Abstract
An increasing amount of evidence points to the possibility that gestational and early childhood vitamin D deficiency [25(OH)D < 40 ng/ml] cause some cases of autism. Vitamin D is metabolized into a seco-steroid hormone that regulates about 3% of the 26,000 genes in the coding human genome. It is also a neurosteroid that is active in brain development, having effects on cellular proliferation, differentiation, calcium signaling, neurotrophic and neuroprotective actions; it also appears to have an effect on neurotransmission and synaptic plasticity. Children who are, or who are destined to become, autistic have lower 25(OH)D levels at 3 months of gestation, at birth and at age 8 compared to their unaffected siblings. Two open label trials found high dose vitamin D improves the core symptoms of autism in about 75% of autistic children. A few of the improvements were remarkable. The vitamin D doses used in these children were 300 IU/KG/day up to a maximum of 5000 IU/day (highest final 25(OH)D level reached was 45 ng/ml). The other study used 150,000 IU/month IM as well as 400 IU/day [highest final 25(OH)D level was 52 ng/ml]. These two open label trials were recently confirmed with a randomized controlled trial (RCT) using 300 IU/kg/day with a maximum of 5000 IU/day and resulted in effects similar to the two open label studies. In terms of prevention, a recent small study showed vitamin D supplementation during pregnancy (5000 IU/day) and during infancy and early childhood (1000 IU/day) significantly reduced the expected incidence of autism in mothers who already had one autistic child from 20% to 5%. Vitamin D is safe; for example, over the last 15 years, Poison Control reports there have been approximately 15,000 cases of vitamin D overdose. However only three of these 15,000 people developed clinical toxicity and no one died. Given those facts, practitioners might consider treating autism with 300 IU/kg/day, and seek to prevent autism by supplementing pregnant and lactating women (5000 IU/day) and infants and young children (150 IU/kg/day) checking 25(OH)D levels every 3 months. These doses will increase 25(OH)D blood levels to those recommended by the Endocrine Society. As the American Academy of Pediatrics recommends vitamin D supplementation during infancy and childhood, pediatricians and family practitioners should evaluate the current evidence on autism and vitamin D and act accordingly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
An epidemic of autism appears to be underway in the United States, reminiscent of another epidemic that swept Europe 250 years ago, with young children as the almost exclusive victims of its devastating effects [1, 2]. That earlier disease was vitamin D deficient rickets. Until recently it was an almost unheard of condition among children in affluent countries. Now the prevalence of rickets is rapidly growing in the United States as evidenced by findings reported in the Mayo Clinic Proceedings [3].
The other disease that is rapidly growing is autism spectrum disorder [ASD or autism], which is a common neurodevelopmental disorder characterized by impaired communication and repetitive behaviors. It has recently shown a dramatically increased prevalence, (see Fig. 1) caused by either improved surveillance, diagnostic substitution, over-diagnosis and/or a true increase in prevalence. ASD is now diagnosed in 1 of every 64 American 8-year-old children according to the CDC. Scientists are desperately searching for something that will both reduce the incidence of, and effectively treat, the core symptoms of ASD [4].
Increase is the prevalence of ASD in Indiana School from 1998 to 2016. (https://www.iidc.indiana.edu/pages/increasing-incidence-of-autism-spectrum-disorders-continues-in-indiana) open access
The cause (s) of most autism is unknown. Multiple genetic and environmental factors have been hypothesized as possible etiologies, but nothing exists to prevent or treat the core symptoms of the disorder. This paper will make the case that vitamin D deficiency, in utero and in early childhood, may be the cause of a significant percentage of ASD. In 2008 Cannell hypothesized, using epidemiological and in vitro data, that vitamin D deficiency [25(OH)D < 40 ng/ml as defined by the Endocrine Society], in pregnant women and children is an important cause of some ASD [5]. In 2013, he hypothesized that high doses of vitamin D would improve the core symptoms of autism in some children [6].
2 Epidemiology
What is causing this dramatic increase in autism? One can get clues from epidemiological data. Studies show autism is more common in urban than rural areas, [7] in cloudy and rainy areas, [8] in areas that get the least solar UVB [9] and in areas with high air pollution [10]. As buildings, rain and clouds all reduce surface UVB (UVB is that spectrum of sunlight that triggers vitamin D production in the skin), these data are all consistent with a vitamin D theory [11].
Does the vitamin D theory explain the multiple studies showing air pollution is associated with autism? [10, 12, 13] It is clear that air pollution dramatically reduces vitamin D produced from UVB in sunlight [14, 15]. Furthermore, if air pollution caused autism, wouldn’t the epidemic have occurred during the 1950s and 60s, when air pollution was much worse?
The U.S. government has not always recommended sun avoidance for infants and toddlers. In 1931, the US government advised mothers to make sure their infants were exposed to sunlight frequently enough to get a suntan. [16] Infants today, if they go into the sun, are usually covered in sunblock. Likewise, toddlers avoid sunlight. [17] To make matters worse, infants today are mostly weaned on unfortified fruit juice [18]. In the 1960s, infants were weaned on vitamin D enriched milk and mothers were advised to make sure their children got “fresh air and sunshine.”
It is not only air pollution and cloudy weather, but seasonal factors, migration of dark-skinned immigrants to poleward latitudes, birth order, gestational diabetes, preeclampsia, caesarean section, autoimmune disease in the family and nutrition are associated with autism [19, 20]. All of the above risk factors can be explained by vitamin D, for example the mother’s vitamin D levels are surely depleted by multiple pregnancies and lactation; the recurrence risk for familial ASD is 14.4% for an inter-birth interval of 18 months or less, compared with 6.8% for an interval of 4 years or more [21]. Likewise, gestational vitamin D deficiency was associated with a 2.66-fold risk for gestational diabetes [22] and in utero exposure to gestational diabetes mellitus give children a 4.4 adjusted odds ratio for ASD [23]. Caesarean section increases the risk of autism [24], and low maternal vitamin D increase the risk of C-sections up to four fold (which, in 2009, were at an all-time high of 32% of all deliveries) [25]. Also, there is some evidence for several different comorbidities of ASD [26], such as seizures and GI problems (constipation and diarrhea) may be helped with vitamin D [27, 28].
If fetuses and infants destined to become autistic have low levels of vitamin D in their brains, it is interesting that an experiment of nature gives us an opportunity to see the personality of individuals whose brains contain pathologically large amount of vitamin D in utero and infancy, which occurs in the Williams syndrome [29, 30]. These children have long been known as having an “un-autistic” personality; recent research confirms these children are social, outgoing and gregarious [31], a personality that is the opposite of autism.
A resurgence of vitamin D deficiency due to sun avoidance may now be threatening our children’s health, as well as that of most adults. [32, 33] A 2015 Dutch study of 6100 young children found only 33% had 25(OH)D > 20 ng/ml. (The Endocrine Society recommends 40–60 ng/ml.) Even among professional basketball players, the prevalence of 25(OH)D < 30 ng/ml is 79% [34]. But according to several respected leaders in child and adult nutrition from across the United States, the current increase in autism spectrum disorders (ASD) may well be a direct consequence of significant vitamin D deficiencies in pregnant women as well as their infants and toddlers, as outlined in an comprehensive and excellent recent review in Nutrients [35]. This insidious deficiency is readily remedied – yet tragically ignored.
We know that certain autoimmune brain diseases, such as multiple sclerosis, are much more common in high latitudes where sunlight is scarce, and many scientists suspect that those conditions are directly related to chronic or seasonal vitamin D deficiencies. Significant positive association between latitude and the prevalence of autism has recently been reported [35]. A 2013 study confirmed that children who live in low UVB light have almost three times the prevalence of ASD compared to children who live in sunny areas. [9].
One might expect that babies born in late winter would have higher rates of autism if vitamin D deficiency were involved, since their mothers would have spent most of their pregnancies in fairly low-sunlight settings. One detailed review of this topic concluded most studies find a late winter increase in autism births. [35].
If adequate amounts of vitamin D prevent autism, one would expect children with rickets to have an increased risk of autism. At least two old papers addressed it, [36, 37] both published before Kanner described autism in 1943. Both papers describe “weak mindedness,” “feeble minds,” “mental dullness,” “odd introverted behavior,” unresponsiveness and developmental delays [38]. Even more intriguing, both papers report that the mental condition in rachitic children improved with vitamin D treatment. More recently, a 2015 study of 35 rachitic children found 25% of the rachitic children also have autism as detected by standardized autism ratings scales [39].
What is undeniable is that there has been a marked increase in the number of children being diagnosed with autism over the past 3 decades [13], (see Fig. 1 below), which show the prevalence of ASD in Indiana schools over last 14 years. Most agree that some of the increase is real and probably represents an interaction between genes and an unknown “environmental factor.” [40] Some make the case that that the “environmental factor” might be air pollution, alcohol, mercury, pesticides or obesity, fatty acids, endocrine disrupting chemicals [41] and others [42]. However, take for example, obesity, which has increased in unison over time with autism and indeed obesity, especially paternal obesity, is a risk factor for autism. [43] However, obesity is also a risk factor for vitamin D deficiency; the prevalence of vitamin D deficiency was 35% higher in obese subjects compared to the normal weight group. [44] Likewise mercury, which can certainly impair brain function, is removed from the body by glutathione in 3 different ways [45]. And, as we will see, vitamin D significantly up-regulates glutathione.
In a mostly white cohort in Iowa, 70% of 4-month-old breastfed infants had mean 25(OH)D < 12 ng/ml (ideal range 40–60 ng/ml) [46]. The prevalence of severe vitamin D deficiency was 50% in summer and 79% in the winter. Fifty-seven percent of infants who were followed for six months still had vitamin D deficiency. In another study from Cincinnati, 18% of exclusively breastfed infants aged 1 month had vitamin D levels <10 ng/ml (in the rachitic range); 76% of the infants and 17% of their mothers had serum 25(OH)D < 20 ng/ml (ideal range 40–60 ng/ml). [47].
Levels of vitamin D in most people in modern industrialized countries are known to be much lower than those of fully sun-exposed individuals [48]. Thus, our behavior has had the paradoxical and unintended consequence of reducing our children’s levels of a vital neurosteroid hormone that, in turn, can influence the very organ of behavior itself, the brain.
The sun phobia and dramatic increase in sunblock use [49] is mainly the result of the 1989 American Medical Association Council on Scientific Affairs report, which warned Americans against sun exposure, but did not include a word about vitamin D [50]. The AMA did not recommend that Americans take vitamin D supplements to make up for what the sun was no longer making in the skin. In fact, in 2001, researchers at the Centers for Disease Control reported that most children were “adequately protected” from sunlight.” [51] That is, the sun scare worked. Couple this with our movement from playing outside to playing video games, and the fear modern mothers have to let their child roam around the neighborhood, and you have the perfect storm for the development of vitamin D deficiency in infancy and toddlerhood.
3 Mechanisms of action
The possible mechanisms of action that explain vitamin D helping prevent and treat ASD have recently been extensively reviewed [52–54]. They include reducing risk and severity inflammatory cytokines through it anti-inflammatory effects in the brain, (For example, Huang et al., recently concluded that calcitriol can be used to alleviate neuro-inflammation (mainly caused by oxidants and toxins [55]). Calcitriol also enhances DNA repair mechanisms, has anti-autoimmune effects, raises seizure threshold, increases T-regulatory cells, protects neural mitochondria and up-regulates glutathione, the master antioxidant, which scavenges oxidative by-products [6, 56]. (see below) Another mechanism is through vitamin D’s effect on serotonin via direct genetic regulation of serotonin’s rate limiting enzymes, both peripheral tryptophan hydroxylase TPH1 and central TPH2. Activated vitamin D (a steroid hormone) down-regulates peripheral TPH1, while up-regulating central TPH2, thus explaining the serotonin paradox in ASD in which peripheral serotonin is increased but central serotonin is decreased [57].
Autistic individuals have abnormalities in immune functions similar to those affected by vitamin D deficiency, such as increased inflammatory cytokine levels [19]. And we know that much of the ongoing inflammation in autistic brains is the result of oxidative stress, [58, 59] just where vitamin D”s powerful anti-inflammatory properties are most useful (and most critical) [60]. Regardless of the cause of the autoimmune inflammatory state, vitamin D supplementation of the infants and children is very likely to help because vitamin D up-regulates production of dendritic (peacemaker) lymphocytes that reduce the intensity of autoimmune attack by up-regulating interleukin-10, an anti-inflammatory cytokine [61].
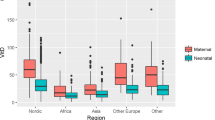
Activated vitamin D hormone (calcitriol) protects brain tissue by reducing inflammatory cytokine levels [62], which, when elevated, are strongly associated with cognitive impairment in ASD. [63] Calcitriol also protects brain tissue by stimulating production of neurotropins, chemicals that combat toxicity from several sources, including toxic levels of intracellular calcium [64]. Very recently, a RCT found vitamin D (4000 IU/day), in a dose dependent manner, significantly increased total antioxidant capacity and total glutathione (the master antioxidant) levels in pregnant diabetic women (P < 0.01) [65]. See Fig. 2.
We now understand that the seco-steroid downstream metabolite of vitamin D, 1,25 (OH)2D (calcitriol), is a neurosteroid hormone, directly responsible for many elements of brain development and behavior and those vitamin D dependent elements appear to be disrupted in autism. Other examples of neurosteroids include derivatives of estrogen, [66] testosterone [67] and cortisol [68], which have effects on many brain systems. Orally ingested vitamin D is actually a pro-pre-hormone, which must be metabolized by the liver into 25-hydroxy vitamin D [25(OH)D], which then forms calcitriol, the potent neurosteroid that helps control brain cell growth, and acts on vitamin D receptor molecules found in most brain cells from the very first days of embryo formation [69].
The calcitriol neurosteroid hormone system is different from all the body”s other steroid hormone systems. While other steroid hormones are produced endogenously directly from the body”s own natural store of precursor compounds (cholesterol) the amount of calcitriol produced is completely dependent on 25(OH)D availability, which, in turn, entirely depends on vitamin D, which entirely depends on our behavior. No other steroid hormone is so dependent on human behavior.
So human behavior, be it the step into the sun, the step to the supplements, the step into the shade, or the step to the sunscreen, directly determine brain calcitriol levels. In the case of the human fetus, the vitamin D neurosteroid calcitriol is directly linked to very early cognitive development; its presence appears to have important implications for the developing baby”s brain [35].
4 Genetics
Genetic factors in the etiology of ASD are very important, as demonstrated by high rates of concurrence in other family members, particularly in twin studies; there is an excellent recent review of the genetics of ASD [70]. Today’s consensus, such as it is, posits that an interaction between genetic and environmental factors causes most ASD. [40] What is not generally known is that a meta-analysis of 11 studies found children with ASD have much lower 25(OH)D levels than do controls. [71] That these differences may be genetic is supported by the fact that 25(OH)D levels of 1st trimester mothers - destined to have a child with autism - are significantly lower than their unaffected siblings and that autistic individuals have significantly lower 25(OH)D at birth (both discussed in detail below).
A recent study showed ASD is strongly associated with polymorphisms of the genes that code for the vitamin D receptor, which are associated with both lower vitamin D levels and ASD [72]. Others have found that a number of polymorphisms of the genes of vitamin D’s metabolic pathway are associated with ASD severity (odds ratio up to 6) [73]. Common vitamin D metabolic polymorphisms predict significantly lower vitamin D levels in healthy Danish children and adults [74].
Also, in a study of siblings who were discordant for ASD, researchers found that the ASD siblings had lower 25(OH)D levels at birth, showing ASD individuals are born with significantly lower vitamin D levels. [75] A recent larger study found pregnant women with 25(OH)D < 10 ng/ml in the first trimester had a two fold higher risk for ASD without mental impairment but a six fold higher risk exits for immigrant vitamin D deficient mothers. [76] A recent study of 4229 women found those with 25(OH)D < 10 ng/ml in mid-gestation and at birth had children with twice the risk of autistic traits as women who had levels >20 ng/ml (mid-gestation n = 2866, β = 0.06, P < 0.001; cord blood n = 1712, β = 0.03, P = 0.01) [77].
Very recently, researchers in China found the lowest quartile of 25(OH)D levels of women in their first trimester were associated with a fourfold risk of ASD in the subsequent offspring [78]. In the same study, higher levels of 25(OH)D were associated with decreasing severity of ASD (R = −0.302, P = 0.001). Maternal 25(OH)D in the lower 3 quartiles [1–3] compared to the highest quartile [4] was associated with increased odds of ASD diagnosis in offspring: [Odds Ratio (OR), Q1: OR =3.99, (P = 0.001); Q2: OR =2.68, (P = 0.006); Q3: OR =1.36, (P = 0.25)].
The above studies imply that at least some of the genes that code for vitamin D’s metabolic pathways interact with vitamin D in the environment to influence the ASD phenotype. Ambient vitamin D overcomes genetic influences as evidenced by a study of 510 Vietnamese twins. [79] In this study, the heritability of 25(OH)D was found to be 70% in the winter (other studies have found a lower heritability) but during the summer 25(OH)D became 100% environmentally determined due to sunshine.
It appears likely that vitamin D is both the long sought environmental and genetic factor that interacts with the environment to determine some ASD phenotypes. If one is born with the genetic tendency for ASD, that tendency may interact with environmentally or genetically determined low 25(OH)D, as the above studies imply. The result of such inheritance is low 25(OHD, starting in the first trimester, continuing at birth and early childhood, as shown by the decreased 25(OH)D levels in ASD children. It is important to point out that most fetuses and infants and toddlers with low vitamin D levels will not get autism; one still needs the genetic predisposition. For those who do, the clinical trials below imply that high dose vitamin D during gestation (enough to obtain 25(OH)D between 40 and 60 ng/ml) and during infancy and early childhood (40–60 ng/ml) may prevent most ASD by overcoming the significant heritability of 25(OH)D levels.
5 Male/female ratio in autism
The fact that vitamin D metabolism differs markedly under the effects of the sex hormones may go a long way towards explaining yet another puzzling fact about autism, namely its strong predilection for boys over girls. For example, researchers in Sweden have shown that estrogen has effects on developing brain tissue that serve to make it more responsive to the neuro-hormonal growth-stimulating effects of calcitriol – results which suggest that estrogen can enhance the beneficial effects of vitamin D on the brain [80]. Injection of estrogen in quall resulted in significant increases of calcitriol. [81] Women taking estrogen have 20% higher 25(OH)D as do controls [82]. At the same time, testosterone significantly inhibits CYP27B1 (the gene that activates vitamin D) while stimulating CYP24A1 (the gene that degrades calcitriol) expression in cultured trophoblasts [83].
Though complex, these studies do support the notion that the developing brain of a female fetus, with its higher estrogen levels, could make more efficient use of available vitamin D than would the brain of a male fetus, with its higher testosterone levels. In a situation where there was plenty of vitamin D present, such differences would go unnoticed - but introduce the all-too-prevalent maternal and early childhood vitamin D deficiency states, and, for some, the stage is set for ASD in boys but a lower incidence in girls, which is of course precisely the situation we see with autism”s gender discrimination.
6 Interventional studies
A recent propionic acid induced toxic rat model of ASD reported that vitamin D, in amounts comparative to high-dose human ones, exerted both a significant protective and treatment effect, with the protective effect more robust than the treatment effect [84].
A case report in Pediatrics described a child with both rickets and autism. Remarkably, his autism essentially went away after his rickets was treated with 150,000 IU/month IM as well as 400 IU/day PO. [85] A 3-month Egyptian open study of 122 subjects with ASD, found serum 25(OH)D levels were inversely correlated with severity on the Childhood Autism Rating Scale (CARS) with (R = 0.5 and p < 0.001) [86]. This open label trial of high-dose vitamin D (300 IU/kg/day up to a maximum of 5000 IU/day) in 83 of those 122 subjects with ASD found significant clinical improvement (mean CARS went from 37 to 30). Approximately 75% of the 83 supplemented ASD children improved (P < 0.05) with no evidence of toxicity. In fact, the highest 25(OH)D level in these children after 3 months of 300 IU/kg/day was 45 ng/ml (range 30–100 ng/ml). The five ASD children whose final 25(OH)D was >40 ng/ml had the most robust improvement on the CARS.
It is important to point out that the CARS has limitations. Scores depend on clinical judgment and it is no better than the sample studied. Unlike CARS2, which involves parental input, CARS generally does not. Like the rest of us, autistic children may have good days and bad days, which will affect the CARS.
Another open label study of 37 children aged 3–11 years with ASD were treated for 3 months with large bolus doses (150,000 IU/month given intramuscularly) together with 400 IU/day by mouth). They found significant vitamin D treatment effects in ASD on standardized rating scales, again with no evidence of toxicity [87]. The mean baseline level of the treatment group was 21 ng/ml. After three [3] months of high dose vitamin D, their mean 25(OH)D was 41 ng/ml with the highest level at 55 ng/ml. Significant improvement was found on the Autism Behavior Checklist (P = 0.038) and the CARS (P = 0.016).
Yet another open label trial of 11 children with ASD studied changes in neurotropic factors as well as changes in the Autism Behavior Checklist after administration of varying amounts of vitamin D. Only small doses of vitamin D were given and 25(OH)D > 20 ng/ml was considered adequate. Nonetheless, a significant treatment effect on standardized scales was found [88].
The first and only randomized controlled trial (RCT), which studied 109 ASD children ages 3–10 using 300 IU/kg/day up to a maximum of 5000 IU/day has been published in a 2016 edition of the Journal of Childhood Psychology and Psychiatry [89]. In this study all autistic children with 25(OH)D < 20 ng/ml were excluded from the study for ethical reasons and treated with vitamin D. Baseline 25(OH)D of the remaining 109 study children (mean age 5.4 years) was around 27 ng/ml in both arms of the study (the FNB says >20 ng/ml is adequate). After the 4-month study, mean 25(OH)D in the treatment group was 47 ng/ml and was unchanged in the placebo arm. The highest 25(OH)D obtained during this “high dose” treatment was 55 ng/ml, range: (40–60 ng/ml). In a per protocol analysis, the total CARS scores significantly decreased (improved) in the vitamin D group while the placebo group remained unchanged (mean treatment CARS ± SD; 30.3 ± 5.9 versus placebo 36.4 ± 6; p = <0.001 respectfully), again with no evidence of toxicity. Younger children responded better than older children.
This RCT, if duplicated, has a number of implications. First, the treated ASD children had 25(OH)D levels that are considered normal by many people. Second, the fact that high dose vitamin D helped some of the treated children, may imply that traditional doses (600 IU/day) will have little or no effect. Third, some of the children (about 25%) did not respond at all, supporting the belief that autism is a multifactorial disease. However, it may be that severe vitamin D deficiency in utero causes a phenotype that cannot be rescued by postnatal vitamin D.
In terms of prevention, an open label study of 20 infants born to mothers who already had one child with ASD, found 5000 IU/day of vitamin D given to the pregnant mothers and 1000 IU/day to the resultant child up to the age of 3 years reduced subsequent ASD incidence to 5% instead of the 20% rate consistently reported in the literature for mothers who already had one or more autistic children [90]. The two children (5%) who developed autism in spite of the treatment each had mild autism with only one of two autism scales positive, and may have responded to higher doses during age 2 and 3. For example, the 300 IU/kg/day dose, as used above in the interventional studies, would be 4500 IU/day for a 15 kg 3-year-old.
7 Dose of vitamin D that may help autism
There is a lot of controversy about what 25(OH)D levels are ideal, with the 2010 Food and Nutrition Board stating levels above >20 ng/ml is adequate. However, the Endocrine Society says levels of 40–60 ng/ml are ideal, which may require doses pediatricians are not comfortable with. Also, in the RCT above the treatment children had 27 ng/ml at baseline. In the past, adequate vitamin D levels have been defined with a biomarker, parathyroid hormone, which tends to be elevated when 25(OH)D levels are low with a flexion point at 20 ng/ml.
However, there is a better biomarker: the 25(OH)D blood levels lactating mothers need to provide substantial amounts of vitamin D in their breast milk for their suckling infants. That level appears to be 40 ng/ml and, for the average lactating woman, requires at least 6600 IU/day for the sucking infant to achieve >30 ng/ml [91]. The amount of vitamin D intake required for infants to achieve a 25(OD)D level greater than 40 ng/ml is unknown.
The fact that most human breast milk has little to negligible vitamin D is odd as most of us think of breast milk as the perfect food. This paradox is probably of our own making and is because the vast majority of lactating women are vitamin D deficient. The problem is so widespread that Danish authors, after studying the D content of breast milk, recently reported that exclusively breastfed infants receive <25% (110 IU/day) of the daily dose of vitamin D recommended by the Food and Nutrition Board (FNB) during the first year of life [92].
Levels of vitamin D in most indoor workers in modern industrialized countries are known to be much lower than those of fully sun-exposed individuals. Thus, our behavior has had the paradoxical and unintended consequence of reducing our children’s levels of a vital neurosteroid hormone that, in turn, can influence the very organ of behavior itself, the brain. In fact, it may take 10,000 IU per day for lactating women for their suckling infants to obtain levels between 40 and 60 ng/ml, levels the Endocrine Society recommends.
Large populations of pregnant women putting small amounts of vitamin D in their mouths – in the form of prenatal vitamins (400 - 600 IU) – instead of generating large amounts in their skins, is novel to human brain development [5]. Since we no longer receive as much sun exposure as we did 3–4 decades ago, we need to either go back into the sun or pay closer attention to how much vitamin D we to get orally. 25(OH)D levels have been falling [93] as sun protection for children has been increasing [94].
The case for high dose oral supplementation (5000–10,000 IU/day) for healthy adults is made when one considers that skin production of vitamin D is so remarkable and robust. In fact, just 20 min of summer sunbathing (10 min on each side) at solar noon by a fair-skinned adult, produces about 20,000 units of vitamin D within 24 h [95]. To get the same amount orally, a pregnant woman would have to drink 200 glasses of milk at 100 IU per glass (and risk fluid intoxication) or take 50 standard prenatal multivitamins, which usually contain 400 IU per tablet, (and risk vitamin A intoxication) to receive the same input as the sun.
Obviously, infants, toddlers and children need adequate vitamin D, although we do not know what that is. It may simply be whatever dose is required to obtain levels between 40 and 60 ng/ml.
8 Summary
There seems to be little doubt that at least some of the increase in autism over the last 25 years is real, and not just a result of over-reporting and over-diagnosis by anxious parents and physicians. There’s equal certainty that we also face an epidemic of vitamin D deficiency as we steadily move away from old ways that exposed us to more vitamin D producing sunlight.
The vitamin D theory of some cases of autism has significant support as outlined above. Several reviews on autism and vitamin D have been recently published. For example, in an exhaustive and excellent review, Mazahery et al. concluded that, until more data are available, practitioners should consider vitamin D as a possible preventive and treatment measure for ASD [35]. Wang et al., in a meta-analysis of 25(OH)D levels in ASD, concluded that the reduced vitamin D levels in autistic children may have clinical consequences and that all children with ASD should have their 25(OH)D level checked and supplemented if low [71]. Kočovská et al., in a family study, showing autistic children have lower 25(OH)D levels than their first degree relatives, concluding that low vitamin D levels may be involved in aberrant brain development leading to autism [56]. Finally, Patrick and Ames, writing in FASEB, concluded that vitamin D is necessary for normal brain development and that vitamin D deficiency is probably the main cause of autism [57].
To my knowledge, only one randomized controlled trial is currently underway (using a small dose of only 2000 IU/day), which will leave many autistic individuals with 25(OH)D < 40 ng/ml. The above studies suggested the best treatment effect is with a 25(OH)D levels in the 40 ng/ml range. The 2000 IU/day ongoing study may be enrolling older autistic subjects, which may be a problem as weight is a main determinate of dose response [96].
We desperately need more studies that adequately supplement pregnant women and their children such as those by Hollis and Wagner. [97–99] Future studies of pregnancy and lactation should not use Food and Nutrition Board (FNB) doses. FNB dose recommendations are to advise an individual not under a physician’s care the dose to take, on his/her own, to prevent rickets and osteomalacia. The FNB went out of its way to stress that when patients are under a doctor’s (or researcher’s) care, they were free to use whatever dose they thought appropriate. Nor do the FNB recommendations constrain the American Academy of Pediatrics or the Congress of Obstetricians and Gynecologists. Like the Endocrine Society, these organizations are free to come up with their own recommendations.
While we are awaiting further RCTs, it seems prudent to maximize vitamin D status in pregnant women, lactating women, infants and young children, as the Endocrine Society recommends, aiming for levels found in humans living in a sun-rich environment (46 ng/ml) [100].
To prevent autism, pregnant and lactating women may have to take up to 10,000 IU/day to get their 25(OH)D above 40 ng/ml [99, 101]. Children, from infants at the breast to 3-year old toddlers to 6-year-old first graders, may have to take 150 IU/lb/day not to exceed 5000 IU/day unless regular 25(OH)D levels are obtained. This means that to try to prevent (not treat) autism, a 20-lb child should take 2000 IU/day and a nursing infant about 1000 IU/day. If the lactating mother is taking 10,000 IU/day, the infant will get all the vitamin D it needs from their mother’s milk but the infant should take 1000 IU/day right after weaning. We know these preventative doses are safe from the above controlled trials, which used twice the dose but only obtaining midrange 25(OH)D levels.
To treat individuals with autism with vitamin D, it may be sensible to choose a dose we know works, that being 300 IU/kg/day with a maximum of 5000 IU/day.
The open study [(Saad et al.) [86] above reports that only 5 children exceeded levels of 40 ng/ml at the end of the study, and the authors noted that those 5 children responded best to treatment. Even the unusual dosage regimen used in China to treat autism (150,000 IU/month delivered intramuscularly combined with 400 IU/day PO for 3 months) did not result in toxicity, with the highest 25(OH)D level at 52 ng/ml. Perhaps future RCTs need to be individualized, checking 25(OH)D every two months and adjusting the dose accordingly until all children are between the 40–60 ng/ml range the Endocrine Society recommends.
The American Academy of Pediatrics (AAP) recommends all healthy infants up to the age of one year take 400 IU/day (10 mcg) of vitamin D and 600 IU/day (15 mcg) after the first birthday to prevent rickets. This dose may help prevent some autism but is much lower than the dose used above in the Stubbs et al. preventative study. However, research has shown that about 70% of American toddlers do not take any vitamin D at all, despite the AAP recommendation [102]. Also, only 20% of American infants get the paltry 400 IU/day the AAP recommends [103]. It is unknown if parents simply ignore the pediatrician’s advice or if pediatricians are forgetting to recommend vitamin D supplements for infants and toddlers.
The scientific data that vitamin D will prevent or help treat autism is preliminary. However, that does not relieve practitioners from using all current available scientific evidence to make a risk benefit analysis of whether or not to treat or supplement their patients with vitamin D up to 40 - 60 ng/ml, the levels recommended by the Endoccrine Society.
Abbreviations
- 25(OH)D:
-
25-hydroxyvitamin D
- ASD:
-
autism spectrum disorder
- CARS:
-
Childhood Autism Rating Scale
- Calcitriol:
-
1,25(OH)D2
References
Larocque R. Deaths at an early age in the city of Quebec, 17th-19th centuries. Can Bull Med Hist. 1999;16:341–61.
Holick MF. Resurrection of vitamin D deficiency and rickets. J Clin Invest. 2006;116:2062–72.
Thacher TD, Fischer PR, Tebben PJ, Singh RJ, Cha SS, Maxson JA, Yawn BP. Increasing incidence of nutritional rickets: a population-based study in Olmsted County. Minnesota Mayo Clin Proc. 2013;88(2):176–83.
Bhat S, Acharya UR, Adeli H, Bairy GM, Adeli A. Autism: cause factors, early diagnosis and therapies. Rev Neurosci. 2014;25(6):841–50. doi:10.1515/revneuro-2014-0056. Review
Cannell JJ. Autism and vitamin D. Med Hypotheses. 2008;70(4):750–9.
Cannell JJ. Autism, will vitamin D treat core symptoms? Med Hypotheses. 2013;81(2):195–8.
Williams JG, Higgins JP, Brayne CE. Systematic review of prevalence studies of autism spectrum disorders. Arch Dis Child. 2006;91(1):8–15.
Waldman M, Nicholson S, Adilov N. Does television cause autism? National Bureau of Economic Research Working Group. 12632. 2006. http://www.nber.org/papers/w12632. Accessed 1/19/2017.
Grant WB, Cannell JJ. Autism prevalence in the United States with respect to solar UV-B doses: an ecological study. Dermatoendocrinol. 2013;5(1):159–64.
Windham GC, Zhang L, Gunier R, Croen LA, Grether JK. Autism spectrum disorders in relation to distribution of hazardous air pollutants in the San Francisco bay area. Environ Health Perspect. 2006;114(9):1438–44.
Wai KM, Yu PK, Lam KS. Reduction of solar UV radiation due to urban high-rise buildings--a coupled Modelling study. PLoS One. 2015;10(8):e0135562.
Vieira SE. The health burden of pollution: the impact of prenatal exposure to air pollutants. Int J Chron Obstruct Pulmon Dis. 2015;10:1111–21.
Agarwal KS, Mughal MZ, Upadhyay P, Berry JL, Mawer EB, Puliyel JM. The impact of atmospheric pollution on vitamin D status of infants and toddlers in Delhi. India Arch Dis Child. 2002;87:111–3.
Kelishadi R, Moeini R, Poursafa P, Farajian S, Yousefy H, Okhovat-Souraki AA. Independent association between air pollutants and vitamin D deficiency in young children in Isfahan. Iran Paediatr Int Child Health. 2014;34(1):50–5.
Baïz N, Dargent-Molina P, Wark JD, Souberbielle JC, Slama R, Annesi-Maesano I. EDEN mother-child cohort study group. Gestational exposure to urban air pollution related to a decrease in cord blood vitamin d levels. J Clin Endocrinol Metab. 2012;97(11):4087–95.
https://www.vitamindcouncil.org/wp-content/uploads/2012/03/Sunlight-for-Babies.pdf. Accessed 1–21-2017.
Gies P, Makin J, Dobbinson S, Javorniczky J, Henderson S, Guilfoyle R, Lock J. Shade provision for toddlers at swimming pools in Melbourne. Photochem Photobiol. 2013;89(4):968–73.
Walker RB, Conn JA, Davies MJ, et al. Mothers’ views on feeding infants around the time of weaning. Public Health Nutr. 2006;9(6):707–13.
Szachta P, Skonieczna-Żydecka K, Adler G, Karakua-Juchnowicz H, Madlani H, Ignyś I. Immune related factors in pathogenesis of autism spectrum disorders. Eur Rev Med Pharmacol Sci. 2016;20(14):3060–72.
Liu L, Zhang D, Rodzinka-Pasko JK, Li YM. Environmental risk factors for autism spectrum disorders. Nervenarzt. 2016. Review.
Risch N, Hoffmann TJ, Anderson M, Croen LA, Grether JK, Windham GC. Familial recurrence of autism spectrum disorder: evaluating genetic and environmental contributions. Am J Psychiatry. 2014;171(11):1206-13. doi:10.1176/appi.ajp.2014.13101359.
Zhang C, Qiu C, Hu FB, David RM, van Dam RM, Bralley A, Williams MA. Maternal plasma 25-hydroxyvitamin D concentrations and the risk for gestational diabetes mellitus. PLoS One. 2008;3(11):e3753.
Nahum Sacks K, Friger M, Shoham-Vardi I, Abokaf H, Spiegel E, Sergienko R, Landau D, Sheiner E. Prenatal exposure to gestational diabetes mellitus as an independent risk factor for long-term neuropsychiatric morbidity of the offspring. Am J Obstet Gynecol. 2016;215(3):380.e1–7.
Curran EA, O'Neill SM, Cryan JF, Kenny LC, Dinan TG, Khashan AS, Kearney PM. Research review: birth by caesarean section and development of autism spectrum disorder and attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. J Child Psychol Psychiatry. 2015;56(5):500–8.
Merewood A, Mehta SD, Chen TC, Bauchner H, Holick MF. Association between vitamin D deficiency and primary cesarean section. J Clin Endocrinol Metab. 2009;94(3):940–5.
Frye RE, Rossignol DA. Identification and treatment of pathophysiological comorbidities of autism Spectrum disorder to achieve optimal outcomes. Clin Med Insights Pediatr. 2016;10:43–56.
Holló A, Clemens Z, Lakatos P. Epilepsy and vitamin D. Int J Neurosci. 2014;124(6):387–93.
Abbasnezhad A, Amani R, Hajiani E, Alavinejad P, Cheraghian B, Ghadiri A. Effect of vitamin D on gastrointestinal symptoms and health-related quality of life in irritable bowel syndrome patients: a randomized double-blind clinical trial. Neurogastroenterol Motil. 2016;28(10):1533–44.
Garabe’dian M, Jacqz E, Guillozo H, et al. Elevated plasma 1,25-dihydroxyvitamin D concentrations in infants with hypercalcemia and an elfin facies. N Engl J Med 1985;312(15):948–952.
Knudtzon J, Aksnes L, Akslen LA, Aarskog D. Elevated 1,25- dihydroxyvitamin D and normocalcaemia in presumed familial Williams syndrome. Clin Genet. 1987;32(6):369–74.
Ng R, Järvinen A, Bellugi U. Toward a deeper characterization of the social phenotype of Williams syndrome: the association between personality and social drive. Res Dev Disabil. 2014;35(8):1838–49.
Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353–73.
Holick MF. Vitamin D deficiency. N Engl J Med 2007;357(3):266–281. Review.
Fishman MP, Lombardo SJ, Kharrazi FD. Vitamin D deficiency among professional basketball players. Orthop J Sports Med. 2016;4(7):2325967116655742.
Mazahery H, Camargo Jr CA, Conlon C, Beck KL, Kruger MC, von Hurst PR. Vitamin D and autism Spectrum disorder: a literature review. Nutrients. 2016;8(4):236.
Hallerhan MM. The effect of rickets on the mental development of young children. Arch Psychol. 1938;229:1–67.
Gilmour A. The mental condition in rickets. School Hygiene. 1912;9:6–16.
Cannell JJ. On the aetiology of autism. Acta Paediatr. 2010;99(8):1128–30.
Zaky EA, et al. Prevalence of Autism Spectrum Disorders in Vitamin D Deficient or Insufficient Rickets IJSR. 2015;4:6.
Chaste P, Leboyer M. Autism risk factors: genes, environment, and gene-environment interactions. Dialogues Clin Neurosci. 2012;14(3):281–92. Review
Koch CA, Diamanti-Kandarakis E. Introduction to endocrine disrupting chemicals--is it time to act? Rev Endocr Metab Disord. 2015;16(4):269–70.
Fujiwara T, Morisaki N, Honda Y, Sampei M, Tani Y. Chemicals, nutrition, and autism Spectrum disorder: a mini-review. Front Neurosci. 2016;10:174.
Surén P, Gunnes N, Roth C, Bresnahan M, Hornig M, Hirtz D, Lie KK, Lipkin WI, Magnus P, Reichborn-Kjennerud T, Schjølberg S, Susser E, Oyen AS, Smith GD, Stoltenberg C. Parental obesity and risk of autism spectrum disorder. Pediatrics. 2014;133(5):e1128–38.
Pereira-Santos M, Costa PR, Assis AM, Santos CA, Santos DB. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Pereira-Santos M, costa PR, Assis AM, Santos CA, Santos DB. Obes Rev. 2015;16(4):341–9.
Patrick L. Mercury toxicity and antioxidants: part 1: role of glutathione and alpha-lipoic acid in the treatment of mercury toxicity. Altern Med Rev. 2002;7(6):456–71. Review
Dawodu A, Wagner CL. Prevention of vitamin D deficiency in mothers and infants worldwide - a paradigm shift. Paediatr Int Child Health. 2012;32(1):3–13.
Dawodu A, Zalla L, Woo JG, Herbers PM, Davidson BS, Heubi JE, Morrow AL. Heightened attention to supplementation is needed to improve the vitamin D status of breastfeeding mothers and infants when sunshine exposure is restricted. Matern Child Nutr. 2014;10(3):383–97.
Vieth R. What is the optimal vitamin D status for health? Prog Biophys Mol Biol. 2006;92:26–32.
http://www.strategyr.com/MarketResearch/Sun_Care_Products_Market_Trends.asp. Accessed 1/23/2017
Council on Scientific Affairs. Harmful effects of ultraviolet radiation. JAMA. 1989;262:380–384.
Hall HI, Jorgensen CM, McDavid K, Kraft JM, Breslow R. Protection from sun exposure in US white children ages 6 months to 11 years. Public Health Rep. 2001;116(4):353–61.
Ali A, Cui X, Eyles D. Developmental vitamin D deficiency and autism: putative pathogenic mechanisms. J Steroid Biochem Mol Biol. 2016. doi:10.1016/j.jsbmb.2016.12.018.
DeLuca GC, Kimball SM, Kolasinski J, et al. Review: the role of vitamin D in nervous system health and disease. Neuropathol Appl Neurobiol. 2013;39(5):458–84.
Cannell JJ, Grant WB. What is the role of vitamin D in autism? Dermatoendocrinol. 2013;5(1):199–204.
Huang YN, Ho YJ, Lai CC, Chiu CT, Wang JY. 1,25-dihydroxyvitamin D3 attenuates endotoxin-induced production of inflammatory mediators by inhibiting MAPK activation in primary cortical neuron-glia cultures. J Neuroinflammation. 2015;12:147.
Kočovská E, Fernell E, Billstedt E, et al. Vitamin D and autism: clinical review. Res Dev Disabil. 2012;33(5):1541–50.
Patrick RP, Ames BN. Vitamin D Hormone regulates serotonin synthesis. Part 1: relevance for autism. FASEB J 2014;28(6):2398–2413.
Smaga I, Niedzielska E, Gawlik M, Moniczewski A, Krzek J, Przegaliński E, Pera J, Filip M. Oxidative stress as an etiological factor and a potential treatment target of psychiatric disorders. Part 2. Depression, anxiety, schizophrenia and autism. Pharmacol Rep. 2015;67(3):569–80.
Cortelazzo A, De Felice C, Guerranti R, Signorini C, Leoncini S, Zollo G, et al. Expression and oxidative modifications of plasma proteins in autism spectrum disorders: interplay between inflammatory response and lipid peroxidation. Proteomics Clin Appl. 2016;10(11):1103-1112. doi:10.1002/prca.201500076.
Gatti D, Idolazzi L, Fassio A. Vitamin D: not just bone, but also immunity. Minerva Med. 2016;107(6):452-460.
Bakdash G, van Capel TM, Mason LM, et al. Vitamin D3 metabolite calcidiol primes human dendritic cells to promote the development of immunomodulatory IL-10-producing T cells. Vaccine. 2014;32(47):6294–302.
Arnson Y, Itzhaky D, Mosseri M, Barak V, Tzur B, Agmon-Levin N, Amital H. Vitamin D inflammatory cytokines and coronary events: a comprehensive review. Clin Rev Allergy Immunol. 2013;45(2):236–47.
Krakowiak P, Goines PE, Tancredi DJ. Ashwood P. Hertz-Picciotto I, et al. Neonatal cytokine profiles associated with autism spectrum disorder. Biol Psychiatry: Hansen RL; 2015.
Wrzosek M, Łukaszkiewicz J, Wrzosek M, Jakubczyk A, Matsumoto H, Piątkiewicz P, Radziwoń-Zaleska M, Wojnar M, Nowicka G. Vitamin D and the central nervous system. Pharmacol Rep. 2013;65(2):271–8. Review
Zhang Q, Cheng Y, He M, Li T, Ma Z, Cheng H. Effect of various doses of vitamin D supplementation on pregnant women with gestational diabetes mellitus: a randomized controlled trial. Exp Ther Med. 2016;12(3):1889–95.
Srivastava DP. Two-step wiring plasticity--a mechanism for estrogen-induced rewiring of cortical circuits. J Steroid Biochem Mol Biol. 2012;131(1–2):17–23.
Höfer P, Lanzenberger R, Kasper S. Testosterone in the brain: neuroimaging findings and the potential role for neuropsychopharmacology. Eur Neuropsychopharmacol. 2013;23(2):79–88.
Payne JD, Nadel L. Sleep, dreams, and memory consolidation: the role of the stress hormone cortisol. Learn Mem. 2004;11(6):671–8. Review
Kesby JP, Eyles DW, Burne TH, McGrath JJ. The effects of vitamin D on brain development and adult brain function. Mol Cell Endocrinol. 2011;347(1–2):121–7.
Shailesh H, Gupta I, Sif S, Ouhtit A. Towards understanding the genetics of Autism. Front Biosci (Elite Ed). 2016;8:412–26.
Wang T, Shan L, Du L, Feng J, Xu Z, Staal WG, Jia F. Serum concentration of 25-hydroxyvitamin D in autism spectrum disorder: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry. 2016;25(4):341–50.
Coşkun S, Şimşek Ş, Camkurt MA, Çim A, Çelik SB. Association of polymorphisms in the vitamin D receptor gene and serum 25-hydroxyvitamin D levels in children with autism spectrum disorder. Gene. 2016;588(2):109–14.
Schmidt RJ, Hansen RL, Hartiala J, Allayee H, Sconberg JL, Schmidt LC, Volk HE, Tassone F. Selected vitamin D metabolic gene variants and risk for autism spectrum disorder in the CHARGE study. Early Hum Dev. 2015;91(8):483–9.
Nissen J, Rasmussen LB, Ravn-Haren G, Andersen EW, Hansen B, Andersen R, Mejborn H, Madsen KH, Vogel U. Common variants in CYP2R1 and GC genes predict vitamin D concentrations in healthy Danish children and adults. PLoS One. 2014;9(2):e89907.
Fernell E, Bejerot S, Westerlund J, Miniscalco C, Simila H, Eyles D, Gillberg C, Humble MB. Autism spectrum disorder and low vitamin D at birth: a sibling control study. Mol Autism. 2015;6:3.
Magnusson C, Lundberg M, Lee BK, Rai D, Karlsson H, Gardner R, Kosidou K, Arver S, Dalman C. Maternal vitamin D deficiency and the risk of autism spectrum disorders: population-based study. BJPsych Open. 2016;2(2):170–2.
Vinkhuyzen AA, Eyles DW, Burne TH, Blanken LM, Kruithof CJ, Verhulst F, et al. Gestational vitamin D deficiency and autism-related traits: the Generation R Study. Mol Psychiatry. 2016. doi:10.1038/mp.2016.213.
Chen J, Xin K, Wei J, Zhang K, Xiao H. Lower maternal serum 25(OH) D in first trimester associated with higher autism risk in Chinese offspring. J Psychosom Res. 2016;89:98–101.
Karohl C, Su S, Kumari M, Tangpricha V, Veledar E, Vaccarino V, Raggi P. Heritability and seasonal variability of vitamin D concentrations in male twins. Am J Clin Nutr. 2010;92(6):1393–8.
Fan X, Warner M, Gustafsson JA. Estrogen receptor beta expression in the embryonic brain regulates development of calretinin-immunoreactive GABAergic interneurons. Proc Natl Acad Sci U S A. 2006;103:19338–43.
Baksi SN, Kenny AD. Estradiol-induced stimulation of 25-hydroxyvitamin D3-1-hydroxylase in vitamin D-deficient Japanese quail. Pharmacology. 1980;20(6):298–303.
Harmon QE, Umbach DM, Baird DD. Use of estrogen-containing contraception is associated with increased concentrations of 25-hydroxy vitamin D. J Clin Endocrinol Metab. 2016;101(9):3370–7.
Olmos-Ortiz A, García-Quiroz J, López-Marure R, González-Curiel I, Rivas-Santiago B, Olivares A, Avila E, Barrera D, Halhali A, Caldiño F, Larrea F, Díaz L. Evidence of sexual dimorphism in placental vitamin D metabolism: testosterone inhibits calcitriol-dependent cathelicidin expression. J Steroid Biochem Mol Biol. 2016;163:173–82.
Alfawaz HA, Bhat RS, Al-Ayadhi L, et al. Protective and restorative potency of vitamin D on persistent biochemical autistic features induced in propionic acid-intoxicated rat pups. BMC Complement Altern Med. 2014;14:416.
Jia F, Wang B, Shan L, Xu Z, Staal WG, Du L. core Symptoms of autism improved after vitamin D supplementation. Pediatrics 2015;135(1):e196–e198.
Saad K, Abdel-Rahman AA, Elserogy YM, et al. Vitamin D status in autism spectrum disorders and the efficacy of vitamin D supplementation in autistic children. Nutr Neurosci. 2015;19(8):346-351.
Feng J, Shan L, Du L. et al. Clinical improvement following vitamin D3 supplementation in autism Spectrum disorder. Nutr Neurosci. 2016. doi:10.1080/1028415X.2015.1123847.
İbili Ucuz II İ, Dursun OB, Esin IS, et al. The relationship between vitamin D, autistic spectrum disorders, and cognitive development: do glial cell line-derived neurotrophic factor and nerve growth factor play a role in this relationship? Int J Dev Disab. 2015;61(4):222–30.
Saad K, Abdel-Rahman AA, Elserogy YM. Al-Atram AA. Othman HA, et al. Randomized controlled trial of vitamin D supplementation in children with autism spectrum disorder. J Child Psychol Psychiatry: El-Houfey AA. 2016. doi:10.1111/jcpp.12652.
Stubbs G, Henley K, Green J. Autism: will vitamin D supplementation during pregnancy and early childhood reduce the recurrence rate of autism in newborn siblings? Med Hypotheses. 2016;88:74–8.
Hollis BW, Wagner CL. Vitamin D requirements during lactation: high-dose maternal supplementation as therapy to prevent hypovitaminosis D for both the mother and the nursing infant. Am J Clin Nutr. 2004;80(6 Suppl):1752S–8S.
Við Streym S, Højskov CS, Møller UK, Heickendorff L, Vestergaard P, Mosekilde L, Rejnmark L. Vitamin D content in human breast milk: a 9-mo follow-up study. Am J Clin Nutr 2016;103(1):107–114.
Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988-1994 compared with 2000-2004. Am J Clin Nutr. 2008;88(6):1519–27.
Lebbé C, Robert C, Ricard S, Sassolas B, Grange F, Saiag P, Lhomel C, Mortier L. Evolution of sun-protection measures for children. J Eur Acad Dermatol Venereol. 2015;29(Suppl 2):20–2.
Holick MF. Photosynthesis of vitamin D in the skin: effect of environmental and life-style variables. Fed Proc. 1987;46:1876–82.
Ekwaru JP, Zwicker JD, Holick MF, Giovannucci E, Veugelers PJ. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS One. 2014;9(11):e111265.
Wagner CL, McNeil RB, Johnson DD, Hulsey TC, Ebeling M, Robinson C, Hamilton SA, Hollis BW. Health characteristics and outcomes of two randomized vitamin D supplementation trials during pregnancy: a combined analysis. J Steroid Biochem Mol Biol. 2013;136:313–20.
Wagner CL, McNeil R, Hamilton SA, Winkler J, Rodriguez Cook C, Warner G, Bivens B, Davis DJ, Smith PG, Murphy M, Shary JR, Hollis BW. A randomized trial of vitamin D supplementation in 2 community health center networks in South Carolina. Am J Obstet Gynecol. 2013;208(2):137.e1–13.
Hollis BW, Johnson D, Hulsey TC, Ebeling M, Wagner CL. Vitamin D supplementation during pregnancy: double-blind, randomized clinical trial of safety and effectiveness. J Bone Miner Res. 2011;26(10):2341–57.
Luxwolda MF, Kuipers RS, Kema IP, Dijck-Brouwer DA, Muskiet FA. Traditionally living populations in East Africa have a mean serum 25-hydroxyvitamin D concentration of 115 nmol/l. Br J Nutr. 2012;108(9):1557–61.
Hollis BW, Wagner CL, Howard CR, Ebeling M, Shary JR, Smith PG, Taylor SN, Morella K, Lawrence RA, Hulsey TC. Maternal versus infant vitamin D supplementation during lactation: a randomized controlled trial. Pediatrics. 2015;136(4):625–34.
Briefel R, Hanson C, Fox MK, et al. Feeding infants and toddlers study: do vitamin and mineral supplements contribute to nutrient adequacy or excess among US infants and toddlers? J Am Diet Assoc 2006;106(1 Suppl. 1):S52–65.
Perrine CG, Sharma AJ, Jefferds ME, et al. Adherence to vitamin D recommendations among US infants. Pediatrics. 2010;125(4):627–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
JJC is president of the non-profit Vitamin D Council; he receives remuneration from Purity Products.
Human and animal studies
No humans or animals were used in this study.
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Cannell, J.J. Vitamin D and autism, what’s new?. Rev Endocr Metab Disord 18, 183–193 (2017). https://doi.org/10.1007/s11154-017-9409-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-017-9409-0