Abstract
Background During care transitions, discrepancies and medication errors often occur, putting patients at risk, especially older patients with polypharmacy. Objective To assess the results of a medication reconciliation and information programme for discharge of geriatric patients conducted through hospital information systems. Setting A 1300-bed university hospital in Madrid, Spain. Method A prospective observational study. Geriatricians selected candidates for medication reconciliation at discharge, and sent an electronic inter-consultation request to the pharmacy department. Pharmacists reviewed the medication list, comparing it with electronic prescriptions, medication previously prescribed by primary care physicians and other medical records, and resolved any discrepancies. An individualized and tailored drug information at discharge sheet was sent to geriatricians and made available to primary care physicians. Main outcome measure The number and type of discrepancies, the number, type and severity of errors, and the main pharmacological groups involved. Results Medication reconciliation was performed for 118 patients with a mean age of 87 years (SD 5.9), involving a total of 2054 medications, or 17.4 per patient. Discrepancies were found in 723 (35 %) drugs, 105 of which were considered medication errors (15 %); 66 patients (56 %) had at least one error. This gave 0.9 reconciliation errors per patient reviewed and 1.6 per patient with errors. Of the 105 errors, 14 (13 %) were considered serious. The most frequent errors were incomplete prescriptions (40 %) and omissions (35 %). Conclusion An electronic medication reconciliation programme helps pharmacists detect serious medication errors in frail elderly patients and provides complete and up-to-date written information to prevent additional errors at home.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impacts on practice
-
Detecting medication discrepancies and giving drug information at discharge becomes even more necessary and complex with highly polymedicated older patients.
-
Working in multidisciplinary teams and using information technology is crucial in implementing and maintaining a medication reconciliation program in a hospital with significant physical barriers to contact between pharmacists, other healthcare professionals and patients.
-
Medication reconciliation can be an important training tool for newly qualified professionals to prevent medication errors.
Introduction
Transitions of care, such as hospital admission and discharge, place hospital in-patients at risk of errors in medication from poor communication or loss of information. One-third of the medication discrepancies that occur during admission or discharge processes cause harm to patients [1]. Medication reconciliation has the potential to identify many of these discrepancies and so reduce harm to patients [2, 3].
Medication reconciliation requires staff to compile a full list of the patient’s previous medication, make a systematic comparison with the active prescription, and analyse and resolve any discrepancies [4, 5]. This process can be performed at different stages of hospital care, such as admission or discharge, and during perioperative periods [6].
Estimates for the presence of at least one unjustified discrepancy in the pharmacotherapeutic records of hospitalised patients have been shown to vary from 10 to 67 % [7], while other sources have shown that over 67 % of patients have discrepancies in their medication when admitted to hospital, with such discrepancies remaining at discharge [8].
Discrepancies, errors, and omissions can be harmful, both during and after hospitalisation, and can lead to inadequate prescriptions or interruption of treatment [7]. Studies have shown that over 25 % of identified errors carry a risk of clinical harm to the patient [9]. The Joint Commission on Accreditation of Healthcare Organizations states that errors in medication reconciliation endanger the patient’s safety and demands that all healthcare organisations establish accredited reconciliation programmes [10, 11].
Approximately 27 % of the medication errors that take place in hospital are due to incomplete medical records at admission. New technologies, such as electronic prescriptions, are indeed useful, but they alone are not sufficient to prevent such errors in medication. Total integration between primary healthcare and hospitals is needed [12], which is why our organisation implemented a medication reconciliation programme. According to published studies, such a programme can reduce errors by up to 70 %, and adverse effects of medication by more than 15 % [13].
Older polymedicated patients are at the greatest risk of medication errors [14]. Up to 53 % of these patients may experience reconciliation errors during their hospital stay, amounting to 14 % of prescribed drugs [15]. There have been a few studies on medication reconciliation programmes in geriatric departments, but most of these were with patients between 65 and 76 years of age [15–18], with few considering patients over 80 years of age [9, 19, 20].
Aim of the study
This study aimed to analyse and quantify the results of a medication reconciliation and information programme during discharge of geriatric patients. The programme was conducted through hospital information systems.
Ethics approval
This study was approved by the Clinical Research Ethics Committee of the University Hospital, Madrid, Spain (PI-1836).
Methods
A prospective observational study was conducted in a 1300-bed university hospital in Madrid, Spain, between January 2013 and April 2014. The hospital performed daily pharmaceutical validation of electronic prescriptions. The study took place in a geriatrics department, and records from a total of 476 patients admitted were considered; 449 (94 %) had presented at the emergency department and 27 at a geriatric outpatient clinic.
The inclusion criteria were patients over 75 years of age with five or more prescribed medications, who were discharged alive. Patients who were discharged to nursing homes or to other hospital units were excluded from the study. This was because other health professionals were going to be in charge of medication, and so would prepare their own drug information sheets.
The programme design followed the recommendations of the European Union Network for Patient Safety and Quality of Care for safe clinical practice on medication reconciliation, part of Work Package 5 (WP5: Patient Safety Initiatives Implementation) [21]. Recommendations made by Martín de Rosales [14] were also taken into consideration.
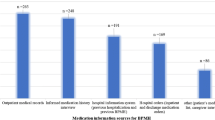
The medication reconciliation process involved a geriatrician selecting candidates for medication reconciliation and performing initial interviews, including taking a pharmacotherapeutic history for each patient. On the last day of the patient’s hospital stay, the clinician asked the hospital pharmacy department for a reconciliation process, using an electronic inter-consultation request. The pharmacist reviewed the medication list at discharge, and compared it with the list registered in the electronic prescription (Farmatools®; Dominion, Bilbao, Spain), medication previously prescribed by the primary care physician (Horus® Information System, Madrid, Spain), and other medical reports. The pharmacist and physician discussed any discrepancies, and a drug information at discharge sheet (DIDS) was completed.
The DIDS was designed by a multidisciplinary team, and prepared using an Access® database (Microsoft, Seattle, WA, USA). It included patient identification data, date of discharge, contact information, and the list of medication prescribed at discharge. For every drug listed, the pharmacist provided detailed information about when, how, and how much to take, its relation to food consumption, the duration of treatment, possible side effects and storage conditions (if necessary). Colour and large print size were used to help the study patients to better read and understand the information.
The DIDS was printed through the hospital network and sent to the hospital clinical station. It was also accessible to primary care physicians through the Horus® visor information system. The geriatrician gave the DIDS to the patient with other discharge documents, and also explained it orally.
The physical separation between pharmacists and patients required pharmacists to invest extra time in the reconciliation process. This limitation was addressed by clearly assigning distinct responsibilities to medical and pharmaceutical practitioners. Geriatricians were in continuous contact with patients and traditionally interviewed them at admission. They therefore continued to do so, while pharmacists were given responsibility for investigating electronic resources, analysing the treatment regime and developing the drug information sheet.
Data analysis
The following data were collected for each patient: age, sex, prescribed medication, medication list at discharge, documented discrepancies (included in clinical records), undocumented intentional discrepancies (required clarification by physicians), unintentional discrepancies (reconciliation errors), unresolved discrepancies, and the medication groups involved when errors were found.
The Consensus Document on Classification and Terminology of Medication Reconciliation of the Spanish Society of Hospital Pharmacy was used to classify discrepancies and errors [22]. Any difference between previous patient medication and the actual prescription given in hospital was considered a ‘discrepancy’. Most of these discrepancies were to adjust ongoing medication to a new clinical status, and were defined as ‘documented discrepancies’. The remaining discrepancies were categorised as ‘undocumented discrepancies’, and required clarification by a physician (e.g. omissions of medication, different dosages). After discussion with a clinician, they were finally classified as ‘intentional’ or ‘unintentional’. Indicators established by the European WP5 working group were calculated. The severity of reconciliation errors was determined using the National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP) classification [23]. This has nine categories ranging from “A) Circumstances or events that have the capacity to cause error” to “I) An error occurred that may have contributed to or resulted in the patient’s death”. The Anatomical Therapeutic Chemical classification system of the World Health Organization was used to provide the therapeutic group for the analysis of medication errors [24].
Statistical analysis
Statistical analysis used SPSS version 11.5. Continuous quantitative variables were calculated as the mean and standard deviation (SD) or interquartile range. Qualitative variables were calculated as absolute and relative frequencies. Comparisons between quantitative variables used the Mann–Whitney non-parametric test. Frequency analysis between qualitative variables used Fisher’s exact test, and correlation analysis between quantitative continuous variables used Spearman’s rank-order correlation.
Results
During the study period, 476 patients were admitted to the geriatrics department. Their ages ranged from 64 to 105 years, with a mean age of 87 years. The mean hospital stay was 8.6 days and the mean number of diagnoses per patient was 10.6. The most frequent reasons for admission were heart failure (12.1 %), respiratory tract infection (10.2 %), pneumonia (9.1 %), sepsis of unknown origin (8.5 %), urinary tract infection (7.6 %), and gastrointestinal disorders (7.4 %).
Medication reconciliation was performed for 118 patients who met the inclusion criteria. Their mean age was 87 years (SD 5.9) and 52 % were male. A total of 2054 medications were reviewed, or 17.4 reconciled medications per patient. Data were obtained on 685 items of medication from hospital medical records, and on 246 from the Horus® Information System. In total, 1156 items of medication were reported in the DIDS (1123 reviewed drugs and 33 new prescriptions added after pharmacist intervention for new indications not treated at discharge). This equated to a mean of 9.8 documented items of medication per patient at discharge.
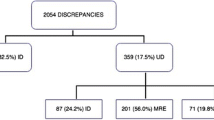
In total, 723 discrepancies were found (35 % of the reconciled medications). Of these, 486 (67 %) were justified without requiring additional explanation (documented discrepancies) and 132 (18 %) were justified after contacting the geriatrician (undocumented intentional discrepancies). The remaining 105 (15 %) were classified as reconciliation errors or unintentional discrepancies (44 % of the discrepancies that required contact with the geriatrician), and represented 5 % of the total number of medication items reviewed. There were no unresolved discrepancies. A weak but statistically significant correlation was found between the number of reconciled items of medication and the number of errors per patient (R = 0.276; p = 0.002). The mean number of errors made in prescriptions was greater when prescriptions were provided by a resident physician (1.02 errors per reconciliation process; SD 1.11) rather than an attending physician (0.65; SD 0.86; p = 0.05).
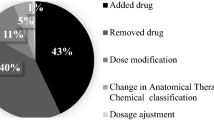
In total, 56 % of the patients (n = 66) suffered at least one reconciliation error, a rate of 0.9 reconciliation errors per reconciled patient and 1.6 reconciliation errors per patient with errors. The most frequent errors were incomplete prescriptions (40 %) and omitted medication (35 %) (Fig. 1).
The classification of errors by therapeutic group (Fig. 2) showed that the most frequent errors in medication were for drugs for the alimentary tract and metabolism (group A), particularly vitamin (e.g., vitamin D) and mineral supplements (e.g., calcium and iron). Nervous system medication such as psycholeptics and psychoanaleptics (group N) showed the next highest error rate, followed by cardiovascular system medication (antihypertensives, diuretics, and beta-blockers; group C), beta2-agonists and inhaled anticholinergics (group R), and the remaining medication groups.
According to the adapted classification of the NCCMERP [23], 26 % (n = 27) of the errors would not have reached the patient (category B); 33 % (n = 35) would have reached the patient, but were unlikely to have caused any harm (category C); 28 % (n = 29) would have reached the patient and would have required monitoring and/or intervention to prevent harm (category D); 11 % (n = 12) would have caused temporary harm (category E); and 2 % (n = 2) would have led to hospitalisation or prolongation of stay (category F). This suggests that 13 % (n = 14) could be considered severe (categories E–I).
All the patients selected for medication reconciliation received their DIDS at discharge.
Discussion
Strengths and limitations
The low levels of direct contact between pharmacists and patients due to their physical separation is a possible limitation of this study. These distances, however, led to the development of an electronic workflow system to permit pharmacists to reconcile patients’ medication from anywhere in the hospital complex. An additional limitation is that we could not reconcile 100 % of the patients discharged from the geriatrics department. Our results, however, substantially exceeded the initial 50 % goal, set with the limited resources in mind. Our results are not necessarily generalisable for patients going into care or transferring to other hospitals.
Population and medication
In the patient cohort in this study, which was characterised by the inclusion of very old acute patients, a mean of 17.4 drugs were reconciled per examined patient. Written information was provided for a mean of 9.8 items of medication per patient. These data confirm high rates of polypharmacy in this age group, indicating the value of medication reconciliation programmes, in line with the studies of Martín de Rosales [14] and Delgado et al. [15].
Discrepancies and medication errors
Discrepancies were found in one-third of the items of medication reconciled. Of the unjustified discrepancies, 44 % were considered to be reconciliation errors, which is significantly lower than the 86 % (555 errors in 644 unjustified discrepancies) described by Delgado et al. [15] in a study on older polymedicated inpatients. Their study showed a 13.9 % error rate, compared with ours of 5 %.The rate of 1.6 errors per patient with any error is comparable to the results of Hernández et al. [16] from a sample of patients admitted to a short stay unit, although patients in that study had a significantly lower mean age (74 ± 14.5 years). Our data show that attending physicians made fewer reconciliation errors than more junior doctors. This was expected because the more junior (resident) physicians had less experience of medication reconciliation.
The percentage of patients with at least one reconciliation error (56 %) in our study was only slightly higher than the 54 % found by Cornish et al. [17] in patients with a mean age of 77 years in an internal medicine department, or the 53 % result of Delgado et al. [15] for patients with a mean age of 76 years.
The type of errors detected most frequently (incomplete prescriptions, omission and dosage errors) were also among the most frequent found in other studies [16, 17]. Of the errors detected, 13 % were considered potentially serious (categories E–I of the NCCMERP [23]), which is similar to the 15 % found by Delgado et al. [15]. The types of errors encountered are also similar to those observed by Andreoli et al. [19] in a 6-month study of 170 patients in an internal medicine department (with a mean age of 82 years). Andreoli and colleagues also found that reconciliation errors involved drugs for the digestive system (25.7 %), cardiovascular system (24 %), and nervous system (19.4 %). Quélennec et al. [9] found similar results for these treatment groups: 20, 18, and 22 %, respectively.
Although our results are similar to those reported in other studies, it is worth noting that our study population was potentially more vulnerable to suffering harmful consequences because of their higher mean age. Most of the previous studies were performed in internal medicine departments, with very few in geriatric departments [20]. The clinical consequences of discrepancies leading to errors in medication are potentially more serious in frail elderly patients than in younger adults. Serious complications could have occurred in our study, as high-risk drugs such as anticoagulants or cardiovascular agents were involved.
Our study highlights the efficacy of medication reconciliation programmes. Previous studies on polymedicated patients reported a significant decrease in 30-day readmissions: 16.8 % when using medication reconciliation versus 26 % (p = 0.006) when reconciliation was not performed. This equates to an absolute risk reduction of 9.2 (10.8 reconciled patients to prevent one 30-day readmission), with consequent cost savings [25], which is consistent with our assessment of serious errors avoided.
Medication information
In a Spanish primary care study, 19.4 % of the surveyed patients declared that they had experienced medication errors. The main causes were physician attention deficits during consultation, and poor provision of information. This demonstrated that insufficient information on medication leads to increased errors [26]. The DIDS provided by the pharmacist is therefore considered critical in ensuring that complete medication information is provided to patients, to avoid medication errors at home. This information sheet also transmits information between hospital and primary care, as a copy is provided in the shared information system. Existing hospital technologies have been crucial to implementing, maintaining and expanding the medication reconciliation programme. Additional economic investments have been avoided.
Implications for practice and research
We have developed a methodology to overcome physical barriers to medication reconciliation. The methodology is reproducible and easy to implement in organizations with similar information technologies. Medication reconciliation can also be a tool to help resident physicians identify and learn about their own prescription errors during care transitions. This project required close collaboration between healthcare providers. Our results suggest that it may be useful to perform additional controlled experimental studies to find out whether electronic medication reconciliation, along with the DIDS, decreases adverse events at home after discharge.
Conclusion
An electronic medication reconciliation programme supports pharmacists in the detection of serious medication errors in frail elderly patients. It also provides complete and up-to-date written information contributing to the prevention of medication errors at home following discharge.
References
Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices a systematic review. Arch Intern Med. 2012;172(14):1057–69.
Delgado Sánchez O, Anoz Jiménez L, Serrano Fabiá A, Pico JN. Medication reconciliation. Med Clin. 2007;129(9):343–8 (Spanish).
Lehnbom EC, Stewart MJ, Manias E, Westbrook JI. Impact of medication reconciliation and review on clinical outcomes. Ann Pharmacother. 2014;48(10):1298–312.
Institute for Healthcare Improvement [Internet]. Cambridge (MA): Medication reconciliation review. c2015 [cited 2015 Sept 17]. http://www.ihi.org/resources/Pages/Tools/MedicationReconciliationReview.aspx.
Institute for Safe Medication Practices Canada (ISMP Canada) [Internet]. Toronto: Medication reconciliation in Acute Care Getting Started Kit. Version 3.0.2011. c2000–2015 [cited 2015 Sept 15]. http://www.ismp-canada.org/medrec/.
Instituto para el Uso Seguro de Medicamentos y Productos Sanitarios (ISMP-España) [Internet]. Salamanca: [Recommendations for prevention of medication errors]. 2011 Dec. c2015 [cited 2015 Sept 18]. http://www.ismp-espana.org/ficheros/Bolet%C3%ADn%20n%C2%BA%2034%20%28Diciembre%202011%29.pdf (Spanish).
Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173(5):510–5. doi:10.1503/cmaj.045311 (Spanish).
Kwan JL, Lo L, Sampson M, Shojania KG. Medication reconciliation during transitions of care as a patient safety strategy. A systematic review. Ann Intern Med. 2013;158(5_Part_2):397–403. doi:10.7326/0003-4819-158-5-201303051-00006.
Quélennec B, Beretz L, Paya D, Blicklé JF, Gourieux B, Andrès E, et al. Potential clinical impact of medication discrepancies at hospital admission. Eur J Intern Med. 2013;24(6):530–5. doi:10.1016/j.ejim.2013.02.007.
Joint Commission on Accreditation of Healthcare Organization [Internet]. United States: National Patient Safety Goals. Goal 3 (NPSG.03.05.01). c2015 [cited 2015 Sept 8]. http://www.jointcommission.org/assets/1/6/2015_NPSG_HAP.pdf.
Joint Commission on Accreditation of Healthcare Organizations [Internet]. United States: Sentinel Event Alert/Topics Library Updates: issue 35; 2006 Jan 25 [updated 2006 Feb 9; cited 2015 Aug 25]. http://www.jointcommission.org/assets/1/18/SEA_35.pdf.
Villamañán E, Larrubia Y, Ruano M, Vélez M, Armada E, Herrero A, Álvarez-Sala R. Potential medication errors associated with computer prescriber order entry. Int J Clin Pharm. 2013;35(4):577–83. doi:10.1007/s11096-013-9771-2.
Zoni AC, Durán García ME, Jiménez Muñoz AB, Salomón Pérez R, Martín P, Herranz Alonso A. Impact of medication reconciliation program at admission in an internal medicine department. Eur J Int Med. 2012;23:696–700. doi:10.1016/j.ejim.2012.08.013.
Martín de Rosales Cabrera AM. Multidisciplinary coordination to ensure correct patient medication: medication reconciliation. Rev Calid Asist. 2010;25(5):239–43. doi:10.1016/j.cali.2010.04.003 (Spanish).
Delgado Sánchez O, Nicolás Picó J, Martínez López I, Serrano Fabiá A, Anoz Jiménez L, Fernández Cortés F. Reconciliation errors at admission and departure in old and polymedicated patients. Prospective, multicenter randomized study. Med Clin (Barc). 2009;133(19):741–4. doi:10.1016/j.medcli.2009.03.023 (Spanish).
Hernández C, Mira A, Arroyo E, Díaz M, Andreu L, Sánchez MI. Conciliation discrepancies at hospital discharge. Aten Primaria. 2008;40(12):597–601 (Spanish).
Cornish PL, Knowles SR, Marchesano R, Tam V, Shadowitz S, Juurlink DN, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165(4):424–9.
Alfaro-Lara ER, Santos-Ramos B, González-Méndez AI, Galván-Banqueri M, Vega-Coca MD, Nieto-Martín MD, et al. Medication reconciliation on hospital admission in patients with multiple chronic diseases using a standardised methodology. Rev Esp Geriatr Gerontol. 2013;48(3):103–8. doi:10.1016/j.regg.2012.11.011 (Spanish).
Andreoli L, Alexandra JF, Tesmoingt C, Eerdekens C, Macrez A, Papo T, et al. Medication reconciliation: a prospective study in an internal medicine unit. Drugs Aging. 2014;31(5):387–93.
Peña Pedrosa JA, Santiago Pérez A, Bilbao Gómez-Martino C, Arias Fernández L. Influence of a medication reconciliation program in elderly patients on readmission rate. Pharm Care Esp [Internet]. 2014 [cited 2015 Aug 28];16(4):130–141. http://www.pharmcareesp.com/index.php/PharmaCARE/article/view/185/167. (Spanish).
European Union Network for Patient Safety and Quality of Care [Internet]. Saint-Denis La Plaine: Safe Clinical Practices for Implementation (WP5); c2012 [cited 2015 Aug 26]. http://www.pasq.eu/Wiki/SCP.aspx.
Roure C, Aznar T, Delgado O, Fuster L, Villar I, et al. Consensus document on terminology and classification in medication reconciliation. Barcelona: Ediciones Mayo; 2009. ISBN 978-84-9905-044-7. http://www.sefh.es/bibliotecavirtual/conciliacion/Libro_consenso_terminologia_conciliacion.pdf (Spanish).
Hartwig SC, Denger SD, Schneider PJ. Severity-indexed, incident report-based medication error-reporting program. Am J Hosp Pharm. 1991;48(12):2611–6.
World Health Organization Collaborating Centre for Drug Statistics Methodology [Internet]. Oslo: ATC/DDD Index 2015. C2015 [updated 2013 Dec 19; cited 2015 Jun 19]. http://www.whocc.no/atc_ddd_index/.
Pal A, Babbott S, Wilkinson ST. Can the targeted use of a discharge pharmacist significantly decrease 30-day readmissions? Hosp Pharm. 2013;48(5):380–8. doi:10.1310/hpj4805-380.
Mira JJ, Navarro IM, Guilabert M, Aranaz J. Frequency of medication errors by patients. Rev Panam Salud Publica. 2012;31(2):95–101 (Spanish).
Acknowledgments
We are grateful to Dr. Alberto Pardo Hernández for his support and collaboration in the structure of the project and to Dr. César Nombela Arrieta for his invaluable help in publishing it.
Funding
No funding support was obtained for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Moro Agud, M., Menéndez Colino, R., Mauleón Ladrero, M.d. et al. Analysis of an electronic medication reconciliation and information at discharge programme for frail elderly patients. Int J Clin Pharm 38, 996–1001 (2016). https://doi.org/10.1007/s11096-016-0331-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-016-0331-4