Abstract
Background
Recently we have demonstrated a dose-dependent improvement of endothelial function after administration of a single loading dose of clopidogrel in patients with coronary artery disease (CAD). We therefore hypothesized that chronic therapy with clopidogrel may improve endothelial function in patients with CAD.
Methods
In a double-blind, randomized, monocentric study 120 patients with established CAD were randomized to one of the following treatment arms: clopidogrel 75 mg q.d., acetylsalicylic acid (ASA) 100 mg q.d., or a combination of ASA and clopidogrel. Endothelium-dependent flow-mediated dilation (FMD) and endothelium-independent nitroglycerin-mediated dilation (NMD) of the brachial artery were determined before and after 28 days of treatment. The effect of clopidogrel was monitored in vitro by ADP-induced platelet aggregation in platelet-rich plasma. Effects of treatment on platelet superoxide production were measured by lucigenin-enhanced chemiluminescence in washed platelets. C-reactive protein, RANTES and monocyte chemoattractant protein-1 were determined as inflammatory markers. The study was registered as ISRCTN34097747.
Results
Treatment groups were comparable regarding age, gender, cardiovascular risk factor distribution and concomitant medication. FMD [median (IQR) ASA, +0.8 (−2.0; 2.7); ASA + clopidogrel, ±0 (−2.0; 2.9); clopidogrel, +1.0 (−1.1; 2.4); P = n.s.], NMD, platelet superoxide production or inflammatory markers remained unchanged in all treatment groups.
Conclusion
We conclude that the beneficial effects of short-term effects of clopidogrel on endothelial function of patients with CAD are abolished after long-term clopidogrel treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Animal and clinical studies have identified an important role for platelets in the pathogenesis of atherosclerosis. Inhibition of platelet aggregation by acetylsalicylic acid (ASA) involves the inhibition of cyclooxygenase and is part of the chronic standard therapy of patients with coronary artery disease (CAD). The inhibition of ADP-mediated platelet aggregation by clopidogrel has been shown to reduce major adverse events after percutaneous coronary intervention and in acute coronary syndrome compared with treatment with ASA alone [8]. The underlying mechanisms of this positive clinical effect of clopidogrel is currently assumed to be the inhibition of thrombus formation within the inserted coronary stent and/or dilated coronary artery segment or the improvement of the coronary flow of the microcirculation by inhibition of peripheral microembolization. However, ex vivo studies indicate important interactions between different cell types (platelets, endothelial cells, vascular smooth muscle cells, leukocytes) in the atherosclerotic vasculature [10]. Atherosclerosis is associated with or secondary to endothelial dysfunction that is characterized by reduced vascular nitric oxide bioavailability leading to enhanced platelet aggregation and adhesion. Recent studies suggest that activated human platelets of diabetic [9] and hypercholesterolemic patients [7] in turn can cause endothelial dysfunction via release of reactive oxygen species such as superoxide anions due to the activation of superoxide producing enzymes in platelets and/or the vasculature such as the NAD(P)H oxidase, cyclooxygenase, xanthine oxidase, or an uncoupled nitric oxide synthase or indirectly via activation of leukocytes. We have previously demonstrated that a loading dose of clopidogrel improves endothelial function in patients with stable CAD and have found that this effect is dose dependent [17]. The aim of the present study was to determine whether these beneficial effects of clopidogrel therapy on endothelial function are long lasting in patients with CAD or whether they are subject to tolerance. We also sought to gain insight into the mechanism of platelet-induced endothelial dysfunction by measurement of platelet superoxide production and markers of inflammation.
Methods
Patients
The “Effect of Clopidogrel vs. ASA and Clopidogrel or ASA alone on Brachial Flow Mediated Vasodilation in Patients with Coronary Artery Disease” (CASSANDRA) study was conducted as a prospective, randomized, double-blind, three-armed, single-center study. The study included patients who were previously treated at our institution for CAD. The main inclusion criteria were the angiographical documentation of CAD and the absence of unstable angina pectoris within the previous 4 weeks. The most relevant exclusion criteria were a cerebrovascular accident or peripheral artery revascularisation within 12 weeks prior to the study, clopidogrel or ticlopidine treatment within 28 days prior to the study, planned coronary or peripheral stent implantation within the following 6 weeks, renal failure (serum creatinine >2.0 mg/dl or known nephrotic syndrome), chronic inflammatory bowel disease with malabsorption in the small intestine, gastric ulcer or history of upper or lower gastrointestinal bleeding, hematological disease (hemoglobin <12 g/dl, WBC <4,000/μl, thrombocytes <100,000/μl), left ventricular ejection fraction <40%, uncontrolled hypertension, and an onset of ACE-inhibitor, AT1-RB, calcium channel antagonist, statin therapy within 14 days prior to study inclusion. Written informed consent was obtained. The study protocol was approved by the independent ethics committee of the chamber of physicians of Rhineland-Palatinate, Mainz, Germany. Investigations were undertaken in accordance with the Declaration of Helsinki. The study is registered as a controlled trial with the ISRCTN34097747.
Study protocol
Patients were screened by revision of the hospital charts. The stable character of CAD was verified by documentation of a negative bicycle stress test at the time of inclusion. ASA treatment was stopped for 7 days prior to randomization. After informed consent patients fulfilling all inclusion criteria and none of the exclusion criteria were randomized to take either ASA 100 mg q.d., combined ASA 100 mg and clopidogrel 75 mg q.d., or clopidogrel 75 mg q.d. for 28 days. All patients took 2 tablets/day, one looking identical to ASA and the other one looking identical to clopidogrel, in order to ensure blindness to the treatment. Depending on the treatment arm, the second tablet in the clopidogrel or ASA treatment arm consisted of matching placebos. The study course consisted of three visits: visit 1 included the screening procedure, visit 2 after 7 days included measurements of flow-mediated dilation (FMD), nitroglycerin-mediated dilation (NMD) and blood sampling for platelet function, platelet superoxide measurements and determination of inflammatory markers. Visit 3 was held after 35 days to repeat vascular function and laboratory tests after 4 weeks of therapy. Resting systolic, diastolic and mean arterial blood pressures were measured in the supine position after 10 min rest using a non-invasive blood pressure monitor (DINAMAP 100, Critikon).
Assessment of vascular function
Endothelium-dependent FMD of the brachial artery was non-invasively examined by 2-dimensional high-resolution ultrasonic imaging, as described previously [16]. Briefly, 2-dimensional images of the right brachial artery and pulsed-Doppler flow velocity signals were obtained before and 60 s after generation of reactive hyperemia by a 5-min period of upper arm occlusion. The nitroglycerin-mediated, endothelium-independent dilation (NMD) was measured before and 4 min after sublingual administration of nitroglycerin (0.8 mg). All images were digitally recorded in DICOM format for later analysis. Brachial artery imaging and pulsed-Doppler velocity profile analysis were performed as described previously. FMD was calculated as the percentage change in brachial artery diameter in response to hyperemia. The relative increase in blood flow during reactive hyperemia was expressed as the percentage increase in flow from baseline. Image acquisition and analysis were performed in a blinded manner. Room temperature was held constant at 21–23°C.
Analysis of platelet aggregation
Platelet aggregation was evaluated by light transmission aggregometry in platelet-rich plasma (PRP). Briefly, PRP was prepared by centrifugation of citrated venous blood at 220 g for 20 min at room temperature. PRP was carefully transferred to a fresh tube avoiding the transfer of red and white blood cells. Aggregation of platelets in PRP was induced by stimulation with ADP [diluted in platelet-poor plasma (PPP) yielding a final concentration of 20 μM]. The platelet aggregatory response to stimulation was monitored in a Chrono-Log Series 560 aggregometer (Probe&Go, Endingen, Germany) under continuous stirring at 37°C for 5 min. Platelet aggregation was expressed as the maximum percentage change in light transmittance from baseline, with PPP used as a reference for 100% aggregation.
Analysis of platelet superoxide production
Platelet superoxide production was measured in washed platelets that were prepared as described previously [17]. Results are expressed in nmol/108 platelets min.
Blood analyses
A venous blood sample was obtained after overnight fast, centrifuged at 2,000g for 10 min at 4°C and stored at −80°C until further analysis. Plasma cholesterol, HDL, triglycerides, fasting glucose and uric acid were measured using an automated analyzer. LDL-cholesterol was calculated by the Friedewald formula. Concentrations of plasma C-reactive protein (CRP) were measured by a high-sensitive immunoturbidimetric method (Tina-quant CRP, Roche Diagnostics). The pro-inflammatory and pro-atherosclerotic chemokine monocyte chemoattractant protein-1 (MCP-1) and the platelet-derived chemokine regulated on activation, normal T cell expressed and secreted (RANTES) were determined by ELISA (R&D Diagnostics, Wiesbaden, Germany).
Statistical analysis
The prospectively determined primary endpoint of the study was the absolute change of FMD before and after treatment. The estimation of the group size in order to detect a significant difference of 2% FMD based upon the assumption of a standard deviation of 4%, an α-error of 5% and a statistical power of 80% revealed 40 patients per group. Normality of distribution was tested by the Kolmogorov–Smirnov test. Variables were compared before and after treatment within groups by paired student’s t test or by Wilcoxon signed rank test when normality test failed. Comparisons between groups were performed by one-way analysis of variance or Kruskal–Wallis One-way analysis of variance on ranks when normality test failed. Baseline data of the three study groups were compared using the unpaired Student’s t test or chi-square test as appropriate. Correlation between ADP-responses and changes in FMD were examined by calculation of the Pearson correlation coefficient. Analysis was performed in the intention-to-treat population. Data were analyzed by SPSS 17.0, SPSS Inc. All data are presented as mean ± SD or median (interquartile range). P values of <0.05 were considered significant.
Results
Study patients
A total of 120 patients were enrolled in the study. The three groups were comparable with regard to age, sex, body mass index, resting blood pressure, blood cholesterol levels, the percentage of current smokers or patients with diabetes, or concomitant statin therapy. Three patients did not complete the study course. Therefore, 117 patients constituted the intention-to-treat population. Demographic, clinical and biochemical characteristics of the patients are displayed in Table 1.
Vascular function
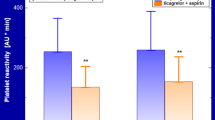
Arterial baseline diameter and FMD were comparable among all groups before treatment. There was no detectable difference in the change of FMD after treatment with ASA, ASA + clopidogrel or clopidogrel, respectively (Fig. 1). Brachial artery variables are displayed in Table 2. Nitroglycerin-induced endothelium-independent dilation of the brachial artery remained unchanged in all groups (Table 2). Changes in FMD were independent from changes in ADP-induced platelet aggregation as the correlation coefficient between change in ADP-induced platelet aggregation and change in FMD were in the ASA group −0.02 (P = 0.91), ASA + clopidogrel group −0.14 (P = 0.41) and clopidogrel group 0.2 (P = 0.21), respectively. Subdivision of the clopidogrel groups in clopidogrel low-responder versus responder indicating low-responder by a cut-off value of >50% of ADP-induced platelet aggregation at the end of the treatment did not reveal differences in the change in FMD supporting our main result that FMD is unaffected by long-term clopidogrel treatment [absolute change in FMD (%)] for ASA + clopidogrel group: responder, +0.69 ± 2.61; low-responder, +0.85 ± 2.85; clopidogrel group: responder, −0.24 ± 3.15; low-responder, +0.84 ± 2.58 (all data in mean ± SD).
Results of the primary study objective: Effect of treatments on flow-mediated dilation (FMD) of the right brachial artery. Data are presented in box-whisker plots demonstrating median, 25th and 75th percentile, 10th and 90th percentile (error bars), and single outlying values (black dots) of absolute changes in FMD before and after treatment in the three treatment groups
ADP-induced platelet aggregation
ADP-induced platelet aggregation was comparable in all groups before treatment. After treatment, ADP-induced platelet aggregation was significantly inhibited in the ASA + clopidogrel and clopidogrel group, but not in the ASA group, with significant difference in ASA + clopidogrel and clopidogrel group compared to ASA group (Table 3). The platelet aggregation measurements indicate effective clopidogrel treatment.
Platelet superoxide production
Basal platelet superoxide production was comparable at baseline and remained unchanged in each of the three treatment groups after treatment (Table 3).
Markers of inflammation
Plasma concentrations of CRP, MCP-1 and RANTES were comparable at baseline and did not change after treatment (Table 3).
Discussion
Traditionally, the clinical benefit of clopidogrel has been attributed to its inhibition of platelet activation and aggregation. However, recent research has suggested additional pleiotropic anti-atherosclerotic roles of clopidogrel such as modulation of vascular tone, improvement of NO bioavailability as well as inhibition of inflammation and oxidative stress. The results of our double-blind, randomized study, however, argue against pleiotropic effects of clopidogrel since endothelial function, inflammatory markers and platelet superoxide production remained unchanged in patients with stable CAD after 4 weeks of treatment with clopidogrel in the clinically routinely used dose of 75 mg/day.
A growing body of literature has suggested that antiplatelet therapies improve endothelial function in atherosclerosis. Improvement of endothelial function has been shown for the cyclooxygenase antagonist ASA [5], glycoprotein IIb/IIIa receptor antagonists tirofiban and eptifibatide [3, 16] and the P2Y12 ADP-receptor antagonist clopidogrel [4, 17]. The proposed underlying mechanisms are likely multifactorial and include, but are not limited to, the decrease in platelet NO consumption [20], inhibition of platelet–leukocyte–endothelium cross talk, inhibition of platelet-derived reactive oxygen species production or direct drug effects on the endothelium. In our previous study we were able to demonstrate that oral administration of a single loading dose of clopidogrel (300 and 600 mg, respectively) leads to dose-dependent improvement of endothelial function in patients with stable CAD [17]. Surprisingly, this effect did not correlate with the platelet inhibitory effect of clopidogrel pointing towards effects independent of the ADP-receptor inhibition being responsible for the improvement in endothelial function. We had speculated that clopidogrel either directly or indirectly via its active metabolite may affect vascular proteins and functions other than the platelet ADP P2Y12 receptor. This speculation was based on recent findings from animal and in vitro studies that have identified platelet-independent effects of thienopyridines and thienopyrimidinones on the vasculature itself. Studies by Jakubowski et al. [6] identified direct stimulation of NO-dependent coronary vasodilation by clopidogrel independent of its antiplatelet action in the isolated guinea pig heart. If direct effects of clopidogrel or an active metabolite may have caused the effect on endothelial function in our previous study, the negative result with regards to the effect on endothelial function in the present study may be explained by the lower dose of clopidogrel used or by compensatory or tolerance mechanisms that may have taken effect within the treatment period of 4 weeks. Direct effects may include interaction with P2Y12 ADP-receptors on vascular cells that are expressed in endothelial and vascular smooth muscle cells of various vascular beds [12, 19]. The results of our study could not confirm the results of the only study published to date that investigated the effects of long-term clopidogrel treatment on endothelial function in patients with stable CAD [4]. While the study population was very similar, Heitzer et al. investigated patients on ASA treatment, conducted the study openly and measured endothelial function of arterioles via plethysmography and not of large conductance arteries.
Recently, McVeigh and coworkers have demonstrated an increase in platelet superoxide production in hypertensive diabetic patients [2] and patients with decompensated heart failure due to uncoupling of platelet nitric oxide synthase. However, in the present study, platelet superoxide production was unaffected by clopidogrel treatment rendering antioxidative effects unlikely. Importantly and supportive for the validity of our results, we can exclude ineffective treatment with clopidogrel because the ADP-induced platelet aggregation was significantly reduced in the clopidogrel treatment groups. Our study design allowed us to test the effects of ASA 100 mg/day on endothelial function in patients with stable CAD as well. Previous studies have demonstrated an improvement in endothelial function upon application of ASA in patients with atherosclerosis [5]. Importantly, the dose of ASA used in the study of Husein et al. to improve endothelial function was 1 g and therefore ASA was used in an antirheumatic dose, therefore not comparable with the low dose of ASA used in the present study. Another study by Williams et al. [20] in healthy volunteers demonstrated that platelet NO consumption was markedly reduced in response to 75 mg/day ASA treatment and that this effect directly correlated with the inhibition of COX, but the authors did not check whether this maneuver may have beneficial effects on endothelial function in the investigated subjects. The results of our present study, however, suggest that a dose of 100 mg ASA/day that is routinely applied in clinical setting is not sufficient to improve endothelial function in patients with established CAD.
Expanding evidence supports the existence of a close relationship between platelets, endothelium, leukocytes, atherosclerosis and atherothrombosis. Platelet activation leads to the release of pro-inflammatory mediators that initiate the cross talk between platelets, leukocytes and cells of the vascular wall. Accordingly, we have studied the effect of long-term clopidogrel treatment on CRP, MCP-1 and RANTES plasma concentrations. While CRP is a more general indicator of inflammation, MCP-1 is a key mediator of monocyte trafficking made by multiple cell types including endothelial cells, smooth muscle cells and macrophages, and RANTES is a pro-inflammatory mediator predominantly released by platelets. In contrast to the accumulated evidence of anti-inflammatory effects of clopidogrel [14], we could not detect anti-inflammatory properties of clopidogrel at least with our dose of 75 mg/day. However, the evidence of anti-inflammatory properties of clopidogrel mainly derives from preclinical studies or studies in patients with acute exacerbation of atherosclerosis such as acute coronary syndrome or acute stroke and after percutaneous coronary intervention. Anti-inflammatory effects of clopidogrel may be detectable due to activation of inflammatory cascades that is well described in these settings. The levels of CRP in our study were quite low with median levels between 1.6 and 1.7 mg/l, respectively. Therefore, anti-inflammatory effects of clopidogrel may have been masked possibly due to the stability of CAD and the background therapy with statin and/or inhibitors of the renin–angiotensin system (RAS). While our results are in contrast to the findings reported by Heitzer et al.[4], they are in line with the results of other randomized studies with regards to the effect of clopidogrel on hs-CRP, MCP-1 and RANTES in patients with stable CAD [1, 13, 15].
Conclusions
Taken together, at least for the used dose of 75 mg clopidogrel per day, as applied in clinical routine, for the treatment period of 4 weeks and for patients with stable CAD and moderately intense protective background therapy with statins and RAS inhibitors, we conclude that long-term clopidogrel in a dose of 75 mg/day is without effect on endothelial function, inflammation and platelet superoxide production. We can also state that low-dose ASA therapy is not able to improve endothelial function in this patient group. The lack of effect of clopidogrel on endothelial function may be due to tolerance mechanisms, due to the fact that the dose was too low or the lack of activation of the inflammatory cascade in our patient population. These results, of course, do not diminish the benefit of treatment in acute coronary syndrome and after PCI, but do not support the expansion of clinical use of clopidogrel as “anti-inflammatory” or endothelium-protective drug. Even if pleiotropic effects were dose dependent, an increase in clopidogrel dose would not be justified due to increased risk of bleeding. Whether newer antiplatelet drugs such as prasugrel or ticagrelor in clinically applied doses exert pleiotropic effects on the vasculature and inflammation remains to be investigated.
Study limitations
We could not incorporate a placebo group since 4 weeks of treatment of patients with CAD without an antiplatelet agent is unethical. In previous randomized studies we have detected an increase in FMD of median 1.1% after 8 weeks [11] and median 1.6% after 12 weeks [18] of placebo treatment as a control group. Since the median changes in FMD were between 0 and 1% in the present study, a placebo group for comparison would probably have confirmed the lack of effect on FMD or even demonstrated deterioration of FMD in the treatment groups. For technical reasons the measurements of arachidonic acid-induced platelet aggregation failed in a considerable number of samples and therefore we cannot present a proof of effectiveness of ASA treatment.
References
Azar RR, Kassab R, Zoghbi A et al (2006) Effects of clopidogrel on soluble CD40 ligand and on high-sensitivity C-reactive protein in patients with stable coronary artery disease. Am Heart J 151:521e1–521e4
Dixon LJ, Hughes SM, Rooney K et al (2005) Increased superoxide production in hypertensive patients with diabetes mellitus: role of nitric oxide synthase. Am J Hypertens 18:839–843
Heitzer T, Ollmann I, Koke K et al (2003) Platelet glycoprotein IIb/IIIa receptor blockade improves vascular nitric oxide bioavailability in patients with coronary artery disease. Circulation 108:536–541
Heitzer T, Rudolph V, Schwedhelm E et al (2006) Clopidogrel improves systemic endothelial nitric oxide bioavailability in patients with coronary artery disease: evidence for antioxidant and antiinflammatory effects. Arterioscler Thromb Vasc Biol 26:1648–1652
Husain S, Andrews NP, Mulcahy D et al (1998) Aspirin improves endothelial dysfunction in atherosclerosis. Circulation 97:716–720
Jakubowski A, Chlopicki S, Olszanecki R et al (2005) Endothelial action of thienopyridines and thienopyrimidinones in the isolated guinea pig heart. Prostaglandins Leukot Essent Fatty Acids 72:139–145
Kaul S, Waack BJ, Padgett RC et al (1993) Altered vascular responses to platelets from hypercholesterolemic humans. Circ Res 72:737–743
Mehta SR, Yusuf S, Peters RJ et al (2001) Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 358:527–533
Oskarsson HJ, Hofmeyer TG (1997) Diabetic human platelets release a substance that inhibits platelet-mediated vasodilation. Am J Physiol 273:H371–H379
Sachais BS (2001) Platelet–endothelial interactions in atherosclerosis. Curr Atheroscler Rep 3:412–416
Schnorbus B, Schiewe R, Ostad MA et al (2010) Effects of pentaerythritol tetranitrate on endothelial function in coronary artery disease: results of the PENTA study. Clin Res Cardiol 99:115–124
Shanker G, Kontos JL, Eckman DM et al (2006) Nicotine upregulates the expression of P2Y12 on vascular cells and megakaryoblasts. J Thromb Thrombolysis 22:213–220
Solheim S, Pettersen AA, Arnesen H, Seljeflot I (2006) No difference in the effects of clopidogrel and aspirin on inflammatory markers in patients with coronary heart disease. Thromb Haemost 96:660–664
Steinhubl SR, Badimon JJ, Bhatt DL et al (2007) Clinical evidence for anti-inflammatory effects of antiplatelet therapy in patients with atherothrombotic disease. Vasc Med 12:113–122
Waehre T, Damas JK, Pedersen TM et al (2006) Clopidogrel increases expression of chemokines in peripheral blood mononuclear cells in patients with coronary artery disease: results of a double-blind placebo-controlled study. J Thromb Haemost 4:2140–2147
Warnholtz A, Ostad MA, Heitzer T et al (2005) Effect of tirofiban on percutaneous coronary intervention-induced endothelial dysfunction in patients with stable coronary artery disease. Am J Cardiol 95:20–23
Warnholtz A, Ostad MA, Velich N et al (2008) A single loading dose of clopidogrel causes dose-dependent improvement of endothelial dysfunction in patients with stable coronary artery disease: results of a double-blind, randomized study. Atherosclerosis 196:689–695
Warnholtz A, Wild P, Ostad MA et al (2009) Effects of oral niacin on endothelial dysfunction in patients with coronary artery disease: results of the randomized, double-blind, placebo-controlled INEF study. Atherosclerosis 204:216–221
Wihlborg AK, Wang L, Braun OO et al (2004) ADP receptor P2Y12 is expressed in vascular smooth muscle cells and stimulates contraction in human blood vessels. Arterioscler Thromb Vasc Biol 24:1810–1815
Williams PC, Coffey MJ, Coles B et al (2005) In vivo aspirin supplementation inhibits nitric oxide consumption by human platelets. Blood 106:2737–2743
Acknowledgments
We are indebted to Mr. Fresenius from the GCP pharmacy of the Johannes Gutenberg-University Medical Center for the accurate preparation of the blinded study drug. We acknowledge the excellent technical assistance of Mrs. K. Havliczek and Mrs. H. Seiler. This study was financially supported by Bristol-Myers Squibb.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ostad, M.A., Nick, E., Paixao-Gatinho, V. et al. Lack of evidence for pleiotropic effects of clopidogrel on endothelial function and inflammation in patients with stable coronary artery disease: results of the double-blind, randomized CASSANDRA study. Clin Res Cardiol 100, 29–36 (2011). https://doi.org/10.1007/s00392-010-0199-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-010-0199-6