Abstract
The prognostic role of neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) in patients with stable coronary artery disease (CAD) is still unclear. We enrolled 500 patients undergoing elective percutaneous coronary intervention (PCI). Blood samples were drawn prior to PCI for NLR and PLR calculation. Major adverse clinical events (MACE), which included death, myocardial infarction (MI), and target vessel revascularization (TVR), were recorded up to 5 years. Patients in the higher tertile of NLR presented higher Kaplan–Meier estimates of MACE (26.0% vs. 16.9% in tertile 2 vs. 14.3% in tertile 1; p = 0.042) and death (12.0% vs 6.9% in tertile 2 vs. 4.6% in tertile 1; p = 0.040), whereas there were no significant differences in the estimates of MI and TVR. NLR in the higher tertile was an independent predictor of MACE (HR 1.65, 95% CI 1.07–2.55, p = 0.024). No significant difference was observed across tertiles of PLR. Unlike PLR, elevated pre-procedural NLR is associated with an increased risk of 5-year clinical adverse events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory cells and platelets play a pivotal role in the pathogenesis and evolution of atherosclerosis and cardiovascular diseases [1,2,3,4]. While increased neutrophil count is associated with a higher risk of cardiovascular events, low lymphocyte count may reflect general stress and immunodeficiency and has been associated with cardiovascular complications and increased mortality rates [5, 6]. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR), two easily available parameters inferable from blood cell count, have emerged as potential inflammatory markers able to predict both cardiac and non-cardiac events [7, 8]. Previous studies have shown that elevated pre-procedural NLR and PLR in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI) were associated with an increased risk of adverse cardiac events at follow-up [8, 9]. However, the prognostic role of NLR and PLR in patients with stable coronary artery disease (CAD) treated with elective PCI is still unclear. The aim of this study was to determine whether pre-procedural values of NLR and PLR are able to predict long-term clinical outcomes of patients with stable CAD undergoing elective PCI.
Methods
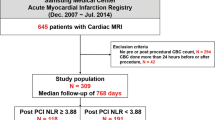
In this prospective observational study, we enrolled a total of 500 patients with clinically stable CAD undergoing elective PCI at our institution from February 2013 to November 2014. We excluded patients with no available complete blood cell count and patients with systemic inflammatory disease or on drug therapy potentially affecting inflammatory cell count. We also excluded patients with severe left ventricular dysfunction (ejection fraction < 30%), chronic total coronary occlusions, lesions with extensive calcifications requiring rotational atherectomy, bypass surgery in the previous 3 months, severe pulmonary disease, and neoplasm. The ethical committee of Campus Bio-Medico University of Rome approved the study and all patients signed written informed consent for participation and data collection. Blood samples comprising complete blood cell count, cardiac biomarkers, and renal function panel were obtained in all patients from venous blood drawn at admission and 6 and 24 h after the procedure. NLR was calculated as the ratio of the absolute number of neutrophils to the absolute number of lymphocytes, whereas PLR was calculated as the ratio of the absolute platelet count to the absolute lymphocyte count. All patients were on chronic aspirin treatment and received either 600-mg clopidogrel loading dose (at least 6 h before intervention) or were on therapy with clopidogrel 75 mg/day for at least 5 days. Procedural anti-coagulation was achieved by administration of unfractionated heparin (100 U/kg) in all patients. Procedural success was defined as a reduction in percent diameter stenosis to below 30% and the presence of Thrombolysis In Myocardial Infarction (TIMI) flow grade 3 in the main vessel and all side branches > 2 mm in diameter. The primary end point of the study was the occurrence of major adverse cardiac events (MACE), which included all-cause death, non-fatal myocardial infarction (MI), or target vessel revascularization (TVR). Clinical follow-up data were obtained up to 5 years by means of office visit, telephone interview, and chart review. All events were classified and adjudicated by a physician not involved in the follow-up process. Non-fatal MI was defined according to the European Society of Cardiology (ESC), American College of Cardiology (ACC), American Heart Association (AHA), and World Heart Federation definitions [10]. TVR was defined as any clinically driven repeat PCI or surgical bypass of any segment within the entire epicardial coronary artery containing the target lesion based on the Academic Research Consortium definition [11]. Cardiac death was also monitored and defined as death resulting from an acute myocardial infarction (MI), sudden cardiac death, and death due to heart failure [12]. All single components of the primary end point, as well as cardiac death, were also analyzed separately.
Categorical variables are reported as frequencies and percentages. Continuous variables are reported as mean ± SD or as median (lower and upper quartiles). Comparisons between categorical variables were evaluated using the Fisher’s exact test or the Pearson’s chi-square test, as appropriate. Comparisons between continuous variables were performed using the Student’s t test or Mann–Whitney U test, as appropriate. The primary event analyses were done with time-to-event data (for which patients were censored at 5-year follow-up or at last contact in case they were lost to follow-up), determined with Kaplan–Meier method, and compared by use of the log-rank test. Cox proportional hazard analysis was used to estimate the association between NLR and PLR tertiles and long-term clinical outcomes, also after adjusting for age, hypertension, diabetes mellitus, chronic renal failure, left ventricle ejection < 40%. Statistical analysis was performed using Stata/IC, version 12.0 (STATA Corp., College Station, TX), and p values < 0.05 (two-tailed) were considered significant.
Results
Clinical follow-up information at 5 years was available in 471 patients (94.2%). Patients were stratified into tertiles according to pre-procedural NLR (lower tertile < 2.95, mid tertile 2.95–3.68, higher tertile > 3.68) and PLR (lower tertile < 86.36, mid tertile 86.36–121.67, higher tertile > 121.67). Clinical and procedural characteristics of the overall population and according to NLR and PLR tertiles are reported in Tables 1 and 2, respectively. All patients underwent successful and uncomplicated PCI. Patients in the higher NLR tertile more frequently displayed chronic kidney disease, while there were no other significant differences with regard to any other characteristics. Patients in the lower PLR tertile were younger and presented a higher prevalence of male sex and smoking habit compared with the higher tertile. Kaplan–Meier curves for all cause death and cardiac death for NLR and PLR tertiles are reported in Figs. 1 and 2, respectively, while Cox proportional hazard analyses for NLR tertiles are reported in Table 3. Patients in the higher tertile of NLR presented significantly higher Kaplan–Meier estimates of MACE (26.0% vs. 16.9% in the mid tertile vs. 14.3% in the lower tertile; log-rank p = 0.042) and death (12.0% vs 6.9% in the mid tertile vs. 4.6% in lower tertile; log-rank p = 0.040), whereas there were no significant differences in the estimates of MI (log-rank p = 0.886) and TVR (log-rank p = 0.616). At Cox proportional hazard analysis, NLR in the higher tertile (vs tertiles 1 and 2 grouped together) was an independent predictor of MACE (hazard ratio 1.65, 95% confidence interval 1.07–2.55, p = 0.024) after adjusting for age, hypertension, diabetes mellitus, chronic renal failure, and left ventricle ejection < 40%. No significant differences were observed between tertiles of pre-procedural PLR for any of the study end points. Furthermore, no impact of post-procedural NLR and PLR on clinical outcomes was observed.
Discussion
The main finding of our study is that in patients with stable CAD undergoing elective PCI, pre-procedural NLR in the higher tertile independently predicts the occurrence of MACE at long-term follow-up, whereas pre-procedural PLR does not significantly impact on clinical outcomes. The role of inflammation in the pathogenesis of CAD has been well established, and the predictive ability of inflammatory cell count as an independent risk factor for coronary heart disease has been investigated extensively for varying cardiovascular outcomes [5]. In particular, neutrophil activation and proliferation in response to an acute injury may slow down and mitigate further damage [13], whereas lymphocyte reactivity is downgraded during active inflammation as regulatory pathways lead to lymphocyte apoptosis [14]. NLR, a simple index which integrates information from both cells types, seems to have a prognostic role in patients with atherosclerotic disease. In patients with ACS, where a generally enhanced inflammatory status is expected, high NLR has been shown to predict worse clinical outcomes both at short- and long-term post-PCI [15, 16]. Nevertheless, various conditions leading to heighted pre-procedural inflammatory status might occur even in patients with stable CAD, warranting an accurate evaluation of inflammatory markers prior to coronary revascularization. However, few studies have evaluated the potential prognostic role of NLR in patients with stable CAD undergoing PCI. Recently, Wada et al. [17] identified elevated pre-procedural NLR as in independent predictor of all cause and cardiac mortality in patients undergoing elective PCI. Our findings confirm this evidence showing that high pre-procedural NLR may predict long-term MACE, which were mainly driven by the occurrence of all-cause death, and further extends this evidence with regard to the fact that PLR seems to have no significant impact on clinical outcomes following PCI. Increased platelet reactivity can promote endothelial dysfunction, atherosclerosis development, and thrombotic complications during and following PCI [18,19,20,21]. Furthermore, platelet count, although not directly related to platelet reactivity, increases in response to systemic inflammation as well [22]. Similar to NLR, elevated PLR has been associated with an increased risk of cardiovascular events and long-term mortality in patients at high risk of CAD or presenting with an ACS [8, 9, 23, 24]. Cho et al. found that high pre-intervention values of both PLR and NLR, especially when combined, are independent predictors of long-term adverse clinical outcomes such as all-cause mortality, cardiac death, and MI in patients with unstable angina and non-ST-elevation MI treated with PCI [8]. However, such findings were not confirmed in a small subgroup (n = 80) of patients with stable CAD. Unlike with NLR, in our study, no significant difference was observed among tertiles of PLR for any of the study end points and high pre-procedural PLR was not predictive of future adverse events. This could be explained with the fact that the pathophysiological role of platelets is less pronounced in stable patients compared with those presenting with an ACS [24, 25]. Moreover, all our patients were on chronic aspirin therapy on admission and this might have influenced the results of the study. Chronic treatment with aspirin may lead to an increase in platelet count [26] and should therefore be taken into account when evaluating the prognostic role of PLR.
This study has several limitations that need to be considered. First, this was a single-center observational study with a relatively small sample size and therefore subject to selection bias. Second, we did not account for lipid panel, hepatic function, coagulation parameters, and other traditional markers of inflammation which could influence white blood cell and platelets count. Although blood samples were collected at three time points, and post-PCI values of NLR and PLR were not predictive of clinical outcomes, it cannot be excluded that further measurements might be helpful in predicting future adverse events. Finally, the prevalence of chronic renal failure was significantly higher in tertile 3, consistently with previous evidence that higher NLR levels are strongly correlated with worse renal function, suggesting that renal impairment could be a consequence of higher inflammatory environment [27,28,29]. However, in our study, the higher NLR values remained independently associated with worse clinical outcomes even after adjustment for the presence of chronic renal failure.
In conclusion, unlike PLR, high pre-intervention NLR values are associated with an increased risk of 5-year adverse clinical events in patients with stable CAD undergoing PCI. NLR may represent a simple and useful tool for risk stratification and a potential therapeutic target for patients undergoing elective percutaneous revascularization.
References
Ross, R. (1999). Atherosclerosis—an inflammatory disease. The New England Journal of Medicine, 340(2), 115–126.
Ridker, P. M., Everett, B. M., Thuren, T., MacFadyen, J. G., Chang, W. H., Ballantyne, C., Fonseca, F., Nicolau, J., Koenig, W., Anker, S. D., Kastelein, J. J. P., Cornel, J. H., Pais, P., Pella, D., Genest, J., Cifkova, R., Lorenzatti, A., Forster, T., Kobalava, Z., Vida-Simiti, L., Flather, M., Shimokawa, H., Ogawa, H., Dellborg, M., Rossi, P. R. F., Troquay, R. P. T., Libby, P., Glynn, R. J., & CANTOS Trial Group. (2017). Antiinflammatory therapy with canakinumab for atherosclerotic disease. The New England Journal of Medicine, 377(12), 1119–1131.
Davì, G., & Patrono, C. (2007). Platelet activation and atherothrombosis. The New England Journal of Medicine, 357(24), 2482–2494.
Mangiacapra, F., & Barbato, E. (2013). Clinical implications of platelet-vessel interaction. Journal of Cardiovascular Translational Research, 6(3), 310–315.
Sabatine, M. S., Morrow, D. A., Cannon, C. P., Murphy, S. A., Demopoulos, L. A., et al. (2002). Relationship between baseline white blood cell count and degree of coronary artery disease and mortality in patients with acute coronary syndromes: a TACTICS-TIMI 18 (Treat Angina with Aggrastat and determine Cost of Therapy with an Invasive or Conservative Strategy—Thrombolysis in Myocardial Infarction 18 trial) substudy. Journal of the American College of Cardiology, 40, 1761–1768.
Onsrud, M., & Thorsby, E. (1981). Influence of in vivo hydrocortisone on some human blood lymphocyte subpopulations. I. Effect on natural killer cell activity. Scandinavian Journal of Immunology, 13, 573–579.
Bressi, E., Mangiacapra, F., Ricottini, E., Cavallari, I., Colaiori, I., Di Gioia, G., Creta, A., & Di Sciascio, G. (2016). Relation of neutrophil to lymphocyte ratio with periprocedural myocardial damage in patients undergoing elective percutaneous coronary intervention. The American Journal of Cardiology, 118(7), 980–984.
Cho, K. I., Ann, S. H., Singh, G. B., Her, A. Y., & Shin, E. S. (2015). Combined usefulness of the platelet-to-lymphocyte ratio and the neutrophil-to-lymphocyte ratio in predicting the long-term adverse events in patients who have undergone percutaneous coronary intervention with a drug-eluting stent. PLoS One, 10(7), e0133934.
Park, J. J., Jang, H. J., Oh, I. Y., Yoon, C. H., Suh, J. W., et al. (2013). Prognostic value of neutrophil to lymphocyte ratio in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. The American Journal of Cardiology, 111, 636–642.
White, H., Thygesen, K., Alpert, J. S., & Jaffe, A. (2014). Universal MI definition update for cardiovascular disease. Current Cardiology Reports, 16(6), 492.
Cutlip, D. E., Windecker, S., Mehran, R., Boam, A., Cohen, D. J., van Es, G. A., et al. (2007). Clinical end points in coronary stent trials: a case for standardized definitions. Circulation, 115, 2344–2351.
Hicks, K. A., Tcheng, J. E., Bozkurt, B., Chaitman, B. R., Cutlip, D. E., Farb, A., Fonarow, G. C., Jacobs, J. P., Jaff, M. R., Lichtman, J. H., Limacher, M. C., Mahaffey, K. W., Mehran, R., Nissen, S. E., Smith, E. E., & Targum, S. L. (2015). 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). Journal of the American College of Cardiology, 66(4), 403–469.
Van Tassell, B. W., Toldo, S., Mezzaroma, E., & Abbate, A. (2013). Targeting interleukin-1 in heart disease. Circulation, 128(17), 1910–1923.
Hotchkiss, R. S., & Karl, I. E. (2003). The pathophysiology and treatment of sepsis. The New England Journal of Medicine, 348, 138–150.
Kaya, M. G., Akpek, M., Lam, Y. Y., Yarlioglues, M., Celik, T., et al. (2013). Prognostic value of neutrophil/lymphocyte ratio in patients with ST-elevated myocardial infarction undergoing primary coronary intervention: a prospective, multicenter study. International Journal of Cardiology, 168, 1154–1159.
Wang, X., Zhang, G., Jiang, X., Zhu, H., Lu, Z., & Xu, L. (2014). Neutrophil to lymphocyte ratio in relation to risk of all-cause mortality and cardiovascular events among patients undergoing angiography or cardiac revascularization: a meta-analysis of observational studies. Atherosclerosis, 234, 206–213.
Wada, H., Dohi, T., Miyauchi, K., Shitara, J., Endo, H., Doi, S., Konishi, H., Naito, R., Tsuboi, S., Ogita, M., Kasai, T., Hassan, A., Okazaki, S., Isoda, K., Suwa, S., & Daida, H. (2017). Pre-procedural neutrophil-to-lymphocyte ratio and long-term cardiac outcomes after percutaneous coronary intervention for stable coronary artery disease. Atherosclerosis, 265, 35–40.
Muller, O., Hamilos, M., Bartunek, J., Ulrichts, H., Mangiacapra, F., Holz, J. B., Ntalianis, A., Trana, C., Dierickx, K., Vercruysse, K., De Bruyne, B., Wijns, W., & Barbato, E. (2010). Relation of endothelial function to residual platelet reactivity after clopidogrel in patients with stable angina pectoris undergoing percutaneous coronary intervention. The American Journal of Cardiology, 105(3), 333–338.
Mangiacapra, F., Bartunek, J., Bijnens, N., Peace, A. J., Dierickx, K., Bailleul, E., Di Serafino, L., Pyxaras, S. A., Fraeyman, A., Meeus, P., Rutten, M., De Bruyne, B., Wijns, W., van de Vosse, F., & Barbato, E. (2012). Periprocedural variations of platelet reactivity during elective percutaneous coronary intervention. Journal of Thrombosis and Haemostasis, 10(12), 2452–2461.
Mangiacapra, F., Colaiori, I., Ricottini, E., Creta, A., Di Gioia, G., Cavallari, I., Bressi, E., Capuano, M., Barbato, E., & Di Sciascio, G. (2018). Impact of platelet reactivity on 5-year clinical outcomes following percutaneous coronary intervention: a landmark analysis. Journal of Thrombosis and Thrombolysis, 45(4), 496–503.
Leader, A., Pereg, D., & Lishner, M. (2012). Are platelet volume indices of clinical use? A multidisciplinary review. Annals of Medicine, 44(8), 805–816.
Ricottini, E., Mangiacapra, F., Nusca, A., Melfi, R., Cavallari, I., Miglionico, M., Gallo, P., Pozzilli, P., & Di Sciascio, G. (2018). Relation of platelet indexes to platelet reactivity and periprocedural myocardial infarction in patients who underwent percutaneous coronary angioplasty. The American Journal of Cardiology, 121(9), 1027–1031.
Lee, Y. S. G., Baradi, A., Peverelle, M., Sultani, R., Adams, H., Garlick, J., & Wilson, A. M. (2018). Usefulness of platelet-to-lymphocyte ratio to predict long-term all-cause mortality in patients at high risk of coronary artery disease who underwent coronary angiography. The American Journal of Cardiology, 121(9), 1021–1026.
Li, H., Zhou, Y., Ma, Y., Han, S., & Zhou, L. (2017). The prognostic value of the platelet-to lymphocyte ratio in acute coronary syndrome: a systematic review and meta-analysis. Kardiologia Polska, 75(7), 666–673.
Olędzki, S., Kornacewicz-Jach, Z., Safranow, K., Kiedrowicz, R., Gawrońska-Szklarz, B., Jastrzębska, M., & Gorący, J. (2017). Variability of platelet response to clopidogrel is not related to adverse cardiovascular events in patients with stable coronary artery disease undergoing percutaneous coronary intervention. European Journal of Clinical Pharmacology, 73(9), 1085–1094.
Erhart, S., Beer, J. H., & Reinhart, W. H. (1999). Influence of aspirin on platelet count and volume in humans. Acta Haematologica, 101(3), 140–144.
Tonyali, S., Ceylan, C., Yahsi, S., & Karakan, M. S. (2018). Does neutrophil to lymphocyte ratio demonstrate deterioration in renal function? Renal Failure, 40(1), 209–212.
Neuen, B. L., Leather, N., Greenwood, A. M., Gunnarsson, R., Cho, Y., & Mantha, M. L. (2016). Neutrophil-lymphocyte ratio predicts cardiovascular and all-cause mortality in hemodialysis patients. Renal Failure, 38(1), 70–76.
Seropian, I. M., Romeo, F. J., Pizarro, R., Vulcano, N. O., Posatini, R. A., Marenchino, R. G., Berrocal, D. H., & Belziti, C. A. (2018). Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio as predictors of survival after heart transplantation. ESC Heart Fail., 5(1), 149–156.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Associate Editor Craig Stolen oversaw the review of this article
Key Messages
The results of our study suggest that neutrophil-to-lymphocyte ratio (NLR), a simple and easily available inflammatory marker, may be used for risk stratification of patients undergoing elective percutaneous coronary revascularization, in that elevated pre-procedural values of NLR may help identify those patients at higher risk of future clinical adverse events. These patients may potentially benefit from tailored therapeutic strategies, such as more aggressive anti-inflammatory and anti-thrombotic treatment. This hypothesis warrants further investigation.
Rights and permissions
About this article
Cite this article
Bressi, E., Mangiacapra, F., Ricottini, E. et al. Impact of Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio on 5-Year Clinical Outcomes of Patients with Stable Coronary Artery Disease Undergoing Elective Percutaneous Coronary Intervention. J. of Cardiovasc. Trans. Res. 11, 517–523 (2018). https://doi.org/10.1007/s12265-018-9829-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-018-9829-6