Abstract
Clopidogrel reduces long-term ischemic events in patients with acute coronary syndrome or stable angina (SA) undergoing percutaneous coronary intervention (PCI). Endothelial function improvement has been proposed, among other factors, for this beneficial effect of clopidogrel, but whether this might be associated to its anti-platelet action remains unclear. We tested the hypothesis that clopidogrel improvement of peripheral vascular endothelial function might be associated with inhibition of platelet aggregation. Endothelial function was evaluated before and at least 12 h after 600 mg clopidogrel in 43 SA pts undergoing elective PCI by: (a) reactive hyperemia peripheral arterial tonometry (measuring the Endoscore); (b) circulating endothelial microparticles (EMPs). Response to clopidogrel was measured with point-of-care VerifyNow P2Y12 assay and expressed as platelet reaction unit (PRU) and percent platelet inhibition (%PI). High platelet reactivity after clopidogrel was defined as PRU ≥ 240. Endothelial function improved after clopidogrel in 20 pts. Changes in Endoscore (Δ Endoscore) were significantly correlated with both PRU (r = −0.61, P < 0.001) and %PI (r = 0.57, P < 0.001). Endoscore significantly increased after clopidogrel in pts with PRU < 240 (0.38 ± 0.26 to 0.57 ± 0.33, P < 0.001), but did not in pts with PRU ≥ 240 (0.53 ± 0.31 to 0.40 ± 0.37, P = 0.12). EMPs were also significantly reduced in pts with PRU < 240 (222 [140–593] to 142 [83–371]/μl, P = 0.001), while no changes were observed in pts with PRU ≥ 240 (256 [178–531] to 388 [238–499]/μl, P = 0.55). In patients with stable coronary artery disease, a single 600 mg clopidogrel loading dose improves vascular endothelial function. This improvement is associated with optimal platelet inhibition and it is not observed in patients with post-clopidogrel high platelet reactivity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clopidogrel has been associated with better long-term outcome in patients with acute coronary syndrome or stable angina (SA) whether or not undergoing percutaneous coronary intervention (PCI) [1–3]. Beyond the inhibition of platelet aggregation, this beneficial effect of clopidogrel has been explained by potential vasoprotective mechanisms. In particular, clopidogrel has been shown to increase nitric oxide (NO) production in cultured endothelial cells and to improve NO mediated-vasodilatation in animal models [4, 5]. In patients with stable coronary artery disease (CAD), clopidogrel administration both as loading-dose or chronic therapy, has been associated with improvement in forearm blood flow and reduction of biomarkers of oxidative stress and inflammation [6, 7], suggesting a direct effect of clopidogrel on vascular endothelium, irrespective of its anti-platelet action.
Nevertheless, these studies have been conducted in patients with uniform optimal platelet inhibition to clopidogrel, therefore leaving unanswered the question as to whether endothelium improvement might also be associated with the degree of platelet inhibition [6, 7]. We tested the hypothesis that clopidogrel improvement of endothelial function is associated with inhibition of platelet aggregation.
Methods
Patient population
Patients with stable angina undergoing coronary angiography were consecutively screened for coronary artery disease amenable of percutaneous coronary intervention. Stable angina patients had typical stable chest pain or positive functional stress-tests. Only patients in whom PCI was electively staged (n = 43) were finally included in the study protocol. Patients were excluded in the presence of acute coronary syndrome, chronic therapy with or known allergy to clopidogrel, history of gastrointestinal bleeding or thrombocytopenia, platelet count < 100/nl, chronic renal failure (glomerular filtration rate < 90 ml/min), serious comorbidities, left ventricular ejection fraction <40%, IIb/IIIa inhibitors administration. All patients were under chronic aspirin treatment (160–325 mg). All patients received 600 mg clopidogrel loading dose at the time of hospital admission for the planned PCI.
Study protocol
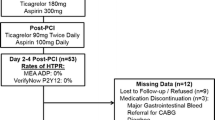
Peripheral endothelial function assessment and blood sample withdrawal was performed in the morning, after 12-h fasting state (Fig. 1). All vasoactive medications were withheld at least 24 h before the measurements: e.g. ace-inhibitors, calcium-antagonists, nitrates, beta-blockers. Protocol A was performed in 30 patients: baseline endothelial and platelet function assessment was performed the morning after the diagnostic coronary angiography. PCI was then electively staged in order to administer clopidogrel 600 mg loading dose uniformly at least 12 h before PCI. Second endothelial and platelet function assessment occurred in the morning right before the planned PCI after a mean time from clopidogrel administration of 14 ± 1 h. Except for clopidogrel, no changes in the ongoing medical therapy were allowed between the diagnostic and the interventional procedure. Mean time between baseline and post-clopidogrel endothelial and platelet function assessments was 27 ± 2 days. Protocol B was performed in 13 patients: at variance with protocol A, all the endothelial and biomarker measurements were performed at the time of the hospital admission for PCI. Baseline endothelial and platelet function assessment was performed in the morning, the day before the planned PCI. Clopidogrel 600 mg loading dose was administered thereafter. The morning after, the second endothelial and platelet function assessment occurred right before the planned PCI, after a mean time from clopidogrel administration of 16 ± 3 h.
Flow chart of the study protocols: patients were considered for inclusion in the study after coronary angiogram and in the presence of coronary stenosis amenable for elective PCI. Patients included in protocol A performed the baseline endothelial assessment the day after coronary angiography, while the post-clopidogrel assessment took place at the time of hospital admission for PCI. Patients included in protocol B performed both baseline and post-clopidogrel endothelial assessment during the admission for PCI
Protocol C was performed in 9 patients (control group), undergoing coronary angiography for suspected coronary artery disease, in whom no significant lesions could be detected and therefore a conservative medical treatment was advised: baseline endothelial function assessment (only Endoscore) was performed the morning after the diagnostic coronary angiography. Second endothelial assessment (only Endoscore) occurred the next morning.
The study was approved by local Ethics Committee and all patients provided written informed consent. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee.
Measurements of peripheral endothelial function
Peripheral endothelial function was measured by digital pulse amplitude with the Endothelial Peripheral Arterial Tonometry (Endo-PAT2000, Itamar Medical, Caesarea, Israel) as previously described [8, 9]. Briefly, the device measures distal finger blood volume changes accompanying pulse waves. A peripheral arterial tonometry (PAT) finger probe is placed at the tip of each index finger and a blood pressure cuff is placed at the level of the study arm. After a 5-min resting period (baseline), blood pressure cuff is inflated 20 mmHg above systolic pressure for 5 min (occlusion). Thereafter blood pressure cuff is deflated and PAT recording continued for additional 5 min (hyperemia). Endothelial responses were assessed by using the recently validated Framingham Reactive Hyperemia Index (Endoscore) [8], according to the following formula:
where lan is natural base log; RH is reactive hyperemia = mean pulse wave amplitude (PWA) of post occlusion section/mean PWA of baseline region of interest; OCC is occluded indicating the test arm, e.g. the arm on which the cuff is placed; CONT is control indicating the control arm; PWA is pulse wave amplitude.
Endothelial microparticles
Endothelial microparticles (EMPs) are sub-microscopic membrane vesicles shed from endothelial cells during activation and/or apoptosis and can be measured as a marker for endothelial injury [10–12]. Levels of EMPs before and after clopidogrel treatment were analyzed by flow cytometry. Blood samples were drawn into Monovette® collection tubes containing К2-EDTA (Sarstedt). Plasma was obtained by centrifugation for 10 min at 2,500×g. Further centrifugation for 25 min at 13,500×g was performed to obtain platelet free plasma (PFP). The PFP was stored at −80°C and thawed once before analysis. A volume of 50 μl of PFP was incubated with 5 μl of respectively CD42a-FITC, CD31-PE and CD45-PerCP (3-D) for 30 min in the dark at room temperature after which 2 ml of filtered (22 μm) FACSFlowTM solution (Becton–Dickinson) was added. Finally in each sample, 50 μl of SPHEROTM AccuCount particles (Spherotech Inc.) was added as reference particles with known number of particles per ml used to calculate the number of microparticles/μl detected in the samples. Microparticles were analyzed on a BD FACSCantoTM and were defined as particles <1 μm on a fluorescence/forward light scatter plot with the use of 1 μm diameter precision particles (microparticles GmbH, Germany). The EMP population was characterized as CD31+/CD42a− microparticles.
Assessment of platelet response
VerifyNow assay was used to assess platelet response to aspirin and clopidogrel. VerifyNow is a rapid platelet-function cartridge-based assay with specific cartridges for the P2Y12 pathway (clopidogrel) and for aspirin. The Verify Now P2Y12 is designed to directly measure the effects of drugs on the P2Y12 receptor, using prostaglandin E1 in addition to adenosine diphosphate to increase intraplatelet cyclic adenosine monophosphate, whereas the VerifyNow aspirin cartridge uses arachidonic acid. The results provided are expressed in P2Y12 reaction units (PRUs) and as aspirin reaction units (ARUs). Percentage inhibition P2Y12 from baseline activation by Thrombin Receptor Activating Peptide (TRAP) was calculated as (1 − PRU/baseline) × 100. Residual High platelet reactivity (HPR) is defined as PRU ≥ 240 to identify those patients with sub-optimal platelet response to clopidogrel. This PRU value has been previously proposed as optimal cut-off to discriminate patients undergoing PCI at higher risk of 30-day major adverse cardiovascular events (MACEs) [13, 14].
Statistical analysis
Statistical analysis was performed using the GraphPad Prism software, version 5. Normal distribution of measured parameters among the whole population was confirmed by Kolmogorov–Smirnov test. Continuous data are summarized as mean ± standard deviation and as median (interquartile ranges) in case of data not normally distributed (PRU, %PI, EMP, ∆EMP). Categorical variables are reported as frequencies and percentages. Student’s t test was used to compare continuous variables (age, BMI, LVEF, number of diseased vessels, cholesterol levels, Endoscore, ARU, PRU, %PI, EMP) between patients with LPR and HPR. χ2 test was used to test the differences in categorical variables between the 2 groups. Paired t test or Wilcoxon matched test were used to compare changes in Endoscore and EMPs before and after clopidogrel administration within groups. Correlation between variables was determined by Pearson or Spearman correlation tests as appropriate.
Variability between serial measurements was assessed in 6 normal volunteers by performing peripheral endothelial function assessment with Endo-PAT 2000 on 2 consecutive days in the morning, after 12-h fasting state. Average coefficient of variation between 2 consecutive measurements was 15 ± 9%, in line with previous reports [15]. Taking into account Endo-PAT test variability, the study was designed to have 80% power based on a difference of 3.0% points of Endoscore change after 600 mg clopidogrel as previously observed [7], with a minimum sample size of 10 patients per group (group with LPR vs. group with HPR). A P value of <0.05 was considered statistically significant.
Results
Baseline patients’ characteristics are shown in Table 1. Patients with HPR were more frequently diabetics, hypertensives and smokers. Body mass index (BMI) was found significantly elevated in patients with HPR, who were also more frequently treated with ACE-inhibitors.
Platelet response to clopidogrel
Platelet response to aspirin and clopidogrel is summarized in Tables 1 and 2. HPR was present in 23 patients, where LPR was present in the remaining 20 patients. Platelet percent inhibition was significantly lower in patients with HPR as compared with patients with LPR. ARU was not different between patients with HPR and LPR.
Peripheral endothelial function
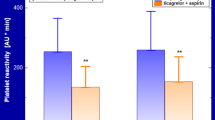
A significant inverse correlation was found between Endoscore changes (∆%) and PRU (r = −0.61, P < 0.001) (Fig. 2, panel a). A significant direct correlation was found between ∆% Endoscore and % platelet inhibition (r = 0.57, P < 0.001) (Fig. 2, panel b). A significant overall Endoscore improvement was observed in patients with LPR after clopidogrel (from 0.38 ± 0.26 to 0.57 ± 0.33, P < 0.001) (Table 2). No significant difference was observed after clopidogrel in patients with HPR (from 0.53 ± 0.31 to 0.40 ± 0.37, P = 0.10). Baseline and post-clopidogrel Endoscore in patients undergoing protocol A and B are reported in Table 2. In the control group, Endoscore did not significantly differ between the second and first endothelial function assessment (0.57 ± 0.22 vs. 0.52 vs. 0.20, P = 0.42).
A variable response to 600 mg clopidogrel loading dose was observed in the patients population. A linear correlation between Endoscore and PRU (panel a) and between Endoscore and % platelet inhibition (panel b) suggest an effect of the anti-platelet efficacy of clopidogrel on endothelial function improvement
Endothelial microparticles
Endothelial microparticles (EMPs) were slightly but significantly increased after clopidogrel administration in the overall patient population undergoing protocol A, while no significant difference was observed in patients undergoing protocol B (Table 2). Overall, a significant direct correlation was found between EMP changes (∆%) and PRU (r = 0.47, P = 0.002), and a significant inverse correlation was found between ∆% EMP and % platelet inhibition (r = −0.36, P = 0.02, Fig. 3). A significant EMP decrease was observed after clopidogrel in patients with LPR undergoing protocol A, while a trend to a decrease was observed in patients with LPR undergoing protocol B (Table 2). No difference was observed after clopidogrel in patients with HPR irrespective of protocol A or B (Table 2).
Discussion
In the present study we demonstrated that a significant improvement of peripheral endothelial function is observed in patients with LPR after 600 mg clopidogrel loading-dose. This improvement was not observed in patients with HPR.
Platelet–endothelium interaction
Platelets are actively involved in the onset of endothelial dysfunction and development of vascular atherosclerosis [16–18]. Platelets are activated in patients with coronary artery disease [19], where they adhere to vascular endothelium potentially triggering adverse vascular events through oxidative and pro-inflammatory mechanisms [20]. In addition, platelet inhibition with aspirin and IIb/IIIa inhibitors has been demonstrated to improve vascular endothelial function [21–23], confirming the importance of platelet–endothelium interactions in the pathogenesis of endothelial dysfunction.
Clopidogrel and vascular endothelium
Clopidogrel has been demonstrated to directly improve vascular endothelial function. Clopidogrel increases nitric oxide (NO) production in cultured endothelial cells and improves NO mediated-vasodilatation in animal models [4, 5]. In patients with stable coronary artery disease (CAD), clopidogrel administration both as loading-dose or chronic therapy, improves forearm blood flow and reduces biomarkers of oxidative stress and inflammation [6, 7]. These findings suggested a direct improvement of the endothelial function by clopidogrel irrespective of its anti-platelet action. Yet, all these studies were conducted in patients with uniform optimal response to clopidogrel, therefore not allowing any conclusion concerning the effect of clopidogrel in patients with suboptimal platelet inhibition.
Our study adds on the current body of evidence, because in patients with HPR after clopidogrel, no significant endothelial function improvement can be expected, irrespective of the protocol performed (Table 2; Fig. 2). On the contrary, in patients with LPR, we confirmed with both protocols a significant Endoscore increase (Fig. 2; Table 2) in agreement with previous studies [6, 7]. These observations were corroborated by assessing endothelial microparticles (EMPs), used as marker of endothelial dysfunction and atherosclerosis [10, 24–30]. EMPs were significantly reduced after clopidogrel in patients with optimal platelet inhibition (LPR), while no significant changes were observed in HPR patients (Fig. 3; Table 2). This confirms the Endoscore data and suggests an association between the degree of platelet inhibition with clopidogrel and improvement in endothelial function.
In an independent patient population, we have recently demonstrated an inverse correlation between endothelial function and residual platelet reactivity after 600 mg clopidogrel [31]. In the present study, we further extended these findings to the potential modulation of endothelial function exerted by clopidogrel. At variance with the previous study, coronary anatomy here was already investigated at the moment the first endothelium evaluation was performed, in order to select only those patients candidate to elective percutaneous coronary intervention, therefore undergoing clopidogrel loading. The lower platelet reactivity after 600 mg clopidogrel is not only predictive of lower endothelial impairment, as previously shown [31], but also, according to the present findings, it is associated with significant improvement of endothelial function. Yet, Warnholtz et al. [7] failed to show any correlation between changes in flow mediated dilatation and changes in platelet reactivity index after two different clopidogrel loading doses (300 and 600 mg). This apparent discrepancy with our findings can be explained by the significantly lower flow mediated dilatation observed in this study at 2 and 4 h in patients loaded with 300 mg clopidogrel versus patients loaded with 600 mg which parallels different degree of P2Y12 platelet inhibition. At 22 h, in fact, when platelet inhibition with both doses reaches a comparable plateau, no significant differences in flow mediated dilation are anymore detectable in the 2 groups. More recently, the same investigators have found neither an effect of chronic clopidogrel treatment (75 mg/day for 1 month) on endothelial function nor a correlation with the degree of platelet inhibition [32]. Several differences do not allow comparisons with our study: e.g., clopidogrel loading dose was not administered, platelet reactivity was assessed with light trasmittance aggregometry, threshold chosen to evaluate low responders to clopidogrel, chronic versus acute administration.
Clinical implications
In addition to a direct effect, our study suggests that the degree of platelet inhibition represents an important additional mechanism by which clopidogrel improves endothelial function. Importantly, degree of platelet inhibition with clopidogrel is variable, and it is common to observe with the same 600 mg loading dose patients with suboptimal platelet inhibition (Fig. 2) or high platelet reactivity (HPR). Presence of HPR, in particular, has been associated with increased cardiovascular events both at the time of the percutaneous coronary intervention and at long-term follow-up [13, 14). On the other side, a more aggressive and effective anti-platelet therapy has been associated with a significant improvement in clinical outcome as compared to clopidogrel [33, 34]. Endothelial dysfunction predicts adverse clinical outcome and can be reverted with appropriate pharmacologic therapy. Whether a more effective anti-platelet therapy is able to prevent not only thrombotic events but also revert endothelial dysfunction, with potential positive impact on clinical outcome, is an intriguing hypothesis that needs to be further investigated.
Study limitations
The study is limited in its non-randomized and not-blinded nature. In addition, this study is not designed to distinguish between the relative contribution of direct stimulatory effect of clopidogrel on endothelial NO from the one mediated by platelet P2Y12 receptor inhibition.
Genetic polymorphisms have been recently described in the subtype 2C19 of cytochrome P-450 enzyme which results into a reduced transformation of clopidogrel into its active metabolite [35]. In this study, we cannot exclude that in some of our patients suboptimal platelet inhibition to clopidogrel might be genetically determined. Nevertheless, we believe this to be of little impact on our findings because: (1) we focused on the final target of activated clopidogrel; (2) intra-individual endoscore changes before and after 600 mg clopidogrel were measured, therefore preventing potential genetic bias linked to inter-individual comparisons.
Withdrawal of nitrates has been reported to alter coronary endothelial vasomotor response [36]. In our study, a minority of patients was on nitrates, therefore endothelial assessment might have been influenced by nitrates withdrawal. Yet, we believe this to be of limited impact on our findings because: (1) the same experimental conditions were kept during baseline and post-clopidogrel endothelial assessment; (2) Patients on nitrates were equally distributed in both LPR and HPR group (15% vs. 22%, P = 0.7).
Conclusions
A significant improvement of endothelial function is observed in patients with low residual platelet reactivity after 600 mg clopidogrel loading-dose. This improvement is associated with the degree of platelet P2Y12-inhibition as it is not observed in patients with high platelet reactivity after clopidogrel.
References
Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK (2001) Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 345(7):494–502
Mehta SR, Yusuf S, Peters RJ et al (2001) Clopidogrel in Unstable angina to prevent Recurrent Events trial (CURE) Investigators. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 358:527–533
Steinhubl SR, Berger PB, Mann JT III et al, CREDO Investigators (2002) Clopidogrel for the reduction of events during observation. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA 19:2411–2420
Ziemianin B, Olszanecki R, Uracz W, Marcinkiewicz E, Gryglewski RJ (1999) Thienopyridines: effects on cultured endothelial cells. J Physiol Pharmacol 50:597–604
Jakubowski A, Chlopicki S, Olszanecki R et al (2005) Endothelial action of thienopyridines and thienopyrimidinones in the isolated guinea pig heart. Prostaglandins Leukot Essent Fatty Acids 72:139–145
Heitzer T, Rudolph V, Schwedhelm E et al (2006) Clopidogrel improves systemic endothelial nitric oxide bioavailability in patients with coronary artery disease: evidence for antioxidant and antiinflammatory effects. Arterioscler Thromb Vasc Biol 26(7):1648–1652
Warnholtz A, Ostad MA, Velich N et al (2008) A single loading dose of clopidogrel causes dose-dependent improvement of endothelial dysfunction in patients with stable coronary artery disease: results of a double-blind, randomized study. Atherosclerosis 196:689–695
Hamburg NM, Keyes MJ, Larson MG et al (2008) Cross-sectional relations of digital vascular function to cardiovascular risk factors in the Framingham Heart Study. Circulation 117(19):2467–2474
Bonetti PO, Pumper GM, Higano ST, Holmes DR, Kuvin JT, Lerman A (2004) Noninvasive identification of patients with early coronary atherosclerosis by assessment of digital reactive hyperemia. J Am Coll Cardiol 44:2137–2141
Werner N, Wassmann S, Ahlers P, Kosiol S, Nickenig G (2006) Circulating CD31+/annexin V+ apoptotic microparticles correlate with coronary endothelial function in patients with coronary artery disease. Arterioscler Thromb Vasc Biol 26(1):112–116
Boulanger CM, Amabile N, Tedgui A (2006) Circulating microparticles: a potential prognostic marker for atherosclerotic vascular disease. Hypertension 48(2):180–186
Bernal-Mizrachi L, Jy W, Fierro C et al (2004) Endothelial microparticles correlate with high-risk angiographic lesions in acute coronary syndromes. Int J Cardiol 97(3):439–446
Patti G, Nusca A, Mangiacapra F, Gatto L, D’Ambrosio A, Di Sciascio G (2008) Point-of-care measurement of clopidogrel responsiveness predicts clinical outcome in patients undergoing percutaneous coronary intervention results of the ARMYDA-PRO (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty-Platelet Reactivity Predicts Outcome) study. J Am Coll Cardiol 52(14):1128–1133
Price MJ, Endemann S, Gollapudi RR et al (2008) Prognostic significance of post-clopidogrel platelet reactivity assessed by a point-of-care assay on thrombotic events after drug-eluting stent implantation. Eur Heart J 29(8):992–1000
Crandall JP, Shamoon H, Cohen HW et al (2009) Post-challenge hyperglycemia in older adults is associated with increased cardiovascular risk profile. J Clin Endocrinol Metab 94(5):1595–1600
Gawaz M, Neumann FJ, Ott I et al (1997) Vitronectin receptor (alpha(v)beta3) mediates platelet adhesion to the luminal aspect of endothelial cells: implications for reperfusion in acute myocardial infarction. Circulation 96:1809–1818
May AE, Seizer P, Gawaz M (2008) Platelets: inflammatory firebugs of vascular walls. Arterioscler Thromb Vasc Biol 28(3):s5–s10
Gawaz M, Langer H, May AE (2005) Platelets in inflammation and atherogenesis. J Clin Investig 115(12):3378–3384
Furman MI, Benoit SE, Barnard MR et al (1998) Increased platelet reactivity and circulating monocyte-platelet aggregates in patients with stable coronary artery disease. J Am Coll Cardiol 31(2):352–358
Davi G, Patrono C (2007) Platelet activation and atherothrombosis. N Engl J Med 357:2482–2494
Husain S, Andrews NP, Mulcahy D, Panza JA, Quyyumi AA (1998) Aspirin improves endothelial dysfunction in atherosclerosis. Circulation 97:716–720
Quyyumi AA (1998) Effects of aspirin on endothelial dysfunction in atherosclerosis. Am J Cardiol 82(10A):31S–33S
Heitzer T, Ollmann I, Koke K, Meinertz T, Munzel T (2003) Platelet glycoprotein IIb/IIIa receptor blockade improves vascular nitric oxide bioavailability in patients with coronary artery disease. Circulation 108:536–541
Morel O, Toti F, Hugel B et al (2006) Procoagulant microparticles: disrupting the vascular homeostasis equation? Arterioscler Thromb Vasc Biol 26:2594–2604
Bernal-Mizrachi L, Jy W, Jimenez JJ et al (2003) High levels of circulating endothelial microparticles in patients with acute coronary syndromes. Am Heart J 145:962–970
Ettelaie C, Collier ME, James NJ, Li C (2006) Induction of tissue factor expression and release as microparticles in ECV304 cell line by Chlamydia pneumoniae infection. Atherosclerosis 190:343–351
Leroyer AS, Isobe H, Lesèche G (2007) Cellular origins and thrombogenic activity of microparticles isolated from human atherosclerotic plaques. J Am Coll Cardiol 49:772–777
Mause SF, von Hundelshausen P, Zernecke A, Koenen RR, Weber C (2005) Platelet microparticles: a transcellular delivery system for RANTES promoting monocyte recruitment on endothelium. Arterioscler Thromb Vasc Biol 25:1512–1518
Morel O, Pereira B, Averous G et al (2009) Increased levels of procoagulant tissue factor-bearing microparticles within the occluded coronary artery of patients with ST-segment elevation myocardial infarction: role of endothelial damage and leukocyte activation. Atherosclerosis 204:636–641
Juul-Möller S, Edvardsson N, Jahnmatz B, Rosén A, Sorensen S, Ömblus R (1992) Double-blind trial of aspirin in primary prevention of myocardial infarction in patients with stable chronic angina pectoris. The Swedish Angina Pectoris Aspirin (SAPAT) trial. Lancet 340:1421–1425
Muller O, Hamilos M, Bartunek J, Ulrichts H, Mangiacapra F, Holz JB, Ntalianis A, Trana C, Dierickx K, Vercruysse K, De Bruyne B, Wijns W, Barbato E (2010) Relation of endothelial function to residual platelet reactivity after clopidogrel in patients with stable angina pectoris undergoing percutaneous coronary intervention. Am J Cardiol 105:333–338
Ostad MA, Nick E, Paixao-Gatinho V, Schnorbus B, Schiewe R, Tschentscher P, Munzel T, Warnholtz A (2011) Lack of evidence for pleiotropic effects of clopidogrel on endothelial function and inflammation in patients with stable coronary artery disease: results of the double-blind, randomized CASSANDRA study. Clin Res Cardiol 100(1):29–36
Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM, Triton-TIMI 38 Investigators (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357(20):2001–2015
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, Mahaffey KW, Scirica BM, Skene A, Steg PG, Storey RF, Harrington RA, Freij A, Thorsen M, PLATO Investigators (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361(11):1045–1057
Collet JP, Hulot JS, Pena A et al (2009) Cytochrome P450 2C19 polymorphism in young patients treated with clopidogrel after myocardial infarction: a cohort study. Lancet 373:309–317
Azevedo ER, Schofield AM, Kelly S, Parker JD (2001) Nitroglycerin withdrawal increases endothelium-dependent vasomotor response to acetylcholine. J Am Coll Cardiol 37:505–509
Acknowledgments
This work was supported by an unrestricted grant from Meijer Lavino Foundation for Cardiovascular Research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Michalis Hamilos, Olivier Muller are the two authors contributed equally to this study.
Rights and permissions
About this article
Cite this article
Hamilos, M., Muller, O., Ntalianis, A. et al. Relationship between peripheral arterial reactive hyperemia and residual platelet reactivity after 600 mg clopidogrel. J Thromb Thrombolysis 32, 64–71 (2011). https://doi.org/10.1007/s11239-011-0557-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-011-0557-x