Abstract
The increased cardiovascular risk in RA (rheumatoid arthritis) cannot be explained by common quantitative circulating lipid parameters. The objective of the study was to characterize the modifications in HDL phosphosphingolipidome in patients with RA to identify qualitative modifications which could better predict the risk for CVD. Nineteen patients with RA were compared to control subjects paired for age, sex, BMI, and criteria of metabolic syndrome. The characterization of total HDL phosphosphingolipidome was performed by LC-MS/MS. RA was associated with an increased HDL content of lysophosphatidylcholine and a decreased content of PC (phosphatidylcholine), respectively, positively and negatively associated with cardiovascular risk. A discriminant molecular signature composed of 18 lipids was obtained in the HDL from RA patients. The detailed analysis of phospholipid species showed that molecules carrying omega-3 FA (fatty acids), notably docosahexaenoic acid (C22:6 n-3), were depleted in HDL isolated from RA patients. By contrast, two PE (phosphatidylethanolamine) species carrying arachidonic acid (C20:4 n-6) were increased in HDL from RA patients. Furthermore, disease activity and severity indexes were associated with altered HDL content of 4 PE and 2 PC species. In conclusion, the composition of HDL phosphosphingolipidome is altered during RA. Identification of a lipidomic signature could therefore represent a promising biomarker for CVD risk. Although a causal link remains to be demonstrated, pharmacological and nutritional interventions targeting the normalization of the FA composition of altered phospholipids could help to fight against RA-related inflammation and CVD risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease characterized by progressive joint destruction, disability and premature death with an increased CVD mortality due to accelerated atherosclerosis [4]. The CVD mortality is increased by 50% and the risk of major adverse cardiovascular events by 48% in the RA population compared to the general population [5]. RA itself is an independent CVD risk factor that carries as much weight as type 2 diabetes [21]. The reasons resulting in CVD risk excess are still to be clarified. Traditional CVD risk factors (hypertension, metabolic syndrome, smoking, age) only partly explain the increased CVD risk in rheumatic diseases [23, 25]. Chronic inflammation promotes atherosclerosis, exacerbates the effects of established CVD risk factors, and contributes to the alterations in lipid profiles. Hence, in the context of inflammatory arthritis, the traditional atherogenic lipid profile characterized by increased low-density lipoprotein-cholesterol (LDL-C) and decreased high-density lipoprotein-cholesterol (HDL-C) levels is not observed. Paradoxically, an inverse relationship between CVD risk and lipid levels, also termed the “lipid paradox”, was reported during active RA leading to reduced levels of total cholesterol, LDL-C, and HDL-C, though the CVD risk was enhanced [24], suggesting lipoprotein dysfunctions in addition to quantitative abnormalities [3, 14, 17]. Hence, inflammation may lead to modifications in the lipoprotein composition, thereby altering protective functions of HDL such as antioxidative properties and cholesterol efflux capacities. A more relevant diagnostic tool of CVD risk consisting in the determination of the composition of small atherogenic HDL particles was recently proposed [14]. Alterations in the lipidome (PA, PI, and PG contents) of small and dense HDL particles were already described in a small sample population of RA patients suggesting specific alterations in some subfractions. However, isolation of small HDL subpopulations is, however, laborious and cannot be readily employed in clinical studies. Identification of specific biomarkers in the total HDL fraction could therefore represent a useful predictive tool.
The main objective of this study was to investigate qualitative and quantitative changes in phospholipid (PL) and sphingolipid (SL) composition of HDL by lipidomic analysis in a RA population in comparison to age- and sex-matched control subjects. The secondary objective was to correlate PL and SL profiles in HDL to disease’s characteristics and CVD risk. This is a pilot study aiming to identify a phenotype using the lipidome associated with elevated CVD risk in these populations, thereby improving the physiopathological understanding and the risk prediction for these patients.
Materials and methods
Description of RA population
Patients over 18 years old with RA and starting first biologic disease-modifying anti-rheumatic drugs (DMARD) were included from 2014 in the longitudinal cohort of RCVRIC analyzing cardiovascular risk and chronic inflammatory rheumatism (PHRC RCVRIC AOI 2014 N° ID-RCB-A01847-40). The patients fulfilled the 2010 RA classification criteria [2] and had active disease as defined by disease activity score in 28 joints (DAS28) > 3.2.
Standard demographic data, disease and imaging characteristics, and cardiometabolic profile of patients were recorded at inclusion. The duration, extra articular manifestations, the presence of rheumatoid factor and/or anti-CCP antibodies, and biological markers of inflammation (erythrocyte sedimentation rate (ESR; mm/h) and circulating concentration of C-reactive protein (CRP; mg/l)) were recorded. RA activity was evaluated by the DAS 28VS/CRP. All treatments were registered: conventional or biological DMARDs, steroids, nonsteroidal anti-inflammatory drugs (NSAIDs). Radiographic erosions were recorded on baseline feet and hands X-ray.
Patients were questioned for common cardiovascular risk factors including age, sex, family, or personal history of cardiovascular disease, such as stroke, myocardial infarction or sudden death, type 2 diabetes or impaired fasting glucose, past and current smoking, history of hypertension, dyslipidemia (plasma LDL-C, HDL-C, and TG), familial dyslipidemia. Blood pressure, body weight, body height, and waist circumference were measured. Ten-year CVD risk was calculated using the Systematic COronary Risk Evaluation (SCORE) equation [1].
Common clinical blood parameters were evaluated and recorded, including blood cell count, ESR, C-reactive protein (CRP), fasting blood glycemia, insulin, and creatinine.
Patients with pathologies or treatments which could interfere with lipid profile (hereditary dyslipidemia, thyroid disease, kidneys and/or liver deficiency, dyslipidemia treatment, diabetes mellitus, pregnancy, chronic infections, active neoplasia, ethanol consumption of > 30 g a day) were excluded.
Control subjects
Non-RA controls were recruited in the RESOLVE (REverse metabolic SyndrOme by Lifestyle and Various Exercises) trial between May 2009 and October 2011 [10] and matched with RA patients for age, sex, BMI, and criteria of metabolic syndrome. For matching, BMI was categorized as < 25 kg/m2, 25–30 kg/m2, and > 30 kg/m2.
Blood samples and analysis
Plasma was collected at inclusion for each patient and control subject, aliquoted and stored at − 80 °C until analyses. Plasma levels of TG, glucose, total cholesterol, HDL-C, and apolipoproteins A1 (apoA1) and B (apoB) were quantified on KONELAB analyzer (ThermoFisher Scientific, Massachusetts, USA). Circulating insulin was evaluated using an enzyme-linked immunosorbent assay (ELISA) according to the manufacturer instructions (kit reference KAQ1251, Fisher Scientific, Illkirch, France). Each assay was performed in duplicate with an intra-assay variation < 10%. Insulin resistance was evaluated using the HOMA-IR homeostatic model [(fasting insulin × fasting glucose) / 22.5].
Isolation of HDL from plasma
Plasma lipoproteins were separated according to their respective densities using serial ultracentrifugation using a Beckman Coulter LE-80k ultracentrifugation system and a Type 100 Ti rotor (Beckman Coulter France, Villepinte, France). For the first ultracentrifugation, 400 μl of plasma was deposited in a 2-ml quick seal tube (Beckman Coulter France), supplemented with 1000 μl of a potassium bromide (KBr) solution of a density of 1.006 g/ml for a total volume of 1400 μl. Then, 448 μl of a KBr solution of a density of 1.24 g/ml was added to obtain a final density of 1.063 g/ml. Ultracentrifugation was performed at 80,000 rpm (512,312 g) for 8.5 h at 15 °C, allowing HDL to be separated from the other lipoproteins. Very low and low-density lipoproteins located in the upper half of the tube were discarded. The lower half (approx 850 μl) containing HDL was recovered and mixed with 1086 μl of a new KBr solution of a density of 1.34 g/ml to obtain final density of 1.21 g/ml. This solution was then centrifuged at 80,000 rpm for 14.5 h at 15 °C to isolate HDL particles. Finally, 725 μl of the upper phase containing HDL was recovered. The samples were extensively dialyzed against PBS. After three changes of dialysis buffer (every 5–8 h), samples were stored in cryotubes at − 80 °C until lipidomic analyses.
Lipidomics analysis of HDL
HDL lipidomic analysis was performed by LC-MS/MS to assess the composition in phospholipid (PL) and sphingolipid (SL) subclasses and their corresponding molecular species, specifically those of phosphatidylcholine (PC), lysophosphatidylcholine (LPC), phosphatidylethanolamine (PE), phosphatidylinositol (PI), phosphatidylserine (PS), phosphatidylglycerol (PG), phosphatidic acid (PA), sphingomyelin (SM), and ceramides (Cer).
Lipids were isolated using the modified Folch’s method [19]. Briefly, 0.8 ml of water was added to 30 μg of enzymatically quantified phospholipids before adding 0.8 ml of acidified methanol containing a mixture of internal standards and 0.8 ml of chloroform. The suspension was vortexed for 1 min and centrifuged at 3600g for 10 min at 4 °C. Lipids were recovered and dried before dissolution into LC/MS solvent. Internal standards were purchased from Avanti Polar Lipids (Alabaster, AL, USA). LC-MS-grade solvents were used without further purification and obtained from Sigma-Aldrich (St Louis, MO, USA). Lipids were quantified by LC-ESI/MS/MS using a Prominence UFLC (Shimadzu, Tokyo, Japan) and QTrap 4000 mass spectrometer (AB Sciex, Framingham, MA, USA) equipped with a turbo spray ion source (450 °C) combined with an LC20AD HPLC system, a SIL-20AC autosampler (Shimadzu, Kyoto, Japan), and the Analyst 1.5 data acquisition system (AB Sciex, Framingham, MA, USA).
Quantification of PL and SL molecular species was performed in positive ion mode. Sample (4 μl) was injected to a Kinetex HILIC 2.6-μm 2.1 × 150-mm column (Phenomenex, CA, USA) maintained at 45 °C. Lipid species were detected using scheduled multiple reaction monitoring (sMRM) reflecting the head group fragmentation of each lipid class. Typically, PC, LPC, and SM species were detected as product ions of m/z 184, PE, PI, PS, PG, and PA as neutral losses of, respectively, m/z 141, 277, 185, 189, and 115 as described previously [29]. Nitrogen was used as nebulization and collision gas. Air was used for exhaust.
An in-house developed R script adapted from Ejsing CS et al. [11] was used to correct for isotopic contribution to MRM signals. Lipids were quantified using 37 calibration curves specific for the 16 individual lipid subclasses and up to 12 fatty acid (FA) moieties. More abundant lipid species which displayed non-linear response in non-diluted extracts (typically PC and SM) were quantified from a 20-fold diluted sample. Structural determination of major PL chains was performed by LC/MS/MS using a reversed-phase separation onto a symmetry shield RP8 50 mm × 2.1 mm, 3.5-μm column (Waters Corporation, Milford, MA, USA) as previously described [7] and negative ionization using precursor ion scans (PIS) of FA chains.
Statistical analysis
Sample size was estimated according to (i) the CONSORT 2010 statement, extension to randomized pilot and feasibility trials [12] and (ii) Cohen’s recommendations [8], which define effect-size bounds as follows: small (ES: 0.2), medium (ES: 0.5), and large (ES: 0.8, “grossly perceptible and therefore large”). We were able to collect data and perform biochemical explorations on 19 RA patients. To maximize the sample size in RA group, one control was paired with two patients. The characteristics of the 19 RA patients and 18 control subjects are shown in Table 1. With 19 paired subjects per group, a minimal effect size greater than 0.8 could be highlighted, for a two-sided type I error at 1% (correction due to multiple comparisons) and a statistical power at 80%. All statistical analyses were performed using Stata software (version 13, StataCorp, College Station, TX) and R software (https://cran.r-project.org/, with ADE4 package). The analyses were carried out for a two-sided type I error at 5%. Continuous variables were presented as mean and standard deviation (SD) or median and interquartile range. The assumption of normality was evaluated using the Shapiro-Wilk test. Then, quantitative variables were compared between groups by Student’s t test or Mann-Whitney test if assumptions of t test were not met (normality, homoscedasticity analyzed using Fisher-Snedecor test). The results were expressed as effect size (ES) and 95% confidence interval. For categorical variables, comparisons between groups were done by Chi-squared or when appropriate by Fischer’s exact test. Random-effects models were added to statistical plan in order to measure and model possible effect of matching (between and within pair variability, as random-effect). Finally, multivariable analyses were performed using multiple regression models to take into account possible confounding variables determined according to the results of univariate analyses and to the clinical relevance: age, tobacco consumption, steroids use. The normality of residuals was checked for all models. When appropriate, a logarithmic transformation was applied to access the normality of the distributions of dependent variables. To take into account multiple comparisons, correction of type I error proposed by Benjamini-Hochberg was applied.
Multidimensional analyses as factorial mixed data analysis (FMDA) were used in order to analyze assets as elements of qualitative and quantitative variables. This method allows to (1) uncover the underlying relationships and structures of the measured variables and (2) to aggregate subjects into clusters. When quantitative and categorical data are studied together, quantitative variables were transformed and categorized to generate an exploratory multiple correspondence analysis.
Results
Characteristics of rheumatoid arthritis patients and matched non-rheumatoid arthritis controls
The characteristics of control and RA subjects could be found in Table 1. RA patients had inflammatory active disease as defined by a DAS28 higher than 3.2 and high CRP levels. The disease had been evolving for several years and was severe, associated with erosive destruction of cartilage and bone in more than a half of the patients and with rheumatoid factor or anti-cyclic citrullinated protein antibodies in the majority of them. Current treatment with steroids was reported in 53% of patients and with methotrexate in 79% of patients. RA patients had more CVD risk factors and exhibited a non-significant elevation of their CVD risk (SCORE equation) compared to controls. In contrast, plasmatic parameters related to lipid metabolism (cholesterol, LDL-C, TG, apoA1, apoB) did not differ between controls and RA patients (Table 1). Only HDL-C was marginally, but not significantly, reduced in RA patients. Atherogenic index, as defined by the total cholesterol to HDL-C ratio, did not differ between the groups. As indexes of metabolic status, the concentration of insulin and glucose in plasma was not affected in RA patients. Thus, HOMA index was also similar between RA and control groups (Table 1).
Lipidome of HDL particles in RA patients compared to controls
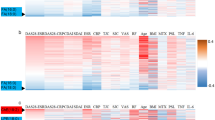
Statistical analyses of lipidomic data were performed after adjustments for age, sex, smoking status, and the use of corticosteroid therapy. Among the main phospholipid classes, a reduced proportion of PC (− 2.4% vs control, p < 0.05) and an increased proportion of LPC (+ 30% vs control, p < 0.05) were observed in RA patients (Fig. 1). Proportions of PE, PI, PA, SM, LPC, and LPE in HDL were similar between RA patients and controls. As shown in Table 2, we identified 18 molecular species in HDL which were significantly affected by RA (p < 0.05 vs control group). The highest magnitudes of variation (as illustrated by the size effect) were observed for PC 40:8 (18:2_22:6), LPC 16:0, and LPC 18:0 (Table 3). The elucidation of the FA composition of these phospholipids indicated a reduced levels of the omega-3 fatty acids docosahexaenoic acid (DHA, C22:6 n-3) in PC compared to controls (Table 4). The complete list of these species and their relative abundance in RA and control subjects is provided in Supplementary Table S1. The detailed chemical characterization of the most abundant PL species can be found in Supplementary Table S2. A hierarchical clustering of subjects using significant PL showed a good separation of patients and control subjects (Fig. 2).
Classification of subjects according to lipidomic data heatmap representing relative amounts of discriminant lipids in plasma HDL between RA and control (C) subjects. Variables with a very low absolute value were removed from the analysis (CER 18:1–26:0 and PG 38:6). Rows (subjects) and columns (variables) were clustered using the Pearson correlation to define similarity and Ward linkage rule
Associations between HDL phospholipid profile, disease’s characteristics, and CVD risk
A multidimensional analysis was performed to identify associations between HDL lipidome and clinical parameters. As shown in Fig. 3, we observed an association between HDL abundances of total LPC, LPC 16:0, LPC 18:0, LPE 18:0, atherogenic index, apoB to apoA1 ratio, plasma triglycerides, and RA population. Phospholipid species for which abundance in HDL was the most strongly associated with RA activity (DAS28, CRP) and severity (erosion, seropositivity for rheumatoid factors or anti-CCP) included PE 38:4 and PE 36:4 carrying arachidonic acid (C20:4 n-6), PE 34:2, PE 38:3, PC 38:3, and PC 40:4. Abundances of those PL were also associated with traditional CVD risk factors, such as high blood pressure (hbp), tobacco use, insulin level, and NSAID use. By contrast, abundances of PC 40:7 and PC 40:8, which contain 50% of C22:6 n-3 fatty acid, and HDL-C exhibited inverse associations with RA indexes (Fig. 3).
Multiple factorial analysis of clinical and biological characteristics and discriminant lipids. Each subject is labeled with a dot. The left panel shows association between variables. The right panel shows the segregation between RA (red) and control (blue) groups according to the association between variables as represented on the left panel; each dot represents a subject from RA or control groups
Discussion
The present study aimed to determine a molecular lipid signature in the total HDL from a population of RA patients in comparison to control subjects matched for age, sex, and BMI. Because classical risk factors could not be used as the most relevant predictors of mortality due to CVD [15], the HDL lipidomic signature would help to better predict the CVD risk in RA patients. We then explored a more qualitative view of HDL composition and observed that RA induced specific alterations in the HDL lipidome. The analysis of the main PL and SL classes in HDL showed an enrichment of LPC and a depletion of PC in RA patients. LPC and PC were, respectively, positively and negatively associated with cardiovascular risk. No other major PL fractions were globally altered. HDL was proposed to be able to trap LPC in order to prevent LDL from oxidative damage [18]. A higher degree of LDL oxidation in RA patients in the present study remains to be demonstrated, but this hypothesis could explain the increased percentage of LPC in HDL from RA patients. A second hypothesis would be an increased degradation of PC leading to a higher generation of LPC from PC. Hence, an increased activity of Lp-PLA2 which catalyzes the hydrolysis of oxidized PC to generate LPC and oxidized non-esterified FA has been proposed as a biomarker of chronic inflammation and a predictor of CVD [20, 28]. Finally, a third hypothesis would link the decrease in HDL PC content and a reduction in PC synthesis from PE by PEMT, notably in the liver. PC with long polyunsaturated FA is preferentially synthetized by this pathway [9]. The activity of the enzyme is sensitive to individual’s status in vitamins of the B family and homocysteine [27]. This hypothesis would require complementary investigations because the prevalence of vitamin B12 deficiency could be slightly increased in RA patients [13]. Very high levels of CRP are frequently observed in RA patients and are strongly associated with CVD risk [15]. We confirmed the association between plasma CRP, DA28, and some risk factors for CVD index in RA patients. Moreover, these markers of RA activity were associated with an enrichment in four molecular species of PE, two molecular species of PC, and a depletion of three other molecular species of PC in the total HDL fraction. The detailed analysis of PL species showed that molecules carrying omega-3 FA, notably docosahexaenoic acid (C22:6 n-3), were depleted in HDL isolated from RA patients. By contrast, two molecular PE species carrying arachidonic acid (C20:4 n-6) were increased in HDL isolated from RA patients. Dietary intakes were not recorded in this study, but it should be noted that the French population has an inadequate intake of omega 3 FA [26]. Although we cannot completely rule out a possible different intake of omega 3 FA between the two groups, these observations are in agreement with the anti-inflammatory and pro-inflammatory properties of omega-3 and omega-6 FA, respectively. Polyunsaturated omega-3 FA are converted to bioactive anti-inflammatory and pro-revolving mediators called protectins and resolvins [6]. The proinflammatory cyclooxygenase (COX) pathway is probably strongly involved in the pathology of RA. Omega-3 FA are good inhibitors of this pathway that is on the contrary activated by arachidonic acid. It has been demonstrated that the use of fish oil, enriched in long chain omega-3 FA, represents a relevant nutritional therapy against RA-related inflammation and CVD risk [22]. On the other hand, the levels of saturated FA-containing LPCs were elevated during the disease. Notably, a 1.9-fold increase in LPC containing palmitic acid (C16:0) was detected in HDL from RA patients. This PL was previously associated with metabolic abnormalities in the liver [16].
The combined exploration of clinical and biochemical data demonstrated the association between inflammatory markers, CVD risk, and PL composition of HDL in RA patients. It validates the concept that the use of HDL lipidome could be a promising target for further validation of these biomarkers in a larger population. It would be relevant to determine if a normalization of the sphingolipidomic signature could be obtained in patients receiving a therapy. Although the present study has provided preliminary promising data, it has some limitations. First, the evaluation of cardiovascular risk was performed using blood lipid parameters in a RA population. Other relevant biomarkers of both inflammation (haptoglobin, SAA protein, or fibrinogen) and CVD risk together with subclinical atherosclerosis assessment (vascular function and structural remodeling), which could not be measured here, should be determined in the future to explore their association with HDL lipidome in a larger population of patients. This population should also better reflect a women/men ratio of 4–5 as observed in the RA population. Finally, alterations in HDL PL composition should also be correlated with atheroprotective functionality of HDL particles.
Conclusion
We identified 5 PC, 4 PE, 4 lysophospholipids, 2 PI, 1 PG, 1 PS, and 1 ceramide which were differentially represented in HDL isolated from RA patients as compared to paired control subjects. The use of the relative amount of these molecules for a hierarchical clustering of subjects allowed a good separation of RA and control groups. We identified PL species associated with inflammation or CVD risk that were increased in HDL from RA patients. On the contrary, omega-3 FA with anti-inflammatory properties were depleted suggesting that nutritional and pharmacological interventions aiming at modifying PL composition of HDL could help to reduce RA-related inflammation and CVD risk. These results warrant to be confirmed with further investigations on a larger population.
Abbreviations
- apoA1:
-
apolipoprotein A1
- apoB:
-
apolipoprotein B
- Cer:
-
ceramides
- CRP:
-
c-reactive protein
- HOMA-IR:
-
Homeostatic Model Assessment of Insulin Resistance
- LPC:
-
lysophosphatidylcholine
- NSAIDs:
-
nonsteroidal anti-inflammatory drugs
- PA:
-
phosphatidic acid
- PC:
-
phosphatidylcholine
- PE:
-
phosphatidylethanolamine
- PG:
-
phosphatidylglycerol
- PI:
-
phosphatidylinositol
- PL:
-
phospholipids
- PS:
-
phosphatidylserine
- RA:
-
rheumatoid arthritis
- SCORE:
-
Systematic COronary Risk Evaluation
- SL:
-
sphingolipids
References
Agca R, Heslinga SC, Rollefstad S, Heslinga M, McInnes IB, Peters MJL, Kvien TK, Dougados M, Radner H, Atzeni F, Primdahl J, Södergren A, Wallberg Jonsson S, van Rompay J, Zabalan C, Pedersen TR, Jacobsson L, de Vlam K, Gonzalez-Gay MA, Semb AG, Kitas GD, Smulders YM, Szekanecz Z, Sattar N, Symmons DPM, Nurmohamed MT (2017) EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis 76(1):17–28
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO, Birnbaum NS, Burmester GR, Bykerk VP, Cohen MD, Combe B, Costenbader KH, Dougados M, Emery P, Ferraccioli G, Hazes JM, Hobbs K, Huizinga TW, Kavanaugh A, Kay J, Kvien TK, Laing T, Mease P, Menard HA, Moreland LW, Naden RL, Pincus T, Smolen JS, Stanislawska-Biernat E, Symmons D, Tak PP, Upchurch KS, Vencovsky J, Wolfe F, Hawker G (2010) 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis 69(9):1580–1588
Annema W, von Eckardstein A (2013) High-density lipoproteins. Multifunctional but vulnerable protections from atherosclerosis. Circ J 77(10):2432–2448
Avina-Zubieta JA, Choi HK, Sadatsafavi M, Etminan M, Esdaile JM, Lacaille D (2008) Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum 59(12):1690–1697
Avina-Zubieta JA, Thomas J, Sadatsafavi M, Lehman AJ, Lacaille D (2012) Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis 71(9):1524–1529
Calder PC (2010) Omega-3 fatty acids and inflammatory processes. Nutrients 2(3):355–374
Camont L, Lhomme M, Rached F, le Goff W, Nègre-Salvayre A, Salvayre R, Calzada C, Lagarde M, Chapman MJ, Kontush A (2013) Small, dense high-density lipoprotein-3 particles are enriched in negatively charged phospholipids: relevance to cellular cholesterol efflux, antioxidative, antithrombotic, anti-inflammatory, and antiapoptotic functionalities. Arterioscler Thromb Vasc Biol 33(12):2715–2723
Cohen J. second ed (1988) Statistical Power Analysis for the Behavioral Sciences, ed. J. Cohen: Hillsdale, NJ: Lawrence Erlbaum Associates, Publishers
DeLong CJ, Shen YJ, Thomas MJ, Cui Z (1999) Molecular distinction of phosphatidylcholine synthesis between the CDP-choline pathway and phosphatidylethanolamine methylation pathway. J Biol Chem 274(42):29683–29688
Dutheil F, Lac G, Lesourd B, Chapier R, Walther G, Vinet A, Sapin V, Verney J, Ouchchane L, Duclos M, Obert P, Courteix D (2013) Different modalities of exercise to reduce visceral fat mass and cardiovascular risk in metabolic syndrome: the RESOLVE randomized trial. Int J Cardiol 168(4):3634–3642
Ejsing CS, Duchoslav E, Sampaio J, Simons K, Bonner R, Thiele C, Ekroos K, Shevchenko A (2006) Automated identification and quantification of glycerophospholipid molecular species by multiple precursor ion scanning. Anal Chem 78(17):6202–6214
Eldridge SM, Chan CL, Campbell MJ et al (2016) CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud 2:64
Emamifar A, Jensen Hansen IM (2018) The influence of thyroid diseases, diabetes mellitus, primary hyperparathyroidism, vitamin B12 deficiency and other comorbid autoimmune diseases on treatment outcome in patients with rheumatoid arthritis: an exploratory cohort study. Medicine (Baltimore) 97(21):e10865
Gomez Rosso L, Lhomme M, Merono T et al (2014) Altered lipidome and antioxidative activity of small, dense HDL in normolipidemic rheumatoid arthritis: relevance of inflammation. Atherosclerosis 237(2):652–660
Goodson NJ, Symmons DP, Scott DG, Bunn D, Lunt M, Silman AJ (2005) Baseline levels of C-reactive protein and prediction of death from cardiovascular disease in patients with inflammatory polyarthritis: a ten-year followup study of a primary care-based inception cohort. Arthritis Rheum 52(8):2293–2299
Huang Y, Fu JF, Shi HB, Liu LR (2011) Metformin prevents non-alcoholic fatty liver disease in rats: role of phospholipase A2/lysophosphatidylcholine lipoapoptosis pathway in hepatocytes. Zhonghua Er Ke Za Zhi 49(2):139–145
Liao KP, Playford MP, Frits M, Coblyn JS, Iannaccone C, Weinblatt ME, Shadick NS, Mehta NN (2015) The association between reduction in inflammation and changes in lipoprotein levels and HDL cholesterol efflux capacity in rheumatoid arthritis. J Am Heart Assoc 4(2)
Mahfouz MM, Kummerow FA (2003) High density lipoprotein can modulate the inhibitory effect of oxLDL on prostacyclin generation by rat aorta in vitro. Prostaglandins Other Lipid Mediat 72(3–4):91–114
Milne S, Ivanova P, Forrester J, Alex Brown H (2006) Lipidomics: an analysis of cellular lipids by ESI-MS. Methods 39(2):92–103
Oei H-HS, IMvd M, Hofman A et al (2005) Lipoprotein-associated phospholipase A2 activity is associated with risk of coronary heart disease and ischemic stroke. Circulation 111(5):570–575
Peters MJ, van Halm VP, Voskuyl AE et al (2009) Does rheumatoid arthritis equal diabetes mellitus as an independent risk factor for cardiovascular disease? A prospective study. Arthritis Rheum 61(11):1571–1579
Proudman SM, James MJ, Spargo LD, Metcalf RG, Sullivan TR, Rischmueller M, Flabouris K, Wechalekar MD, Lee AT, Cleland LG (2015) Fish oil in recent onset rheumatoid arthritis: a randomised, double-blind controlled trial within algorithm-based drug use. Ann Rheum Dis 74(1):89–95
Robertson J, Peters MJ, McInnes IB, Sattar N (2013) Changes in lipid levels with inflammation and therapy in RA: a maturing paradigm. Nat Rev Rheumatol 9(9):513–523
Semb AG, Kvien TK, Aastveit AH, Jungner I, Pedersen TR, Walldius G, Holme I (2010) Lipids, myocardial infarction and ischaemic stroke in patients with rheumatoid arthritis in the apolipoprotein-related mortality RISk (AMORIS) study. Ann Rheum Dis 69(11):1996–2001
Tournadre A, Mathieu S, Soubrier M (2016) Managing cardiovascular risk in patients with inflammatory arthritis: practical considerations. Ther Adv Musculoskelet Dis 8(5):180–191
Tressou J, Pasteau S, Darrigo Dartinet S, Simon N, Le Guillou C (2016) Données récentes sur les apports en acides gras des Français. OCL 23(3):D303
Vance DE (2014) Phospholipid methylation in mammals: from biochemistry to physiological function. Biochim Biophys Acta 1838(6):1477–1487
Zalewski A, Macphee C (2005) Role of lipoprotein-associated phospholipase A2 in atherosclerosis: biology, epidemiology, and possible therapeutic target. Arterioscler Thromb Vasc Biol 25(5):923–931
Zemski Berry KA, Murphy RC (2004) Electrospray ionization tandem mass spectrometry of glycerophosphoethanolamine plasmalogen phospholipids. J Am Soc Mass Spectrom 15(10):1499–1508
Acknowledgments
We are grateful to Jean Paul Rigaudière, Chrystèle Jouve and Sarah de Saint Vincent for their technical assistance.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
This work was supported by a grant from the French Minister of health (PHRC RCVRIC AOI 2014) and from UCB (“Bourse Sirius”).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study was approved by the local ethics committee (Institutional Review Boards: 2014-A01847-40). All patients received verbal and written information and signed a consent form prior to inclusion. Control subjects were recruited via advertisements. They provided written informed consent. The RESOLVE study was reviewed and approved by the human ethics committees from St Etienne, France.
Consent for publication
All authors have seen and approved the manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• RA induced alterations in phospholipid and sphingolipid composition of HDL
• Phospholipids carrying omega-3 fatty acids were depleted during RA
• HDL lipidome was associated with disease activity and severity
• A signature composed of 18 lipids allowed to discriminate patients and controls
Electronic supplementary material
ESM 1
(DOCX 58.5 kb)
Rights and permissions
About this article
Cite this article
Giraud, C., Tournadre, A., Pereira, B. et al. Alterations of HDL particle phospholipid composition and role of inflammation in rheumatoid arthritis. J Physiol Biochem 75, 453–462 (2019). https://doi.org/10.1007/s13105-019-00694-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-019-00694-4