Abstract
Prior studies demonstrated the association between the major adverse cardiovascular outcomes and both higher platelet and lower lymphocyte counts. Our study explores the value of the platelet/lymphocyte ratio (PLR) as a marker of long-term mortality in patients presented with non-ST segment elevation myocardial infarction (NSTEMI). This is an observational study with a total 619 NSTEMI patients admitted to a tertiary center between 2004 and 2006. Patients were stratified into equal tertiles according to their admission PLR. The primary outcome, 4 year all-cause mortality, was compared among the PLR tertiles. The first, second and third PLR tertiles were PLR < 118.4, 118.4 ≤ PLR ≤ 176, and PLR > 176, respectively) included 206, 206 and 207 patients, respectively. There was a significant higher 4 year all-cause mortality in the higher PLR tertiles (the mortalities were 17, 23 and 42 % for the first, second and third PLR tertiles respectively, p < 0.0001). After exclusion of patients expired in the first 30 days, patients in the first PLR tertile had a significant lower 4 year mortality (33/205, 16 %) versus those in the third PLR tertile (72/192, 38 %), p < 0.0001. After controlling for Global Registry of Acute Coronary Events risk scores and other confounders, the hazard ratio of mortality increased 2 % per each 10 U increase of PLR (95 % CI 1.01–1.03, p < 0.0001). In patients with PLR ≥ 176, the mortality rate was statistically higher in those received mono-antiplatelet (30/60 = 50 %) compared to those received dual antiplatelet therapy (48/149 = 32 %), p = 0.0018. However in PLR < 176, the mortality was not significantly different between mono-antiplatelet group (20/94 = 21 %) versus dual antiplatelets group (53/213 = 25 %), p = 0.56. The PLR is a significant independent predictor of long-term mortality after NSTEMI. Among patients with PLR > 176, patients with dual antiplatelet therapy had lower mortality versus those with mono-platelet therapy. Further studies are needed to clarify these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous studies demonstrated the association between elevated peripheral blood platelet count and major adverse cardiovascular adverse outcomes [1–4]. Additionally, elevated platelet count was independently associated with an inadequate platelet response to aspirin [5]. On the contrary, a low peripheral blood lymphocyte count was associated with major adverse cardiovascular outcomes [6–10]. Interestingly, the platelet lymphocyte ratio (PLR) was found to be a significant inflammatory marker to predict mortality in cancer population [11–13]. The aim of our study was to investigate the usefulness of PLR in predicting the long-term mortality in coronary artery disease using our non-ST segment elevation myocardial infarction (NSTEMI) database.
Methods
Total of 619 patients from our NSTEMI/neutrophil lymphocyte ratio (NLR) database [14] was studied to investigate the predictive value of PLR on all-cause long-term mortality. The patients were discharged from the only tertiary angioplasty center in Staten Island, between September 2004 and December 2006. Inclusion and exclusion criteria for the study subjects are shown in Table 1. Our primary end-point, all-cause 4 year mortality, was assessed by reviewing the electronic medical record and the social security death index till February 2011.
Complete blood count was obtained from the initial (within 1 h of admission), second and last blood cells counts in the same index hospitalization and was determined by the Coulter counter technique (Coulter Gen.S Hematology Analyzer, Beckman Coulter Corp, Hialeah, Florida). Serum chemistries were determined by Beckman coulter (Synchron® system, Anaheim, California). The medical record for each patient was independently reviewed by two physicians for the baseline characteristics, clinical presentation and the modalities of management (Table. 2). The left ventricular ejection fraction was retrieved from the echocardiography reports. Positive smoking status included both current and prior smokers. The appropriate discharge and admission Global Registry of Acute Coronary Events (GRACE) scores [15] were calculated for each index case. The GRACE score on discharge was used because of its superiority and validity to predict up to 4 year mortality [16]. GRACE score on discharge was calculated from the following variables: age, systolic pressure, heart rate, history of congestive heart failure, serum creatinine, cardiac enzyme status, presence of ST segment deviation, past history of myocardial infarction, in-hospital coronary bypass surgery (CABG) or in-hospital percutaneous angioplasty (PCI). The study design protocol was approved by our institution review board.
Statistical considerations
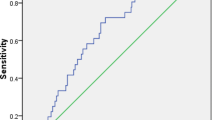
The primary aim of this study was to determine the usefulness of PLR in predicting mortality in NSTEMI population (n = 619 subjects). For ease of interpretation and for clinical relevance the admission PLR, calculated as platelet count/lymphocyte count, was divided into tertiles as follows: first tertile (206 patients) with PLR < 118, second tertile (206 patients) with PLR ≥ 118 or ≤ 176 and the third tertile (207 patients) with PLR > 176. The chi-square test or Fisher’s exact test was used to compare these three groups for categorical variables and analysis of variance (ANOVA) was used for continuous variables (Table 2). The analysis of mortality was accomplished by applying standard methods of survival analysis, i.e., computing the Kaplan–Meier product limit curves (Fig. 1), where the data was stratified by PLR tertiles. The three PLR groups were compared using the log-rank test. A univariate screen of all potential predictors of mortality using a separate Cox proportional hazards model for each variable was performed (Tables 3 and 4). The GRACE score was divided into low risk (≤108), moderate risk (108–141), and high risk (≥141). Those variables that were found to be statistically significant (p < 0.10) as well as clinically meaningful in the univariate analyses were included in the multivariate model. Backwards selection was used to remove variables which did not significantly contribute information to this model, given other factors included in the model. The purpose of the study was to determine the predictive ability of admission PLR in the presence of other multiple predictor variables. To meet this objective, admission PLR was forced into the final multivariate model in conjunction with the other set of significant predictor variables from the model selection procedure.
Admission PLR, along with 16 other candidate variables (i.e. categorical GRACE, history of congestive heart failure, admission hemoglobin, use of aspirin or clopidogrel, prior CABG, prior PCI, ejection fraction, diabetes mellitus, end-stage kidney disease, use of warfarin, history of cerebrovascular events, use of statin, serum glucose, history of hypertension, atrial fibrillation, and body mass index) were included in the selection process as they were potential risk factors associated with mortality. Admission platelet count and lymphocyte count were excluded from the selection process as they are used in the calculation of admission PLR. Age, admission creatinine, history of congestive heart failure, systolic blood pressure, pulse, in-hospital angioplasty, in-hospital CABG, ST deviation, and history of myocardial infarction were also excluded from the selection process as they are used in the calculation of the GRACE score. Our final model included k = 8 predictors (Table 3). In addition, to prove the superiority of PLR over other hemogram parameters, we built separate multivariate models for other hemogram parameters (total WBC count, neutrophil count, platelet count and lymphocyte count) by including that parameter and the same confounding variables (without PLR) in that model (Table 5). We ran additional sets of stratified analysis to evaluate the predictive value of PLR in patients with different ranges of lymphocyte and platelet count and age, in order to evaluate whether PLR is independent of lymphopenia, high platelet count and age in predicting mortality. In order to evaluate any association between the highest tertile of PLR (PLR > 176 vs. PLR ≤176) and type of antiplatelet therapy received (mono vs. dual antiplatelet therapy) in predicting mortality, we performed subgroup analysis of PLR in the two antiplatelet therapy subgroups. Two tailed Fisher’s exact tests were used to compare these subgroups. All analyses were performed using SAS version 9.2 (SAS Institute; Cary, NC). A result was considered statistically significant at the p < 0.05 level of significance.
Results
Baseline characteristics
Table 2 demonstrates the baseline characteristics of our NSTEMI patients sorted by their PLR tertiles. The patients in the highest PLR tertile (PLR > 176) were significantly older with higher prevalence of female gender and cerebrovascular events but lower frequency of smoking and lower body mass index compared to those in the lowest PLR tertile (PLR < 118.4). Additionally, patients in the highest PLR tertile had a worse presentation than those in the lowest PLR tertile (i.e. higher GRACE score and more prevalence of Killip class ≥ 3). According to the admission laboratory work-up, patients in the highest PLR tertile (PLR > 176) had significantly higher serum creatinine but lower mean platelet volume and hemoglobin level than those in the lowest PLR tertile. We also observed among the patients within the highest PLR tertile a lower rate of aspirin, clopidogrel, and in-hospital coronary angioplasty treatments in comparison to those in the lowest PLR tertile.
The primary outcome according the PLR tertiles
Of the 619 included patients, 155 died (27.1 %) over an average 55 months follow-up period. The 4 year all-cause mortality were 17, 23 and 42 % for the first,second and third PLR tertiles respectively, p < 0.0001. Likewise, the Kaplan–Meier curves of the all-cause mortality for the three PLR tertiles demonstrated significant higher mortality in the highest PLR tertile in comparison to the lower two PLR tertiles, log-rank test chi-square = 43.25, p < 0.0001 (Fig. 1). Interestingly, after exclusion of patients expiring in the first 30 days (n = 22), the patients in the first PLR tertile still had a significant lower 4 year mortality (33/205, 16 %) compared to those in the third PLR tertile (72/192, 38 %), p < 0.0001. Similarly, we repeated this analysis after excluding patients dying in the first 6 months post NSTEMI (n = 44), and the patients in the first PLR tertile continued to have a significantly lower mortality compared to those in the third tertile (15 vs. 33 %, p < 0.001). Table 3 shows all potential predictors of mortality with p < 0.1 in the univariate screen using separate Cox proportional hazards models.
Multivariate model
After controlling for 16 confounding variables (Table 4), PLR remained independent predictor of higher 4 year mortality. The hazard ratio of mortality increases by 1.02 per each ten unit increase of PLR (95 % CI 1.01–1.03, p < 0.0001). After transforming PLR from a continuous to a categorical variable defined by three tertiles, we repeated the multivariate analysis using the same confounding variables. It showed that the highest tertile of PLR remained a significant predictor of 4 year mortality, with a hazard ratio of 1.65 (1.08–2.51, p = 0.02) between third and first tertile and HR of 1.62 (1.15–2.26, p = 0.005) between the third tertile versus bottom two tertiles (Table 4). Thus, those in the highest tertile of PLR (PLR > 176) had a 62 % higher mortality compared to those in the lower two tertiles (PLR ≤176).
Table 5 shows multivariate models built using other hemogram parameters. In the univariate screen, absolute neutrophil count, absolute lymphocyte count, lymphopenia (absolute lymphocyte count < 1.5 k/ml) and high platelet count (defined as greater than 75th percentile i.e. > = 300,000/ml), but not total WBC count or admission platelet count, were significant predictors of mortality. In multivariate models, total WBC count, absolute neutrophil count on admission and absolute lymphocyte count were no longer significant predictors of mortality whereas admission platelet count, although not significant in the univariate screen, became significant. Lymphopenia and high platelet count remained significant predictors in the multivariate models. However, after forcing lymphopenia in Cox regression model of admission PLR and other co-variates, HR of lymphopenia became non-significant and HR of PLR remained significant at p = 0.014. Similarly, after forcing admission platelet count in the Cox regression model, HR of platelet count became non-significant and HR of PLR remained significant at p = 0.015. This shows that predictive value of PLR is independent of lymphocyte or platelet counts taken individually. In order to further assess the possible confounding effect of different ranges of lymphocyte and platelet count on PLR, we performed a stratified analysis.
Stratified subgroup analyses
Long-term mortality according PLR and lymphocyte count subgroups
Since low lymphocyte count was significantly associated with a higher mortality in the Cox proportional hazard model, we decided to perform a stratified analysis to evaluate the relationship between PLR and mortality in two lymphocyte subgroups: normal lymphocyte count i.e. ≥1.5 k/cc (n = 390) and lymphopenia i.e. lymphocyte count <1.5 k/cc (n = 220). We compared the highest tertile of PLR (PLR > 176) with the two lower tertiles (PLR ≤ 176). In the subgroup with lymphocyte count ≥1.5 k/cc, there was a significant higher 4 year mortality among the patients with PLR > 176 (16/49 = 33 %) compared to those with PLR ≤ 176 (55/341 = 16 %), p = 0.009. In the subgroup of lymphocyte count <1.5 k/cc, the patients with PLR > 176 still had a higher 4 year mortality rate than patients with PLR ≤ 176 (45 vs. 30 %, p = 0.03) (Fig. 2). This shows that the effect of PLR on mortality is independent of the lymphocyte count and it persists in the subgroup of patients with lymphopenia on admission.
Long-term mortality according PLR and platelet count subgroups
Since high platelet count (greater than 75th percentile or > = 300,000/ml) was associated with a higher mortality in the Cox regression model, we decided to perform a stratified analysis to evaluate the relationship between PLR and mortality in two platelet count subgroups. In the subgroup with platelet count <300,000/ml (n = 476), patients with PLR > 176 had significantly higher mortality compared to patients with PLR ≤ 176 (43 % vs. 18 %, chi-square p < 0.001). This effect persisted in the subgroup of platelet count >300,000/ml (n = 146), with mortality 41 % in highest PLR tertile versus 21 % in the lower two tertiles (p = 0.017) (Fig. 3).
Long-term mortality according PLR and age subgroups
Since higher PLR was associate with a greater age, we decided to perform a stratified analysis to evaluate the effect of PLR in two age sub-groups of age ≤65 years (n = 318) and age >65 years (n = 301).In the younger subgroup (patients ≤65 years), those with PLR > 176 had a significant higher mortality in comparison to the patients with PLR ≤176 (19/79 = 24 % vs. 16/239 = 7 %, respectively, p < 0.0001), an effect which persisted in the older subgroup of patients >65 years (mortality 53 vs. 35 % p = 0.001, Fig. 4).
Long-term mortality according PLR and anti-platelets subgroups
In the group with PLR > 176, the mortality rate was statistically higher in those received mono- antiplatelet (30/60 = 50 %) compared to those received dual antiplatelet therapy (48/149 = 32 %), p = 0.00184. However among the patients with PLR ≤ 176, the mortality was not statistically significant between patients received mono-antiplatelet therapy (20/94 = 21 %) versus those received dual antiplatelets (53/213 = 25 %), p = 0.5618.
Discussion
The main finding
Our study’s main finding was that higher PLR is an independent significant predictor of long-term mortality after NSTEMI, even after adjusting for the possible confounding predictors. This association between PLR and survival status was not solely explained by lymphopenia as the same finding was noticed among patients with normal lymphocyte count (i.e. ≥1.5 k/cc). Interestingly, after exclusion of the patients that died in the first 30 days as well as first 6 months post-NSTEMI, PLR > 176 remained a significant predictor of 4 year all-cause mortality. These findings highlight that elevated PLR is a predictor of long-term mortality rather than just a marker of an acute medical condition. Although there was a significant higher frequency of some of the cardiovascular risk factors among patients with high PLR, this did not affect the significant association between PLR and mortality in the multivariate analysis.
Superiority of PLR to separate platelet or lymphocyte counts
While some studies demonstrated the association between higher platelet count and adverse outcomes [1–4], Muller et al. in their large observational study failed to demonstrate an association between platelet count and mortality in patients with acute coronary syndrome [17]. High platelet counts may represent higher degree of antiplatelet drug resistance and higher propensity to form platelet rich thrombi on atherosclerotic plaques, leading to worse outcomes. Moreover, higher platelet counts may reflect underlying inflammation as several inflammatory mediators stimulate megakaryocytic proliferation and produce relative thrombocytosis. Moreover, studies have shown patients with CAD to have increased levels platelet monocyte aggregates (PMA) in their bloodstream, which correlate with plaque stability [18, 19]. Elevated levels of PMA in NSTEMI patients has been shown to be associated with worse in-hospital outcomes and increased risk of future cardiac events [20]. Previously studies have shown that a low lymphocyte count has been associated with an adverse mortality/CV outcome in patients with chest pain, stable CAD [9], unstable angina [8] as well as CHF [10]. The underlying mechanism behind this is speculative. It has been proposed that in response to physiologic stress during myocardial ischemia/infarction, there is release of cortisol. High cortisol leads to lymphopenia [21]. High level of physiologic stress means high level of cortisol which can be translated as a lower lymphocyte count. On the contrary, higher lymphocyte count represents a more appropriate immune response and a stable, quiescent inflammatory pathway [8]. Hence a low lymphocyte count is associated with worse outcomes in NSTEMI patients. In our study, we did have a significant association between lower lymphocyte count and higher platelet count with higher mortality; however we showed that the effect of PLR on mortality was independent of platelet or lymphocyte counts alone. We speculate two factors that explain the superiority of PLR to either individual lymphocyte or platelet counts. First, the stability of PLR compared to the absolute platelet or lymphocyte counts, which could be altered by many physiological and pathological conditions. Secondly and most importantly, the PLR represent two inversely related predictors and immune pathways. We hypothesize that higher platelet count is a marker of ongoing destructive inflammatory response and prothrombotic status. A positive correlation was found between the acute phase reactants and proinflammatory proteins (C reactive protein, tumor necrosis factor alpha, interleukin-1, and IL-6) and the elevated platelet count in nonspecific inflammatory conditions [22, 23]. Moreover, Lordkipanidzé et al. [5] demonstrated that elevated platelet count is an independent predictor of aspirin resistance. Similarly, Narvaez et al. [24] found a significant higher platelet count in patients with aspirin resistance versus those without. On the other hand, lymphocytes represent a quiescent and controlling inflammatory pathway. In cancer patients, lymphocyte was responsible on the programmed cell death, apoptosis [25]. We suggest that the lymphocyte-mediated apoptosis is less destructive to the adjacent myocardial cells compared to the uncontrolled ischemic and inflammatory cell death models.
Relation between PLR and antiplatelet therapy
Interestingly, we observed a significant higher mortality in patients with PLR > 176 who received mono-antiplatelet therapy in comparison to those who received dual antiplatelet therapy, whereas mono-versus dual antiplatelet therapy showed no difference in mortality among those with PLR ≤ 176. This finding could be explained by the association between high platelet count and resistance to antiplatelet therapy [5, 24]; thereby suggesting that dual antiplatelet therapy may be associated with better outcomes compared to monotherapy, in the subgroup of NSTEMI patients in the highest PLR tertile. While many laboratory tools are emerging to measure the platelet responsiveness to various antiplatelet therapies, we advocate that simple tools in hemogram (i.e. complete blood count) will be cheaper and more available tools for the daily practice. We suggest the need for further evaluation of PLR and our previous reported mean platelet volume/platelet ratio [26] as predictors of responsiveness to antiplatelet therapies in prospective and laboratory studies.
Limitations
This present study inherited the same limitations of our NSTEMI/NLR database (i.e. an observational study, missing other adverse outcomes than all-cause mortality), lacking other data that could be relevant to the PLR (e.g. platelet aggregation, inflammatory markers), the relatively small number of high prevalent disease and single center study. Moreover, using tertiles for PLR make the absolute number of PLR associated with adverse outcomes (PLR > 176) difficult to reproduce in other populations which may have a different range of PLR. Despite these limitations, we present the first study that focused on the predictive value of PLR in NSTEMI patients.
Conclusion
The highest tertile of PLR (PLR > 176) is a significant independent predictor of long-term (4 year) mortality after NSTEMI. PLR > 176 remained significantly associated with long-term mortality in NSTEMI patients after exclusion of those who died within the first 30 days and those who died in the first 6 months after the NSTEMI. In subjects with PLR > 176, there was a significantly lower long-term mortality among NSTEMI patients treated with dualantiplatelet therapy compared to those with monotherapy. Further studies are needed to validate these findings. A larger, prospective, multi-center, study is needed to explain the mechanisms for this association of the PLR with survival at the molecular level.
References
Thaulow E, Erikssen J, Sandvik L, Stormorken H, Cohn PF (1991) Blood platelet count and function are related to total and cardiovascular death in apparently healthy men. Circulation 84(2):613–617
Iijima R, Ndrepepa G, Mehilli J, Bruskina O, Schulz S, Schomig A et al (2007) Relationship between platelet count and 30 day clinical outcomes after percutaneous coronary interventions. Pooled analysis of four ISAR trials. Thromb Haemost 98(4):852–857
Nikolsky E, Grines CL, Cox DA, Garcia E, Tcheng JE, Sadeghi M et al (2007) Impact of baseline platelet count in patients undergoing primary percutaneous coronary intervention in acute myocardial infarction (from the CADILLAC trial). Am J Cardiol 99(8):1055–1061. doi:10.1016/j.amjcard.2006.11.066
Vidwan P, Lee S, Rossi JS, Stouffer GA (2010) Relation of platelet count to bleeding and vascular complications in patients undergoing coronary angiography. Am J Cardiol 105(9):1219–1222. doi:10.1016/j.amjcard.2009.12.035
Lordkipanidze M, Diodati JG, Turgeon J, Schampaert E, Palisaitis DA, Pharand C (2010) Platelet count, not oxidative stress, may contribute to inadequate platelet inhibition by aspirin. Int J Cardiol 143(1):43–50. doi:10.1016/j.ijcard.2009.01.037
Ommen SR, Hammill SC, Gibbons RJ (2002) The relative lymphocyte count predicts death in patients receiving implantable cardioverter defibrillators. Pacing Clin Electrophysiol 25(10):1424–1428
Acanfora D, Gheorghiade M, Trojano L, Furgi G, Pasini E, Picone C et al (2001) Relative lymphocyte count: a prognostic indicator of mortality in elderly patients with congestive heart failure. Am Heart J 142(1):167–173
Zouridakis EG, Garcia-Moll X, Kaski JC (2000) Usefulness of the blood lymphocyte count in predicting recurrent instability and death in patients with unstable angina pectoris. Am J Cardiol 86(4):449–451
Ommen SR, Gibbons RJ, Hodge DO, Thomson SP (1997) Usefulness of the lymphocyte concentration as a prognostic marker in coronary artery disease. Am J Cardiol 79(6):812–814
Ommen SR, Hodge DO, Rodeheffer RJ, McGregor CG, Thomson SP, Gibbons RJ (1998) Predictive power of the relative lymphocyte concentration in patients with advanced heart failure. Circulation 97(1):19–22
Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O’Reilly DS et al (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 47(17):2633–2641. doi:10.1016/j.ejca.2011.03.028
Smith RA, Bosonnet L, Raraty M, Sutton R, Neoptolemos JP, Campbell F et al (2009) Preoperative platelet–lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg 197(4):466–472. doi:10.1016/j.amjsurg.2007.12.057
Smith RA, Ghaneh P, Sutton R, Raraty M, Campbell F, Neoptolemos JP (2008) Prognosis of resected ampullary adenocarcinoma by preoperative serum CA19-9 levels and platelet–lymphocyte ratio. J Gastrointest Surg 12(8):1422–1428. doi:10.1007/s11605-008-0554-3
Azab B, Zaher M, Weiserbs KF, Torbey E, Lacossiere K, Gaddam S et al (2010) Usefulness of neutrophil to lymphocyte ratio in predicting short- and long-term mortality after non-ST-elevation myocardial infarction. Am J Cardiol 106(4):470–476. doi:10.1016/j.amjcard.2010.03.062
Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP et al (2003) Predictors of hospital mortality in the Global Registry of Acute Coronary Events. Arch Intern Med 163(19):2345–2353. doi:10.1001/archinte.163.19.2345
Tang EW, Wong CK, Herbison P (2007) Global Registry of Acute Coronary Events (GRACE) hospital discharge risk score accurately predicts long-term mortality post acute coronary syndrome. Am Heart J 153(1):29–35. doi:10.1016/j.ahj.2006.10.004
Mueller C, Neumann FJ, Hochholzer W, Trenk D, Zeller T, Perruchoud AP et al. The impact of platelet count on mortality in unstable angina/non-ST-segment elevation myocardial infarction. Am Heart J. 2006;151(6):1214 e1–7. doi:10.1016/j.ahj.2006.03.011
Furman MI, Benoit SE, Barnard MR, Valeri CR, Borbone ML, Becker RC et al (1998) Increased platelet reactivity and circulating monocyte–platelet aggregates in patients with stable coronary artery disease. J Am Coll Cardiol 31(2):352–358
Linden MD, Furman MI, Frelinger AL III, Fox ML, Barnard MR, Li Y et al (2007) Indices of platelet activation and the stability of coronary artery disease. J Thromb Haemostasis 5(4):761–765. doi:10.1111/j.1538-7836.2007.02462.x
Zhang SZ, Jin YP, Qin GM, Wang JH (2007) Association of platelet–monocyte aggregates with platelet activation, systemic inflammation, and myocardial injury in patients with non-st elevation acute coronary syndromes. Clin Cardiol 30(1):26–31. doi:10.1002/clc.2
Thomson SP, McMahon LJ, Nugent CA (1980) Endogenous cortisol: a regulator of the number of lymphocytes in peripheral blood. Clin Immunol Immunopathol 17(4):506–514
Alexandrakis MG, Passam FH, Moschandrea IA, Christophoridou AV, Pappa CA, Coulocheri SA et al (2003) Levels of serum cytokines and acute phase proteins in patients with essential and cancer-related thrombocytosis. Am J Clin Oncol 26(2):135–140. doi:10.1097/01.COC.0000017093.79897.DE
Alexandrakis MG, Passam FH, Perisinakis K, Ganotakis E, Margantinis G, Kyriakou DS et al (2002) Serum proinflammatory cytokines and its relationship to clinical parameters in lung cancer patients with reactive thrombocytosis. Respir Med 96(8):553–558
Narvaez I, Sagastagoitia JD, Vacas M, Saez Y, Lafita M, Monica S et al (2007) Prevalence and biologic profile of aspirin resistance in patients with angiographically proven coronary artery disease. Thromb Res 120(5):671–677. doi:10.1016/j.thromres.2006.12.020
Niederhuber JE (1997) Cancer vaccines: the molecular basis for T cell killing of tumor cells. Oncologist 2(5):280–283
Azab B, Torbey E, Singh J, Akerman M, Khoueiry G, McGinn JT et al (2011) Mean platelet volume/platelet count ratio as a predictor of long-term mortality after non-ST-elevation myocardial infarction. Platelets 22(8):557–566. doi:10.3109/09537104.2011.584086
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Azab, B., Shah, N., Akerman, M. et al. Value of platelet/lymphocyte ratio as a predictor of all-cause mortality after non-ST-elevation myocardial infarction. J Thromb Thrombolysis 34, 326–334 (2012). https://doi.org/10.1007/s11239-012-0718-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-012-0718-6