC: phosphatidylcholine, PCA: principal component analysis, PE: phosphatidylethanolamine, SM: sphingomyelin, TG: triacylglycerol, VIP score: variable importance in projection score.
PCA and OPLS-DA of plasma lipid profile from female or male RA patients for comparisons between glucocorticoid users and non-users. Plasma lipid profile from RA patients were analyzed separately by gender. a The analysis of only female patients. The left and middle graphs are 2D scores plots of PCA and OPLS-DA. The right graph showed the top 10 lipids in the VIP score of the OPLS-DA model with lipid concentrations in GC users and non-users groups. b The analysis of only male patients. Abbreviations: Cer: ceramide, DG: diacylglycerol, FA(16:0): palmitic acid, FA(18:0): stearic acid, GC: glucocorticoid, LPE: lysophosphatidylethanolamine, OPLS-DA: orthogonal partial least squares discriminant analysis, PC: phosphatidylcholine, PCA: principal component analysis, PE: phosphatidylethanolamine, PI: phosphatidylinositol, TG: triacylglycerol. VIP score: variable importance in projection score.
Since stearic acid had the highest partial correlation coefficient with DAS28-ESR, we focused on stearic acid as a lipid associated with disease activity in RA. Scatter plots of stearic acid and each clinical parameter in all patients are shown in Fig. 4. In addition to DAS28-ESR, stearic acid negatively correlated with DAS28-CRP, CDAI, SDAI, ESR, CRP, TJC, SJC, global VAS, RF, age, and the dosage of PSL. No correlation between stearic acid and use of TNF or IL-6 inhibitors was shown. Scatter plots of stearic acid and each clinical parameter for female patients are shown in Supplementary Fig. 1. The results obtained for female patients were similar to those for all patients. Although the results obtained for male patients were also similar to those for all patients, stearic acid only negatively correlated with DAS28-ESR, ESR, and the dosage of PSL (Supplementary Fig. 2).
Correlations of stearic acid and clinical parameters in all patients. a Scatter plots of stearic acid and clinical parameters. The y-axis shows the arbitrary unit of stearic acid, while the x-axis shows each clinical parameter. Correlation coefficients were analyzed by Spearman’s rank correlation test. b Dot plots presenting the concentrations of stearic acid in users and non-users of biologics. Data are shown as the mean ± SEM. Abbreviations: CDAI: clinical disease activity index, CRP: C-reactive protein, DAS28: disease activity score in 28 joints, ESR: erythrocyte sedimentation rate, IL-6: interleukin-6, MTX: dose of methotrexate, PSL: dose of prednisolone, RF: rheumatoid factor, SDAI: simplified disease activity index, SJC: swollen joint count, TJC: tender joint count, TNF: tumor necrosis factor, VAS: global visual analog scale.
Effects of Stearic Acid on Osteoclastogenesis
Since stearic acid negatively correlated with the disease activity of RA, we examined the pathological effects of stearic acid on RA. Bone destruction is a characteristic of RA; therefore, we focused on the effects of stearic acid on osteoclastogenesis. Peripheral blood monocytes were differentiated to osteoclasts by a stimulation with M-CSF and RANKL. However, an incubation with stearic acid inhibited the differentiation to osteoclasts (Fig. 5a). Additionally, we examined expression of NFATC1, a pivotal transcription factor for osteoclast differentiation. Stearic acid significantly decreased the expression of NFATC1 (Fig. 5b).
Effects of stearic acid on osteoclast differentiation of CD14-positive monocytes. CD14-positive monocytes were cultured with 20 ng/mL of M-CSF and 40 ng/mL of RANKL with different concentrations of stearic acid for 8 days. a The number of TRAP-positive MNC. TRAP staining was performed on day 8. b Expression of NFATC1 mRNA level normalized against ACTB (β-actin) expression. Total RNA was extracted on day 8, cDNA was synthesized, and a real-time RT-PCR was performed. Data are shown as the mean ± SEM. *P < 0.05. **P < 0.01. ***P < 0.005. Abbreviations: MNC: multinucleated cells, TRAP: tartrate-resistant acid phosphatase.
To confirm that these results were not due to cytotoxicity by stearic acid, LDH was measured using monocyte culture supernatants. As shown in Supplementary Fig. 3, the addition of stearic acid did not increase LDH.
Effect of Stearic Acid on FLSs of RA
To investigate the effect of stearic acid on FLSs from RA, FLSs was stimulated with TNF and the effect of stearic acid on their IL-6 production was examined. Stimulation of FLSs with TNF for 24 h markedly increased IL-6 production, and the addition of stearic acid slightly increased IL-6 production (Fig. 6).
DISCUSSION
We herein examined the lipid profile of plasma from RA patients during treatment. The results obtained showed that stearic acid, palmitic acid, phosphatidylcholine and lysophosphatidylcholine negatively correlated with DAS28-ESR, while sphingomyelins positively correlated in both females and males. Negative correlations were still observed for stearic acid, palmitic acid, bilirubin, and lysophosphatidylcholines in analyses adjusted for age, BMI, and therapeutic drugs. In PCA of the lipid profile, clear cluster separation was not observed on differences in disease activity, gender, or treatment. On the other hand, the OPLS-DA discriminated the lipid profile males from that of females. Although OPLS-DA could not separate that of RA patients with moderate disease activity from that of patients with low disease activity, the VIP scores of stearic acid, palmitic acid, and lysophosphatidylcholine were high, and the concentrations of these lipids were high in patients with low disease activity.
We found that stearic acid and palmitic acid negatively correlated with disease activity in RA, which was not consistent with previous studies. Cuppen et al. [8] showed that stearic acid and palmitic acid positively correlated with CRP, ESR and DAS28. On the other hand, Rodríguez-Carrio et al. [15], who measured fatty acids, including stearic acid and palmitic acid, in RA patients, reported no significant differences in DAS28 between the high fatty acid group and low fatty acid group. The reasons for these differences currently remain unclear, but may be attributed to the analysis method or patient profiles, such as racial differences. Furthermore, the study of Cuppen et al. [8] enrolled RA patients with higher disease activity, where the more than 50% of patients were in remission in our study. Differences in disease activity of RA and therapeutic drugs may also have caused differences in lipid profiles.
Stearic acid and palmitic acid are long-chain fatty acids; stearic acid has 18 carbons and palmitic acid has 16. They are classified as saturated fatty acids, which do not contain double bonds in the carbon chain. Fatty acids are a good energy source as a result of their oxidation, a major component of cell membrane phospholipids, and a mediator with biological activity. Stearic acid and palmitic acid are also bioactive substances. Palmitic acid has been suggested to act as a Toll-like receptor (TLR) 4 agonist and trigger for an inflammatory response, activating NF-κB through the myeloid differentiation primary response gene 88 (MyD88)-dependent pathway [16, 17]. Stearic acid has also been shown to express cyclooxygenase (COX) via TLR4 and activate monocytes through a MyD88-independent pathway [17, 18]. In contrast, few studies have suggested that stearic acid has an anti-inflammatory function. Stearic acid was previously found to inhibit nitric oxide production by lipopolysaccharide-stimulated RAW264 cells [19], increase IL-10 production in rat hepatocytes [20], and suppress NF-κB activity and myeloperoxidase activity in rat cholestasis-related liver injury [21]. In this study, stearic acid slightly increased IL-6 production from TNF-stimulated FLSs. However, since the increase in IL-6 production was small, it is unclear whether the proinflammatory effect of stearic acid is physiologically significant. On the other hand, we found that stearic acid inhibited osteoclast differentiation from peripheral blood monocytes and also reduced the expression of NFATC1, a pivotal transcription factor of osteoclast differentiation, suggesting that a reduction in plasma stearic acid contributes to osteoclastogenesis and bone destruction in RA patients.
Bilirubin also showed a negative correlation with disease activity. Bilirubin, a degraded metabolite of hemoglobin, causes jaundice, but has potent antioxidant properties [22]. An epidemiological study demonstrated that the risk of developing RA inversely correlated with serum levels of total bilirubin [22]. The protective effects of bilirubin on RA may be due to its antioxidant properties.
Lysophosphatidylcholine, a bioactive lipid, also showed a negative correlation with the disease activity of RA regardless of sex. Consistent with the present results, two recent studies reported a decrease in lysophosphatidylcholine in the serum of patients with active RA [8, 10]. Lysophosphatidylcholine is known to exert pro-inflammatory effects. It is highly expressed at inflammatory sites [23], and its expression is followed by inflammatory responses to lysophosphatidylcholine in various cells. A stimulation with lysophosphatidylcholine induced inflammatory responses, such as the expression of adhesion molecules and production of COX-2, in vascular endothelial cells [24], chemotaxis, and pro-inflammatory cytokine production in monocytic cells [25], and evoked T-cell chemotaxis [26]. On the other hand, polyunsaturated lysophosphatidylcholine has been reported to possess anti-inflammatory properties [27]. However, in this study, unsaturated fatty acids, whether monovalent [LPC (18:1)] or polyvalent [LPC (18:2)], negatively correlated with RA disease activity. On the other hand, a decrease in lysophosphatidylcholine may reflect an increase in lysophosphatidic acid. Lysophosphatidylcholine is cleaved at the choline group by autotaxin, a secreted lysophospholipase D, to form lysophosphatidic acid. Previous studies reported that autotaxin was up-regulated in the synovial fluid and synovial tissues of RA patients [28, 29], and lysophosphatidic acid receptors were also up-regulated in RA synovial cells [28]. Lysophosphatidic acid is involved in the regulation of cellular survival, proliferation, differentiation, and motility [28]. Mice lacking lysophosphatidic acid receptors did not develop arthritis, and the administration of a lysophosphatidic acid receptor antagonist reduced the severity of arthritis in murine collagen-induced arthritis [28]. Therefore, lysophosphatidylcholine may be decreased in RA patients because of the promotion of the pathway for the formation of lysophosphatidic acid from lysophosphatidylcholine.
Few studies that performed a lipidomic analysis of RA focused on sex differences in lipid profiles. The present study analyzed lipid changes by sex in RA patients and found that some lipids correlated differently with disease activity according to sex. It should be noted that the result from all patients was similar to that from only female patients, since 82% of participants in this study were female. Furthermore, we performed PCA and OPLS-DA and showed that lipid profile of RA patients differed by gender, and it was shown that sphingomyelins and phosphatidylcholines greatly contributed to gender differences. However, Mekawa et al. [30] showed that in also healthy Japanese subjects, sphingomyelin and phosphatidylcholine levels were higher in females than in males. Therefore, the results of our OPLS-DA may be based on gender differences in the general lipid profiles of the Japanese population. Additionally, changes in lipid profiles due to RA treatment may differ by gender. It was reported that serum concentrations of lysophosphatidylcholines and lysophosphatidylethanolamines were elevated in GC-users compared to non-GC users in female RA patients, but not in males [31]. In this study, we found that phosphatidylcholine was higher in GC-users in female, but lower in male. RA occurs more frequently in females [32], but it is unclear whether the different lipid profiles in males and females are related to gender differences in RA development. In this study, since there were no healthy controls, it is difficult to verify whether the lipid profile contribute the development of RA. We therefore, need to clarify this important point in future.
It was not clear whether saturated fatty acids such as stearic acid, lysophosphatidylcholine and phosphatidylcholine can be applied to the management of RA (diagnosis, assessment of disease activity, treatment, and etc.). It also remains unclear whether the inhibition of stearic acid can be applied clinically for osteoporosis. Future research will be needed for clinical application of the lipids.
In the present study, we disclosed that plasma stearic acid, palmitic acid, bilirubin, phosphatidylcholine, and lysophosphatidylcholine levels negatively correlated with the disease activity of RA. Although we showed that stearic acid inhibited osteoclastogenesis, the contribution of other lipids to the pathogenesis of RA remains unknown. Further studies are needed to clarify the effects of an altered lipid profile on RA.
Data Availability
The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request.
References
McInnes, I.B., and G. Schett. 2011. The pathogenesis of rheumatoid arthritis. New England Journal of Medicine 365: 2205–2219.
Xue, J., L. Xu, H. Zhu, M. Bai, X. Li, Z. Zhao, H. Zhong, G. Cheng, X. Li, F. Hu, et al. 2020. CD14(+)CD16(-) monocytes are the main precursors of osteoclasts in rheumatoid arthritis via expressing Tyro3TK. Arthritis Research & Therapy 22: 221.
Gengenbacher, M., H.J. Sebald, P.M. Villiger, W. Hofstetter, and M. Seitz. 2008. Infliximab inhibits bone resorption by circulating osteoclast precursor cells in patients with rheumatoid arthritis and ankylosing spondylitis. Annals of the Rheumatic Diseases 67: 620–624.
Shang, W., L.J. Zhao, X.L. Dong, Z.M. Zhao, J. Li, B.B. Zhang, and H. Cai. 2016. Curcumin inhibits osteoclastogenic potential in PBMCs from rheumatoid arthritis patients via the suppression of MAPK/RANK/c-Fos/NFATc1 signaling pathways. Molecular Medicine Reports 14: 3620–3626.
Leuti, A., D. Fazio, M. Fava, A. Piccoli, S. Oddi, and M. Maccarrone. 2020. Bioactive lipids, inflammation and chronic diseases. Advanced Drug Delivery Reviews 159: 133–169.
Dorochow, E., M. Kohm, L. Hahnefeld, and R. Gurke. 2022. Metabolic profiling in rheumatoid arthritis, psoriatic arthritis, and psoriasis: Elucidating pathogenesis, improving diagnosis, and monitoring disease activity. Journal of Personalized Medicine 12: 924.
Luczaj, W., A. Moniuszko-Malinowska, P. Domingues, M.R. Domingues, E. Gindzienska-Sieskiewicz, and E. Skrzydlewska. 2018. Plasma lipidomic profile signature of rheumatoid arthritis versus Lyme arthritis patients. Archives of Biochemistry and Biophysics 654: 105–114.
Cuppen, B.V., J. Fu, H.A. van Wietmarschen, A.C. Harms, S. Koval, A.C. Marijnissen, J.J. Peeters, J.W. Bijlsma, J. Tekstra, J.M. van Laar, et al. 2016. Exploring the Inflammatory Metabolomic Profile to Predict Response to TNF-alpha Inhibitors in Rheumatoid Arthritis. PLoS ONE 11: e0163087.
Luan, H., W. Gu, H. Li, Z. Wang, L. Lu, M. Ke, J. Lu, W. Chen, Z. Lan, Y. Xiao, et al. 2021. Serum metabolomic and lipidomic profiling identifies diagnostic biomarkers for seropositive and seronegative rheumatoid arthritis patients. Journal of Translational Medicine 19: 500.
Koh, J.H., S.J. Yoon, M. Kim, S. Cho, J. Lim, Y. Park, H.S. Kim, S.W. Kwon, and W.U. Kim. 2022. Lipidome profile predictive of disease evolution and activity in rheumatoid arthritis. Experimental & Molecular Medicine 54: 143–155.
Aletaha, D., T. Neogi, A.J. Silman, J. Funovits, D.T. Felson, C.O. Bingham 3rd., N.S. Birnbaum, G.R. Burmester, V.P. Bykerk, M.D. Cohen, et al. 2010. 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Annals of the Rheumatic Diseases 69: 1580–1588.
Saito, K., Y. Ohno, and Y. Saito. 2017. Enrichment of resolving power improves ion-peak quantification on a lipidomics platform. Journal of Chromatography. B, Analytical Technologies in the Biomedical and Life Sciences 1055–1056: 20–28.
Saito, K., M. Ikeda, Y. Kojima, H. Hosoi, Y. Saito, and S. Kondo. 2018. Lipid profiling of pre-treatment plasma reveals biomarker candidates associated with response rates and hand-foot skin reactions in sorafenib-treated patients. Cancer Chemotherapy and Pharmacology 82: 677–684.
Prevoo, M.L., M.A. van’t Hof, H.H. Kuper, M.A. van Leeuwen, L.B. van de Putte, and P.L. van Riel. 1995. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis & Rheumatism 38: 44–48.
Rodriguez-Carrio, J., M. Alperi-Lopez, P. Lopez, F.J. Ballina-Garcia, and A. Suarez. 2016. Non-Esterified Fatty Acids Profiling in Rheumatoid Arthritis: Associations with Clinical Features and Th1 Response. PLoS ONE 11: e0159573.
Huang, S., J.M. Rutkowsky, R.G. Snodgrass, K.D. Ono-Moore, D.A. Schneider, J.W. Newman, S.H. Adams, and D.H. Hwang. 2012. Saturated fatty acids activate TLR-mediated proinflammatory signaling pathways. Journal of Lipid Research 53: 2002–2013.
Lee, J.Y., K.H. Sohn, S.H. Rhee, and D. Hwang. 2001. Saturated fatty acids, but not unsaturated fatty acids, induce the expression of cyclooxygenase-2 mediated through Toll-like receptor 4. Journal of Biological Chemistry 276: 16683–16689.
Kochumon, S., H. Arefanian, R. Azim, S. Shenouda, T. Jacob, N. Abu Khalaf, F. Al-Rashed, A. Hasan, S. Sindhu, F. Al-Mulla, et al. 2020. Stearic acid and TNF-alpha Co-Operatively potentiate MIP-1alpha production in monocytic cells via MyD88 independent TLR4/TBK/IRF3 signaling pathway. Biomedicines 8: 403.
Kawabata, K., N. Baba, T. Sakano, Y. Hamano, S. Taira, A. Tamura, S. Baba, M. Natsume, T. Ishii, S. Murakami, et al. 2018. Functional properties of anti-inflammatory substances from quercetin-treated Bifidobacterium adolescentis. Bioscience, Biotechnology, and Biochemistry 82: 689–697.
Nishitani, Y., S. Okazaki, K. Imabayashi, R. Katada, K. Umetani, H. Yajima, and H. Matsumoto. 2007. Saturated and monounsaturated fatty acids increase interleukin-10 production in rat hepatocytes. Nihon Arukoru Yakubutsu Igakkai Zasshi 42: 32–35.
Pan, P.H., S.Y. Lin, Y.C. Ou, W.Y. Chen, Y.H. Chuang, Y.J. Yen, S.L. Liao, S.L. Raung, and C.J. Chen. 2010. Stearic acid attenuates cholestasis-induced liver injury. Biochemical and Biophysical Research Communications 391: 1537–1542.
Fischman, D., A. Valluri, V.S. Gorrepati, M.E. Murphy, I. Peters, and P. Cheriyath. 2010. Bilirubin as a Protective Factor for Rheumatoid Arthritis: An NHANES Study of 2003–2006 Data. Journal of Clinical Medical Research 2: 256–260.
Secchi, A.G., I. Fregona, and F. D’Ermo. 1979. Lysophosphatidyl choline in the aqueous humour during ocular inflammation. British Journal of Ophthalmology 63: 768–770.
Rikitake, Y., K. Hirata, S. Kawashima, S. Takeuchi, Y. Shimokawa, Y. Kojima, N. Inoue, and M. Yokoyama. 2001. Signaling mechanism underlying COX-2 induction by lysophosphatidylcholine. Biochemical and Biophysical Research Communications 281: 1291–1297.
Olofsson, K.E., L. Andersson, J. Nilsson, and H. Bjorkbacka. 2008. Nanomolar concentrations of lysophosphatidylcholine recruit monocytes and induce pro-inflammatory cytokine production in macrophages. Biochemical and Biophysical Research Communications 370: 348–352.
Ryborg, A.K., B. Deleuran, K. Thestrup-Pedersen, and K. Kragballe. 1994. Lysophosphatidylcholine: A chemoattractant to human T lymphocytes. Archives of Dermatological Research 286: 462–465.
Hung, N.D., D.E. Sok, and M.R. Kim. 2012. Prevention of 1-palmitoyl lysophosphatidylcholine-induced inflammation by polyunsaturated acyl lysophosphatidylcholine. Inflammation Research 61: 473–483.
Miyabe, Y., C. Miyabe, Y. Iwai, A. Takayasu, S. Fukuda, W. Yokoyama, J. Nagai, M. Jona, Y. Tokuhara, R. Ohkawa, et al. 2013. Necessity of lysophosphatidic acid receptor 1 for development of arthritis. Arthritis and Rheumatism 65: 2037–2047.
Santos, A.N., D. Riemann, A.N. Santos, A. Kehlen, K. Thiele, and J. Langner. 1996. Treatment of fibroblast-like synoviocytes with IFN-gamma results in the down-regulation of autotaxin mRNA. Biochemical and Biophysical Research Communications 229: 419–424.
Maekawa, K., K. Okemoto, M. Ishikawa, R. Tanaka, Y. Kumagai, and Y. Saito. 2017. Plasma Lipidomics of Healthy Japanese Adults Reveals Gender- and Age-Related Differences. Journal of Pharmaceutical Sciences 106: 2914–2918.
Fu, J., B.V. Cuppen, P.M. Welsing, H. van Wietmarschen, A.C. Harms, R. Barger, S. Koval, R.D. Fitsch-Stork, J.W. Bijlsma, T. Hankemeier, et al. 2016. Differences between serum polar lipid profiles of male and female rheumatoid arthritis patients in response to glucocorticoid treatment. Inflammopharmacology 24: 397–402.
Maranini, B., A. Bortoluzzi, E. Silvagni, and M. Govoni. 2022. Focus on Sex and Gender: What We Need to Know in the Management of Rheumatoid Arthritis. Journal of Personalized Medicine 12: 499.
Funding
This work was supported in part by a Research Promotion Grant from Toho University Graduate School of Medicine (No. 17–01, 20–01); the Program for the Strategic Research Foundation for Private Universities (S1411015) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; and the Private University Research Branding Project from the Ministry of Education, Culture, Sports, Science, and Technology, Japan.
Author information
Authors and Affiliations
Contributions
SMasuoka, SY, AI, SK, YS, and TN contributed to the design of the study. All authors contributed to material collection, material preparation, and data collection or analysis. SMasuoka and TN wrote the draft of the manuscript. All authors reviewed the manuscript and approved the final draft.
Corresponding author
Ethics declarations
Ethical Approval
The study protocol was approved by the Ethics Committees of the Faculty of Medicine, Toho University (approval numbers: A22060_A19020_A17059_A16030 and A21014_A18084_27060) and National Institute of Health Sciences (approval numbers: 271, 271–2, 271–3). All participants provided their written informed consent for this study.
Competing Interests
JN received research funding from Asahi Kasei Pharma Corp., Chugai Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Boehringer Ingelheim Co., Ltd., Nippon Kayaku Co., Ltd., Ayumi Pharmaceutical Corp., Abbvie GK, Abbott Japan LLC, and GlaxoSmithKline plc. KK has received research grants and/or speaking fees from AbbVie GK, Astellas Pharma Inc., AstraZeneca K.K., Chugai Pharmaceutical Co., Ltd., Daiichi Sankyo Co. Ltd., Eisai Co., Ltd., Eli Lilly Japan K.K., GlaxoSmithKline plc., Janssen Pharmaceutical K.K., Mitsubishi Tanabe Pharma Corp., Ono Pharmaceutical Co., Ltd., Pfizer Japan Inc., and Teijin Pharma Ltd. HS has received speaking fees and/or teaching fees from Chugai Pharmaceutical Co., Ltd., Eisai Co., Ltd., Eli Lilly Japan K.K., Janssen Pharmaceutical K.K., Ono Pharmaceutical Co., Ltd., Asahi Kasei Pharma Corp., and Taisho Pharmaceutical Co., Ltd. SMuraoka has received consultant fee from Asahi Kasei Pharma Corp., and speaker’s bureau from Ono Pharmaceutical Co., Ltd., Eisai Co., Ltd., Asahi Kasei Pharma Corp. and Astellas Pharma Inc. MK has received speaking fees from Ayumi Pharmaceutical Corp., Asahi Kasei Pharma Corp., AstraZeneca K.K., Chugai Pharmaceutical Co., Ltd., Gilead Sciences Inc, GlaxoSmithKline K.K., Mitsubishi-Tanabe Pharma Corp., Nippon Boehringer Ingelheim Co., Ltd. and Taisho Pharmaceutical Co., Ltd. SMizutani received lectures fees from Janssen Pharmaceutical K.K., Bristol-Myers Squibb Co., Chugai Pharmaceutical Co., Ltd., Mitsubishi-Tanabe Pharma Corp., Novartis Pharma K.K., Eli Lilly Japan K.K., Asahikasei Pharma Corp., Taisho Pharma Co., Ltd., and Ono Pharmaceutical Co., and speakers fees from Chugai Pharmaceutical Co., Ltd., Mitsubishi-Tanabe Pharma Corp., Novartis Pharma K.K., Asahikasei Pharma Corp. and Taisho Pharma Co., Ltd. SK has received research grants and/or speaking fees from AbbVie GK, Astellas Pharma Inc., Ayumi Pharmaceutical Corp., Chugai Pharmaceutical Co., Ltd., Daiichi Sankyo Co. Ltd., Eisai Co., Ltd., Eli Lilly Japan K.K., Janssen Pharmaceutical K.K., Mitsubishi Tanabe Pharma Corp., Nippon Zoki Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Pfizer Japan Inc., Santen Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., and Teijin Pharma Ltd. TN received grant/research support from Chugai Pharmaceutical Co., Ltd, Eisai Co., Ltd., Eli Lilly Japan K.K., Bristol Myers Squibb Co., Ono Pharmaceutical Co., Ltd., Asahikasei Pharma Corp., Mitsubishi Tanabe Pharma Corp., Ayumi Pharmaceutical Corp, Nippon Kayaku Co., Ltd., AbbVie GK, Sanofi K.K., Teijin Pharma Ltd., Taisho Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd., Astellas Pharma Inc., UCB Japan Co., Ltd., Pfizer Japan Inc. and Takeda Pharmaceutical Co., Ltd., consultant fees from UCB Japan Co., Ltd., Eisai Co., Ltd. and Chugai Pharmaceutical Co., Ltd., and speakers fees from Ono Pharmaceutical Co., Ltd., Chugai Pharmaceutical Co., Ltd., Eisai Co., Ltd., Astellas Pharma Inc., Janssen Pharmaceutical K.K., Pfizer Japan Inc., Asahikasei Pharma Corp., Eli Lilly Japan K.K., Mylan N.V., AbbVie GK, Takeda Pharmaceutical Co., Ltd., Ayumi Pharmaceutical Corp., Daiichi Sankyo Co., Ltd., Mitsubishi Tanabe Pharma Corp., UCB Japan Co. Ltd., Nippon Kayaku Co., Ltd., Sanofi K.K., Teijin Pharma Ltd., Gilead Sciences, Inc. and Taisho Pharmaceutical Co., Ltd. The remaining authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Masuoka, S., Nishio, J., Yamada, S. et al. Relationship Between the Lipidome Profile and Disease Activity in Patients with Rheumatoid Arthritis. Inflammation 47, 1444–1458 (2024). https://doi.org/10.1007/s10753-024-01986-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-024-01986-8